Usefulness and Validity of a Jaw-Closing Force Meter in Older Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
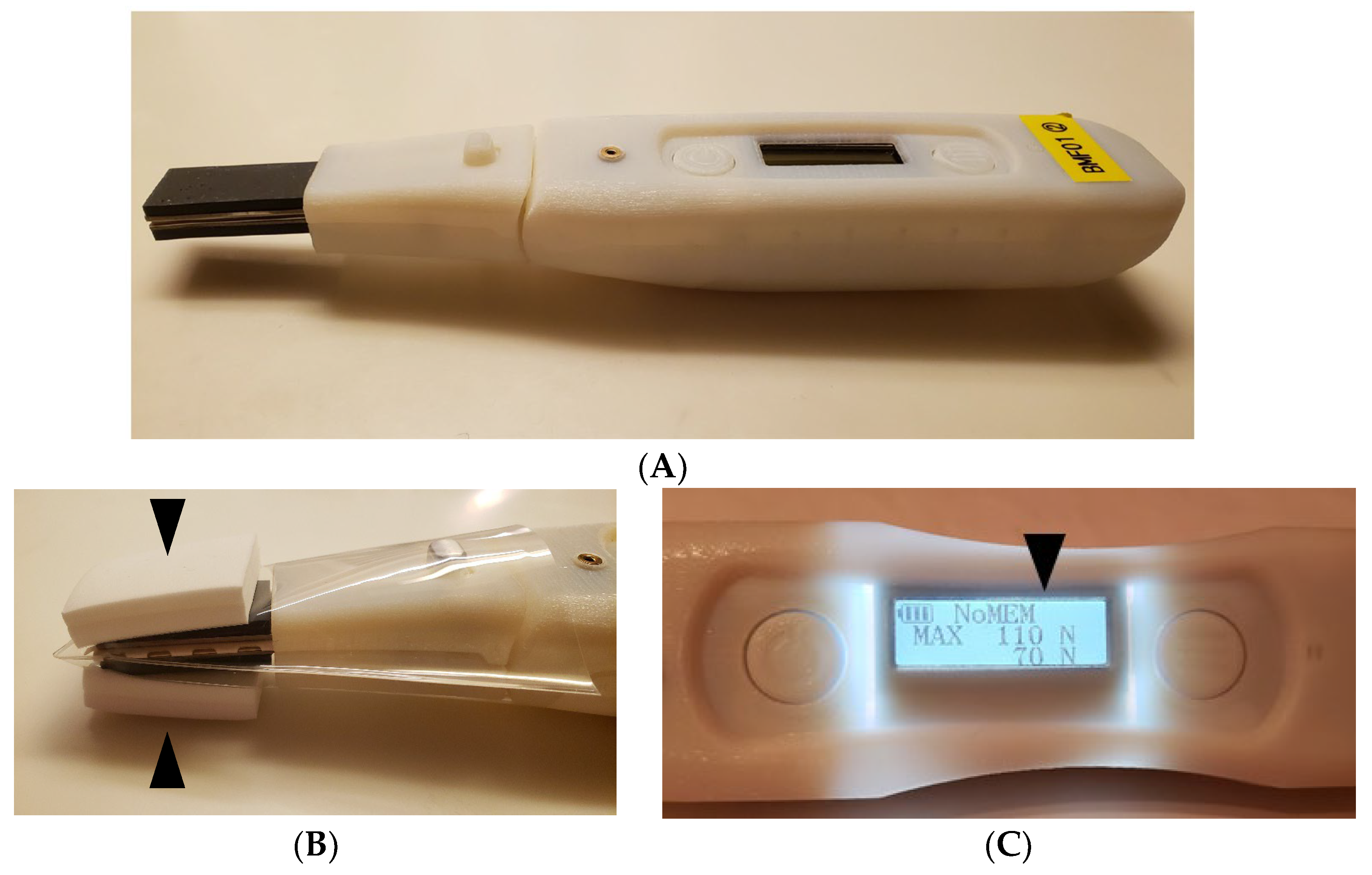
2.2. The Jaw-Closing Force Meter (JCF Meter)
2.3. Data Collection
2.3.1. Reliability of the JCF Meter
2.3.2. Examination of Factors Correlated and Related to Jaw-Closing Force
2.4. Data Analysis
3. Results
3.1. Reliability and Validity of the JCF Meter
3.2. Correlation of Each Item with the Ability to Close One’s Jaw
3.3. Examination of Factors Associated with Jaw-Closing Force
4. Discussion
4.1. Reliability of the Prototyped JCF Meter
4.2. Characteristics of Prototyped JCF Meter and Comparison with Existing Occlusion Meters
4.3. Factors Associated with Jaw-Closing Force
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Minakuchi, S.; Tsuga, K.; Ikebe, K.; Ueda, T.; Tamura, F.; Nagao, K.; Furuya, J.; Matsuo, K.; Yamamoto, K.; Kanazawa, M.; et al. Oral hypofunction in the older population: Position paper of the Japanese Society of Gerodontology in 2016. Gerodontology 2018, 35, 317–324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iinuma, T.; Arai, Y.; Fukumoto, M.; Takayama, M.; Abe, Y.; Asakura, K.; Nishiwaki, Y.; Takebayashi, T.; Iwase, T.; Komiyama, K.; et al. Maximum occlusal force and physical performance in the oldest old: The Tokyo oldest old survey on total health. J. Am. Geriatr. Soc. 2012, 60, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Hatta, K.; Gondo, Y.; Kamide, K.; Masui, Y.; Inagaki, H.; Nakagawa, T.; Matsuda, K.I.; Inomata, C.; Takeshita, H.; Mihara, Y.; et al. Occlusal force predicted cognitive decline among 70- and 80-year-old Japanese: A 3-year prospective cohort study. J. Prosthodont. Res. 2020, 64, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Ikebe, K.; Matsuda, K.; Morii, K.; Nokubi, T.; Ettinger, R.L. The relationship between oral function and body mass index among independently living older Japanese people. Int. J. Prosthodont. 2006, 19, 539–546. [Google Scholar] [PubMed]
- Ikebe, K.; Nokubi, T.; Morii, K.; Kashiwagi, J.; Furuya, M. Association of bite force with ageing and occlusal support in older adults. J. Dent. 2005, 33, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Haraldson, T.; Karlsson, U.; Carlsson, G.E. Bite force and oral function in complete denture wearers. J. Oral Rehabil. 1979, 6, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Okada, T.; Ikebe, K.; Inomata, C.; Takeshita, H.; Uota, M.; Mihara, Y.; Matsuda, K.; Kitamura, M.; Murakami, S.; Gondo, Y.; et al. Association of periodontal status with occlusal force and food acceptability in 70-year-old adults: From SONIC Study. J. Oral Rehabil. 2014, 41, 912–919. [Google Scholar] [CrossRef] [PubMed]
- Minakuchi, S.; Takaoka, S.; Ito, J.; Shimoyama, K.; Uematsu, H. Factors affecting denture use in some institutionalized elderly people. Spec. Care Dentist. 2006, 26, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Inomata, C.; Ikebe, K.; Okubo, H.; Takeshita, H.; Mihara, Y.; Hatta, K.; Tada, S.; Enoki, K.; Ogawa, T.; Matsuda, K.; et al. Dietary intake is associated with occlusal force rather than number of teeth in 80-y-old Japanese. JDR Clin. Transl. Res. 2017, 2, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Kumagai, H.; Watanabe, T.; Uchida, T.; Nagao, M. Evaluation of complete denture occlusal contacts using pressure-sensitive sheets. Int. J. Prosthodont. 1997, 10, 386–391. [Google Scholar] [PubMed]
- Sakaguchi, M.; Ono, N.; Turuta, H.; Yoshiike, J.; Ohhashi, T. Development of new handy type occlusal force gauge. Jpn. J. Med. Electron. Biol. Eng. 1996, 34, 53–55. [Google Scholar]
- Kikutani, T.; Tamura, F.; Nishiwaki, K.; Kodama, M.; Suda, M.; Fukui, T.; Takahashi, N.; Yoshida, M.; Akagawa, Y.; Kimura, M. Oral motor function and masticatory performance in the community-dwelling elderly. Odontology 2009, 97, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Eichner, K. Über eine gruppeneintelung des lückengebisses für die prothetik. Dtsch. Zahnärztl. Z. 1955, 10, 1831–1834. (In German) [Google Scholar]
- Yoshimi, K.; Nakagawa, K.; Hara, K.; Yamaguchi, K.; Nakane, A.; Kubota, K.; Furuya, J.; Tohara, H. Relationship between tongue pressure and back muscle strength in healthy elderly individuals. Aging Clin. Exp. Res. 2020, 32, 2549–2555. [Google Scholar] [CrossRef] [PubMed]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamaguchi, K.; Tohara, H.; Hara, K.; Nakane, A.; Yoshimi, K.; Nakagawa, K.; Minakuchi, S. Factors associated with masseter muscle quality assessed from ultrasonography in community-dwelling elderly individuals: A cross-sectional study. Arch. Gerontol. Geriatr. 2019, 82, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, K.; Tohara, H.; Hara, K.; Nakane, A.; Kajisa, E.; Yoshimi, K.; Minakuchi, S. Relationship of aging, skeletal muscle mass, and tooth loss with masseter muscle thickness. BMC Geriatr. 2018, 18, 67. [Google Scholar] [CrossRef] [PubMed]
- Ohi, T.; Komiyama, T.; Miyoshi, Y.; Murakami, T.; Tsuboi, A.; Tomata, Y.; Tsuji, I.; Watanabe, M.; Hattori, Y. Maximum occlusal force and incident functional disability in older adults: The Tsurugaya project. JDR Clin. Transl. Res. 2018, 3, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Kato, K.; Matsuda, N.; Takahata, M.; Koseki, C.; Yamaki, M.; Sato, T. Relationship between occlusal force and endothelial function in community-dwelling elderly women: A pilot study. Clin. Exp. Dent. Res. 2022, 8, 1207–1212. [Google Scholar] [CrossRef] [PubMed]
| Intraclass Correlation Coefficient | 95% Confidence Interval | p-Value | ||
|---|---|---|---|---|
| Intra-rater reliability | Right | 0.811 | [0.406, 0.942] | 0.003 |
| Left | 0.691 | [0.027, 0.905] | 0.023 | |
| Inter-rater reliability | Right | 0.706 | [0.105, 0.905] | 0.007 |
| Left | 0.789 | [0.309, 0.932] | 0.006 |
| Characteristics | ||
|---|---|---|
| Age (years), median (IQR) | 73.5 (70.3, 80.0) | |
| Sex, N (%) | Male | 38 (61.3) |
| Female | 24 (38.7) | |
| Eichner classification, N (%) | A | 59 (95.2) |
| B | 2 (3.2) | |
| C | 1 (1.6) | |
| BMI (kg/m2), mean ± SD | 22.5 ± 2.7 | |
| OF: R (N), median (IQR) | 352.6 (209.6, 458.5) | |
| OF: L (N), median (IQR) | 300.1 (196.5, 451.1) | |
| JCF: R (N), median (IQR) | 326.7 (210.0, 466.7) | |
| JCF: L (N), median (IQR) | 280.0 (158.3, 422.5) | |
| Age | BMI | OF (R) | OF (L) | JCF (R) | JCF (L) | |
|---|---|---|---|---|---|---|
| Age | 1 | |||||
| BMI | 0.119 | 1 | ||||
| OF (R) | −0.312 * | −0.042 | 1 | |||
| OF (L) | −0.165 | −0.045 | 0.684 ** | 1 | ||
| JCF (R) | −0.413 ** | −0.103 | 0.433 ** | 0.299 * | 1 | |
| JCF (L) | −0.190 | −0.113 | 0.303 * | 0.298 * | 0.712 ** | 1 |
| Standardizing Coefficient (β) | p-Value | VIF | |
|---|---|---|---|
| Age | −0.24 | 0.038* | 1.23 |
| Sex | −0.19 | 0.070 | 1.05 |
| BMI | −0.10 | 0.344 | 1.02 |
| OF | 0.22 | 0.043 * | 1.11 |
| Presence of denture | −0.43 | <0.001 ** | 1.25 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kawashima, M.; Yoshimi, K.; Nakagawa, K.; Yamaguchi, K.; Ishii, M.; Hasegawa, S.; Moritoyo, R.; Nakane, A.; Tohara, H. Usefulness and Validity of a Jaw-Closing Force Meter in Older Adults. Geriatrics 2022, 7, 145. https://doi.org/10.3390/geriatrics7060145
Kawashima M, Yoshimi K, Nakagawa K, Yamaguchi K, Ishii M, Hasegawa S, Moritoyo R, Nakane A, Tohara H. Usefulness and Validity of a Jaw-Closing Force Meter in Older Adults. Geriatrics. 2022; 7(6):145. https://doi.org/10.3390/geriatrics7060145
Chicago/Turabian StyleKawashima, Mina, Kanako Yoshimi, Kazuharu Nakagawa, Kohei Yamaguchi, Miki Ishii, Shohei Hasegawa, Rieko Moritoyo, Ayako Nakane, and Haruka Tohara. 2022. "Usefulness and Validity of a Jaw-Closing Force Meter in Older Adults" Geriatrics 7, no. 6: 145. https://doi.org/10.3390/geriatrics7060145





