Abstract
The skin mycobiota plays a significant role in infection risk, pathogen transmission, and personalized medicine approaches in intensive care settings. This prospective multicenter study aimed to enhance our understanding of intensive care units’ (ICUs’) Candida colonization dynamics, identify modifiable risk factors, and assess their impact on survival risk. Specimens were taken from 675, 203, and 110 patients at the admission (D1), 5th (D5), and 8th (D8) days of ICU stay, respectively. The patient’s demographic and clinical data were collected. Candida isolates were identified by conventional culture-based microbiology combined with molecular approaches. Overall, colonization was 184/675 (27.3%), 87/203 (42.8%), and 58/110 (52.7%) on D1, D5, and D8, respectively. Candida colonization dynamics were significantly associated with ICU type (odds ratio (OR) = 2.03, 95% CI 1.22–3.39, p = 0.007), respiratory infection (OR = 1.74, 95% CI 1.17–2.58, p = 0.006), hemodialysis (OR = 2.19, 95% CI 1.17–4.10, p = 0.014), COVID-19 (OR = 0.37, 95% CI 0.14–0.99, p = 0.048), and with a poor 3-month outcome (p = 0.008). Skin Candida spp. colonization can be an early warning tool to generate valuable insights into the epidemiology, risk factors, and survival rates of critically ill patients, and should be considered for epidemiological surveillance.
1. Introduction
A dramatic global increase in the incidence of fungal diseases has been documented in the past 20 years, which represents a public health problem with unique challenges due to the lack of sensitivity of diagnostic tools and the high morbidity and mortality caused by these infections [1,2]. Candida spp. are the third leading cause of nosocomial bloodstream infections, but rank first in terms of mortality [3]. Candida spp. are commensal yeasts that are part of the normal human skin and gut microbiota, and they are detectable in up to 60% of healthy individuals [4]. Invasive disease is usually a consequence of increased or abnormal colonization together with a local or generalized defect in host defenses [4,5,6].
ICU patients often have multiple risk factors for invasive candidiasis (IC), including prolonged hospitalization, use of broad-spectrum antibiotics, invasive procedures, and immunosuppression [7]. The diagnosis of IC can be challenging due to several factors, including the lack of pathognomonic symptoms, and the low sensitivity of diagnostic tests, displaying a variety of prediction rules for invasive Candida infection [8]. Candida multifocal colonization has been suggested as an independent risk factor for IC and helps to distinguish between high- and low-risk patients [9]. As a result, Candida colonization screening based on multiple body sites has been performed routinely in many ICUs, but the body sites surveyed vary considerably [10]. The skin microbiota of patients and healthcare workers can serve as reservoirs for potential pathogens, facilitating their transmission within the healthcare setting, namely C. parapsilosis and C. auris [11].
Although C. albicans is still considered the most common cause of colonization/infection, over the past decade, a change in favor of non-albicans Candida (NAC) has been confirmed in many studies worldwide, with regional heterogeneity [12]. In addition, the rise of fluconazole-resistant non-albicans Candida species, such as Candida auris [13], has caused great concern for healthcare across the globe, making the establishment of adequate empiric antifungal regimens difficult [14].
This study aimed to understand the dynamics of skin mycobiota colonization among ICU patients and evaluate the association between Candida colonization and the patient’s outcome.
2. Materials and Methods
2.1. Study Population
This study was conducted in three ICUs of two tertiary care hospitals in the metropolitan Lisbon area, Portugal. Hospital Professor Doutor Fernando Fonseca (FFH) is an 802-bed hospital with two ICUs (general and surgery) and Beatriz Ângelo Hospital (BAH) is a 424-bed hospital with one general ICU. Patients admitted to the ICU between January 2020 and December 2022 were enrolled in the study with the following exceptions: patients under 18 years of age, pregnant women, and mentally disabled individuals. The patient cohort met at least one of the following inclusion criteria: antimicrobial therapy in the last 48 h, presence of a central intravascular catheter, receiving parenteral nutrition, undergoing hemodialysis, receiving invasive assisted ventilation, having a bladder catheter, recent surgery, diagnosis of HIV/AIDS, other forms of immunodeficiency, hematological malignancies, other types of cancer, neutropenia (<500/mm3), anemia with hemoglobin levels below 10 mg/dL, and diabetes.
The study was approved by both Hospitals Hospital Ethics Committee. The sampling of each patient was performed by a non-invasive, bilateral axillary/inguinal combined swab. Collections were made upon the admission of patients to the ICU (D1) and continued during the ICU stay: 5th day (D5) and 8th day (D8), when applicable.
The sequential timing of collecting samples (D1, D5, and D8) during the ICU stay was undertaken with the objective of closely observing the influence of the ICU setting, providing insights into the progression of colonization and the effectiveness of intervention strategies [15,16].
2.2. Data Collected for Analysis
Demographic data, such as age, gender, history of travel abroad, underlying diseases [pulmonary infection, cardiovascular disease, gastrointestinal pathology, urinary tract infection, solid tumor, HIV/AIDS, hematological malignancy (lymphoma, leukemia, and another neoplasm), severe immunodeficiency, neutropenia, hemoglobin <10 g/dL, diabetes, and COVID-19], the history of antibiotic and antifungal therapy, and individual host risk factors related to the ICU setting [central intravascular catheter (CVC), invasive assisted ventilation, abdominal surgery, hemodialysis (HD), total parenteral nutrition (TPN), and vesical catheter] were recorded.
2.3. Surveillance Cultures and Identification
Swabs were collected in liquid Amies transport medium and 50 µL aliquots of the suspensions were spread directly onto appropriate culture media: Sabouraud Gentamicin Chloramphenicol 2 agar (SDA) (bioMérieux, Marcy l’Etoile, France) and a commercially Candida Chromogenic Medium (CHROMagar TM Candida, CHROMagar, Paris, France). Plates were incubated aerobically for 48 h, one set of plates at 25 °C and a second set at 37 °C, and the colony-forming units (CFUs) counted.
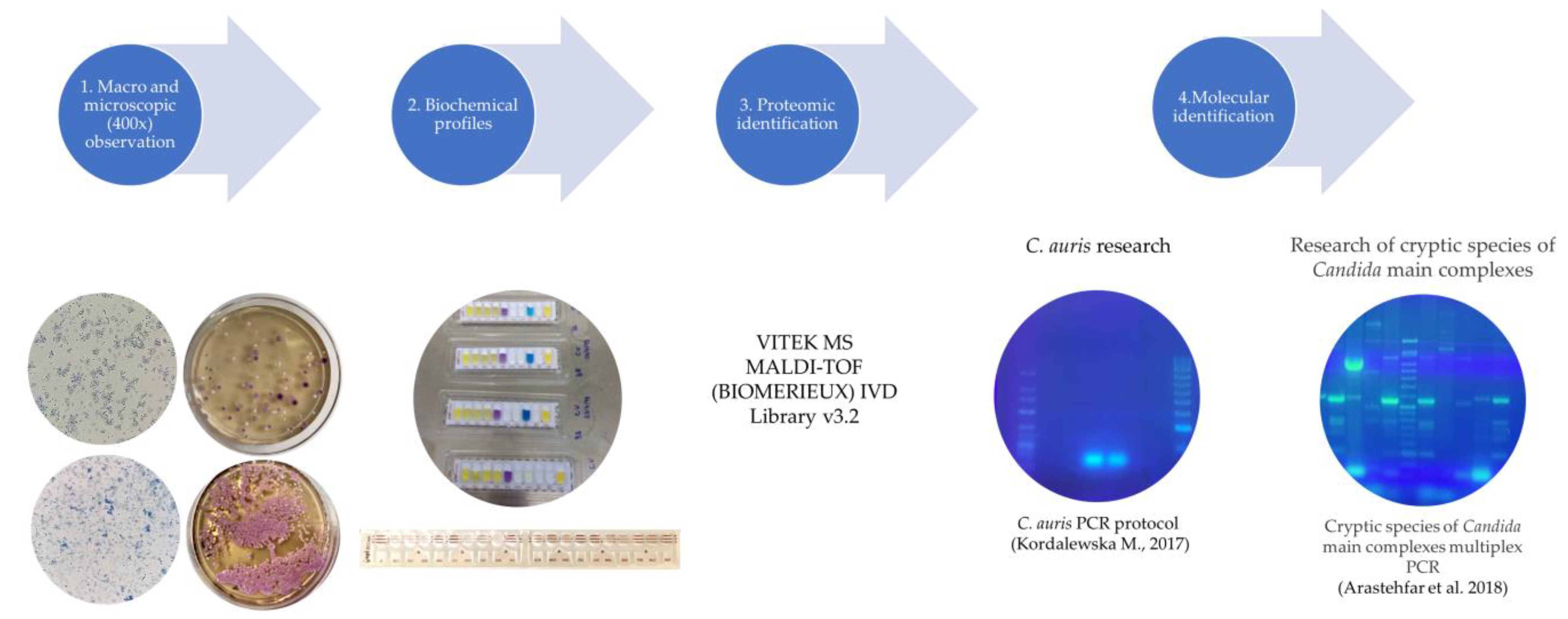
The presumptive identification of isolates was based on standard criteria of macroscopic and microscopic morphologies, growth temperature, biochemical profile of aerobic sugar assimilation, and appearance on chromogenic agar (Figure 1). All isolates were further processed for analysis with MALDI-TOF MS—VITEK MS (bioMérieux, Marcy l’Etoile, France) using VITEK MS v3.2 software [17]. All identifications displaying a single result with a confidence value of 99.9% were considered acceptable (Figure 1).
Figure 1.
Workflow of the identification procedures used with Candida spp. isolates [18,19].
All Candida isolates were also subjected to a C. auris-specific polymerase chain reaction (PCR) assay [18] and screened to identify any potential Candida cryptic species from the main complexes [19]. For this purpose, total DNA was extracted from the isolates using a NZYMicrobial gDNA Isolation Kit® (Nzytech, Lisboa, Portugal), according to the manufacturer’s instructions. Primers used in both PCR assays were previously described [15,16] and synthesized by Stab Vida, Portugal. PCRs were performed in a T100 thermal cycler (Bio-Rad Laboratories, Inc., Hercules, CA, USA). Amplified products were analyzed using 2% agarose gels stained with greensafe (Nzytech, Portugal) and visualized on a UV transilluminator with an exposure time of 4 s (Figure 1).
2.4. Quantification of Growth
Isolates recovered from swab samples were subjected to quantification based on the initial volume of sample spread. Counts were delineated to correspond with visual thresholds, ensuring practicality and accuracy in the assessment process. Colonization density was distributed into three groups: <100 CFU/mL; 100–1000 CFU/mL; and >1000 CFU/mL [20]. Namely, counts below 100 CFU/mL were categorized as a maximum of 5 CFUs, those between 100 and 1000 CFU/mL (maximum of 50 CFUs), and counts exceeding 1000 CFU/mL (>50 CFUs). High colonization was defined by the detection of more than 50 CFUs, as previously described [21]. Cultures were visually examined at 24 h and 48 h and an evaluation was performed independently by two different qualified investigators.
2.5. Statistical Analysis
A database was created with the demographic, clinical, and mycological characteristics of the study group, and data were analyzed using the IBM SPSS Statistics v. 29.0 (IBM Corp., Armonk, NY, USA) package program. An exploratory and descriptive analysis of the data was carried out to identify patterns for each variable. The categorical variables were expressed as frequencies and percentages. Comparisons of categorical variables were performed using the chi-squared test. Univariable and multivariable logistic regression models were performed to identify the predictors of Candida colonization at admission and during the whole length of the ICU stay. A p-value < 0.05 was taken to be statistically significant for all the above inferential analyses.
3. Results
3.1. Demographic and Clinical Characteristics of Patients
A total of 675 patients were enrolled during the two-year study period, 2020–2022, with 71, 64, and 540 patients attending, respectively, the general FFH ICU, surgical FFH ICU, and BAH ICU. From this cohort, all patients who met the inclusion criteria upon admission and remained hospitalized throughout the study period were followed up. A total of 203 patients were followed up with a second collection on day 5 (D5), and, from these, 89 patients were further sampled at day 8 (D8). Twenty-one patients were sampled at D1 and D8 (but not D5). Overall, 988 swab samples were collected: 675 on admission, 203 on D5, and 110 on D8.
A total of 401 patients (60.0%) were male and 566 (83.0%) were leucodermic with a median age of 67 years. A significant percentage had relevant underlying comorbidities at admission to each ICU, namely pulmonary infection for general FFH ICU; solid organ tumors and hematological neoplasms for surgical FFH ICU; and cardiovascular pathology, anemia, immunodeficiency, and COVID-19 for BAH ICU. Risks factors associated with the ICU setting are relevant for surgical the FFH ICU and include the presence of a central venous catheter, mechanical ventilation, and abdominal surgery. The use of antibiotics and antifungals can also be seen to be significant for the FFH ICU in this cohort. Antifungal use was for prophylaxis (fluconazole or echinocandins) and considered only in targeted patient groups, namely, patients with recent abdominal surgery and recurrent gastrointestinal perforations or diabetic (Table S1). The complete demographic and clinical characteristics of the study population is reported in Table 1.

Table 1.
Demographic and clinical characteristics of patients by hospital ICU 1.
3.2. Rates of Colonization
Fungal species were isolated from 184/675 (27.3%), 87/203 (42.9%), and 58/110 (52.7%) patients, respectively upon admission, D5 and D8. Increased colonization was observed in patients monitored during the whole length of stay.
The dynamics of colonization expressed in terms of variations with time of stay in ICU evidenced that, from the 203 patients with collection at D5, 74 (36.5%) were previously colonized at D1. For the 110 patients with collection at D8, 48/110 (43.6%) and 42/110 (38.2%) were already colonized, respectively, at D1 and D5 (Table 2). The overall colonization showed 232/675 (34.4%) colonized patients, whereby 48/313 (15.3%) became colonized in the ICU and 26/89 (29.2%) stayed colonized during the whole length of stay at the ICU (Table 2).

Table 2.
Dynamics of patient stay at ICU vs. colonization rate, from D1 to D8 1.
3.3. Burden of Colonization
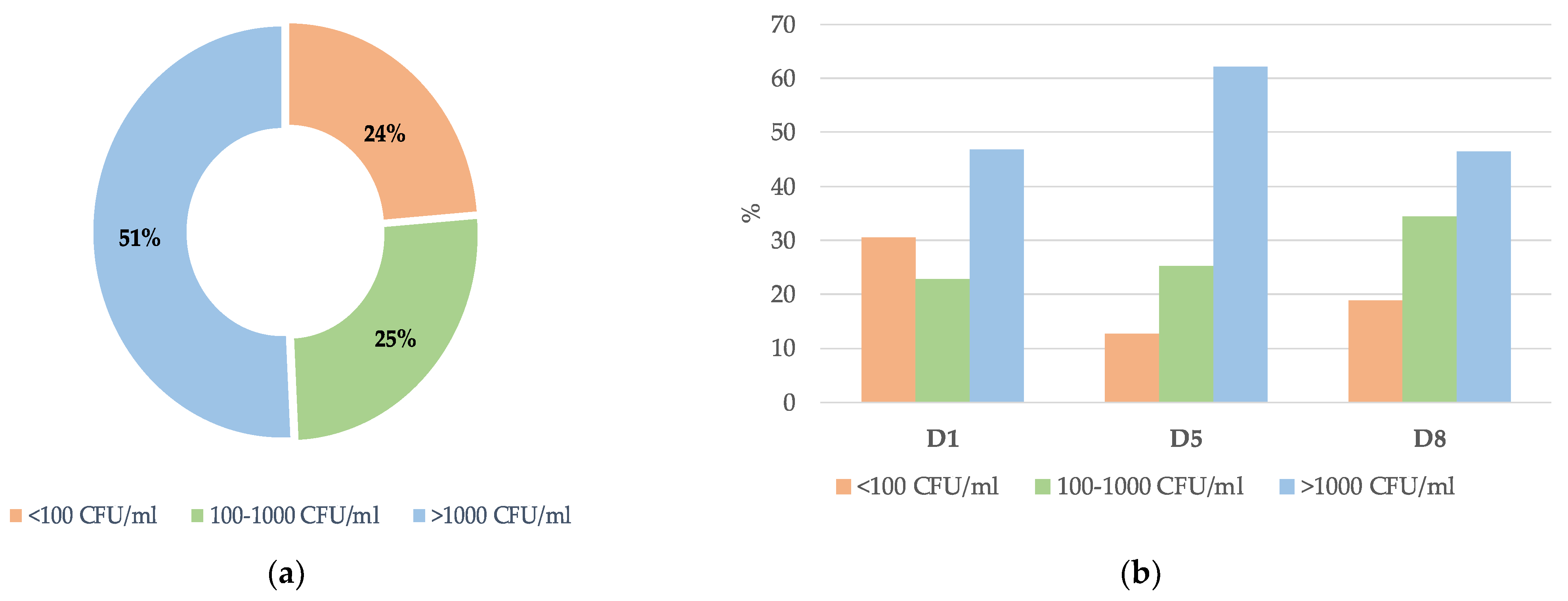
From the 329 positive samples for fungi isolation, 167 (50.8%), 84 (25.4%), and 78 (23.8%) presented, respectively, with a high fungal density (>1000 CFU/mL), average density (100–1000 CFU/mL), and low density (100 CFU/mL) (Figure 2a).
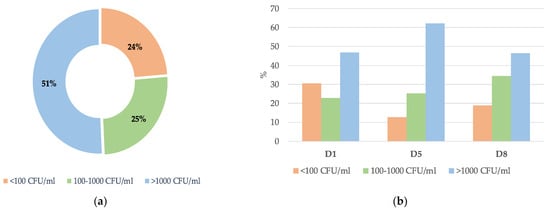
Figure 2.
Distribution of colonization density in the ICU: (a) overall; (b) on admission day (D1); day 5 (D5); and day 8 (D8).
The rate of colonization throughout the ICU stay reflected some variations depending on the level of CFU/mL. For patients with a rate of colonization <100 CFU/mL, there was a slight decrease after admission to the ICU and an increase after D5 of hospitalization (D1: 30.4%; D5: 12.6%; and D8: 19.0%). For intermediate colonization values in the range of 100–1000 CFU/mL, there was an increase along the prevalence points (D1: 22.8%; D5: 25.3%; and D8: 34.5%). The densely colonized samples (>1000 CFU/mL) gradually increased until D5 of hospitalization and by D8 showed similar colonization rates to D1 (D1: 46.7%; D5: 62.1%; and D8: 46.6%) (Figure 2b). However, no statistical differences were found at each of the collection points and the level of CFU/mL (D1, p = 0.223; D5, p = 0.939; and D8, p = 0.669).
3.4. Diversity of Colonizing Species
A total of 371 isolates were obtained from the 329 culture-positive samples. Most samples yielded single isolates, 286/329 (86.9%), and 43/329 (13.1%) samples yielded mixed cultures with two or more fungal species present. Mixed cultures were particularly observed at D1, with a decrease over the collection points [D1 (25/43, 58.1%); D5 (12/43, 27.9%); and D8 (6/43, 14.0%)].
Four genera of yeast-like fungi were found with a predominance of Candida spp., 355/371 (95.7%), followed by Rhodotorula spp., 9/371 (2.4%), Trichosporon spp., 6/371 (1.6%), and Saccharomyces spp., 1/371 (0.3%).
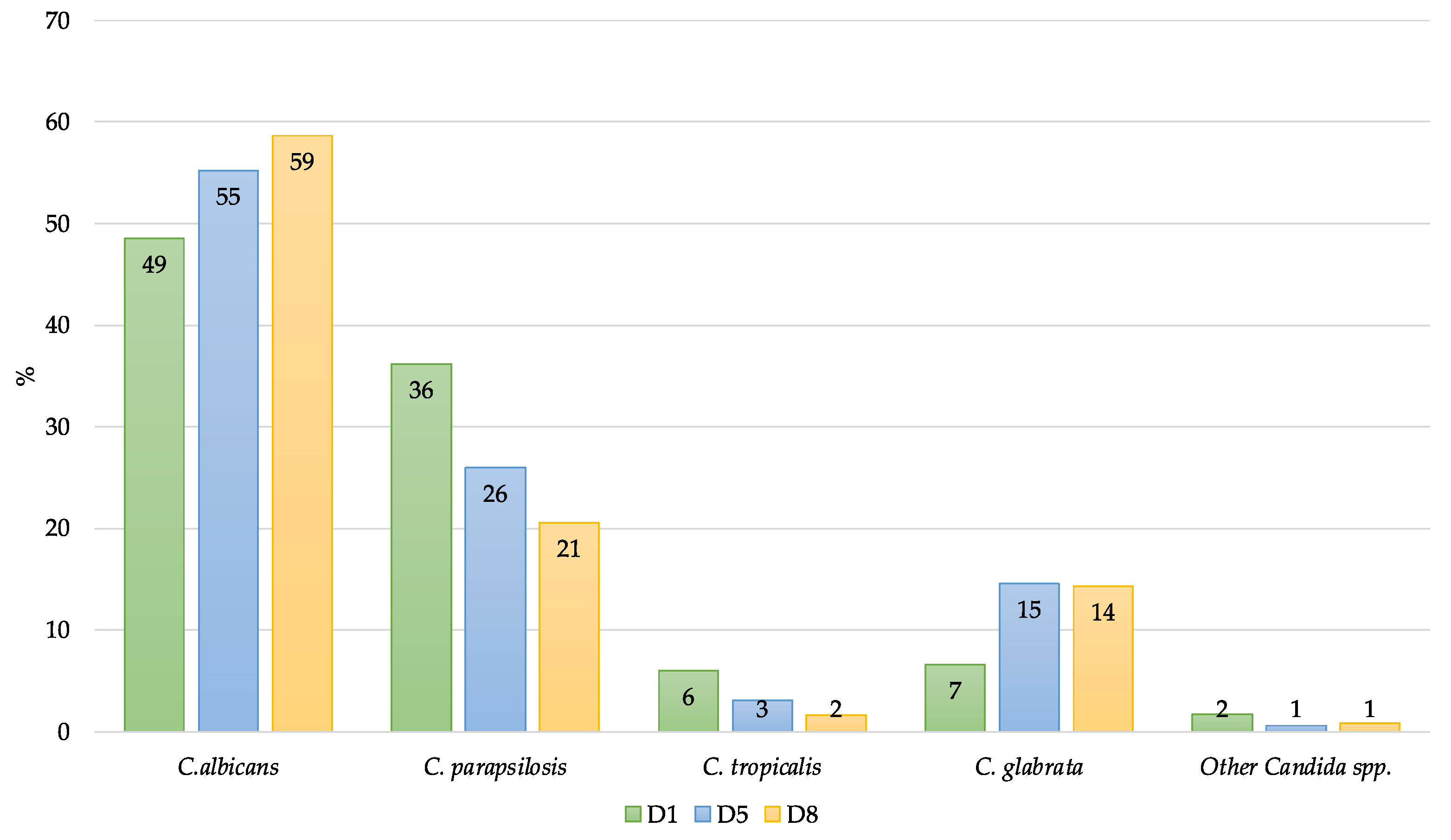
After identification to the species level, eight Candida species were identified: C. albicans sensu stricto (n = 185), C. parapsilosis complex (n = 112) [C. parapsilosis sensu stricto (n = 109), C. orthopsilosis (n = 2), C. metapsilosis (n = 1)], Nakaseomyces glabrata (Candida glabrata) sensu stricto (n = 36), C. tropicalis (n = 15), Clavispora lusitaniae (Candida lusitaniae) (n = 4), and Meyerozyma guilliermondii (Candida guilliermondii) (n = 3). C. auris or other emerging Candida species, like the C. haemulonii complex, C. rugosa, or C. vulturna, were not detected. C. albicans remained the most isolated species with 185/355 (52.1%). The distribution of Candida spp. Over the collection points evidenced a relevant colonization by C. albicans in the ICU setting (D5 and D8) at the expense of non-albicans species (Figure 3).
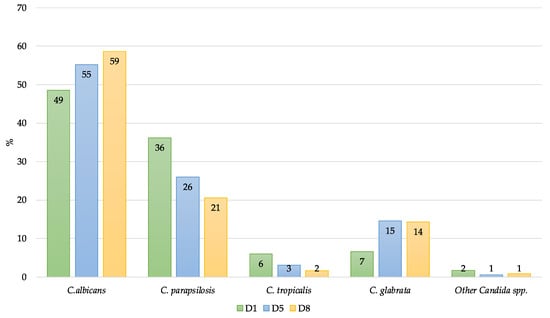
Figure 3.
Diversity of Candida spp. during the whole length of ICU stay (D1, D5, and D8).
3.5. Demographics, Clinical Characteristics, and Outcomes of Patients Colonized
We observed that gender, race, and patient age did not pose a positive impact on the fungal colonization density rates. As summarized in Table 3, at ICU admission, the most susceptible patients to colonization were admitted to FFH general ICU, accounting for 29/71 (40.8%) (p = 0.007). Importantly, among the various relevant risk factors, which significantly influenced the incidence of Candida colonization and possible infection, pulmonary infection, the presence of CVC, mechanical ventilation, and dialysis were found to be statistically significant (p < 0.05) (Table 3). Other risk factors did not show significant differences (p > 0.05), including urinary catheterization, abdominal surgery, total parenteral nutrition, neutropenia, cancer (leukemia and solid tumor), anemia, diabetes mellitus, and treatment with antibiotics and antifungals (Table 3).

Table 3.
Univariate risk evaluation toward patient colonization at admission to the ICU *.
Considering the univariate risk evaluation for permanent colonization during the whole length of stay at the ICU (D1–D8), no significant association was observed for colonization in both tertiary hospitals, including the ICU unit (Table S2).
Multivariate analysis was performed to detect potential risk factors associated with fungal colonization. Subjacent pulmonary infection and being on dialysis had statistical significance as increased risk predictors toward Candida colonization (OR = 1.74, CI 95% 1.17–2.58, p = 0.006 and OR = 2.19, 95% CI 1.17–4.10, p = 0.014, respectively), as did the presence of COVID-19 (OD = 0.37, 95% CI 0.14–0.99, p = 0.048), but in this case, lowering the risk toward colonization (Table 4).

Table 4.
Multivariate risk evaluation towards patient colonization at admission to the ICU *.
Regarding patient outcomes, the three-month survival rate was determined at the BAH ICU for a one-year collection period (n = 497), between September 2021 and September 2022. The fatality rate was 161/497 (32.4%). No statistically significant associations were identified between risk factors for colonization already identified in this study or other risk factors related to underlying conditions or the ICU. Fatality was significantly higher in patients colonized at ICU admission (p = 0.010) and with a longer length of stay in the ICU (p = 0.006). The results show that being colonized with C. albicans is associated with a poor outcome (p = 0.042). However, the analysis did not reveal a significant association between colonization density and survival rates (p = 0.132) (Table 5).

Table 5.
Survival risk evaluation (3-month outcome) for colonization during the whole length of stay at the Beatriz Ângelo Hospital (BAH) ICU (D1–D8) 1.
From the one-year BAH cohort, it is worth mentioning that 17 patients were colonized during the whole length of stay, and 8/17 (47.0%) had a poor 3-month outcome.
4. Discussion
There has been a significant increase in the incidence of invasive fungal infections worldwide, especially in patients admitted to intensive care units [3]. Among different fungal pathogens, colonization by Candida species is very frequent in ICU patients and a necessary first step in the pathogenesis of systemic infection.
Collecting samples upon admission provided a baseline understanding of the initial Candida colonization status of patients entering the ICU. This helped establish a starting point for comparison with subsequent samples [16]. The one-week mark after ICU admission (D5 and D8) allowed us to access the effectiveness of interventions implemented during the ICU stay on Candida colonization.
The prevalence values of Candida colonization were 27.3%, 42.9%, and 52.7%, respectively, upon admission, D5 and D8. During the whole length of ICU stay, 15.3% more of the patients evidenced newly acquired fungal colonization. Out of the 89 patients who underwent sampling at the three specified time points, 29.2% were consistently positive for fungi, which demonstrates the importance of the ICU environment in Candida colonization.
Our results are consistent with a progressive increase in Candida colonization in the ICUs. Although colonization on admission may reflect the previous colonization of patients, it increased during the study period. Prevalence reported by other studies over the last decade point toward increasing Candida prevalence, but these studies observed different rates of colonization. Studies by Ahmad et al., Charles et al., and León et al. showed higher proportions of patients, respectively, 45.6%, 39.1%, and 52.2%, already colonized at the time of admission to the ICU [22,23,24]. The overall prevalence in our study (232/675, 34.4%) is consistent with a previous observational study in a surgical and trauma ICU in a university hospital [20]. However, comparing colonization rates with previous studies presents a challenge because those studies focused on determining Candida colonization rates in different types of septic samples just on ICU admission.
To the authors’ knowledge, this is the first Portuguese multicenter observational and descriptive study that provides insights into Candida colonization and predictive risk factors in an ICU setting. Previous studies conducted in Portugal have predominantly focused on cases of candidemia, often being retrospective in nature [25,26,27]. Nevertheless, comparing the overall distribution of Candida species with previous Portuguese candidemia studies, a steady pattern of Candida species ranks yielded by Portuguese ICU patients was observed [28]. Namely, a prevalence of C. albicans alongside the occurrence of cryptic species only from the C. parapsilosis complex [26,28,29].
Colonization densities were found to be mostly high in our study (>1000 CFU/mL) (167/329; 50.8%), but did not change significantly over the first 8 days of stay in intensive care unit patients, as already described by other authors [22]. This might be due to a short time of surveillance, as other studies evidenced that patients colonized with Candida had a significantly longer length of ICU and hospital stays [30].
Our results suggest that the risk of being colonized is dependent on the healthcare unit. The probability of a patient being colonized in the general FFH ICU is significant, compared to the other ICUs under study (p = 0.004). It is noteworthy that the assessed patient populations are very heterogeneous with a significant association within clinical characteristics between ICUs. Regarding the colonization results that reflect the colonization acquired in each ICU (collections on D5 and D8), the rate did not differ significantly between the ICUs. These rates for Candida colonization and respective density are suggestive of association with increasing exposure to risk factors and the local unit.
Candida colonization and infection are almost indistinguishable in the natural history of candidemia, and multiple-site colonization by Candida species is commonly recognized as a major risk factor for invasive fungal infection in critically ill patients [12,16]. Several risk factors have been associated with Candida colonization, namely, extremes of age (low-birthweight newborns and the elderly), hematological neoplasms and other cancers, chemotherapy, neutropenia, digestive tract mucositis, intravenous catheters and/or long-term treatment with corticosteroids, and even antimicrobials, including antifungal drugs [31].
For our cohort of patients, logistic regression analysis revealed significant independent predictors of Candida colonization in the ICU and identified three risk factors mostly related to medical interventions during intensive care or to comorbid conditions, namely an underlying respiratory infection and being under hemodialysis. These results agree with previous studies, considering respiratory disease as one of the best risk predictors for Candida infection development [7,32,33].
Patients with coronavirus disease 2019 (COVID-19) were also significantly associated but, contrary to our expectations, COVID-19 had a protective effect against the development of Candida colonization. COVID-19 patients in the ICU receive intensive medical care and these practices can help prevent Candida colonization from the skin mycobiome or the ICU environment. It is described that COVID-19 patients present multiple reasons to be at a higher risk for developing candidemia due to the need for intensive care management [34,35]. Our results, showing different but interesting effects of COVID-19 on critically ill patients, should be confirmed by further studies.
It is noteworthy that, for pointed risk factors, all ORs were small, which is in line with a recent meta-analysis that identified 29 risk factors for invasive Candida infection in ICUs from 34 studies, with most ORs small [7].
No statistically significant association was found in our study for risk factors predicting Candida colonization for all lengths of stay in the ICU. The results obtained are not in line with previously published studies, since there was no statistically significant association between Candida colonization and the presence of risk factors, such as diabetes, abdominal surgery, HIV, hematological neoplasms, solid tumors, parental nutrition, abdominal surgery, and use of extended-spectrum antibiotics [7,35,36]. This discrepancy may be due to the biological sample used in this research, combined axilla/groin swabs, while other studies used blood samples.
Our findings for 3-month mortality for the ICU under evaluation suggested a statistically significant association with the length of ICU stay and colonization by C. albicans, which is consistent with the observations of other studies that validated the incidence value of Candida colonization [16,33,37,38,39]. C. albicans is the main cause of IC worldwide, except in India [40], and over the infection process uses multiple virulence factors. Although C. albicans shows a good susceptibility profile to antifungal drugs, the in vivo response is greatly hampered by the presence of biofilm. Nevertheless, its persistence of colonization over time may be related to its potent infective potential [41]. However, there is a limitation in our study as we do not know if IC/candidemia was the sole reason that contributed or not to death in our patient cohort. With the clinical data provided, we do not have enough information to assume that colonization does or does not increase the possibility of developing candidemia and invasive infection, but we found a significant association between a poor prognosis and Candida colonization.
When the number of Candida CFUs present in patient samples was monitored over time to assess the extent of colonization, no significant association with a poor 3-month outcome was found. While high CFU counts may indicate increased colonization, it seems that they do not necessarily associate directly with the clinical outcome, as other factors, such as host immunity and underlying medical conditions, also play a role. Nevertheless, our results from the burden of colonization (D1 to D8) show that healthcare units should consider the implementation of infection control measures to mitigate the risks associated with Candida colonization.
Clinicians and healthcare systems can address the progressive increase in Candida colonization in ICUs by employing several key strategies. Firstly, they should prioritize a regular analysis of trends and patterns to detect emerging issues early, allowing for timely intervention. Rapid diagnostic tests should be utilized to promptly identify Candida colonization in ICU patients, enabling a swift initiation of appropriate management. Additionally, infection control practices must be strengthened, particularly emphasizing hand hygiene and environmental cleaning. Special attention should be paid to patients undergoing hemodialysis and those with respiratory infections, with tailored measures implemented to mitigate the risk of Candida colonization and transmission in these populations. By implementing these measures, clinicians and healthcare systems can effectively combat the rising prevalence of Candida colonization in ICUs and improve patient outcomes.
We showed that monitoring Candida CFU colonization burden in the ICUs, along with other relevant clinical and epidemiological data, can provide valuable insights into the risk factors and dynamics of Candida colonization in the hospital setting. In view of the results, it is possible to consider skin Candida colonization as an early warning tool in critically ill patients and can be considered the site of choice for epidemiological surveillance of critically ill patients.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jof10060378/s1. Table S1: Demographic and clinical characteristics of patients under prophylactic antifungal therapy by hospital ICU. Table S2: Univariate risk evaluation for permanent colonization during the whole length of stay at the ICU (D1–D8).
Author Contributions
Conceptualization, T.N., J.I., P.D., P.P., C.T., L.P. and H.B.; Project administration and funding acquisition, H.B.; investigation, T.N., D.G., C.T., J.I. and H.B.; formal analysis, L.P.; supervision, J.I. and H.B.; writing—original draft, T.N.; writing—review and editing, T.N., J.I., L.P., C.T. and H.B. All authors have read and agreed to the published version of the manuscript.
Funding
The authors thank FCT/MCTES for the financial support to CiiEM (10.54499/UIDB/04585/2020) through national funds.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee of Hospital Prof. Doutor Fernando Fonseca (59/2019, 13 November 2019) and the Institutional Ethics Committee of Hospital Beatriz Ângelo (3655/2021, 21 July 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Materials, further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Lamoth, F.; Lewis, R.E.; Kontoyiannis, D.P. Role and Interpretation of Antifungal Susceptibility Testing for the Management of Invasive Fungal Infections. J. Fungi 2020, 7, 17. [Google Scholar] [CrossRef]
- Lamoth, F. Novel Therapeutic Approaches to Invasive Candidiasis: Considerations for the Clinician. Infect. Drug Resist 2023, 16, 1087–1097. [Google Scholar] [CrossRef] [PubMed]
- Poissy, J.; Rouzé, A.; Cornu, M.; Nseir, S.; Sendid, B. The Changing Landscape of Invasive Fungal Infections in ICUs: A Need for Risk Stratification to Better Target Antifungal Drugs and the Threat of Resistance. J. Fungi 2022, 8, 946. [Google Scholar] [CrossRef]
- Pappas, P.G.; Lionakis, M.S.; Arendrup, M.C.; Ostrosky-Zeichner, L.; Kullberg, B.J. Invasive candidiasis. Nat. Rev. Dis. Primers 2018, 4, 18026. [Google Scholar] [CrossRef]
- Donnelly, J.P.; Chen, S.C.; Kauffman, C.A.; Steinbach, W.J.; Baddley, J.W.; Verweij, P.E.; Clancy, C.J.; Wingard, J.R.; Lockhart, S.R.; Groll, A.H.; et al. Revision and Update of the Consensus Definitions of Invasive Fungal Disease From the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clin. Infect. Dis. 2020, 71, 1367–1376. [Google Scholar] [CrossRef]
- Alenazy, H.; Alghamdi, A.; Pinto, R.; Daneman, N. Candida colonization as a predictor of invasive candidiasis in non-neutropenic ICU patients with sepsis: A systematic review and meta-analysis. Int. J. Infect. Dis. 2021, 102, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Thomas-Rüddel, D.O.; Schlattmann, P.; Pletz, M.; Kurzai, O.; Bloos, F. Risk Factors for Invasive Candida Infection in Critically Ill Patients: A Systematic Review and Meta-analysis. Chest 2022, 161, 345–355. [Google Scholar] [CrossRef]
- Fang, W.; Wu, J.; Cheng, M.; Zhu, X.; Du, M.; Chen, C.; Liao, W.; Zhi, K.; Pan, W. Diagnosis of invasive fungal infections: Challenges and recent developments. J. Biomed. Sci. 2023, 30, 42. [Google Scholar] [CrossRef]
- Das, S.; Tigga, R.; Rai, G.; Singh, P.K.; Datt, S.; Tyagi, A.; Singh, N.P. Candida auris colonization in an immunocompetent patient: A new threat in medical ICU. Med. Mycol. Case Rep. 2018, 21, 54–56. [Google Scholar] [CrossRef]
- Li, Z.; Jiang, C.; Dong, D.; Zhang, L.; Tian, Y.; Ni, Q.; Mao, E.; Peng, Y. The Correlation Between Candida Colonization of Distinct Body Sites and Invasive Candidiasis in Emergency Intensive Care Units: Statistical and Molecular Biological Analysis. Mycopathologia 2016, 181, 475–484. [Google Scholar] [CrossRef]
- Sayeed, M.A.; Farooqi, J.; Jabeen, K.; Mahmood, S.F. Comparison of risk factors and outcomes of Candida auris candidemia with non- Candida auris candidemia: A retrospective study from Pakistan. Med. Mycol. 2020, 58, 721–729. [Google Scholar] [CrossRef] [PubMed]
- Soulountsi, V.; Schizodimos, T.; Kotoulas, S.C. Deciphering the epidemiology of invasive candidiasis in the intensive care unit: Is it possible? Infection 2021, 49, 1107–1131. [Google Scholar] [CrossRef] [PubMed]
- Martins-Santana, L.; Rezende, C.P.; Rossi, A.; Martinez-Rossi, N.M.; Almeida, F. Addressing Microbial Resistance Worldwide: Challenges over Controlling Life-Threatening Fungal Infections. Pathogens 2023, 12, 293. [Google Scholar] [CrossRef] [PubMed]
- Soriano, A.; Honore, P.M.; Puerta-Alcalde, P.; Garcia-Vidal, C.; Pagotto, A.; Gonçalves-Bradley, D.C.; Verweij, P.E. Invasive candidiasis: Current clinical challenges and unmet needs in adult populations. J. Antimicrob. Chemother. 2023, 78, 1569–1585. [Google Scholar] [CrossRef] [PubMed]
- Lau, A.F.; Kabir, M.; Chen, S.C.; Playford, E.G.; Marriott, D.J.; Jones, M.; Lipman, J.; McBryde, E.; Gottlieb, T.; Cheung, W.; et al. Candida colonization as a risk marker for invasive candidiasis in mixed medical-surgical intensive care units: Development and evaluation of a simple, standard protocol. J. Clin. Microbiol. 2015, 53, 1324–1330. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, D.M.; Beyda, N.D.; Asuphon, O.; Alam, M.J.; Garey, K.W. Host factors and clinical outcomes of Candida colonization in critically ill patients. Mycopathologia 2015, 179, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Sarvestani, H.K.; Ramandi, A.; Getso, M.I.; Razavyoon, T.; Javidnia, J.; Golrizi, M.B.; Saboor-Yaraghi, A.A.; Ansari, S. Mass spectrometry in research laboratories and clinical diagnostic: A new era in medical mycology. Braz. J. Microbiol. 2022, 53, 689–707. [Google Scholar] [CrossRef]
- Kordalewska, M.; Zhao, Y.; Lockhart, S.R.; Chowdhary, A.; Berrio, I.; Perlin, D.S. Rapid and Accurate Molecular Identification of the Emerging Multidrug-Resistant Pathogen Candida auris. J. Clin. Microbiol. 2017, 55, 2445–2452. [Google Scholar] [CrossRef] [PubMed]
- Arastehfar, A.; Fang, W.; Pan, W.; Liao, W.; Yan, L.; Boekhout, T. Identification of nine cryptic species of Candida albicans, C. glabrata, and C. parapsilosis complexes using one-step multiplex PCR. BMC Infect. Dis. 2018, 18, 480. [Google Scholar] [CrossRef]
- Eggimann, P.; Pittet, D. Candida colonization index and subsequent infection in critically ill surgical patients: 20 years later. Intensiv. Care Med. 2014, 40, 1429–1448. [Google Scholar] [CrossRef]
- Fanello, S.; Bouchara, J.P.; Sauteron, M.; Delbos, V.; Parot, E.; Marot-Leblond, A.; Moalic, E.; Flohicc, A.M.L.; Brangerd, B. Predictive value of oral colonization by Candida yeasts for the onset of a nosocomial infection in elderly hospitalized patients. J. Med. Microbiol. 2006, 55, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.; Khan, Z.; Mustafa, A.S.; Khan, Z.U. Epidemiology of Candida colonization in an intensive care unit of a teaching hospital in Kuwait. Med. Mycol. 2003, 41, 487–493. [Google Scholar] [CrossRef] [PubMed]
- Charles, P.E.; Dalle, F.; Aube, H.; Doise, J.M.; Quenot, J.P.; Aho, L.S.; Chavanet, P.; Blettery, B. Candida spp. colonization significance in critically ill medical patients: A prospective study. Intensiv. Care Med. 2005, 31, 393–400. [Google Scholar] [CrossRef] [PubMed]
- León, C.; Alvarez-Lerma, F.; Ruiz-Santana, S.; León, M.A.; Nolla, J.; Jordá, R.; Saavedra, P.; Palomar, M.; Group, E.S. Fungal colonization and/or infection in non-neutropenic critically ill patients: Results of the EPCAN observational study. Eur. J. Clin. Microbiol. Infect. Dis. 2009, 28, 233–242. [Google Scholar] [CrossRef] [PubMed]
- Pinto-Magalhães, S.; Martins, A.; Lacerda, S.; Filipe, R.; Prista-Leão, B.; Pinheiro, D.; Silva-Pinto, A.; Santos, L. Candidemia in a Portuguese tertiary care hospital: Analysis of a 2-year period. J. Mycol. Med. 2019, 29, 320–324. [Google Scholar] [CrossRef] [PubMed]
- Boattini, M.; Pinto, M.F.; Christaki, E.; Fasciana, T.; Falces-Romero, I.; Tofarides, A.; Bianco, G.; Cendejas-Bueno, E.; Tricoli, M.R.; Tsiolakkis, G.; et al. Multicentre Surveillance of Candida Species from Blood Cultures during the SARS-CoV-2 Pandemic in Southern Europe (CANCoVEU Project). Microorganisms 2023, 11, 560. [Google Scholar] [CrossRef] [PubMed]
- Aydın, S.; Mert, A.; Yılmaz, M.; Al Maslamani, M.; Rahimi, B.A.; Ayoade, F.; El-Kholy, A.; Belitova, M.; Sengel, B.E.; Jalal, S.; et al. Understanding clinical outcomes and factors influencing mortality in intensive care unit patients with COVID-19-associated candidemia. Mycoses 2024, 67, e13687. [Google Scholar] [CrossRef] [PubMed]
- Faria-Ramos, I.; Neves-Maia, J.; Ricardo, E.; Santos-Antunes, J.; Silva, A.T.; Costa-de-Oliveira, S.; Cantón, E.; Rodrigues, A.G.; Pina-Vaz, C. Species distribution and in vitro antifungal susceptibility profiles of yeast isolates from invasive infections during a Portuguese multicenter survey. Eur. J. Clin. Microbiol. Infect. Dis. 2014, 33, 2241–2247. [Google Scholar] [CrossRef] [PubMed]
- Afzal, A.; Ahmed, A.; Baronia, A.; Yadav, R.; Sharma, P.; Marak, R. Epidemiology of Candida colonization and infection in medical surgical intensive care unit of a tertiary care hospital. J. Microbiol. Infect. Dis. 2018, 8, 147–152. [Google Scholar] [CrossRef]
- Ferreira, D.; Grenouillet, F.; Blasco, G.; Samain, E.; Hénon, T.; Dussaucy, A.; Millon, L.; Mercier, M.; Pili-Floury, S. Outcomes associated with routine systemic antifungal therapy in critically ill patients with Candida colonization. Intensiv. Care Med. 2015, 41, 1077–1088. [Google Scholar] [CrossRef]
- Caggiano, G.; Puntillo, F.; Coretti, C.; Giglio, M.; Alicino, I.; Manca, F.; Bruno, F.; Montagna, M.T. Candida colonization index in patients admitted to an ICU. Int. J. Mol. Sci. 2011, 12, 7038–7047. [Google Scholar] [CrossRef] [PubMed]
- Quindós, G.; Marcos-Arias, C.; San-Millán, R.; Mateo, E.; Eraso, E. The continuous changes in the aetiology and epidemiology of invasive candidiasis: From familiar Candida albicans to multiresistant Candida auris. Int. Microbiol. 2018, 21, 107–119. [Google Scholar] [CrossRef] [PubMed]
- Chakraborti, A.; Jaiswal, A.; Verma, P.K.; Singhal, R. A Prospective Study of Fungal Colonization and Invasive Fungal Disease in Long-Term Mechanically Ventilated Patients in a Respiratory Intensive Care Unit. Indian J. Crit. Care Med. 2018, 22, 597–601. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.; Qi, M.; Hu, Y.; Yu, M.; Liang, Z. The impact of Candida spp airway colonization on clinical outcomes in patients with ventilator-associated pneumonia: A systematic review and meta-analysis. Am. J. Infect. Control 2020, 48, 695–701. [Google Scholar] [CrossRef] [PubMed]
- Colaneri, M.; Giusti, E.M.; Genovese, C.; Galli, L.; Lombardi, A.; Gori, A. Mortality of Patients With Candidemia and COVID-19: A Systematic Review With Meta-analysis. Open Forum Infect. Dis. 2023, 10, ofad358. [Google Scholar] [CrossRef] [PubMed]
- Kayaaslan, B.; Kaya Kalem, A.; Asilturk, D.; Kaplan, B.; Dönertas, G.; Hasanoglu, I.; Eser, F.; Korkmazer, R.; Oktay, Z.; Ozkocak Turan, I.; et al. Incidence and risk factors for COVID-19 associated candidemia (CAC) in ICU patients. Mycoses 2022, 65, 508–516. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez, D.; Weinstock, A.; Antharam, V.C.; Gu, H.; Jasbi, P.; Shi, X.; Dirks, B.; Krajmalnik-Brown, R.; Maldonado, J.; Guinan, J.; et al. Antibiotic-induced gut metabolome and microbiome alterations increase the susceptibility to Candida albicans colonization in the gastrointestinal tract. FEMS Microbiol. Ecol. 2020, 96, fiz187. [Google Scholar] [CrossRef] [PubMed]
- Lagunes, L.; Rello, J. Invasive candidiasis: From mycobiome to infection, therapy, and prevention. Eur. J. Clin. Microbiol. Infect. Dis. 2016, 35, 1221–1226. [Google Scholar] [CrossRef] [PubMed]
- Day, A.W.; Kumamoto, C.A. Interplay between host and Candida albicans during commensal gut colonization. PLoS Pathog. 2023, 19, e1011607. [Google Scholar] [CrossRef]
- Sharma, M.; Chakrabarti, A. Candidiasis and Other Emerging Yeasts. Curr. Fungal. Infect. Rep. 2023, 17, 15–24. [Google Scholar] [CrossRef]
- Macias-Paz, I.U.; Pérez-Hernández, S.; Tavera-Tapia, A.; Luna-Arias, J.P.; Guerra-Cárdenas, J.E.; Reyna-Beltrán, E. Candida albicans the main opportunistic pathogenic fungus in humans. Rev. Argent. Microbiol. 2022, 55, 189–198. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).