Pneumonia, Aspiration Pneumonia, or Frailty-Associated Pneumonia?
Abstract
:1. Introduction
2. Pneumonia
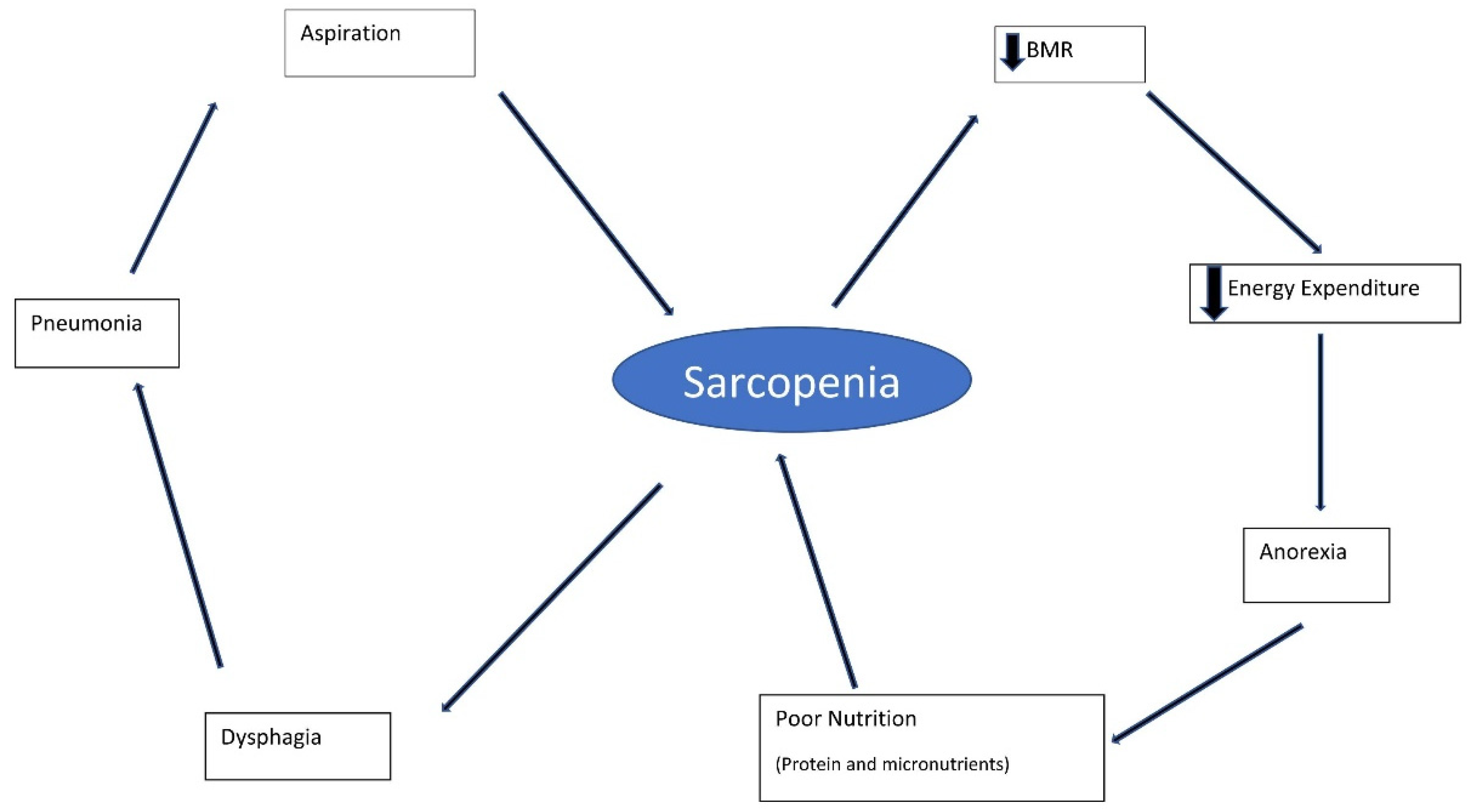
3. Nutrition
4. Frailty and Oral Frailty
5. Frailty and Immunity
6. Lungs and Immunity
7. Dysphagia
8. Pneumonia and Frailty
9. Is It Time for Frailty-Associated Pneumonia?
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eurostats. European Health Information Gateway European Mortality Database. Available online: https://gateway.euro.who.int/en/datasets/european-mortality-database/#population-and-icd-used (accessed on 9 December 2019).
- World Health Organization. World Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2015.
- Smithard, D.G. Dysphagia: A geriatric giant? Med. Clin. Rev. 2016, 2, 5. [Google Scholar] [CrossRef]
- Baijens, L.W.; Clavé, P.; Cras, P.; Ekberg, O.; Forster, A.; Kolb, G.F.; Leners, J.C.; Masiero, S.; Del Nozal, J.M.; Ortega, O.; et al. European Society for Swallowing Disordrs—European Union Geriatric Medicine Society white paper: Oropharyngeal dysphagia as a geriatric syndrome. Clin. Investig. Aging 2016, 11, 1403–1428. [Google Scholar] [CrossRef] [Green Version]
- Higashiguchi, T.; Ohara, H.; Kamakura, Y.; Kikutani, T.; Kuzuya, M.; Enoki, H.; Sanada, H.; Matsuzaki, M.; Maruyama, M. Efficacy of a new post-mouthwash intervention (wiping plus oral nutritional supplements) for preventing aspiration pneumonia in elderly people: A multicentre, randomized, comparative trial. Ann. Nutr. Metab. 2017, 71, 253–260. [Google Scholar] [CrossRef]
- Torres, A.; Peetermans, W.E.; Viegi, G.; Blasi, F. Risk factors for community-acquired pneumonia in adults in Europe: A literature review. Thorax 2013, 68, 1057–1065. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bohte, R.; Van Furth, R.; Broek, P.J.V.D. Aetiology of community-acquired pneumonia: A prospective study among adults requiring admission to hospital. Thorax 1995, 50, 543–647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, X.; Douiri, A.; Gulliford, M. Pneumonia incidence trends in UK primary care from 2002–2017: Population based cohort study. Epidemiol. Infect. 2019, 147, e263. [Google Scholar] [CrossRef] [Green Version]
- Marik, P.E. Aspiration pneumonitis and aspiration pneumonia. N. Engl. J. Med. 2001, 344, 665–671. [Google Scholar] [CrossRef]
- Koivula, I.; Sten, M.; Makela, P.H. Risk factors for pneumonia in the elderly. Am. J. Med. 1994, 96, 313–320. [Google Scholar] [CrossRef]
- Jain, S.; Self, W.H.; Wunderink, R.G.; Fakhran, S.; Balk, R.; Bramley, A.M.; Reed, C.; Grijalva, C.G.; Anderson, E.J.; Courtney, C.M.; et al. Community-Acquired Pneumonia Requiring Hospitalization among U.S. Adults. N. Engl. J. Med. 2015, 373, 415–427. [Google Scholar] [CrossRef] [Green Version]
- Metlay, J.P.; Waterer, G.W.; Long, A.C.; Anzueto, A.; Brozek, J.; Crothers, K.; Cooley, L.A.; Dean, N.C.; Fine, M.J.; Flander, S.A.S.; et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Disease Society of America. Am. J. Respir. Crit. Care Med. 2019, 200, e45–e67. [Google Scholar] [CrossRef]
- Feldman, C.; Anderson, R. Epidemiology, virulence factors and management of pneumococcus. F1000Research 2016, 5, 2320. [Google Scholar] [CrossRef] [PubMed]
- Manabe, T.; Teramoto, S.; Tamiya, N.; Okochi, J.; Hizawa, N. Risk factors for aspiration pneumonia in older adults. PLoS ONE 2015, 10, e0140060. [Google Scholar] [CrossRef] [PubMed]
- Meldrum, O.W.; Chotirmall, S.H. Mcus, microbiome and pulmonary disease. Biomedicines 2021, 9, 675. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://statistics.blf.org.uk/pneumonia (accessed on 24 July 2021).
- Samuelson, D.R.; Welsh, D.A.; Shellito, J.E. Regulation of lung immunity and host defense by intestinal microbiota. Front. Microbiol. 2015, 6, 1085. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cramer, J.T.; Cruz-Jentoft, A.J.; Landi, F.; Hickson, M.; Zamboni, M.; Pereira, S.L.; Hustead, D.S.; Mustad, V.A. Impacts of high-protein oral nutritional supplements among malnourished men and women with sarcopenia: A multicenter randomized, double-blinded, controlled trial. J. Am. Med. Dir. Assoc. 2016, 17, 1044–1055. [Google Scholar] [CrossRef] [Green Version]
- Robinson, S.; Granic, A.; Sayer, A.A. Nurition and muscle strength, as a key component of sarcopenia: An overview of current evidence. Nutrients 2019, 11, 2942. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Welch, A. Micronutrient malnutrition across the life course, sarcopenia and frailty. Proc. Nutr. Soc. 2021, 80, 279–282. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in Older adults: Evidence for a phenotype. J. Gerontol. Med. Sci. 2001, 56A, M146–M156. [Google Scholar] [CrossRef]
- Gillick, M. Pinning down frailty. J. Gerontol. Med. Sci. 2001, 56A, M134–M135. [Google Scholar] [CrossRef] [Green Version]
- Li, H.; Manwani, B.; Leng, S.X. Frailty, inflammation, and immunity. Aging Dis. 2011, 6, 466–473. [Google Scholar]
- Ferrucci, L.; Penninx, B.W.; Volpato, S.; Harris, T.B.; Bandeen-Roche, K.; Balfour, J.; Leveille, S.G.; Fried, L.P.; Md, J.M. Change in muscle strength explains accelerated decline of physical function in older women with high interleukin-6 serum levels. J. Am. Geriatr. Soc. 2002, 50, 1947–1954. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Darer, J.; Walston, J. Frailty. In Geriatric Medicine; Springer: New York, NY, USA, 2003. [Google Scholar] [CrossRef]
- Rockwood, K.; Song, X.; MacKnight, C.; Bergman, H.; Hogan, D.B.; McDowell, I.; Mitnitski, A. A global clinical measure of fitness and frailty in elderly people. Can. Med. Assoc. J. 2005, 173, 489–495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xue, Q.-L. The frailty sundrome: Definition and natural history. Clin. Geriatr. Med. 2011, 27, 1–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fried, L.P.; Ferrucci, L.; Darer, J.; Williamson, J.D.; Anderson, G. Untangling the concepts of disability, frailty, and comorbidity: Implications for improved targeting and care. J. Gerontol. Ser. A: Biol. Sci. Med. Sci. 2004, 59, M255–M263. [Google Scholar] [CrossRef] [Green Version]
- Phu, S.; Boersma, D.; Duque, G. Exercise and sarcopenia. J. Clin. Densitom. 2015, 18, 488–492. [Google Scholar] [CrossRef] [PubMed]
- Chichero, J.A.Y. Age related changes to eating and swallowing impact frailty: Aspiration, choking risk, modified food texture and autonomy of choice. Geriatrics 2018, 3, 69. [Google Scholar] [CrossRef] [Green Version]
- Semba, R.D.; Blaum, C.S.; Bartali, B.; Xue, Q.L.; Ricks, M.O.; Guralnik, J.M.; Fried, L.P. Denture use, malnutrition, frailty, and mortality among older women living in the community. J. Nutr. Health Aging 2006, 10, M151–M167. [Google Scholar]
- Morley, J.E. Oral Frailty. J. Nutr. Health Aging 2020, 24, 683–684. [Google Scholar] [CrossRef] [PubMed]
- Nakashima, T.; Maeda, K.; Tahira, K.; Taniguchi, K.; Mori, K.; Kiyomiya, H.; Akagi, J. Silent aspiration predicts mortality in older adults with aspiration pneumonia admitted to acute hospitals. Geriatr. Gerontol. Int. 2018, 18, 828–832. [Google Scholar] [CrossRef]
- Yoneyama, T.; Yoshida, M.; Ohrui, T.; Mukaiyama, H.; Okamoto, H.; Hoshiba, K.; Ihara, S.; Yanagisawa, S.; Ariumi, S.; Morita, T.; et al. Oral care reduces pneumonia in older patients in nursing homes. J. Am. Geriatr. Soc. 2002, 50, 430–433. [Google Scholar] [CrossRef]
- Tohara, T.; Kikutani, T.; Tamura, F.; Yoshida, M.; Kuboki, T. Multicentred epidemiological study of factors associated with total bacterial count in the saliva of older people requiring nursing care. Geriatr. Gerontol. Int. 2017, 17, 219–225. [Google Scholar] [CrossRef]
- Nishizawa, T.; Niikura, Y.; Akasaka, K.; Watanabe, M.; Kurai, D.; Amano, M.; Ishii, H.; Matsushima, H.; Yamashita, N.; Takizawa, H. Pilot study for risk assessment of aspiration pneumonia on oral bacteria levels and serum biomarkers. BMC Infect. Dis. 2019, 19, 761. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gosney, M.; Punekar, S.; Playfer, J.R.; Bilsborrow, P.K.; Martin, M.V. The incidence of oral gram-negative bacteria in patients with Parkinson’s disease. Eur. J. Intern. Med. 2003, 14, 484–487. [Google Scholar] [CrossRef] [PubMed]
- Martín, A.; Ortega, O.; Roca, M.; Arús, M.; Clavé Civit, P. Effect of a minimal-massive intervention in hosptalised older patients with oropharyngeal dysphagia: A proof of concept study. J. Nutr. Health Aging 2018, 22, 729–747. [Google Scholar]
- Liu, Z.-Y.; Wei, L.; Ye, R.-C.; Chen, J.; Nie, D.; Zhang, G.; Zhang, X.-P. Reducing the incidence of stroke-associated pneumonia: An evidence-based practice. BMC Neurol. 2022, 22, 297. [Google Scholar] [CrossRef] [PubMed]
- Foltyn, P. Aging, dementia and oral health. Aust. Dent. J. 2015, 60 (Suppl. S1), 86–94. [Google Scholar] [CrossRef]
- Ferruci, L.; Fabbri, E. Inflammageing: Chronic inflammation in ageing, cardiovascular disease, and frailty. Nat. Rev. Cardiol. 2018, 15, 505–522. [Google Scholar] [CrossRef] [PubMed]
- Thannickal, V.J.; Murthy, M.; Balch, W.E.; Chandel, N.S.; Meiners, S.; Eickelberg, O.; Selman, M.; Pardo, A.; White, E.S.; Levy, B.D.; et al. Blue journal conference. Aging and susceptibility to lung disease. Am. J. Respir. Crit. Care Med. 2015, 191, 261–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El-Solh, A.A.; Sikka, P.; Ramadan, F.; Davies, J. Etiology of Severe Pneumonia in the Very Elderly. Am. J. Respir. Crit. Care Med. 2001, 163, 645–651. [Google Scholar] [CrossRef]
- Kikawada, M.; Iwamoto, T.; Takasaki, M. Aspiration and infection in the elderly: Epidemiology, diagnosis and management. Drugs Aging 2005, 22, 115–130. [Google Scholar] [CrossRef]
- Sansoni, P.; Cossarizza, A.; Brianti, V.; Fagnoni, F.; Snelli, G.; Monti, D.; Marcato, A.; Passeri, G.; Ortolani, C.; Forti, E. Lymphocyte subsets and natural killer cell activity in healthy old people and centenarians. Blood 1993, 82, 2767–2773. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meyer, K.C. The role of immunity in susceptibility to respiratory infection in the aging lung. Respir. Physiol. 2001, 128, 23–31. [Google Scholar] [CrossRef]
- Calder, P.C. Nutrition and immunity: Lessons for COVID-19. Eur. J. Clin. Nutr. 2021, 75, 1309–1318. [Google Scholar] [CrossRef] [PubMed]
- Segal, L.N.; Rom, W.N.; Weiden, M.D. Lung microbiome for clinicians. New discoveries about bugs in healthy and diseased lungs. Ann. Am. Thorac. Soc. 2014, 11, 108–116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Segal, L.N.; Clemente, J.C.; Tsay, J.C.; Koralov, S.B.; Keller, B.C.; Wu, B.G.; Li, Y.; Shen, N.; Ghedin, E.; Morris, A.; et al. Enrichment of the lung microbiome with oral taxa is associated with lung inflammation of a Th17 phenotype. Nat. Microbiol. 2016, 1, 16031. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dickson, R.P.; Erb-Downward, J.R.; Huffnagle, G.B. Homeostasis and its disruption in the lung microbiome. Am. J. Physiol. Lung Cell. Mol. Physiol. 2015, 309, L1047–L1055. [Google Scholar] [CrossRef] [Green Version]
- Dickson, R.P.; Erb-Downward, J.R.; Freeman, C.M. Bacterial topography of the healthy human lower respiratory tract. mBio 2017, 8, 14. [Google Scholar] [CrossRef]
- Fujita, Y.; Kadota, T.; Araya, J.; Ochiya, T.; Kuwano, K. Extracellular vesicles: New players in lung immunity. Am. J. Respir. Cell Mol. Biol. 2018, 58, 560–565. [Google Scholar] [CrossRef] [PubMed]
- Rubin, B.K. Physiology of airway mucus clearance. Respir. Care 2002, 47, 761–768. [Google Scholar] [PubMed]
- Nosal, C.; Ehlers, A.; Haspel, J.A. Why lungs keep time: Circadian rhythms and lung immunity. Annu. Rev. Physiol. 2020, 82, 391–412. [Google Scholar] [CrossRef] [Green Version]
- Weiskopf, D.; Weinberger, B.; Grubeck-Loebenstein, B. The Aging of the Immune System. Transpl. Int. 2009, 11, 1041–1050. [Google Scholar] [CrossRef] [PubMed]
- Komatsu, R.; Okazaki, T.; Ebihara, S.; Kobayashi, M.; Tsukita, Y.; Nihei, M.; Sugiura, H.; Niu, K.; Ebihara, T.; Ichinose, M. Aspiration pneumonia induces muscle atrophy in the respiratory, skeletal, and swallowing systems. J. Cachexia Sarcopenia Muscle 2018, 9, 643–653. [Google Scholar] [CrossRef] [PubMed]
- Woodford-Williams, E. Diagnosis and management of pneumonia in the aged. BMJ 1966, 1, 467. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bosch, X.; Formiga, F.; Cuerpo, S.; Torres, B.; Roson, B.; Lopez-Soto, A. Aspiration pneumonia in old patients with dementia. Prognostic factors of mortality. Eur. J. Intern. Med. 2012, 23, 720–726. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, C.M.; Marsland, B.J. Lung homeostasis: Influence of age, microbes, and the immune system. Immunity 2017, 46, 549. [Google Scholar] [CrossRef] [Green Version]
- Nohara, K.; Kaneko, N.; Uchida, Y.; Tanaka, N.; Sakai, T. Relationship between airway clearance function and aspiration pneumonia in geriatric nursing home residents. Dysphagia 2015, 30, 246–247. [Google Scholar]
- Petroianni, A.; Ceccarelli, D.; Conti, V.; Terzano, C. Aspiration pneumonia. Pathophysiological aspects, prevention and management. Panminerva Med. 2006, 48, 231–239. [Google Scholar]
- Marik, P.E.; Kaplan, D. Aspiration pneumonia and dysphagia in the elderly. Chest 2003, 124, 328–336. [Google Scholar] [CrossRef] [Green Version]
- Smithard, D.; Hansjee, D.; Henry, D.; Mitchell, L.; Sabaharwal, A.; Salkeld, J.; Yeung, E.; Younus, O.; Swaine, I. Inter-relationships between frailty, sarcopenia, undernutrition and dysphagia in older people who are admitted to acute frailty and medical wards: Is there an Older Adult Quartet. Geriatrics 2020, 5, 41. [Google Scholar] [CrossRef]
- Rofes, L.; Arreola, V.; Romea, M.; Palomera, E.; Almirall, J.; Cabré, M.; Serra-Prat, M.; Clavé, P. Pathophysiology of oropharyngeal dysphagia in the frail elderly. Neurogastroenterol. Motil. 2010, 22, 851-e230. [Google Scholar] [CrossRef]
- Van der Maarel-Wierink, C.D.; Vanobbergen, J.N.O.; Bronkhorst, E.M.; Schols, J.M.G.A.; de Baat, C. Meta-analysis of dysphagia and aspiration pneumonia in frail elders. J. Dent. Res. 2011, 90, 1398–1404. [Google Scholar] [CrossRef] [PubMed]
- Gleeson, K.; Maxwell, S.; Eggli, D.F. Quantitative aspiration during sleep in normal subjects. Chest 1997, 111, 1266–1272. [Google Scholar] [CrossRef] [PubMed]
- Almirall, J.; Rofes, L.; Serra-Prat, M.; Icart, R.; Palomera, E.; Arreola, V.; Clavé, P. Oropharyngeal dysphagia is a risk factor for community-acquired pneumonia in the elderly. Eur. Respir. J. 2013, 41, 923–926. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smithard, D.; Westmark, S.; Melgaard, D. Evaluation of the prevalence of screening for dysphagia among older people admitted to medical services—An international survey. Geriatrics 2019, 3, 86. [Google Scholar] [CrossRef]
- Chojin, Y.; Kato, T.; Noguchi, S.; Rikihisa, M.; Omori, M.; Mukae, H.; Yatera, K. Evaluating a novel swallowing assessment as a predictor of mortality and recurring pneumonia in elderly patients with pneumonia. Respir. Investig. 2021, 59, 783–791. [Google Scholar] [CrossRef]
- Yoshimatsu, Y.; Smithard, D.G. A Paradigm Shift in the Diagnosis of Aspiration Pneumonia in Older Adults. J. Clin. Med. 2022, 11, 5214. [Google Scholar] [CrossRef]
- Yoshimatsu, Y.; Melgaard, D.; Westergren, A.; Skrubbeltrang, C.; Smithard, D.G. The Diagnosis of Aspiration Pneumonia: A Systematic Review. Eur. Geriatr. Med. 2022; in press. [Google Scholar] [CrossRef]
- Hollaar, V.; Van Der Maarel-Wierink, C.; Van Der Putten, G.-J.; Van Der Sanden, W.; De Swart, B.; De Baat, C. Defoning chracteristics and risk indicators for diagnosing nursing home-acquired pneumonia and aspiration pneumonia in nursing home residents, using the electronically-modified Delphi Method. BMC Geriatr. 2016, 16, 60. [Google Scholar] [CrossRef] [Green Version]
- Yoon, H.-Y.; Shim, S.S.; Kim, S.J.; Lee, J.H.; Chang, J.H.; Lee, S.H.; Ryu, Y.J. Long-term mortality and prognostic factors in aspiration pneumonia. J. Am. Dir. Assoc. 2019, 20, 1098–1104. [Google Scholar] [CrossRef]
- Yamauchi, Y.; Yasunaga, H.; Matsui, H.; Hasegawa, W.; Jo, T.; Takami, K.; Fushimi, K.; Nagase, T. Comparison of clinical characteristics and outcomes between aspiration pneumonia and community acquired pneumonia in patients with chronic obstructive pulmonary disease. BMC Pulm. Med. 2015, 15, 69. [Google Scholar] [CrossRef] [Green Version]
- Akata, K.; Yatera, K.; Yamasaki, K.; Kawanami, T.; Naito, K.; Noguchi, S.; Fukuda, K.; Ishimoto, H.; Taniguchi, H.; Mukae, H. The significance of oral streptococci in patients with pneumonia with risk factors for aspiration: The bacterial floral analysis of 16S ribosomal RNA gene using bronchoalveolar lavage fluid. BMC Pulm. Med. 2016, 16, 79. [Google Scholar] [CrossRef] [Green Version]
- Lanspa, M.J.; Peyrani, P.; Wiemken, T.; Wilson, E.L.; Ramirez, J.A.; Dean, N.C. Characteristics associated with clinician diagnosis of aspiration pneumonia; a descriptive study of afflicted patients and their outcomes. J. Hosp. Med. 2015, 10, 90–96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palacios-Cena, D.; Hernandez-Barrera, V.; Lopez-de-Andres, A.; Fernandez-de-Las-Penas, C.; Palacios-Cena, M.; de Miguel-Diez, J.; Carrasco-Garrido, P.; Jimenez-Garcia, R. Time trends in incidence and outcomes of hospitalizations for aspiration pneumonia among elderly people in Spain (2003–2013). Eur. J. Intern. Med. 2017, 38, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Marik, P.E. Pulmonary aspiration syndromes. Curr. Opin. Pulm. Med. 2011, 17, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Teramoto, S.; Fukuchi, Y.; Sasaki, H.; Sato, K.; Sekizawa, K.; Matsuse, T. High incidence of aspiration pneumonia in community and hospital-acquired pneumonia in hospitalized patients: A multicenter, prospective study in Japan. J. Am. Geriatr. Soc. 2008, 56, 577–579. [Google Scholar] [CrossRef] [PubMed]
- Sarin, J.; Balasubramaniam, R.; Corcoran, A.M.; Laudenbach, J.M.; Stoopler, E.T. Reducing risk of aspiration pneumonia among elderly patients in long-term care facilities through oral health interventions. J. Am. Med. Dir. Assoc. 2008, 9, 128–135. [Google Scholar] [CrossRef]
- Lim, W.S.; Baudouin, S.V.; George, R.C.; Hill, A.T.; Jamieson, C.; Le Jeune, I.; Macfarlane, J.T.; Read, R.C.; Roberts, H.J.; Levy, M.L.; et al. Pneumonia Guidelines Committee of the BTS Standards of Care Committee. BTS guidelines for the management of community acquired pneumonia in adults: Update 2009. Thorax 2009, 64 (Suppl. S3), iii1–iii55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- BTS Care Bundles for CAP and COPD. 2014. Available online: https://www.britthoracic.org.uk/audit-and-quality-improvement/bts-care-bundlesfor-cap-and-copd/ (accessed on 8 September 2022).
- The Japanese Respiratory Society. The JRS Guidelines for the Management of Pneumonia in Adults; Medical Review Co.: Tokyo, Japan, 2017. (In Japanese) [Google Scholar]
- Ebihara, S.; Sekiya, H.; Miyagi, M.; Ebihara, T.; Okazaki, T. Dysphagia, dystussia, and aspiration pneumonia in elderly people. J. Thorac. Dis. 2016, 8, 632–639. [Google Scholar] [CrossRef] [Green Version]
- Langmore, S.; Terpenning, M.S.; Schork, A.; Chen, Y.; Murray, J.T.; Lopatin, D.E.; Loesche, W.J. Predictors of Aspiration Pneumonia:How Important Is Dysphagia? Dysphagia 1998, 13, 69–81. [Google Scholar] [CrossRef] [Green Version]
- Noguchi, S.; Yatera, K.; Kato, T.; Chojin, Y.; Fujino, Y.; Akata, K.; Kawanami, T.; Sakamoto, N.; Mukae, H. Impact of the number of aspiration risk factors on mortality and recurrence in community-onset pneumonia. Clin. Int. Aging 2017, 12, 2087–2094. [Google Scholar] [CrossRef] [Green Version]
- Pieralli, F.; Vannucchi, V.; Mancini, A.; Grazzini, M.; Paolacci, G.; Morettini, A.; Nozzoli, C. Delirium is a predictor of in-hospital mortality in elderly patients with community acquired pneumonia. Intern. Emerg. Med. 2014, 9, 195–200. [Google Scholar] [CrossRef]
- Castejón-Hernández, S.; Latorre-Vallbona, N.; Molist-Brunet, N.; Cubí-Montanyà, D.; Espaulella-Panicot, J. Association between anticholinergic burden and oropharyngeal dysphagia among hospitalized older adults. Aging Clin. Exp. Res. 2021, 33, 1981–1985. [Google Scholar] [CrossRef] [PubMed]
- Hilker, R.; Poetter, C.; Findeisen, N.; Sobesky, J.; Jacobs, A.; Neveling, M.; Heiss, W.-D. Nosocomial pneumonia after stroke. Stroke 2003, 34, 975–981. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Y.; Yang, H.; Wei, H.; Chen, Y.; Lan, M. Stroke-associated pneumonia. A bibliometric analysis of worldwide trends from 2003 to 2020. Medicine 2021, 100, e27321. [Google Scholar] [CrossRef] [PubMed]
- Eltringham, S.A.; Kilner, K.; Gee, M.; Sage, K.; Bray, B.D.; Smith, C.J.; Pownall, S. Factors associated with risk of stroke-associated pneumonia in patients with dysphagia: A systematic review. Dysphagia 2020, 35, 735–744. [Google Scholar] [CrossRef] [Green Version]
- Prass, K.; Meisel, C.; Höflich, C.; Braun, J.; Halle, E.; Wolf, T.; Ruscher, K.; Victorov, I.V.; Priller, J.; Dirnagl, U.; et al. Stroke-induced immunodeficiency promotes spontaneous bacterial infections and is mediated by sympathetic activation reversal by post stroke T Helper cell type 1-like immunostimulation. J. Exp. Med. 2003, 198, 725–736. [Google Scholar] [CrossRef] [Green Version]
- O’Neill, P.A.; Davies, I.; Fullerton, K.; Bennet, D. Stress hormone and blood glucose response following acute stroke in the elderly. Stroke 1991, 22, 842–847. [Google Scholar] [CrossRef] [Green Version]
- Palmer, L.B.; Albulak, K.; Fields, S.; Filkin, A.M.; Simon, S.; Smaldone, G.C. Oral clearance and pathogenic colonistaion in the elderly. Am. J. Resp. Crit. Care Med. 2001, 164, 464–468. [Google Scholar] [CrossRef]
- Komiya, K.; Ishii, H.; Kadota, J. Healthcare-associated pneumonia and aspiration pneumonia. Aging Dis. 2015, 6, 27–37. [Google Scholar] [CrossRef]
- Ferguson, J.; Ravert, B.; Gailey, M. Aspiration: /aspə’rāSH(ə)n/: An ambiguous term used for a diagnosis of uncertainty. Clin. Pulm. Med. 2018, 25, 177–193. [Google Scholar] [CrossRef]

| Acute Stroke (SAP) | Frailty (FAP) |
|---|---|
| Immune dysregulation | Immune dysregulation |
| Reduced airway clearance | Reduced airway clearance |
| Swallowing Impairment | Swallowing Impairment |
| Recurrent Infection | Recurrent Infection |
| Multiple comorbidities/long term conditions | Multiple comorbidities/long term conditions |
| Poor prognosis | Poor prognosis |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smithard, D.G.; Yoshimatsu, Y. Pneumonia, Aspiration Pneumonia, or Frailty-Associated Pneumonia? Geriatrics 2022, 7, 115. https://doi.org/10.3390/geriatrics7050115
Smithard DG, Yoshimatsu Y. Pneumonia, Aspiration Pneumonia, or Frailty-Associated Pneumonia? Geriatrics. 2022; 7(5):115. https://doi.org/10.3390/geriatrics7050115
Chicago/Turabian StyleSmithard, David G., and Yuki Yoshimatsu. 2022. "Pneumonia, Aspiration Pneumonia, or Frailty-Associated Pneumonia?" Geriatrics 7, no. 5: 115. https://doi.org/10.3390/geriatrics7050115
APA StyleSmithard, D. G., & Yoshimatsu, Y. (2022). Pneumonia, Aspiration Pneumonia, or Frailty-Associated Pneumonia? Geriatrics, 7(5), 115. https://doi.org/10.3390/geriatrics7050115







