The Effects of Colchicum Dispert and Bone Marrow-Derived Mesenchymal Stem Cell Therapy on Skeletal Muscle Injury in a Rat Aortic Ischemia–Reperfusion Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Approval and Animal Subjects
2.2. Experimental Design
2.3. Ischemia–Reperfusion Injury Model
2.3.1. Mesenchymal Stem Cell Preparation
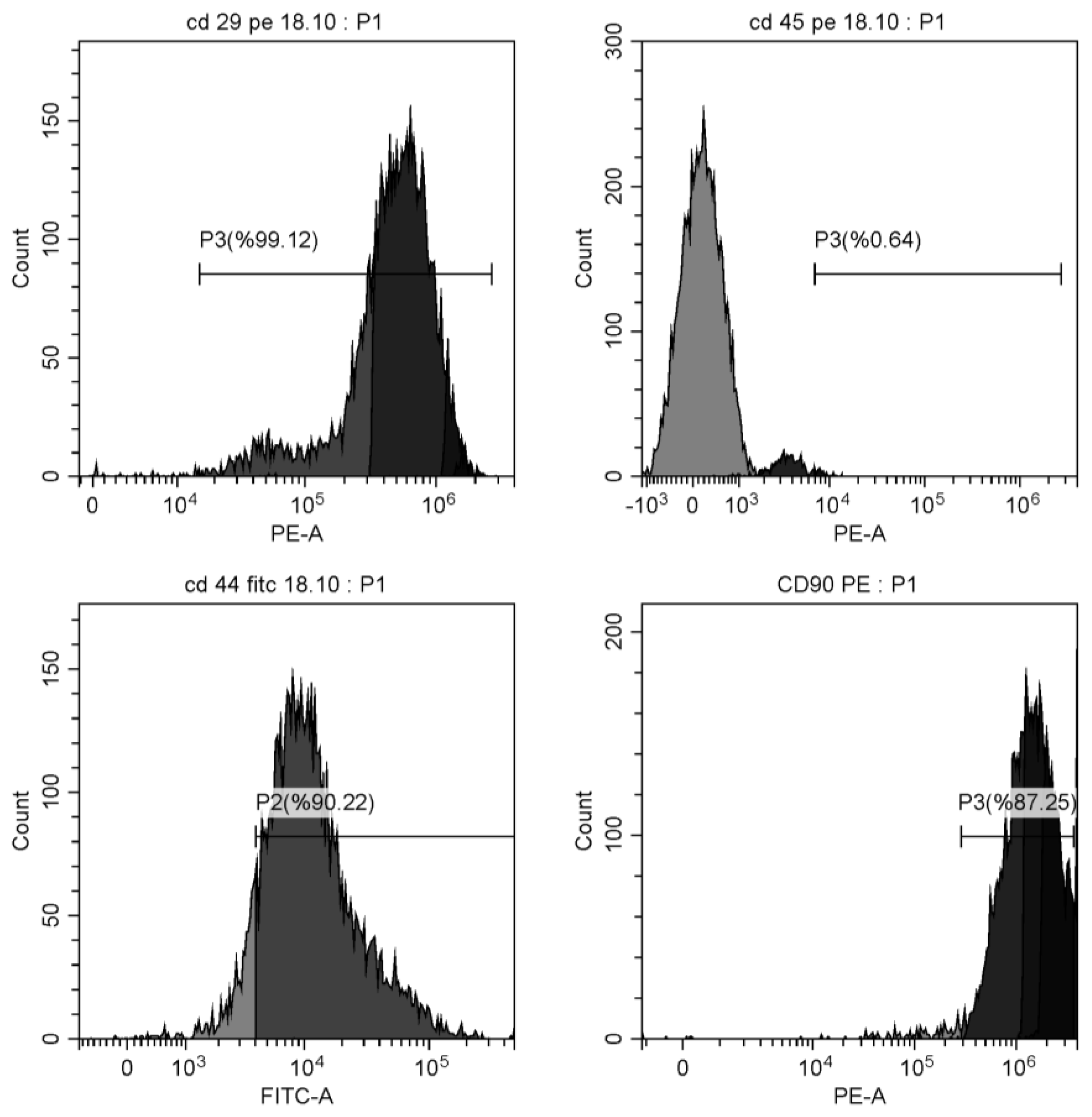
2.3.2. Surface Antigen Characterization
2.4. Blood Sample Analysis
2.5. Tissue Sample Analysis
2.6. Statistical Analysis
3. Results
3.1. Biochemical Results
3.2. Skeletal Muscle Tissue Results
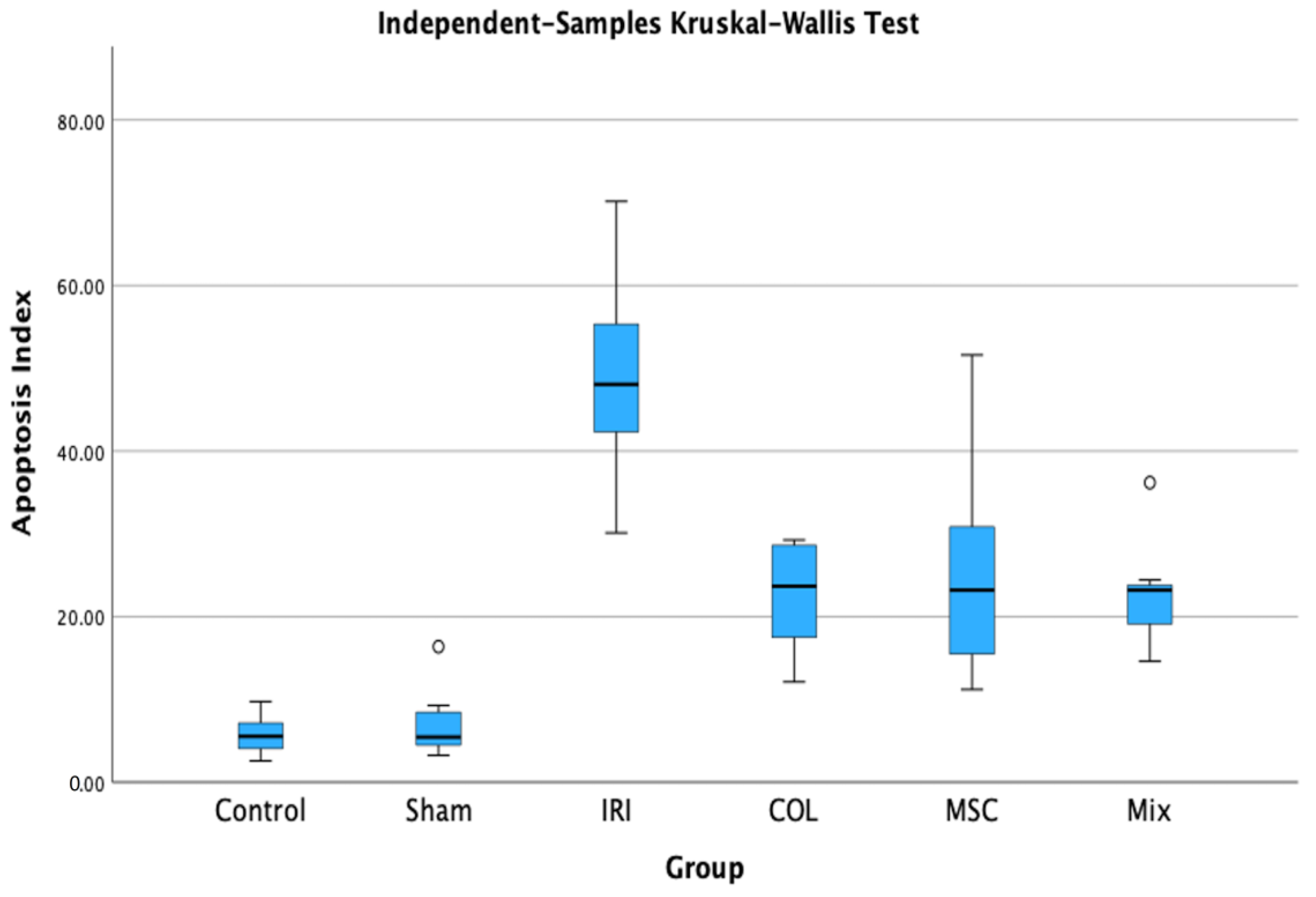
3.3. Apoptosis Results in Skeletal Muscle
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lazaris, A.M.; Maheras, A.N.; Vasdekis, S.N.; Karkaletsis, K.G.; Charalambopoulos, A.; Kakisis, J.D.; Martikos, G.; Patapis, P.; Giamarellos-Bourboulis, E.J.; Karatzas, G.M.; et al. Protective effect of remote ischemic preconditioning in renal ischemia/reperfusion injury, in a model of thoracoabdominal aorta approach. J. Surg. Res. 2009, 154, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Algoet, M.; Janssens, S.; Himmelreich, U.; Gsell, W.; Pusovnik, M.; van den Eynde, J.; Oosterlinck, W. Myocardial ischemia-reperfusion injury and the influence of inflammation. Trends Cardiovasc. Med. 2023, 33, 357–366. [Google Scholar] [CrossRef]
- Lima, V.S.S.; Mariano, D.O.C.; Vigerelli, H.; Janussi, S.C.; Baptista, T.V.L.; Claudino, M.A.; Pimenta, D.C.; Sciani, J.M. Effects of Kynurenic Acid on the Rat Aorta Ischemia-Reperfusion Model: Pharmacological Characterization and Proteomic Profiling. Molecules 2021, 26, 2845. [Google Scholar] [CrossRef] [PubMed]
- Cancel, L.M.; Ebong, E.E.; Mensah, S.; Hirschberg, C.; Tarbell, J.M. Endothelial glycocalyx, apoptosis and inflammation in an atherosclerotic mouse model. Atherosclerosis 2016, 252, 136–146. [Google Scholar] [CrossRef]
- Waksman, R.; Merdler, I.; Case, B.C.; Waksman, O.; Porto, I. Targeting inflammation in atherosclerosis: Overview, strategy and directions. EuroIntervention 2024, 20, 32–44. [Google Scholar] [CrossRef] [PubMed]
- Costa, D.L.; Amaral, E.P.; Andrade, B.B.; Sher, A. Modulation of Inflammation and Immune Responses by Heme Oxygenase-1: Implications for Infection with Intracellular Pathogens. Antioxidants 2020, 9, 1205. [Google Scholar] [CrossRef]
- Zhang, Y.N.; Wu, Q.; Zhang, N.N.; Chen, H.S. Ischemic Preconditioning Alleviates Cerebral Ischemia-Reperfusion Injury by Interfering With Glycocalyx. Transl. Stroke Res. 2023, 14, 929–940. [Google Scholar] [CrossRef]
- Czibik, G.; Derumeaux, G.; Sawaki, D.; Valen, G.; Motterlini, R. Heme oxygenase-1: An emerging therapeutic target to curb cardiac pathology. Basic Res. Cardiol. 2014, 109, 450. [Google Scholar] [CrossRef]
- El-Said, N.T.; Mohamed, E.A.; Raslan, N.; Awad, A.S. Insight into the role of Nrf-2/HO-1 hub in the protective effect of colchicine on renal ischemia-reperfusion induced distance organs dysfunction. Azhar Int. J. Pharm. Med. Sci. 2022, 2, 21–33. [Google Scholar] [CrossRef]
- Mori, H.; Taki, J.; Wakabayashi, H.; Hiromasa, T.; Inaki, A.; Ogawa, K.; Shiba, K.; Kinuya, S. Colchicine treatment early after infarction attenuates myocardial inflammatory response demonstrated by (14)C-methionine imaging and subsequent ventricular remodeling by quantitative gated SPECT. Ann. Nucl. Med. 2021, 35, 253–259. [Google Scholar] [CrossRef]
- Fujisue, K.; Sugamura, K.; Kurokawa, H.; Matsubara, J.; Ishii, M.; Izumiya, Y.; Kaikita, K.; Sugiyama, S. Colchicine Improves Survival, Left Ventricular Remodeling, and Chronic Cardiac Function After Acute Myocardial Infarction. Circ. J. 2017, 81, 1174–1182. [Google Scholar] [CrossRef] [PubMed]
- Oliva, J. Therapeutic Properties of Mesenchymal Stem Cell on Organ Ischemia-Reperfusion Injury. Int. J. Mol. Sci. 2019, 20, 5511. [Google Scholar] [CrossRef]
- Chen, Q.; Liu, Y.; Ding, X.; Li, Q.; Qiu, F.; Wang, M.; Shen, Z.; Zheng, H.; Fu, G. Bone marrow mesenchymal stem cell-secreted exosomes carrying microRNA-125b protect against myocardial ischemia reperfusion injury via targeting SIRT7. Mol. Cell. Biochem. 2020, 465, 103–114. [Google Scholar] [CrossRef]
- Jiang, H.; Qu, L.; Li, Y.; Gu, L.; Shi, Y.; Zhang, J.; Zhu, W.; Li, J. Bone marrow mesenchymal stem cells reduce intestinal ischemia/reperfusion injuries in rats. J. Surg. Res. 2011, 168, 127–134. [Google Scholar] [CrossRef]
- Kanazawa, H.; Fujimoto, Y.; Teratani, T.; Iwasaki, J.; Kasahara, N.; Negishi, K.; Tsuruyama, T.; Uemoto, S.; Kobayashi, E. Bone marrow-derived mesenchymal stem cells ameliorate hepatic ischemia reperfusion injury in a rat model. PLoS ONE 2011, 6, e19195. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Gu, J.; Yang, O.; Wang, J.; Wang, Y.; Kong, J. Bone Marrow Mesenchymal Stem Cell-Derived Exosomal miRNA-29c Decreases Cardiac Ischemia/Reperfusion Injury Through Inhibition of Excessive Autophagy via the PTEN/Akt/mTOR Signaling Pathway. Circ. J. 2020, 84, 1304–1311. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Shan, Y.; Chen, L.; Lin, B.; Xiong, X.; Lin, L.; Jin, L. Colchicine protects rat skeletal muscle from ischemia/reperfusion injury by suppressing oxidative stress and inflammation. Iran. J. Basic Med. Sci. 2016, 19, 670–675. [Google Scholar]
- Akodad, M.; Fauconnier, J.; Sicard, P.; Huet, F.; Blandel, F.; Bourret, A.; de Santa Barbara, P.; Aguilhon, S.; LeGall, M.; Hugon, G.; et al. Interest of colchicine in the treatment of acute myocardial infarct responsible for heart failure in a mouse model. Int. J. Cardiol. 2017, 240, 347–353. [Google Scholar] [CrossRef]
- Awad, A.S.; Elariny, H.A.; Sallam, A.S. The possible protective effect of colchicine against liver damage induced by renal ischemia-reperfusion injury: Role of Nrf2 and NLRP3 inflammasome. Can. J. Physiol. Pharmacol. 2020, 98, 849–854. [Google Scholar] [CrossRef]
- Gozukara, K.H.; Ozcan, O.; Ozgur, T.; Kaya, Y.S.; Tutuk, O. Protective Effects of Colchicine on Testicular Torsion/Detorsion-Induced Ischemia/Reperfusion Injury in Rats. Urol. J. 2020, 17, 294–300. [Google Scholar] [CrossRef]
- Sekmenli, T.; Gunduz, M.; Ozturk, B.; Karabagli, P.; Ciftci, I.; Tekin, G.; Yilmaz, M. The effects of melatonin and colchicine on ischemia-reperfusion injury in experimental rat testicular torsion model. J. Pediatr. Surg. 2017, 52, 582–586. [Google Scholar] [CrossRef] [PubMed]
- Kurt, R.K.; Dogan, A.C.; Dogan, M.; Albayrak, A.; Kurt, S.N.; Eren, F.; Okyay, A.G.; Karateke, A.; Duru, M.; Fadillioglu, E.; et al. Protective effect of colchicine on ovarian ischemia-reperfusion injury: An experimental study. Reprod. Sci. 2015, 22, 545–550. [Google Scholar] [CrossRef]
- Boybeyi, O.; Gunal, Y.D.; Atasoy, P.; Kisa, U.; Aslan, M.K. The effect of colchicine and low-dose methotrexate on intestinal ischemia/reperfusion injury in an experimental model. J. Pediatr. Surg. 2014, 49, 1471–1474. [Google Scholar] [CrossRef]
- El Gammal, Z.; Rashed, L.; Aziz, M.A.; Elwahy, A.H.; Youakim, M.; Seufi, A.M. Comparative study between the attenuation of cardiac fibrosis by mesenchymal stem cells versus colchicine. Acta Medica Int. 2016, 3, 137–145. [Google Scholar] [CrossRef]
- Arriero, M.; Brodsky, S.V.; Gealekman, O.; Lucas, P.A.; Goligorsky, M.S. Adult skeletal muscle stem cells differentiate into endothelial lineage and ameliorate renal dysfunction after acute ischemia. Am. J. Physiol. Renal Physiol. 2004, 287, F621–F627. [Google Scholar] [CrossRef]
- Chen, G.; Wang, M.; Ruan, Z.; Zhu, L.; Tang, C. Mesenchymal stem cell-derived exosomal miR-143-3p suppresses myocardial ischemia-reperfusion injury by regulating autophagy. Life Sci. 2021, 280, 119742. [Google Scholar] [CrossRef] [PubMed]
- Fu, M.; Xie, D.; Sun, Y.; Pan, Y.; Zhang, Y.; Chen, X.; Shi, Y.; Deng, S.; Cheng, B. Exosomes derived from MSC pre-treated with oridonin alleviates myocardial IR injury by suppressing apoptosis via regulating autophagy activation. J. Cell. Mol. Med. 2021, 25, 5486–5496. [Google Scholar] [CrossRef]
- Zahran, R.; Ghozy, A.; Elkholy, S.S.; El-Taweel, F.; El-Magd, M.A. Combination therapy with melatonin, stem cells and extracellular vesicles is effective in limiting renal ischemia-reperfusion injury in a rat model. Int. J. Urol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Yin, T.-C.; Wu, R.-W.; Sheu, J.-J.; Sung, P.-H.; Chen, K.-H.; Chiang, J.Y.; Hsueh, S.-K.; Chung, W.-J.; Lin, P.-Y.; Hsu, S.-L. Combined therapy with extracorporeal shock wave and adipose-derived mesenchymal stem cells remarkably improved acute ischemia-reperfusion injury of quadriceps muscle. Oxidative Med. Cell. Longev. 2018, 2018, 6012636. [Google Scholar] [CrossRef]
- Yeh, K.-H.; Sheu, J.-J.; Lin, Y.-C.; Sun, C.-K.; Chang, L.-T.; Kao, Y.-H.; Yen, C.-H.; Shao, P.-L.; Tsai, T.-H.; Chen, Y.-L. Benefit of combined extracorporeal shock wave and bone marrow-derived endothelial progenitor cells in protection against critical limb ischemia in rats. Crit. Care Med. 2012, 40, 169–177. [Google Scholar] [CrossRef]
- Liu, J.; Qiu, P.; Qin, J.; Wu, X.; Wang, X.; Yang, X.; Li, B.; Zhang, W.; Ye, K.; Peng, Z. Allogeneic adipose-derived stem cells promote ischemic muscle repair by inducing M2 macrophage polarization via the HIF-1α/IL-10 pathway. Stem Cells 2020, 38, 1307–1320. [Google Scholar] [CrossRef]
- Shevtsova, A.; Gordiienko, I.; Tkachenko, V.; Ushakova, G. Ischemia-modified albumin: Origins and clinical implications. Dis. Markers 2021, 2021, 1–18. [Google Scholar] [CrossRef]
- Wudkowska, A.; Goch, J.; Goch, A. Ischemia-modified albumin in differential diagnosis of acute coronary syndrome without ST elevation and unstable angina pectoris. Pol. Heart J. (Kardiol. Pol.) 2010, 68, 437–443. [Google Scholar]
- Öztorun, C.İ.; Doruk, H.; Güney, D.; Köse, Ü.N.İ.; Örnek Demir, T.; Çayhan, V.S.; Demir, S.; Ertürk, A.; Güngör, A.; Kara Uzun, A. Evaluation of dynamic/thiol disulphide balance and ischaemia modified albumin in children with trauma. Int. J. Clin. Pract. 2021, 75, e14713. [Google Scholar] [CrossRef]
- Tain, Y.-L.; Hsu, C.-N. Melatonin Use during Pregnancy and Lactation Complicated by Oxidative Stress: Focus on Offspring’s Cardiovascular–Kidney–Metabolic Health in Animal Models. Antioxidants 2024, 13, 226. [Google Scholar] [CrossRef]
- Ergün, Y.; Kılınç, M.; Aral, M.; Hedef, A.; Kaya, E. Protective effect of epigallocatechin gallate in ischemia-reperfusion injury of rat skeletal muscle. J. Surg. Res. 2020, 247, 1–7. [Google Scholar] [CrossRef]
- Wang, W.Z.; Fang, X.H.; Stephenson, L.L.; Khiabani, K.T.; Zamboni, W.A. Ischemia/reperfusion-induced necrosis and apoptosis in the cells isolated from rat skeletal muscle. J. Orthop. Res. 2008, 26, 351–356. [Google Scholar] [CrossRef]
- Pottecher, J.; Adamopoulos, C.; Lejay, A.; Bouitbir, J.; Meyer, A.; Wolff, V.; Laverny, G.; Geny, B. Diabetes worsens skeletal muscle mitochondrial function, oxidative stress, and apoptosis after lower-limb ischemia-reperfusion: Implication of the RISK and SAFE pathways? Front. Physiol. 2018, 9, 360072. [Google Scholar] [CrossRef]

| Weight Measurement | n | Pre-Study (g) (Mean ± SD) | Study (g) (Mean ± SD) |
|---|---|---|---|
| Control | 6 | 618.67 ± 39.79 | 614.33 ± 40.51 |
| Sham | 7 | 596.86 ± 53.73 | 604.57 ± 59.37 |
| IRI | 8 | 612.75 ± 41.53 | 612.25 ± 45.57 |
| COL | 6 | 602.67 ± 39.87 | 545.00 ± 44.81 |
| MSC | 8 | 598.00 ± 42.28 | 601.50 ± 50.24 |
| Mix | 7 | 596.00 ± 33.86 | 586.43 ± 49.95 |
| p-Value | 0.842 | 0.142 |
| CONTROL (n = 6) | SHAM (n = 7) | IRI (n = 8) | COL (n = 6) | MSC (n = 8) | MIX (n = 7) | p-Value | |
|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | ||
| TAC | 1.47 ± 0.09 | 1.65 ± 0.09 | 1.45 ± 0.11 | 1.34 ± 0.09 | 1.38 ± 0.11 | 1.24 ± 0.12 | 0.52 |
| TOS | 6.72 ± 1.23 | 6.24 ± 2.91 | 11.17 ± 7.17 | 9.11 ± 3.96 | 9.31 ± 6.07 | 8.28 ± 4.26 | 0.039 * |
| OSI | 4.55 ± 0.65 | 3.77 ± 1.72 | 7.61 ± 4.50 | 6.80 ± 2.90 | 6.78 ± 4.46 | 6.92 ± 4.15 | 0.000 * |
| NT (mmol/L) | 159.67 ± 28.93 | 211.14 ± 111.69 | 254.5 ± 85.50 | 297.83 ± 79,71 | 289.63 ± 127.91 | 279.86 ± 124.6 | 0.055 |
| TT (mmol/L) | 288.5 ± 41.38 | 374.29 ± 211.54 | 475.75 ± 193.39 | 464.17 ± 169.36 | 560.75 ± 201.25 | 502.86 ± 183.84 | 0.154 |
| DYSS (mmol/L) | 64.42 ± 21.62 | 81.57 ± 55.53 | 110.63 ± 58.76 | 83.17 ± 46.82 | 135.56 ± 73.29 | 111.5 ± 59.32 | 0.337 |
| DYSS/TT (%) | 22.01 ± 5.64 | 21.69 ± 7.00 | 22.15 ± 4.42 | 16.67 ± 4.79 | 24.52 ± 9.66 | 22.84 ± 9.54 | 0.52 |
| DYSS/NT (%) | 43.00 ± 22.10 | 44.02 ± 27.98 | 42.00 ± 16.32 | 26.24 ± 10.29 | 61.96 ± 43.8 | 56.23 ± 49.77 | 0.52 |
| NT/TT (%) | 55.97 ± 11.28 | 56.63 ± 13.99 | 55.70 ± 8.85 | 66.66 ± 9.57 | 50.96 ± 19.32 | 54.32 ± 19.08 | 0.261 |
| Control (n = 6) | Sham (n = 7) | IRI (n = 8) | COL (n = 6) | MSC (n = 8) | Mix (n = 7) | p-Value | |
|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | ||
| IMA | 1.43 ± 0.28 | 1.68 ± 0.12 | 1.66 ± 0.11 | 1.69 ± 0.11 | 1.65 ± 0.23 | 1.29 ± 0.31 | 0.020 * |
| ADMA | 0.21 ± 0.15 | 0.16 ± 0.09 | 0.26 ± 0.09 | 0.41 ± 0.36 | 0.23 ± 0.09 | 0.3 ± 0.09 | 0.069 |
| SDMA | 0.40 ± 0.26 | 0.34 ± 0.09 | 0.43 ± 0.10 | 0.61 ± 0.42 | 0.40 ± 0.15 | 0.27 ± 0.08 | 0.097 |
| L-NMMA | 0.08 ± 0.06 | 0.07 ± 0.05 | 0.07 ± 0.04 | 0.10 ± 0.10 | 0.06 ± 0.04 | 0.06 ± 0.03 | 1.00 |
| ARG | 69.66 ± 13.77 | 54.87 ± 11.88 | 34.23 ± 20.88 | 67.53 ± 22.78 | 47.35 ± 20.2 | 58.42 ± 18.78 | 0.028 * |
| CIT | 133.45 ± 67.03 | 131.79 ± 66.71 | 206.00 ± 78.48 | 112.15 ± 60.27 | 147.48 ± 63.4 | 103.13 ± 35.31 | 0.132 |
| ORN | 28.25 ± 15.16 | 21.35 ± 10.12 | 30.05 ± 7.28 | 21.22 ± 11.56 | 27.85 ± 11.16 | 20.51 ± 5.74 | 0.336 |
| HoARG | 1.42 ± 0.80 | 1.09 ± 0.39 | 1.64 ± 0.59 | 1.52 ± 0.74 | 1.36 ± 0.98 | 1.08 ± 0.49 | 0.479 |
| CONTROL (n = 6) | SHAM (n = 7) | IRI (n = 8) | COL (n = 6) | MSC (n = 8) | MIX (n = 7) | p-Value | |
|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | ||
| TAC | 1.01 ± 0.08 | 0.98 ± 0.07 | 0.98 ± 0.12 | 0.99 ± 0.14 | 0.83 ± 0.07 | 0.96 ± 0.02 | 0.020 * |
| TOS | 9.86 ± 3.80 | 9.87 ± 3.07 | 11.67 ± 2.86 | 14.63 ± 10.59 | 9.74 ± 2.51 | 11.11 ± 0.01 | 0.577 |
| OSI | 9.74 ± 3.49 | 9.94 ± 2.58 | 11.76 ± 2.06 | 14.09 ± 7.60 | 11.68 ± 2.3 | 11.42 ± 0.01 | 0.499 |
| ADMA | 0.20 ± 0.10 | 0.18 ± 0.09 | 0.23 ± 0.07 | 0.38 ± 0.37 | 0.24 ± 0.06 | 0.39 ± 0.19 | 0.093 |
| SDMA | 0.10 ± 0.06 | 0.11 ± 0.03 | 0.12 ± 0.04 | 0.23 ± 0.17 | 0.07 ± 0.02 | 0.10 ± 0.02 | 0.017 * |
| L-NMMA | 0.03 ± 0.01 | 0.03 ± 0.02 | 0.04 ± 0.03 | 0.04 ± 0.02 | 0.03 ± 0.01 | 0.07 ± 0.05 | 0.417 |
| ARG | 34.52 ± 13.31 | 49.27 ± 16.08 | 38.65 ± 17.80 | 41.95 ± 14.66 | 26.21 ± 11.21 | 42.54 ± 14.43 | 0.108 |
| CIT | 17.53 ± 11.88 | 19.41 ± 8.11 | 22.73 ± 17.69 | 13.70 ± 8.58 | 13.65 ± 3.97 | 37.27 ± 16.66 | 0.036 * |
| ORN | 3.10 ± 1.60 | 3.54 ± 1.86 | 3.83 ± 1.52 | 3.58 ± 0.81 | 3.93 ± 1 | 5.19 ± 1.79 | 0.29 |
| HOARG | 0.20 ± 0.09 | 0.26 ± 0.19 | 0.32 ± 0.51 | 0.19 ± 0.08 | 0.25 ± 0.32 | 1.23 ± 1.51 | 0.092 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Orhan, A.; Çiçek, Ö.F.; Öztürk, B.; Akbayrak, H.; Ünlükal, N.; Vatansev, H.; Solmaz, M.; Büyükateş, M.; Aniç, S.; Ovalı, F.; et al. The Effects of Colchicum Dispert and Bone Marrow-Derived Mesenchymal Stem Cell Therapy on Skeletal Muscle Injury in a Rat Aortic Ischemia–Reperfusion Model. J. Cardiovasc. Dev. Dis. 2024, 11, 251. https://doi.org/10.3390/jcdd11080251
Orhan A, Çiçek ÖF, Öztürk B, Akbayrak H, Ünlükal N, Vatansev H, Solmaz M, Büyükateş M, Aniç S, Ovalı F, et al. The Effects of Colchicum Dispert and Bone Marrow-Derived Mesenchymal Stem Cell Therapy on Skeletal Muscle Injury in a Rat Aortic Ischemia–Reperfusion Model. Journal of Cardiovascular Development and Disease. 2024; 11(8):251. https://doi.org/10.3390/jcdd11080251
Chicago/Turabian StyleOrhan, Atilla, Ömer Faruk Çiçek, Bahadır Öztürk, Hakan Akbayrak, Nejat Ünlükal, Hakan Vatansev, Merve Solmaz, Mustafa Büyükateş, Seda Aniç, Fadime Ovalı, and et al. 2024. "The Effects of Colchicum Dispert and Bone Marrow-Derived Mesenchymal Stem Cell Therapy on Skeletal Muscle Injury in a Rat Aortic Ischemia–Reperfusion Model" Journal of Cardiovascular Development and Disease 11, no. 8: 251. https://doi.org/10.3390/jcdd11080251





