One Step at a Time: Improving Gait Speed Measurement in a Geriatric Medicine Clinic
Abstract
:1. Introduction
1.1. Problem Description
1.2. Available Knowledge
1.3. Rationale
1.4. Specific Aims
2. Materials and Methods
2.1. Context
2.2. 4 m Gait Speed Measurement
2.3. Interventions
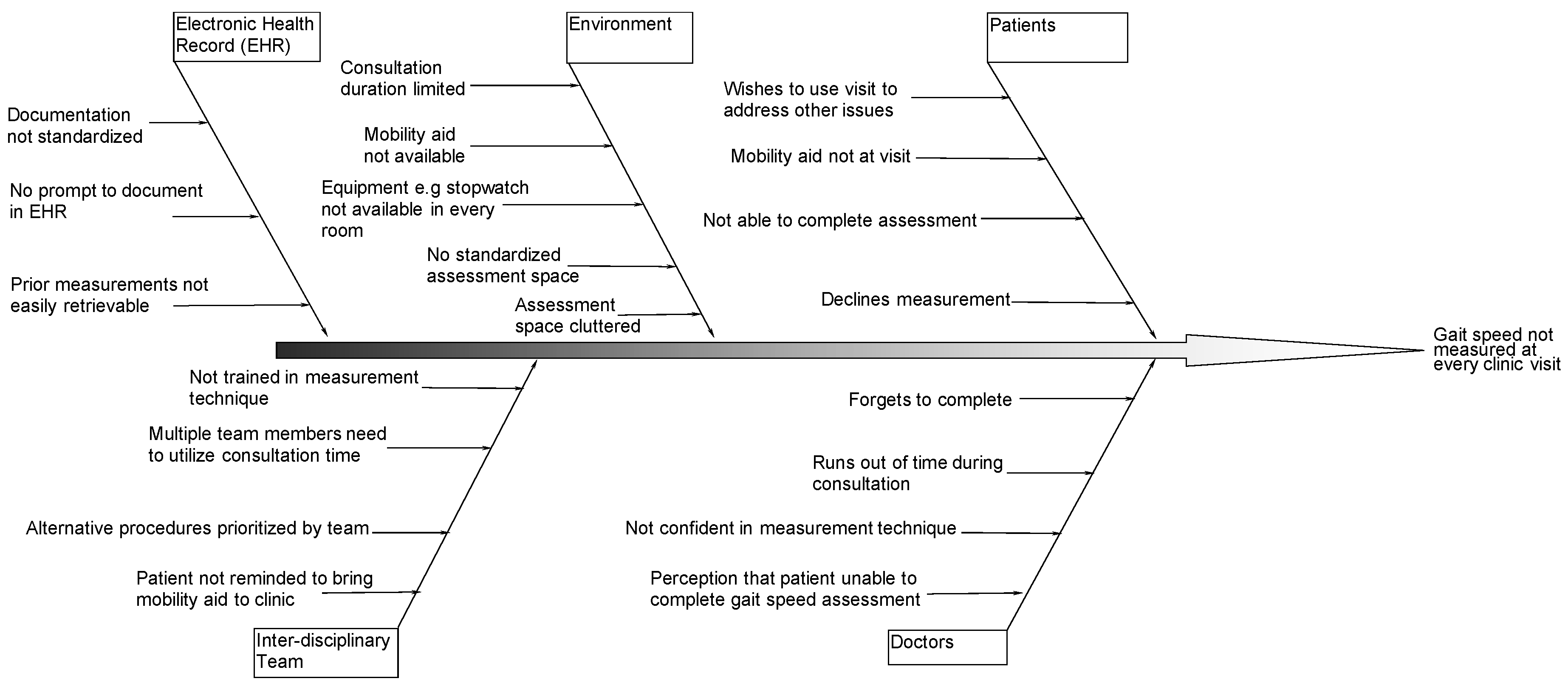
2.3.1. Study of the Interventions
2.3.2. Measures
2.3.3. Analysis
2.3.4. Ethical Considerations
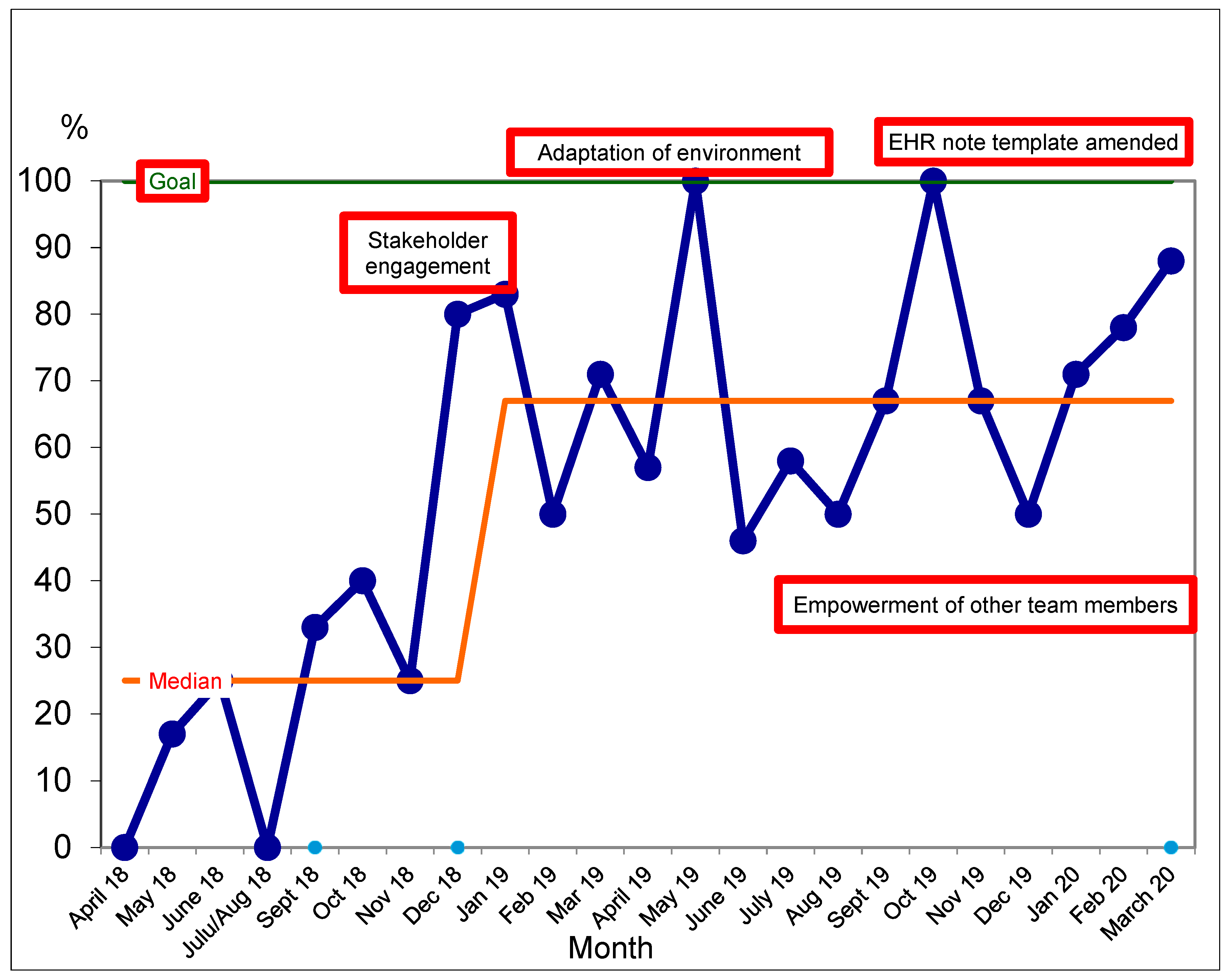
3. Results
Change Interventions
4. Discussion
4.1. Summary
4.2. Interpretation
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Choi, N.G.; Choi, B.Y.; DiNitto, D.M.; Marti, C.N.; Kunik, M.E. Fall-related emergency department visits and hospitalizations among community-dwelling older adults: Examination of health problems and injury characteristics. BMC Geriatr. 2019, 19, 303. [Google Scholar] [CrossRef]
- Burns, E.; Kakara, R. Deaths from Falls Among Persons Aged ≥65 Years—United States, 2007–2016. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 509–514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ellis, G.; Whitehead, M.A.; Robinson, D.; O’Neill, D.; Langhorne, P. Comprehensive geriatric assessment for older adults admitted to hospital: Meta-analysis of randomised controlled trials. BMJ 2011, 343, d6553. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morley, J.E.; Little, M.O.; Berg-Weger, M. Rapid Geriatric Assessment: A Tool for Primary Care Physicians. J. Am. Med. Dir. Assoc. 2017, 18, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Fulmer, T.; Mate, K.S.; Berman, A. The Age-Friendly Health System Imperative. J. Am. Geriatr. Soc. 2018, 66, 22–24. [Google Scholar] [CrossRef]
- Middleton, A.; Fritz, S.L.; Lusardi, M. Walking speed: The functional vital sign. J. Aging Phys. Act. 2015, 23, 314–322. [Google Scholar] [CrossRef]
- Studenski, S.; Perera, S.; Wallace, D.; Chandler, J.M.; Duncan, P.W.; Rooney, E.; Fox, M.; Guralnik, J.M. Physical performance measures in the clinical setting. J. Am. Geriatr. Soc. 2003, 51, 314–322. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.R.; Xu, W.; Zhang, W.; Wang, H.F.; Ou, Y.N.; Qu, Y.; Shen, X.N.; Chen, S.D.; Wu, K.M.; Zhao, Q.H.; et al. Modifiable risk factors for incident dementia and cognitive impairment: An umbrella review of evidence. J. Affect. Disord. 2022, 314, 160–167. [Google Scholar] [CrossRef]
- Lauretani, F.; Russo, C.R.; Bandinelli, S.; Bartali, B.; Cavazzini, C.; Di Iorio, A.; Corsi, A.M.; Rantanen, T.; Guralnik, J.M.; Ferrucci, L. Age-associated changes in skeletal muscles and their effect on mobility: An operational diagnosis of sarcopenia. J. Appl. Physiol. 2003, 95, 1851–1860. [Google Scholar] [CrossRef] [Green Version]
- James, K.; Schwartz, A.W.; Orkaby, A.R. Mobility Assessment in Older Adults. N. Engl. J. Med. 2021, 385, e22. [Google Scholar] [CrossRef]
- Studenski, S.; Perera, S.; Patel, K.; Rosano, C.; Faulkner, K.; Inzitari, M.; Brach, J.; Chandler, J.; Cawthon, P.; Connor, E.B.; et al. Gait speed and survival in older adults. JAMA 2011, 305, 50–58. [Google Scholar] [CrossRef] [Green Version]
- Ekström, H.; Dahlin-Ivanoff, S.; Elmståhl, S. Effects of walking speed and results of timed get-up-and-go tests on quality of life and social participation in elderly individuals with a history of osteoporosis-related fractures. J. Aging Health 2011, 23, 1379–1399. [Google Scholar] [CrossRef]
- Espinoza, S.E.; Orsak, B.; Wang, C.P.; MacCarthy, D.; Kellogg, D.; Powers, B.; Conde, A.; Moris, M.; Padala, P.R.; Padala, K.P. An Individualized Low-Intensity Walking Clinic Leads to Improvement in Frailty Characteristics in Older Veterans. J. Frailty Aging 2019, 8, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Orkaby, A.R.; James, K.; Leuchtenburg, J.; Solooki, E.; Gaziano, J.M.; Driver, J.A. Taking prevention to the next step: Implementation of a brief, sustainable frailty assessment in a cardiology clinic. BMJ Open Qual. 2021, 10, e001140. [Google Scholar] [CrossRef]
- Rydwik, E.; Bergland, A.; Forsén, L.; Frändin, K. Investigation into the reliability and validity of the measurement of elderly people’s clinical walking speed: A systematic review. Physiother. Theory Pract. 2012, 28, 238–256. [Google Scholar] [CrossRef]
- Benneyan, J.C.; Lloyd, R.C.; Plsek, P.E. Statistical process control as a tool for research and healthcare improvement. Qual. Saf. Health Care 2003, 12, 458–464. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ogrinc, G.; Davies, L.; Goodman, D.; Batalden, P.; Davidoff, F.; Stevens, D. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): Revised publication guidelines from a detailed consensus process. BMJ Qual. Saf. 2016, 25, 986–992. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perla, R.J.; Provost, L.P.; Murray, S.K. The run chart: A simple analytical tool for learning from variation in healthcare processes. BMJ Qual. Saf. 2011, 20, 46–51. [Google Scholar] [CrossRef]
- Swed, F.S.; Eisenhart, C. Tables for Testing Randomness of Grouping in a Sequence of Alternatives. Ann. Math. Stat. 1943, 14, 66–87. [Google Scholar] [CrossRef]
- Soubra, R.; Chkeir, A.; Novella, J.L. A Systematic Review of Thirty-One Assessment Tests to Evaluate Mobility in Older Adults. Biomed. Res. Int. 2019, 2019, 1354362. [Google Scholar] [CrossRef]
- Schwartz, A.W.; Driver, J.A.; Pollara, L.M.; Roefaro, J.; Harrington, M.B.; Charness, M.E.; Skarf, L.M. Increasing Telehealth Visits for Older Veterans Associated with Decreased No-Show Rate in a Geriatrics Consultation Clinic. J. Gen. Intern. Med. 2022, 37, 3217–3219. [Google Scholar] [CrossRef] [PubMed]
- Tinetti, M.; Huang, A.; Molnar, F. The Geriatrics 5M’s: A New Way of Communicating What We Do. J. Am. Geriatr. Soc. 2017, 65, 2115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burke, R.E.; Brown, R.T.; Kinosian, B. Selecting implementation strategies to drive Age-Friendly Health System Adoption. J. Am. Geriatr. Soc. 2022, 70, 313–318. [Google Scholar] [CrossRef] [PubMed]
| N = 80 | |
|---|---|
| Mean age (years) | 82 ± 7.7 |
| Male | 98% |
| Visit type | |
| New | 46% |
| Follow up | 54% |
| Patient accompanied by a caregiver | 53% |
| Medical history | |
| Diabetes | 38% |
| Dementia | 51% |
| Social Circumstances | |
| Lives alone (n = 63) | 38% |
| Caregiver stress (n = 64) | 25% |
| ADLs | |
| Independent in all | 51% |
| Requries assistance, some/most/all | 38% |
| Dependent, some or most | 6% |
| Dependent, all | 5% |
| iADLs | |
| Independent, all | 14% |
| Requires assistance, some/most/all | 24% |
| Dependent, some or most | 36% |
| Dependent, all | 26% |
| Mobility | |
| Fall in the past 6 months | 32% |
| Number of falls in past 6 months (range) | 1–5 |
| Median gait speed | 0.69 (IQR: 0.56–0.87) |
| Orthostatic hypotension (n = 49) | 12% |
| Ability to don/doff socks (n = 72) | |
| Able | 54% |
| With difficulty | 24% |
| Unable | 22% |
| Assistive device use | 58% |
| Assistive device type (n = 43) | |
| Cane | 40% |
| Walker | 42% |
| Wheelchair | 18% |
| Type of shoes (n = 50) | |
| Laces | 50% |
| Slip-on | 28% |
| Velcro | 22% |
| Chair stand (n = 69) | |
| Able | 39% |
| With difficulty | 28% |
| Unable | 33% |
| n = 21 | % (n) |
|---|---|
| No assistive device | 33% (7) |
| Wheelchair user | 38% (8) |
| No time | 10% (2) |
| Other/not documented | 19% (4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
James, K.; Growdon, M.E.; Orkaby, A.R.; Schwartz, A.W. One Step at a Time: Improving Gait Speed Measurement in a Geriatric Medicine Clinic. Geriatrics 2023, 8, 81. https://doi.org/10.3390/geriatrics8040081
James K, Growdon ME, Orkaby AR, Schwartz AW. One Step at a Time: Improving Gait Speed Measurement in a Geriatric Medicine Clinic. Geriatrics. 2023; 8(4):81. https://doi.org/10.3390/geriatrics8040081
Chicago/Turabian StyleJames, Kirstyn, Matthew E. Growdon, Ariela R. Orkaby, and Andrea Wershof Schwartz. 2023. "One Step at a Time: Improving Gait Speed Measurement in a Geriatric Medicine Clinic" Geriatrics 8, no. 4: 81. https://doi.org/10.3390/geriatrics8040081
APA StyleJames, K., Growdon, M. E., Orkaby, A. R., & Schwartz, A. W. (2023). One Step at a Time: Improving Gait Speed Measurement in a Geriatric Medicine Clinic. Geriatrics, 8(4), 81. https://doi.org/10.3390/geriatrics8040081







