Impact of COVID-19 Pandemic on Fragility Fractures of the Hip: An Interrupted Time-Series Analysis of the Lockdown Periods in Western Greece and Review of the Literature
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Demographics and Fracture Incidence
3.2. Time to Surgery
3.3. Time to Discharge after Surgery and Total Stay
3.4. Comparing Secondary to Tertiary Healthcare
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bogoch, I.I.; Watts, A.; Thomas-Bachli, A.; Huber, C.; Kraemer, M.U.G.; Khan, K. Pneumonia of Unknown Aetiology in Wuhan, China: Potential for International Spread via Commercial Air Travel. J. Travel Med. 2020, 27, taaa008. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical Features of Patients Infected with 2019 Novel Coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus–Infected Pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef]
- Hernigou, J.; Morel, X.; Callewier, A.; Bath, O.; Hernigou, P. Staying Home during “COVID-19” Decreased Fractures, but Trauma Did Not Quarantine in One Hundred and Twelve Adults and Twenty Eight Children and the “Tsunami of Recommendations” Could Not Lockdown Twelve Elective Operations. Int. Orthop. 2020, 44, 1473–1480. [Google Scholar] [CrossRef]
- Mallah, S.I.; Ghorab, O.K.; Al-Salmi, S.; Abdellatif, O.S.; Tharmaratnam, T.; Iskandar, M.A.; Sefen, J.A.N.; Sidhu, P.; Atallah, B.; El-Lababidi, R.; et al. COVID-19: Breaking down a Global Health Crisis. Ann. Clin. Microbiol. Antimicrob. 2021, 20, 1–30. [Google Scholar] [CrossRef]
- Mungroo, M.R.; Khan, N.A.; Siddiqui, R. Novel Coronavirus: Current Understanding of Clinical Features, Diagnosis, Pathogenesis, and Treatment Options. Pathogens 2020, 9, 297. [Google Scholar] [CrossRef] [Green Version]
- Sharma, A.; Ahmad Farouk, I.; Lal, S.K. COVID-19: A Review on the Novel Coronavirus Disease Evolution, Transmission, Detection, Control and Prevention. Viruses 2021, 13, 202. [Google Scholar] [CrossRef]
- COVID-19 Strategy Update—14 April 2020. Available online: https://www.who.int/publications/i/item/covid-19-strategy-update---14-april-2020 (accessed on 5 April 2023).
- WHO Coronavirus (COVID-19) Dashboard|WHO Coronavirus (COVID-19) Dashboard with Vaccination Data. Available online: https://covid19.who.int/?adgroupsurvey=%7Badgroupsurvey%7D&gclid=Cj0KCQjwt_qgBhDFARIsABcDjOetI-5Y7KuFgCqBsW_YuytVcgvaTEUYV9c8ac0K98X1ogkU-ifkXAgaAneoEALw_wcB (accessed on 25 March 2023).
- Haut, E.R.; Leeds, I.L.; Livingston, D.H. The Effect on Trauma Care Secondary to the COVID-19 Pandemic: Collateral Damage From Diversion of Resources. Ann. Surg. 2020, 272, e204. [Google Scholar] [CrossRef]
- de Simone, B.; Chouillard, E.; Di Saverio, S.; Pagani, L.; Sartelli, M.; Biffl, W.L.; Coccolini, F.; Pieri, A.; Khan, M.; Borzellino, G.; et al. Emergency Surgery during the COVID-19 Pandemic: What You Need to Know for Practice. Ann. R. Coll. Surg. Engl. 2020, 102, 323. [Google Scholar] [CrossRef]
- Orfanos, G.; Al Kaisi, K.; Jaiswal, A.; Lim, J.; Youssef, B. The Effect of COVID-19 Pandemic on the Care of Fragility Hip Fracture Patients in the United Kingdom. A Case Control Study in a Major Trauma Centre. Surgeon 2021, 19, e440–e445. [Google Scholar] [CrossRef]
- Baker, T.; Schell, C.O.; Petersen, D.B.; Sawe, H.; Khalid, K.; Mndolo, S.; Rylance, J.; McAuley, D.F.; Roy, N.; Marshall, J.; et al. Essential Care of Critical Illness Must Not Be Forgotten in the COVID-19 Pandemic. Lancet 2020, 395, 1253. [Google Scholar] [CrossRef]
- Zhu, Y.; Chen, W.; Xin, X.; Yin, Y.; Hu, J.; Lv, H.; Li, W.; Deng, X.; Zhu, C.; Zhu, J.; et al. Epidemiologic Characteristics of Traumatic Fractures in Elderly Patients during the Outbreak of Coronavirus Disease 2019 in China. Int. Orthop. 2020, 44, 1565–1570. [Google Scholar] [CrossRef]
- Druel, T.; Andeol, Q.; Rongieras, F.; Bertani, A.; Bordes, M.; Alvernhe, A. Evaluation of Containment Measures’ Effect on Orthopaedic Trauma Surgery during the COVID-19 Pandemic: A Retrospective Comparison between 2019 and 2020. Int. Orthop. 2020, 44, 2229–2234. [Google Scholar] [CrossRef]
- Donovan, R.L.; Tilston, T.; Frostick, R.; Chesser, T. Outcomes of Orthopaedic Trauma Services at a UK Major Trauma Centre During a National Lockdown and Pandemic: The Need for Continuing the Provision of Services. Cureus 2020, 12, e11056. [Google Scholar] [CrossRef]
- Brown, J.D.; Vouri, S.M.; Manini, T.M. Survey-Reported Medication Changes among Older Adults during the SARS-CoV-2 (COVID-19) Pandemic. Res. Soc. Adm. Pharm. 2021, 17, 1478–1482. [Google Scholar] [CrossRef]
- Lim, S.M.; Tan, M.; Sze, Y.L.; Au, L. Letter to the Editor: Effects of the COVID-19 Pandemic on COVID-19 Negative Geriatric Patients with Hip Fractures. J. Frailty Aging 2021, 10, 75–76. [Google Scholar] [CrossRef]
- Ojeda-Thies, C.; Cuarental-García, J.; Ramos-Pascua, L.R. Decreased Volume of Hip Fractures Observed during COVID-19 Lockdown. Eur. Geriatr. Med. 2021, 12, 759–766. [Google Scholar] [CrossRef]
- Ettinger, B.; Black, D.M.; Dawson-Hughes, B.; Pressman, A.R.; Melton, L.J. Updated Fracture Incidence Rates for the US Version of FRAX®. Osteoporos. Int. 2010, 21, 25. [Google Scholar] [CrossRef] [Green Version]
- Ioannidis, G.; Papaioannou, A.; Hopman, W.M.; Akhtar-Danesh, N.; Anastassiades, T.; Pickard, L.; Kennedy, C.C.; Prior, J.C.; Olszynski, W.P.; Davison, K.S.; et al. Relation between Fractures and Mortality: Results from the Canadian Multicentre Osteoporosis Study. CMAJ 2009, 181, 265–271. [Google Scholar] [CrossRef] [Green Version]
- Bukata, S.V.; Digiovanni, B.F.; Friedman, S.M.; Hoyen, H.; Kates, A.; Kates, S.L.; Mears, S.C.; Mendelson, D.A.; Serna, F.H., Jr.; Sieber, F.E.; et al. A Guide to Improving the Care of Patients with Fragility Fractures. Geriatr. Orthop. Surg. Rehabil. 2011, 2, 5–37. [Google Scholar] [CrossRef]
- Hernlund, E.; Svedbom, A.; Ivergård, M.; Compston, J.; Cooper, C.; Stenmark, J.; McCloskey, E.V.; Jönsson, B.; Kanis, J.A. Osteoporosis in the European Union: Medical Management, Epidemiology and Economic Burden. A Report Prepared in Collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch. Osteoporos. 2013, 8, 1–115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leal, J.; Gray, A.M.; Prieto-Alhambra, D.; Arden, N.K.; Cooper, C.; Javaid, M.K.; Judge, A. Impact of Hip Fracture on Hospital Care Costs: A Population-Based Study. Osteoporos. Int. 2016, 27, 549–558. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Full Guideline|NOGG. Available online: https://www.nogg.org.uk/full-guideline (accessed on 23 April 2023).
- Delinasios, G.J.; Fragkou, P.C.; Gkirmpa, A.M.; Tsangaris, G.; Hoffman, R.M.; Anagnostopoulos, A.K. The Experience of Greece as a Model to Contain COVID-19 Infection Spread. Vivo 2021, 35, 1285–1294. [Google Scholar] [CrossRef] [PubMed]
- Kenanidis, E.; Anagnostis, P.; Arvaniti, K.; Potoupnis, M.E.; Tsiridis, E. Organizing an Orthopaedic Department During COVID-19 Pandemic to Mitigate In-Hospital Transmission: Experience From Greece. Cureus 2020, 12, e8676. [Google Scholar] [CrossRef] [PubMed]
- Population of Greece—ELSTAT. Available online: https://www.statistics.gr/2021-census-res-pop-results (accessed on 30 April 2023).
- Weekly report|CoVid19.Gov.Gr. Available online: https://covid19.gov.gr/covid19-live-analytics/ (accessed on 25 March 2023).
- Coronavirus Disease (COVID-19)—NPHO. Available online: https://eody.gov.gr/en/covid-19/ (accessed on 30 April 2023).
- Maniscalco, P.; Poggiali, E.; Quattrini, F.; Ciatti, C.; Magnacavallo, A.; Vercelli, A.; Domenichini, M.; Vaienti, E.; Pogliacomi, F.; Ceccarelli, F. Proximal Femur Fractures in COVID-19 Emergency: The Experience of Two Orthopedics and Traumatology Departments in the First Eight Weeks of the Italian Epidemic. Acta Bio. Med. Atenei Parm. 2020, 91, 89. [Google Scholar] [CrossRef]
- Egol, K.A.; Konda, S.R.; Bird, M.L.; Dedhia, N.; Landes, E.K.; Ranson, R.A.; Solasz, S.J.; Aggarwal, V.K.; Bosco, J.A.; Furgiuele, D.L.; et al. Increased Mortality and Major Complications in Hip Fracture Care During the COVID-19 Pandemic: A New York City Perspective. J. Orthop. Trauma 2020, 34, 395–402. [Google Scholar] [CrossRef]
- Malik-Tabassum, K.; Crooks, M.; Robertson, A.; To, C.; Maling, L.; Selmon, G. Management of Hip Fractures during the COVID-19 Pandemic at a High-Volume Hip Fracture Unit in the United Kingdom. J. Orthop. 2020, 20, 332. [Google Scholar] [CrossRef]
- Narang, A.; Chan, G.; Aframian, A.; Ali, Z.; Carr, A.; Goodier, H.; Morgan, C.; Park, C.; Sugand, K.; Walton, T.; et al. Thirty-Day Mortality Following Surgical Management of Hip Fractures during the COVID-19 Pandemic: Findings from a Prospective Multi-Centre UK Study. Int. Orthop. 2021, 45, 23. [Google Scholar] [CrossRef]
- Arafa, M.; Nesar, S.; Abu-Jabeh, H.; Jayme, M.O.R.; Kalairajah, Y. COVID-19 Pandemic and Hip Fractures: Impact and Lessons Learned. Bone Jt. Open 2020, 1, 530–540. [Google Scholar] [CrossRef]
- Hall, A.J.; Clement, N.D.; Farrow, L.; MacLullich, A.M.J.; Dall, G.F.; Scott, C.E.H.; Jenkins, P.J.; White, T.O.; Duckworth, A.D. IMPACT-Scot Report on COVID-19 and Hip Fractures. Bone Joint J. 2020, 102-B, 1219–1228. [Google Scholar] [CrossRef]
- Ogliari, G.; Lunt, E.; Ong, T.; Marshall, L.; Sahota, O. The Impact of Lockdown during the COVID-19 Pandemic on Osteoporotic Fragility Fractures: An Observational Study. Arch. Osteoporos. 2020, 15, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Haskel, J.D.; Lin, C.C.; Kaplan, D.J.; Dankert, J.F.; Merkow, D.; Crespo, A.; Behery, O.; Ganta, A.; Konda, S.R. Hip Fracture Volume Does Not Change at a New York City Level 1 Trauma Center During a Period of Social Distancing. Geriatr. Orthop. Surg. Rehabil. 2020, 11, 2151459320972674. [Google Scholar] [CrossRef] [PubMed]
- Wignall, A.; Giannoudis, V.; De, C.; Jimenez, A.; Sturdee, S.; Nisar, S.; Pandit, H.; Gulati, A.; Palan, J. The Impact of COVID-19 on the Management and Outcomes of Patients with Proximal Femoral Fractures: A Multi-Centre Study of 580 Patients. J. Orthop. Surg. Res. 2021, 16, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Crozier-Shaw, G.; Hughes, A.J.; Conlon, B.; Sheehan, E.; Merghani, K. Hip Fracture Care during COVID-19: A Regional Trauma Centre’s Experience. Ir. J. Med. Sci. 2021, 190, 1275. [Google Scholar] [CrossRef] [PubMed]
- da Silva, A.C.; da Silva Santos, G.; Maluf, E.M.C.P.; Borba, V.Z.C. Incidence of Hip Fractures during the COVID-19 Pandemic in the Brazilian Public Health Care System. Arch. Osteoporos. 2022, 17, 42. [Google Scholar] [CrossRef]
- Troiano, E.; Sensi, A.G.D.; Zanasi, F.; Facchini, A.; De Marco, G.; Colasanti, G.B.; Mondanelli, N.; Giannotti, S. Impact of COVID-19 Pandemic on Treatment and Outcome of Fragility Hip In Non-COVID Patients: Comparison Between the Lockdown Period, aHistorical Series and the “Pandemic Normality” in a Single. Geriatr. Orthop. Surg. Rehabil. 2023, 14, 215145932311524. [Google Scholar] [CrossRef]
- Johansen, A.; Inman, D.S. A View of COVID-19 from the Perspective of the National Hip Fracture Database. Bone Jt. J. 2021, 103 B, 1007–1008. [Google Scholar] [CrossRef]
- Kelsey, J.L.; Berry, S.D.; Procter-Gray, E.; Quach, L.; Nguyen, U.S.D.T.; Li, W.; Kiel, D.P.; Lipsitz, L.A.; Hannan, M.T. Indoor and Outdoor Falls in Older Adults Are Different: The MOBILIZE Boston Study. J. Am. Geriatr. Soc. 2010, 58, 2135. [Google Scholar] [CrossRef]
- Bliuc, D.; Nguyen, N.D.; Milch, V.E.; Nguyen, T.V.; Eisman, J.A.; Center, J.R. Mortality Risk Associated with Low-Trauma Osteoporotic Fracture and Subsequent Fracture in Men and Women. JAMA 2009, 301, 513–521. [Google Scholar] [CrossRef] [Green Version]
- Klestil, T.; Röder, C.; Stotter, C.; Winkler, B.; Nehrer, S.; Lutz, M.; Klerings, I.; Wagner, G.; Gartlehner, G.; Nussbaumer-Streit, B. Impact of Timing of Surgery in Elderly Hip Fracture Patients: A Systematic Review and Meta-Analysis. Sci. Rep. 2018, 8, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Ojeda-Thies, C.; Cuarental-García, J.; García-Gómez, E.; Salazar-Zamorano, C.H.; Alberti-Maroño, J.; Ramos-Pascua, L.R. Hip Fracture Care and Mortality among Patients Treated in Dedicated COVID-19 and Non-COVID-19 Circuits. Eur. Geriatr. Med. 2021, 12, 749. [Google Scholar] [CrossRef]
- Dupley, L.; Oputa, T.J.; Bourne, J.T.; Lum, J.; Hodhody, G.; Rogers, S.; Mcloughlin, K.; Murphy, L.; Konarski, A.; Almari, F.; et al. 30-Day Mortality for Fractured Neck of Femur Patients with Concurrent COVID-19 Infection. Eur. J. Orthop. Surg. Traumatol. 2021, 31, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Muñoz Vives, J.M.; Jornet-Gibert, M.; Cámara-Cabrera, J.; Esteban, P.L.; Brunet, L.; Delgado-Flores, L.; Camacho-Carrasco, P.; Torner, P.; Marcano-Fernández, F. Mortality Rates of Patients with Proximal Femoral Fracture in a Worldwide Pandemic: Preliminary Results of the Spanish HIP-COVID Observational Study. J. Bone Jt. Surg. Am. 2020, 102, E69. [Google Scholar] [CrossRef] [PubMed]
- Obamiro, E.; Trivedi, R.; Ahmed, N. Changes in Trends of Orthopedic Services Due to the COVID-19 Pandemic: A Review. World J. Orthop. 2022, 13, 955. [Google Scholar] [CrossRef]
- Catellani, F.; Coscione, A.; D’Ambrosi, R.; Usai, L.; Roscitano, C.; Fiorentino, G. Treatment of Proximal Femoral Fragility Fractures in Patients with COVID-19 During the SARS-CoV-2 Outbreak in Northern Italy. J. Bone Jt. Surg. Am. 2020, 102, e58. [Google Scholar] [CrossRef] [PubMed]
- IMAJ|The Israel Medicine Association Journal|Volume 23, Number 8, August 2021|The Impact of the COVID-19 2020 Pandemic on Hospital Length of Stay Following Fragility Hip Fracture Surgery. Available online: https://www.ima.org.il/MedicineIMAJ/viewarticle.aspx?year=2021&month=08&page=469 (accessed on 25 March 2023).
- Moyet, J.; Deschasse, G.; Marquant, B.; Mertl, P.; Bloch, F. Which Is the Optimal Orthogeriatric Care Model to Prevent Mortality of Elderly Subjects Post Hip Fractures? A Systematic Review and Meta-Analysis Based on Current Clinical Practice. Int. Orthop. 2019, 43, 1449–1454. [Google Scholar] [CrossRef]
- Patel, J.N.; Klein, D.S.; Sreekumar, S.; Liporace, F.A.; Yoon, R.S. Outcomes in Multidisciplinary Team-Based Approach in Geriatric Hip Fracture Care: A Systematic Review. J. Am. Acad. Orthop. Surg. 2020, 28, 128–133. [Google Scholar] [CrossRef]
- Kenanidis, E.; Tsiridis, E. “Flattening the Curve” of COVID-19 Pandemic in Orthopaedics and Trauma: The Greek Perspective. Injury 2020, 51, 1681–1682. [Google Scholar] [CrossRef]
- Koutserimpas, C.; Raptis, K.; Tsakalou, D.; Papadaki, C.; Magarakis, G.; Kourelis, K.; Samonis, G.; Alpantaki, K. The Effect of Quarantine Due to COVID-19 Pandemic in Surgically Treated Fractures in Greece: A Two-Center Study. Mædica 2020, 15, 332. [Google Scholar] [CrossRef]
- Ormeño, J.C.; Martínez, R.; Frías, C.; Von Plessing, C.; Quevedo, I. Impact of the COVID-19 Pandemic on Osteoporotic Hip Fractures in Chile. Arch. Osteoporos. 2022, 17, 130. [Google Scholar] [CrossRef]




| Grouped 2017–2019 | 2020 | Difference | p | ||
|---|---|---|---|---|---|
| GHP | |||||
| Cases, n | 14.3 | 8 | −44% | ||
| Age (y), mean | 83.9 | 80.3 | −3.6 | 0.127 | |
| median | 84 | 81.5 | |||
| SD | 7.8 | 6.9 | |||
| Time to Surgery (d), mean | 2.8 | 1.8 | −36% | 0.200 | |
| median | 2 | 1 | |||
| SD | 2.4 | 1.1 | |||
| Time to Discharge (d), mean | 5.0 | 6.3 | +25% | 0.359 | |
| median | 4 | 4.5 | |||
| SD | 3.5 | 6 | |||
| Total Hospital Stay (d), mean | 7.8 | 8 | +3% | 0.345 | |
| median | 7 | 6 | |||
| SD | 4.2 | 5.8 | |||
| GHA | |||||
| Cases, n | 9.0 | 6 | −33% | ||
| Age (y), mean | 87.1 | 85.5 | −1.6 | 0.303 | |
| median | 88 | 84 | |||
| SD | 7.7 | 8.8 | |||
| Time to Surgery (d), mean | 4.0 | 3.8 | −5% | 0.697 | |
| median | 4 | 4 | |||
| SD | 2.2 | 1.3 | |||
| Time to Discharge (d), mean | 10.0 | 5.8 | −42% | 0.034 | |
| median | 7 | 6 | [g = 0.7] | ||
| SD | 6.8 | 2.0 | |||
| Total Hospital Stay (d), mean | 13.7 | 9.7 | −29% | 0.119 | |
| median | 11 | 10.5 | |||
| SD | 7.9 | 2.8 |
| Grouped 2017–2019 | 2020 | Difference | p | ||
|---|---|---|---|---|---|
| GHP | |||||
| Cases, n | 18.3 | 15 | −18% | ||
| Age (y), mean | 82.5 | 86.1 | +3.6 | 0.061 | |
| median | 84 | 88 | |||
| SD | 6.6 | 7.8 | |||
| Time to Surgery (d), mean | 3.1 | 2.1 | -32% | 0.147 | |
| median | 2 | 2 | |||
| SD | 2.4 | 1.5 | |||
| Time to Discharge (d), mean | 6.0 | 4.4 | −27% | 0.268 | |
| median | 4 | 4 | |||
| SD | 6.3 | 1.1 | |||
| Total Hospital Stay (d), mean | 9.1 | 6.5 | −29% | 0.271 | |
| median | 7 | 6 | |||
| SD | 7.5 | 1.5 | |||
| GHA | |||||
| Cases, n | 10.0 | 6 | −40% | ||
| Age (y), mean | 85.4 | 83.8 | −1.6 | 0.305 | |
| median | 86 | 84.5 | |||
| SD | 7.1 | 7.3 | |||
| Time to Surgery (d), mean | 3.2 | 2.5 | −22% | 0.433 | |
| median | 2 | 2.5 | |||
| SD | 2.2 | 1 | |||
| Time to Discharge (d), mean | 8.7 | 13.7 | +57% | 0.072 | |
| median | 7.5 | 14.5 | |||
| SD | 4.5 | 6.7 | |||
| Total Hospital Stay (d), mean | 11.8 | 16.2 | +37% | 0.109 | |
| median | 10 | 18 | |||
| SD | 5.2 | 6.9 |
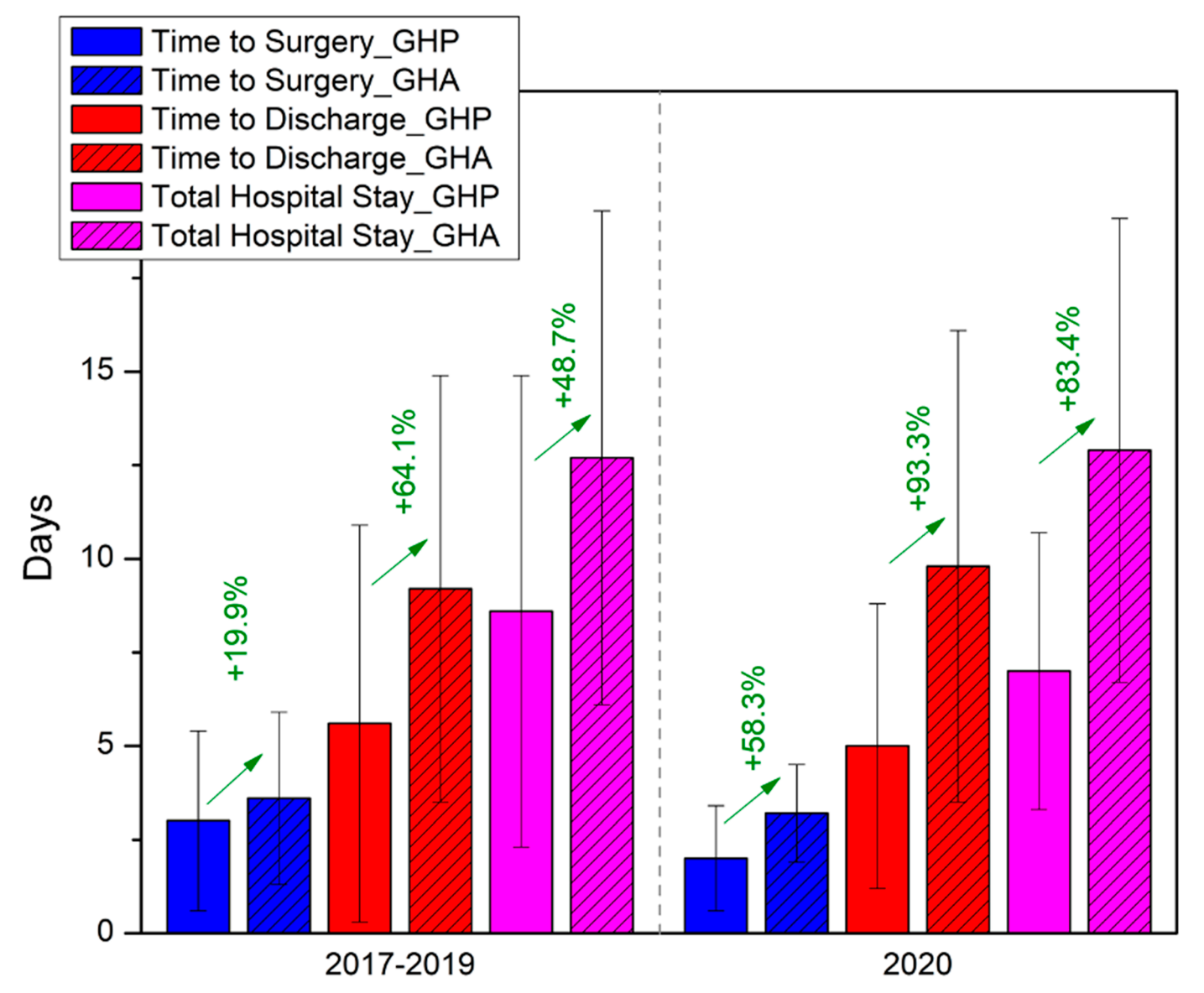
| 9 | Non-COVID/Lockdown Period (2017–2019) | COVID/Lockdown Period (2020) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| GHP | GHA | Difference | p | GHP | GHA | Difference | p | ||
| Cases, n | 98 | 57 | 23 | 12 | |||||
| Age (y), mean | 83.1 | 86.2 | +3.1 y | 0.123 | 84.0 | 84.7 | +0.7 y | 0.976 | |
| median | 84 | 87 | 87 | 84 | |||||
| SD | 7.2 | 7.4 | 8.0 | 8.1 | |||||
| Time to Surgery (d), mean | 3.0 | 3.6 | +19.9% | 0.031 | 2.0 | 3.2 | +58.3% | 0.032 | |
| median | 2 | 3 | [g = 0.4] | 2 | 3.5 | [g = 0.8] | |||
| SD | 2.4 | 2.3 | 1.4 | 1.3 | |||||
| Time to Discharge (d), mean | 5.6 | 9.2 | +64.1% | <0.001 | 5.0 | 9.8 | +93.3% | 0.007 | |
| median | 4 | 7 | [g = 1.1] | 4 | 7 | [g = 1.0] | |||
| SD | 5.3 | 5.7 | 3.8 | 6.3 | |||||
| Total Hospital Stay (d), mean | 8.6 | 12.7 | +48.7% | <0.001 | 7.0 | 12.9 | +83.4% | 0.004 | |
| median | 7 | 11 | [g = 1.0] | 6 | 11.5 | [g = 1.1] | |||
| SD | 6.3 | 6.6 | 3.7 | 6.2 | |||||
| Study | Country | Type of Study | Period of Study | Scope | Incidence of Hip Fractures | Comments |
|---|---|---|---|---|---|---|
| Maniscalo et al., 2020, [31] | Italy | Retrospective | 22/02/20–18/04/20 (rp: 23/02/19–20/04/19) | Local | ↓ | Relative ↓ |
| Egol et al., 2020, [32] | United States of America | Prospective | 01/02/20–15/04/20 (rp: same in 2019) | Regional | ↑ | 138 hip fxs in 2020, 115 in 2019 |
| Malik-Tabassum, et al., 2020, [33] | United Kingdom | Retrospective | 23/03/20–11/05/20 (rp: same in 2018, 2019) | Local | ↓ | General ↓ in trauma workflow, marked ↓in younger adults requiring surgery |
| Narang et al., 2020, [34] | United Kingdom | Prospective | 01/03/20–30/04/20 (rp: same in 2019) | Regional | ↑ | 682 hip fxs in 2020, 664 in 2019 |
| Arafa et al., 2020, [35] | United Kingdom | Retrospective | 01/03/20–31/05/20 (rp: same in 2019) | Local | ↑ | 61.7% increase compared with 2019 |
| Hall et al., 2020, [36] | United Kingdom (Scotland) | Retrospective | 01/03/20–15/04/20 | National | → | Differences between regions due to testing strategies, social distancing policies, and ld measures. |
| Ogliari et al., 2020, [37] | United Kingdom | Prospective | 1st–12th w 2020 (pre-ld), 13th–19th w 2020 (ld) (rp: same in 2015–2019) | Local | → | Hip fxs unchanged during ld, ↓ in nonhip fragility fxs |
| Haskel et al., 2020, [38] | United States of America | Retrospective | 22/03/20–30/04/20 (rp: same in 2019) | Local | → | overall ↓ in ortho cases |
| Ojeda-Thies et al., 2020, [19] | Spain | Retrospective | 01/03/20–01/05/20 (rp: same in 2018, 2019) | Local | ↓ | 5.5% of pts presented >24 h after injury |
| Wignall et al., 2021, [39] | United Kingdom | Retrospective | 01/03/20–30/05/20 (rp: same in 2019) | Regional | ↓ | ↓ admissions in total (304 vs. 276). → average admissions/d. |
| Crozier-Shaw et al., 2021, [40] | Ireland | Retrospective | 20/0320–20/05/20 (rp: same in 2019) | Regional | ↓ | 20% ↓ in hip fxs |
| Da Silva et al., 2022, [41] | Brazil | Retrospective | 03/20–12/20(rp: same in 2019) | National and regional | ↓ | ↓ in domestic accidents |
| Troiano et al., 2023, [42] | Italy | Retrospective | 09/03/2020–03/05/2020, (rp: same in 2019, 2021) | Regional | ↓ | Almost unchanged (36 pts in 2019 vs. 28 in 2020 vs. 29 in 2021) |
| Study | Country | Type of Study | Period of Study | Scope | Time to Surgery | Comments |
|---|---|---|---|---|---|---|
| Egol et al., 2020, [32] | United States of America | Prospective | 01/02/2020–15/04/2020 (rp: same in 2019) | Regional | → | ↑ for COVID-19{+} pts vs. COVID-19{−} pts |
| Malik-Tabassum et al., 2020, [33] | United Kingdom | Retrospective | 23/03/2020–11/05/2020 (rp: same in 2018, 2019) | Local | ↓ | Not statistically significant |
| Muñoz Vives et al., 2020, [49] | Spain | Retrospective | 14/05/2020–04/03/2020 (no rp) | National | → | Results similar to the Spanish National Hip Fracture Registry |
| Narang et al., 2020, [34] | United Kingdom | Prospective | 01/03/2020–30/04/2020 (rp: same in 2019) | Regional | ↑ | Delays due to complex AGPs, |
| Dupley et al., 2020, [48] | United Kingdom | Retrospective | 01/03/2020–26/04/2020 (rp: same in 2016–2019) | National | ↓ | In 64% definitive surgery within 36 h, vs. 60.1% and 58% in March and April 2016–2019 |
| Arafa et al., 2020, [35] | United Kingdom | Retrospective | 01/03/2020–31/05/2020 (rp: same in 2019) | Local | ↑ | Not statistically significant |
| Hall et al., 2020, [36] | United Kingdom (Scotland) | Retrospective | 01/03/2020–14/04/2020 | National | → | No difference when compared 23 d pre and after ld |
| Ojeda-Thies et al., 2021, [47] | Spain | Retrospective | 01/03/2020–01/05/2020 (rp: same in 2018, 2019) | Local | ↓ | Controversial results, authors avoided surgery upon systematic inflammatory involvement |
| Wignall et al., 2021, [39] | United Kingdom | Retrospective | 01/03/2020–30/05/2020 (rp: same in 2019) | Regional | ↑ | COVID-19{+} pts with significantly higher delay compared to COVID-19{−} |
| Crozier-Shaw et al., 2021, [40] | Ireland | Retrospective | 20/03/2020–20/05/2020 (rp: same in 2019) | Local | ↓ | 57.8% of the pts treated within 48 h in 2019, 78% in 2020 |
| Troiano et al., 2023 [42] | Italy | Retrospective | 09/03/2020–03/05/2020 (rp: same in 2019, 2021) | Regional | → | No statistically significant change during ld, longer in 2021 group |
| Study | Country | Type of Study | Period of Study | Scope | Length of Stay | Comments |
|---|---|---|---|---|---|---|
| Egol et al., 2020, [32] | United Kingdom | Prospective | 01/02/2020–15/04/2020 (rp: same in 2019) | Regional | ↑ | COVID-19{+} and pts suspected for infection with greater length of stay than COVID-19{−} pts |
| Malik-Tabassum et al., 2020, [33] | United Kingdom | Retrospective | 23/03/2020–11/05/2020 (rp: same in 2018, 2019) | Local | ↓ | Higher portion of pts discharged to rehabilitation center |
| Arafa et al., 2020, [35] | United Kingdom | Retrospective | 01/03/2020–31/05/2020 (rp: same in 2019) | Local | Variable | Mean total length of stay significantly longer in COVID-19{+} pts compared to COVID-19{−} pts and 2019 pts |
| Hall et al., 2020, [36] | United Kingdom (Scotland) | Retrospective | 01/03/2020–15/04/2020 | National | ↓ | Significant ↓ due to fear of viral transmission, or more resources available from ↓in polytrauma pts |
| Ojeda-Thies et al., 2021, [47] | Spain | Retrospective | 01/03/2020–01/05/2020 (rp: same in 2018, 2019) | Local | ↓ | ↓length of stay in pre COVID-19 period and COVID-19{−} pts |
| Shemesh et al., 2021, [52] | Israel | Retrospective | 01/03/2020–31/05/2020 (rp: same in 2017, 2018) | Local | ↓ | Influenced by the fear of in-hospital viral transmission |
| Wignall et al., 2021, [39] | United Kingdom | Retrospective | 01/03/2020–30/05/2020 (rp: same in 2019) | Regional | ↓ | Significant ↑in pre COVID-19 group and COVID-19{+} pts compared to COVID-19{−} |
| da Silva et al., 2022, [41] | Brazil | Retrospective | 03/2020–12/2020 (rp: same in 2019) | National and regional | ↓ | Reflects the need for beds for COVID-19(+) pts |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iliopoulos, I.D.; Lianou, I.; Kaspiris, A.; Ntourantonis, D.; Arachoviti, C.; Zafeiris, C.P.; Lambrou, G.I.; Chronopoulos, E. Impact of COVID-19 Pandemic on Fragility Fractures of the Hip: An Interrupted Time-Series Analysis of the Lockdown Periods in Western Greece and Review of the Literature. Geriatrics 2023, 8, 72. https://doi.org/10.3390/geriatrics8040072
Iliopoulos ID, Lianou I, Kaspiris A, Ntourantonis D, Arachoviti C, Zafeiris CP, Lambrou GI, Chronopoulos E. Impact of COVID-19 Pandemic on Fragility Fractures of the Hip: An Interrupted Time-Series Analysis of the Lockdown Periods in Western Greece and Review of the Literature. Geriatrics. 2023; 8(4):72. https://doi.org/10.3390/geriatrics8040072
Chicago/Turabian StyleIliopoulos, Ilias D., Ioanna Lianou, Angelos Kaspiris, Dimitrios Ntourantonis, Christine Arachoviti, Christos P. Zafeiris, George I. Lambrou, and Efstathios Chronopoulos. 2023. "Impact of COVID-19 Pandemic on Fragility Fractures of the Hip: An Interrupted Time-Series Analysis of the Lockdown Periods in Western Greece and Review of the Literature" Geriatrics 8, no. 4: 72. https://doi.org/10.3390/geriatrics8040072
APA StyleIliopoulos, I. D., Lianou, I., Kaspiris, A., Ntourantonis, D., Arachoviti, C., Zafeiris, C. P., Lambrou, G. I., & Chronopoulos, E. (2023). Impact of COVID-19 Pandemic on Fragility Fractures of the Hip: An Interrupted Time-Series Analysis of the Lockdown Periods in Western Greece and Review of the Literature. Geriatrics, 8(4), 72. https://doi.org/10.3390/geriatrics8040072








