The Association between Social Vulnerability and Frailty in Community Dwelling Older People: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion Criteria and Study Identification
2.3. Data Extraction and Management
2.4. Quality Appraisal
3. Results
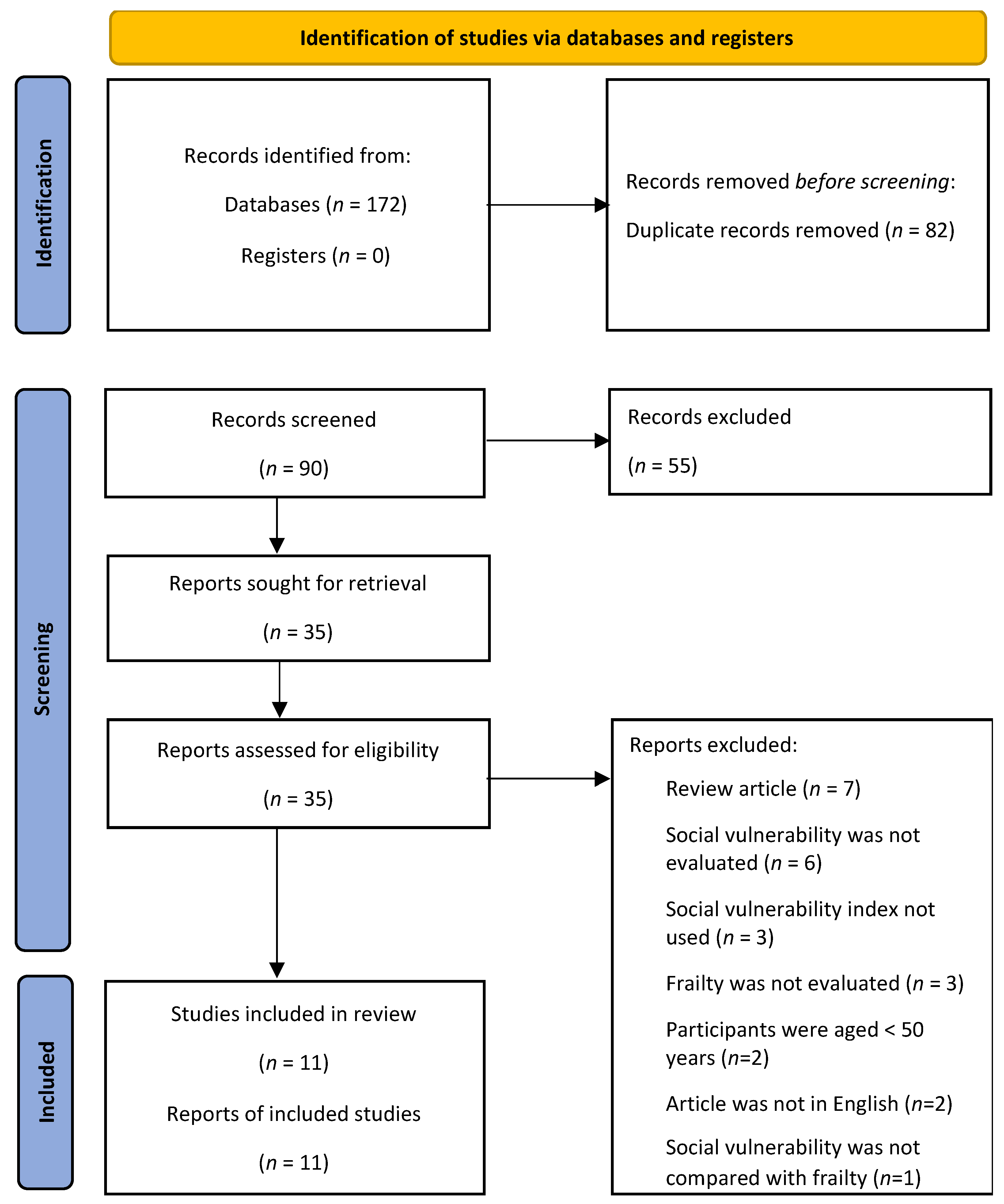
3.1. Article Selection Process
3.2. Study Characteristics
3.3. Social Vulnerability and Frailty Levels
3.4. Social Vulnerability and Mortality
3.5. Association between Social Vulnerability and Frailty
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- United Nations Department of Economic Social Affairs Population Division. World Population Prospects 2019; United Nations: New York, NY, USA, 2019. [Google Scholar]
- Spiers, G.; Matthews, F.E.; Moffatt, S.; Barker, R.O.; Jarvis, H.; Stow, D.; Kingston, A.; Hanratty, B. Impact of social care supply on healthcare utilisation by older adults: A systematic review and meta-analysis. Age Ageing 2019, 48, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Andrew, M.K.; Keefe, J.M. Social vulnerability from a social ecology perspective: A cohort study of older adults from the National Population Health Survey of Canada. BMC Geriatr. 2014, 14, 90. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.N.; Ngangue, P.; Bouhali, T.; Ryan, B.L.; Stewart, M.; Fortin, M. Social Vulnerability in Patients with Multimorbidity: A Cross-Sectional Analysis. Int. J. Environ. Res. Public Health 2019, 16, 1244. [Google Scholar] [CrossRef] [PubMed]
- Shega, J.W.; Andrew, M.; Hemmerich, J.; Cagney, K.A.; Ersek, M.; Weiner, D.K.; Dale, W. The relationship of pain and cognitive impairment with social vulnerability--an analysis of the Canadian Study of Health and Aging. Pain Med. 2012, 13, 190–197. [Google Scholar] [CrossRef]
- De Jonge, P.; Huyse, F.J.; Ruinemans, G.M.F.; Stiefel, F.C.; Lyons, J.S.; Slaets, J.P.J. Timing of psychiatric consultations—The impact of social vulnerability and level of psychiatric dysfunction. Psychosomatics 2000, 41, 505–511. [Google Scholar] [CrossRef]
- Bilotta, C.; Case, A.; Nicolini, P.; Mauri, S.; Castelli, M.; Vergani, C. Social vulnerability, mental health and correlates of frailty in older outpatients living alone in the community in Italy. Aging Ment. Health 2010, 14, 1024–1036. [Google Scholar] [CrossRef]
- Sulander, T.; Pohjolainen, P.; Karvinen, E. Self-rated health (SRH) and socioeconomic position (SEP) among urban home-dwelling older adults. Arch. Gerontol. Geriatr. 2012, 54, 117–120. [Google Scholar] [CrossRef]
- Cappelli, M.; Bordonali, A.; Giannotti, C.; Montecucco, F.; Nencioni, A.; Odetti, P.; Monacelli, F. Social vulnerability underlying disability amongst older adults: A systematic review. Eur. J. Clin. Investig. 2020, 50, e13239. [Google Scholar] [CrossRef]
- Searle, S.D.; Mitnitski, A.; Gahbauer, E.A.; Gill, T.M.; Rockwood, K. A standard procedure for creating a frailty index. BMC Geriatr. 2008, 8, 24. [Google Scholar] [CrossRef]
- Cesari, M.; Calvani, R.; Marzetti, E. Frailty in Older Persons. Clin. Geriatr. Med. 2017, 33, 293–303. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M157. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez-Robledo, L.; Avila-Funes, J. How to Include the Social Factor for Determining Frailty? J. Frailty Aging 2012, 1, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Andrew, M.K. Frailty and social vulnerability. In Frailty in Aging. Biological, Clinical and Social Implications. Interdisciplinary Topics in Gerontology and Geriatrics; Theou, O., Rockwood, K., Eds.; Karger: Basel, Switzerland, 2015; Volume 41, pp. 186–195. [Google Scholar] [CrossRef]
- Andrew, M.K. Social Vulnerability in Old Age. In Brocklehurst’s Textbook of Geriatric Medicine and Gerontology, 7th ed.; Fillit, H.M., Rockwood, K., Woodhouse, K., Eds.; W.B. Saunders: Philadelphia, PA, USA, 2010; pp. 198–204. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welch, V. Cochrane Handbook for Systematic Reviews of Interventions; Cochrane: London, UK, 2021. [Google Scholar]
- Deeks, J.J.; Higgins, J.P.; Altman, D.G. Chapter 10: Analysing data and undertaking meta-analyses. In Cochrane Handbook for Systematic Reviews of Interventions, version 6.3 (updated February 2022) ed.; Higgins, J., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M., Welch, V., Eds.; Cochrane: London, UK, 2022; Available online: www.training.cochrane.org/handbook (accessed on 26 August 2022).
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557. [Google Scholar] [CrossRef] [PubMed]
- RStudio Team. RStudio: Integrated Development Environment for R. RStudio; RStudio PBC: Boston, MA, USA, 2022. [Google Scholar]
- Harrer, M.; Cuijpers, P.; Furukawa, T.A.; Ebert, D.D. Doing Meta-Analysis with R: A Hands-On Guide, 1st ed.; Chapman & Hall: Boca Raton, FL, USA; CRC Press: London, UK, 2021. [Google Scholar]
- Hopkins, W.G.; Marshall, S.W.; Batterham, A.M.; Hanin, J. Progressive statistics for studies in sports medicine and exercise science. Med. Sci. Sports Exerc. 2009, 41, 3–12. [Google Scholar] [CrossRef]
- Downs, S.H.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef]
- Hooper, P.; Jutai, J.W.; Strong, G.; Russell-Minda, E. Age-related macular degeneration and low-vision rehabilitation: A systematic review. Can. J. Ophthalmol. 2008, 43, 180–187. [Google Scholar] [CrossRef]
- Abeliansky, A.L.; Erel, D.; Strulik, H. Social vulnerability and aging of elderly people in the United States. SSM-Popul. Health 2021, 16, 100924. [Google Scholar] [CrossRef]
- Armstrong, J.J.; Andrew, M.K.; Mitnitski, A.; Launer, L.J.; White, L.R.; Rockwood, K. Social vulnerability and survival across levels of frailty in the Honolulu-Asia Aging Study. Age Ageing 2015, 44, 709–712. [Google Scholar] [CrossRef]
- Armstrong, J.J.; Mitnitski, A.; Andrew, M.K.; Launer, L.J.; White, L.R.; Rockwood, K. Cumulative impact of health deficits, social vulnerabilities, and protective factors on cognitive dynamics in late life: A multistate modeling approach. Alzheimers Res. Ther. 2015, 7, 38. [Google Scholar] [CrossRef]
- Andrew, M.K.; Mitnitski, A.B.; Rockwood, K. Social vulnerability, frailty and mortality in elderly people. PLoS ONE 2008, 3, e2232. [Google Scholar] [CrossRef] [PubMed]
- Andrew, M.K.; Rockwood, K. Social vulnerability predicts cognitive decline in a prospective cohort of older Canadians. Alzheimer’s Dement. 2010, 6, 319–325.e1. [Google Scholar] [CrossRef] [PubMed]
- Wallace, L.M.K.; Theou, O.; Pena, F.; Rockwood, K.; Andrew, M.K. Social vulnerability as a predictor of mortality and disability: Cross-country differences in the survey of health, aging, and retirement in Europe (SHARE). Aging Clin. Exp. Res. 2015, 27, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Godin, J.; Theou, O.; Black, K.; McNeil, S.A.; Andrew, M.K. Long-Term Care Admissions Following Hospitalization: The Role of Social Vulnerability. Healthcare 2019, 7, 91. [Google Scholar] [CrossRef]
- Andrew, M.K.; Rockwood, K.; Mitnitski, A.; Kirkland, S.A. The impact of social vulnerability on the survival of the fittest older adults. Age Ageing 2012, 41, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Gu, D.A.; Mitnitski, A. Frailty and life satisfaction in Shanghai older adults: The roles of age and social vulnerability. Arch. Gerontol. Geriatr. 2016, 67, 68–73. [Google Scholar] [CrossRef]
- Sanchez-Garrido, N.; Aguilar-Navarro, S.G.; Avila-Funes, J.A.; Theou, O.; Andrew, M.; Perez-Zepeda, M.U. The Social Vulnerability Index, Mortality and Disability in Mexican Middle-Aged and Older Adults. Geriatrics 2021, 6, 24. [Google Scholar] [CrossRef]
- Cooper, F.; Lewis, E.G.; Urasa, S.; Whitton, L.; Collin, H.; Coles, S.; Wood, G.K.; Ali, A.M.; Mdegella, D.; Mkodo, J.; et al. Social vulnerability, frailty and their association with mortality in older adults living in rural Tanzania. J. Gerontol. A Biol. Sci. Med. Sci. 2022. [Google Scholar] [CrossRef]
- Xiao, Q.; Wu, M.; Zeng, T. Social support networks in Chinese older adults: Health outcomes and health related behaviors: A path analysis. Aging Ment. Health 2019, 23, 1382–1390. [Google Scholar] [CrossRef]
- Song, X.W.; Mitnitski, A.; Rockwood, K. Prevalence and 10-Year outcomes of frailty in older adults in relation to deficit accumulation. J. Am. Geriatr. Soc. 2010, 58, 681–687. [Google Scholar] [CrossRef]
- Reeves, D.; Pye, S.; Ashcroft, D.M.; Clegg, A.; Kontopantelis, E.; Blakeman, T.; van Marwijk, H. The challenge of ageing populations and patient frailty: Can primary care adapt? BMJ 2018, 362, k3349. [Google Scholar] [CrossRef] [PubMed]
- Walkden, G.J.; Anderson, E.L.; Vink, M.P.; Tilling, K.; Howe, L.D.; Ben-Shlomo, Y. Frailty in older-age European migrants: Cross-sectional and longitudinal analyses of the Survey of Health, Aging and Retirement in Europe (SHARE). Soc. Sci. Med. 2018, 213, 1–11. [Google Scholar] [CrossRef] [PubMed]
| Terms | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Community-dwelling older people Aged 50 and above | Studies involving populations in care homes Population included people aged below 50 years |
| Social vulnerability measured using a social vulnerability index | Social vulnerability measured using another tool |
| None | None |
| Frailty measured using a recognized tool | No record of frailty as the outcome or not measured with a recognized tool |
| Cohort studies, cross-sectional studies | Literature review or systematic review |
| Authors | Participants | Sample (n, Age) | Gender (% Female) | Study Design | SVI Items | FI Items | Quality Appraisal |
|---|---|---|---|---|---|---|---|
| Abeliansky et al. (2021) | USA HRS | 17,602 Aged 50+ 68.3 ± 9.7 | 57% | Cohort 12 years | 49 | 38 | 18 |
| Andrew et al. (2008) | Canada CSHA | 3707 77.9 (77.8, 78.1) | 60% | Cohort 5 years | 40 | 31 | 24 |
| Canada NPHS | 2468 73.4 (73.0, 73.7) | 58% | Cohort 8 years | 23 | 36 | 22 | |
| Andrew and Rockwood (2010) | Canada CSHA | 2468 Age 70+ | NS | Cohort 5 years | 40 | 31 | 23 |
| Andrew et al. (2012) | Canada CSHA-2 | 5703 Age 70+ | NS | Cohort 10 years | 40 | 31 | 22 |
| Armstrong et al. (2015a) | Hawaii, USA HAAS | 3271 Aged 72+ | Men only | Cohort 3–6 years | 19 | 58 | 22 |
| Armstrong et al. (2015b) | Hawaii, USA HAAS | 3845 Aged 71+ | Men only | Cohort 3–6 years | 18 | 48 | 22 |
| Cooper et al. (2022) | Tanzania | 235 Aged 60+ 75.2 ± 11.5 | 58% | Cohort 13–19 months | 45 | 37 | 21 |
| Godin et al. (2019) | Canada | 475 Aged 65+ 78.6 ± 7.9 | 58.9% | Cross- sectional | 18 | 39 | 21 |
| Sanchez-Garrido et al. (2021) | Mexico MHAS | 14,217 Age 50+ 63.9 ± 10.1 | 59% | Cohort 3 years | 42 | 60 | 20 |
| Wallace et al. (2015) | Europe SHARE | 18,289 Age 50+ | NS | Cohort 5 years | 32 | 57 | 22 |
| Yang et al. (2016) | China | 1970 Age 65+ | NS | Cross- sectional | 35 | 52 | 21 |
| Authors | Country | Social Vulnerability | Frailty |
|---|---|---|---|
| Abeliansky et al. (2021) | USA | 0.31 ± 0.10 | 0.23 ± 0.16 |
| Andrew et al. (2008) | Canada | CSHA: 0.25 (0.20, 0.31) ‡ | Only histograms provided |
| NPHS: 0.28 (0.21, 0.35) ‡ | |||
| Andrew and Rockwood (2010) | Canada | 0.26 ± 0.09 | 0.16 (0.10, 0.23) ‡ |
| Andrew et al. (2012) | Canada | Not reported | Not reported |
| Armstrong et al. (2015a) | Hawaii, USA | 0.27 ± 0.13 § | 0.15 ± 0.08 § |
| Armstrong et al. (2015b) | Hawaii, USA | 0.25 ± 0.13 § | 0.15 ± 0.09 § |
| Cooper et al. (2022) | Tanzania | 0.47 (0.23) | 0.32 (0.35) |
| Godin et al. (2019) | Canada | 0.30 ± 0.13 § | 0.19 ± 0.10 § |
| Sanchez-Garrido et al. (2021) | Mexico | 0.42 ± 0.12 § | 0.23 ± 0.11 § |
| Wallace et al. (2015) | Europe | Total 0.34 ± 0.09 § Nordic 0.31 ± 0.86 § Continental 0.33 ± 0.09 § Mediterranean 0.36 ± 0.09 § | Total 0.316 ± 0.12 § Nordic 0.13 ± 0.11 § Continental 0.16 ± 0.12 § Mediterranean 0.18 ± 0.13 § |
| Yang et al. (2016) | China | Total 0.15 ± 0.09 § 65–79 0.14 ± 0.09 § 80+ 0.18 ± 0.09 § | Total 0.21 ± 0.15 § 65–79 0.18 ± 0.12 § 80+ 0.30 ± 0.18 § |
| Authors | Dataset | Follow Up | Comparison | Adjustments | n | Effect Statistic (95% CI) |
|---|---|---|---|---|---|---|
| Andrew et al. (2008) | CSHA | 5 years | One more deficit | Age, sex, frailty | 3707 | 1.05 (1.02, 1.07) § |
| 1.03 (1.01, 1.05) | ||||||
| NPHS | 8 years | One more deficit | Age, sex, frailty | 2468 | 1.08 (1.03, 1.14) § | |
| 1.04 (1.01, 1.07) | ||||||
| Andrew et al. (2012) | CSHA | 5 years | Highest third of SVI compared to lowest third | Age, sex | 584 | 2.5 (1.5, 4.3) |
| Age, sex, physical activity, smoking, alcohol | 3.22 (1.80, 5.78) | |||||
| Cooper et al. (2022) | N/A | 16 months | One more deficit | Age, gender, frailty | 235 | 1.06 (0.97, 1.16) |
| Sanchez-Garrido et al. (2021) | MHAS | 3 years | Highest third of SVI compared to lowest third | Physical activity, tobacco, alcohol | 14,217 | 1.7 (1.2, 2.3) |
| Wallace et al. (2015) | SHARE | 5 years | Highest quartile of SVI | Age, sex | 18,289 | 1.88 (1.64, 2.16) |
| Age, sex, frailty, disability | 18,289 | 1.25 (1.07, 1.45) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ayeni, A.; Sharples, A.; Hewson, D. The Association between Social Vulnerability and Frailty in Community Dwelling Older People: A Systematic Review. Geriatrics 2022, 7, 104. https://doi.org/10.3390/geriatrics7050104
Ayeni A, Sharples A, Hewson D. The Association between Social Vulnerability and Frailty in Community Dwelling Older People: A Systematic Review. Geriatrics. 2022; 7(5):104. https://doi.org/10.3390/geriatrics7050104
Chicago/Turabian StyleAyeni, Ayodele, Adrienne Sharples, and David Hewson. 2022. "The Association between Social Vulnerability and Frailty in Community Dwelling Older People: A Systematic Review" Geriatrics 7, no. 5: 104. https://doi.org/10.3390/geriatrics7050104
APA StyleAyeni, A., Sharples, A., & Hewson, D. (2022). The Association between Social Vulnerability and Frailty in Community Dwelling Older People: A Systematic Review. Geriatrics, 7(5), 104. https://doi.org/10.3390/geriatrics7050104







