Malignant Keratitis Caused by a Highly-Resistant Strain of Fusarium Tonkinense from the Fusarium Solani Complex
Abstract
1. Introduction
2. Case Report
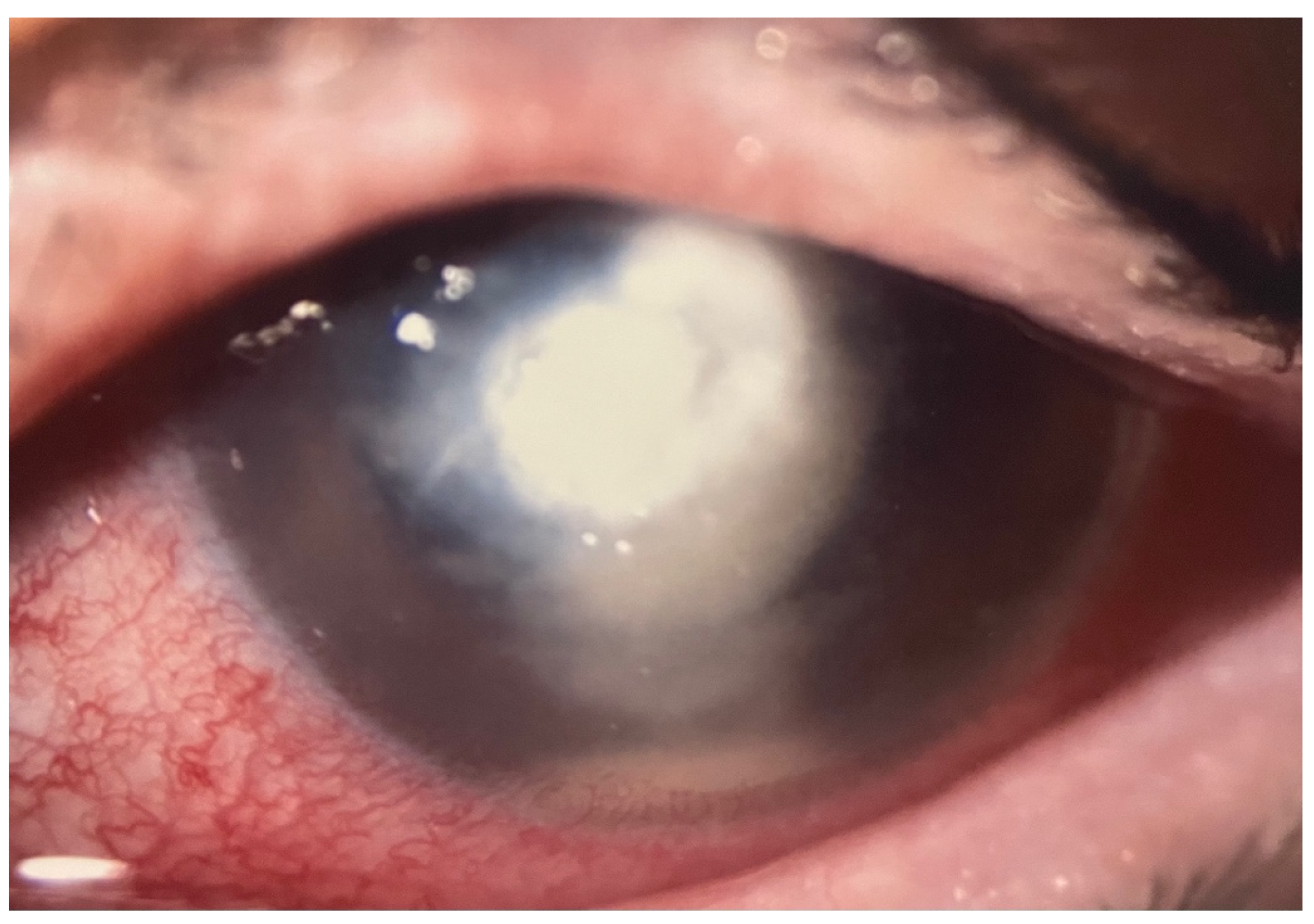
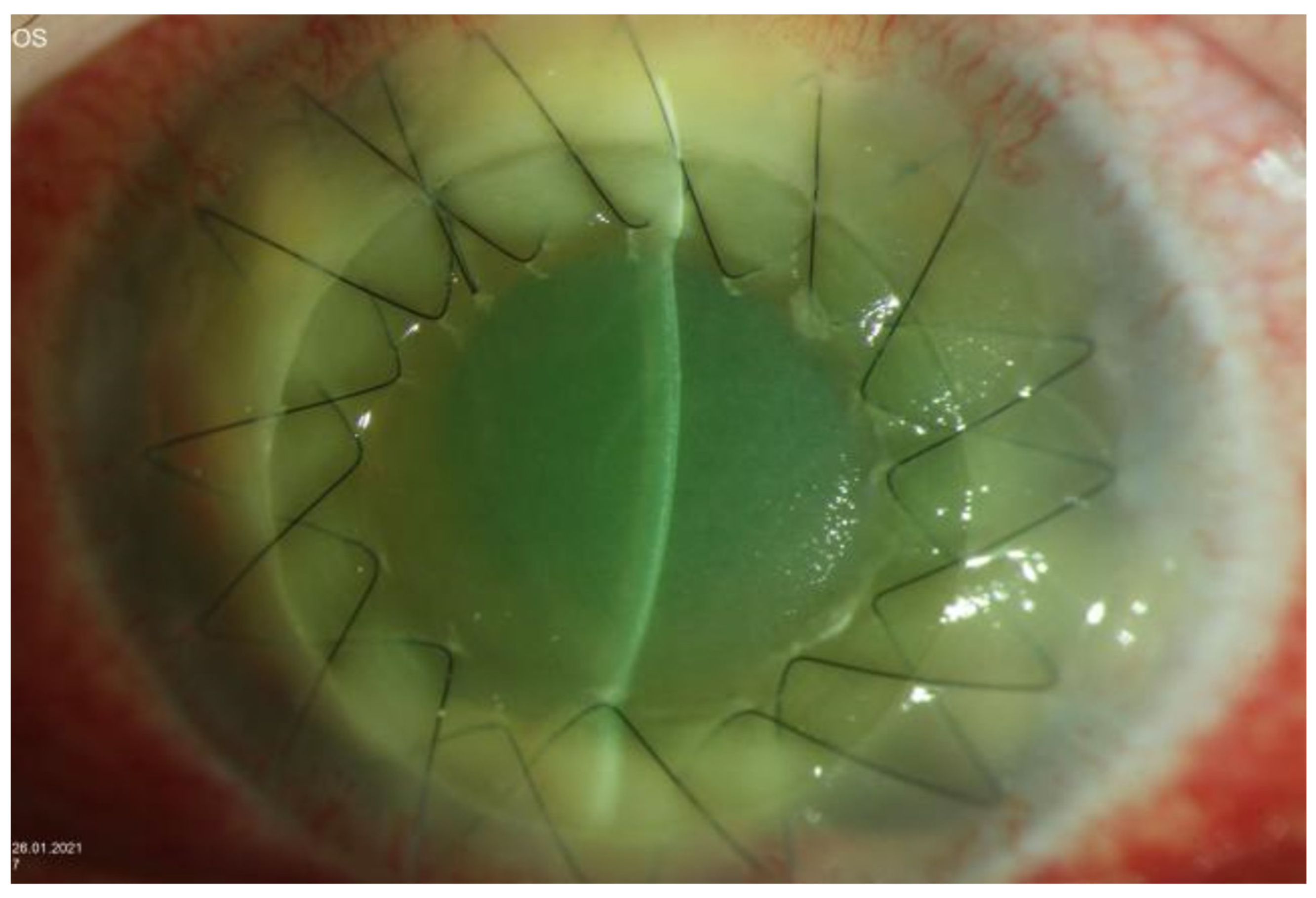
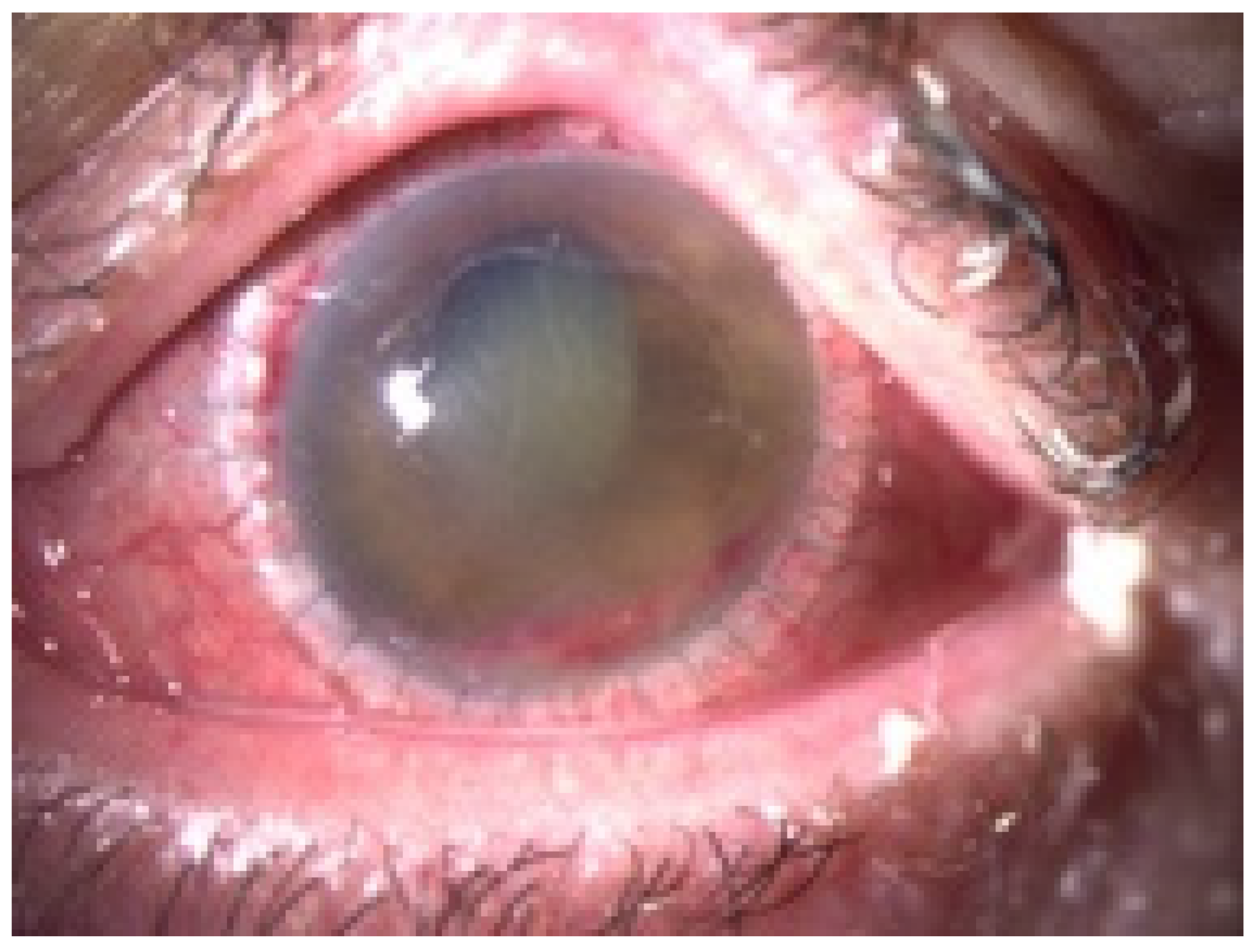
2.1. Clinical Presentation
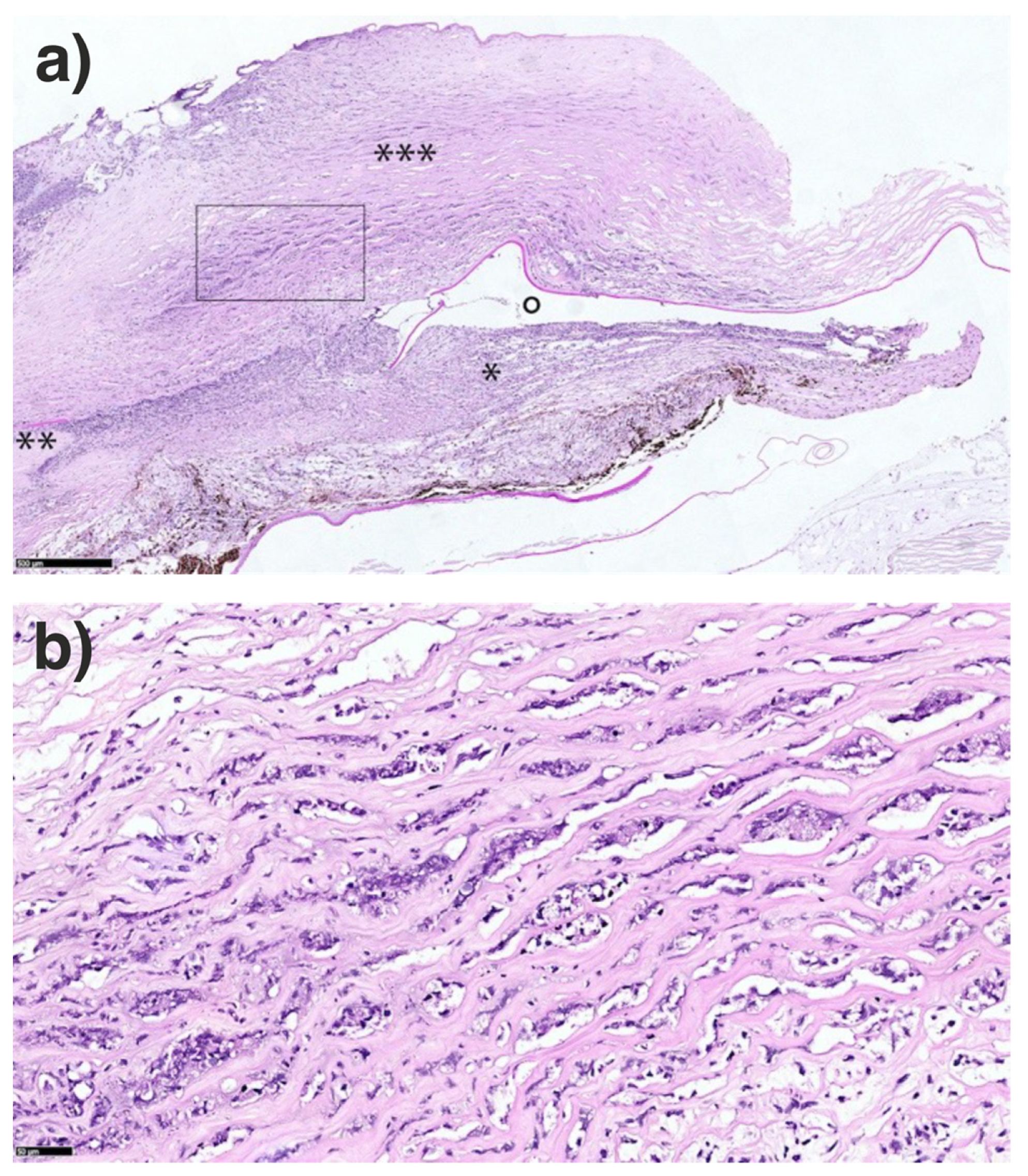
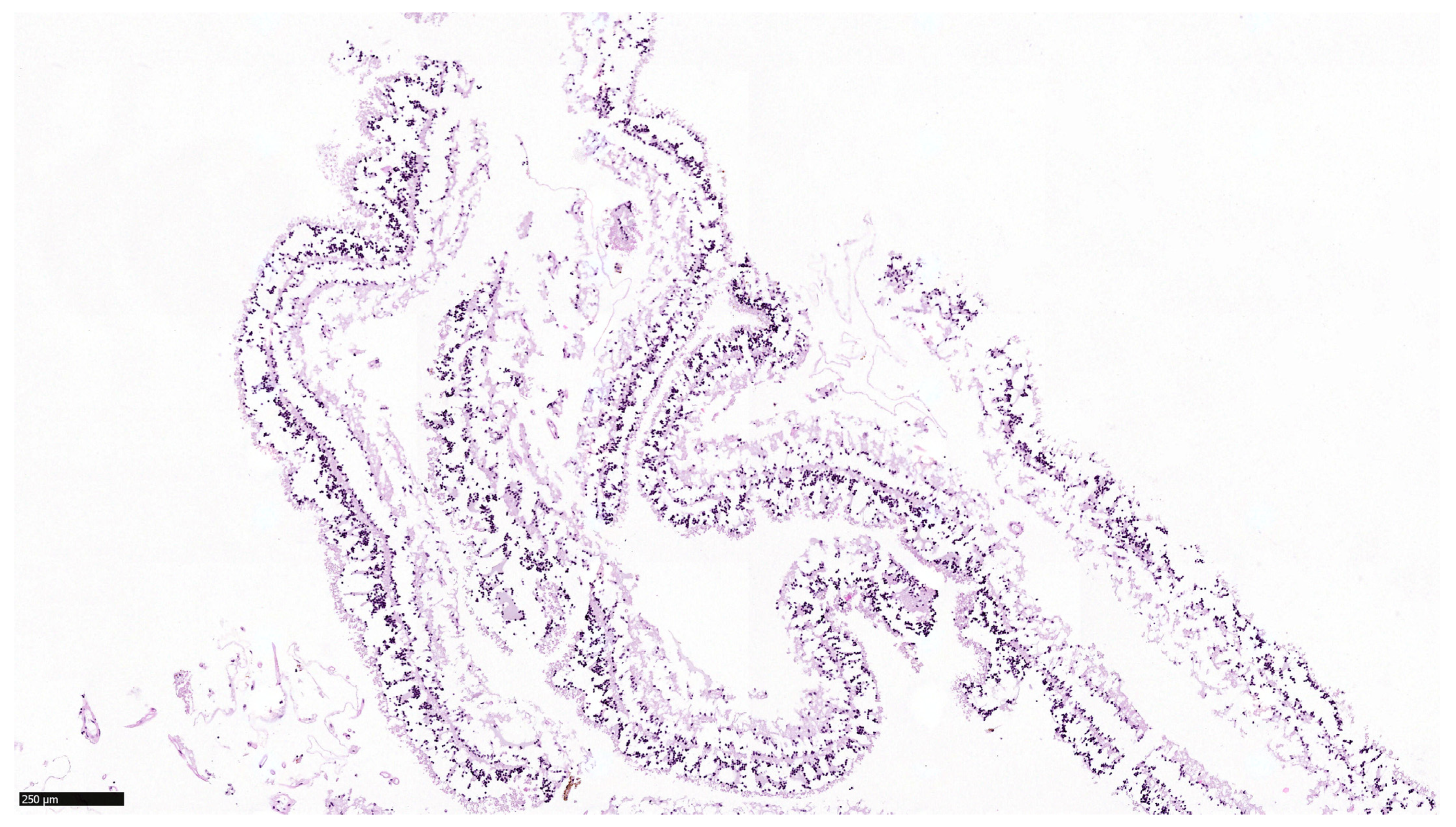
2.2. Histology
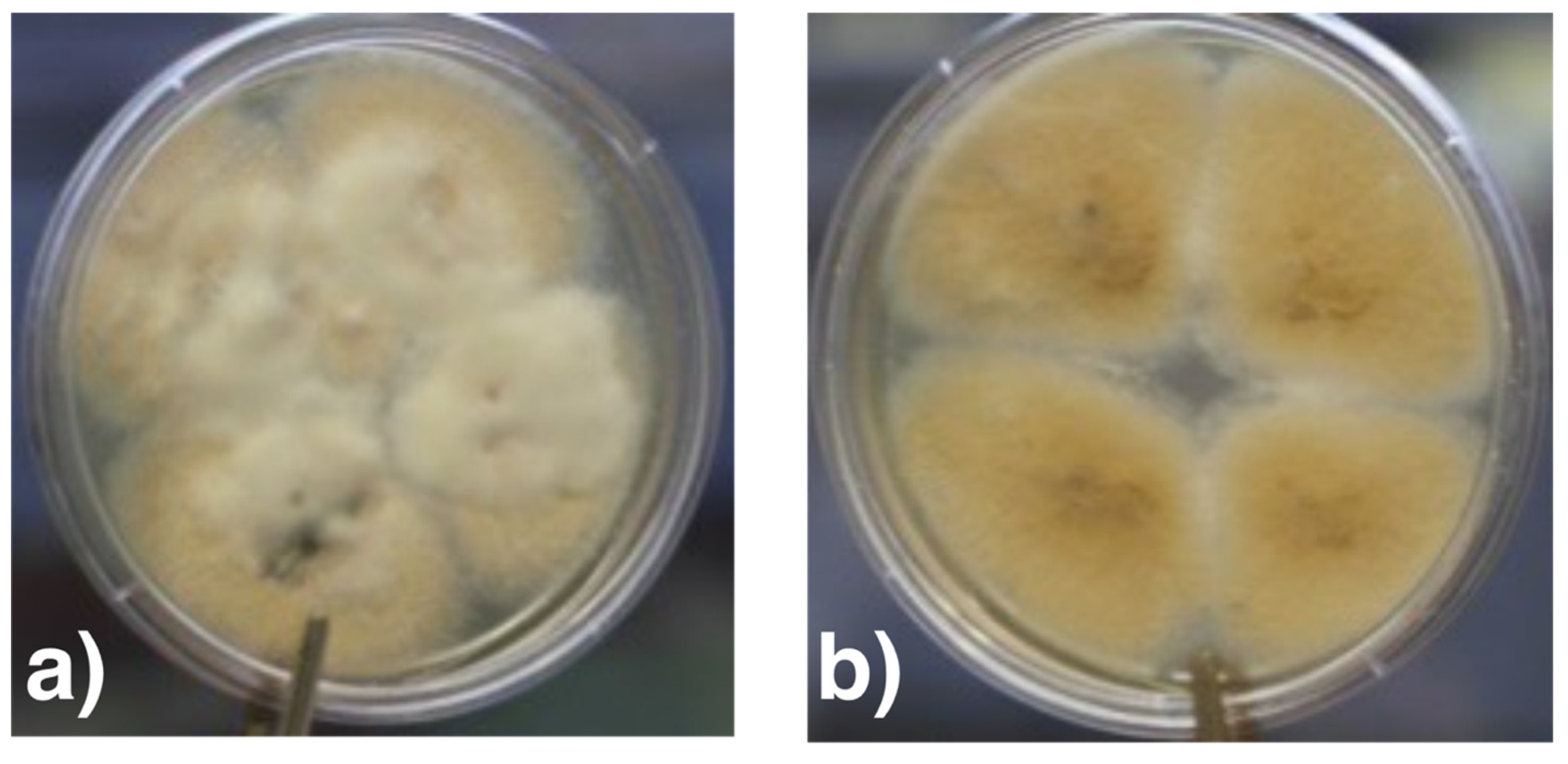
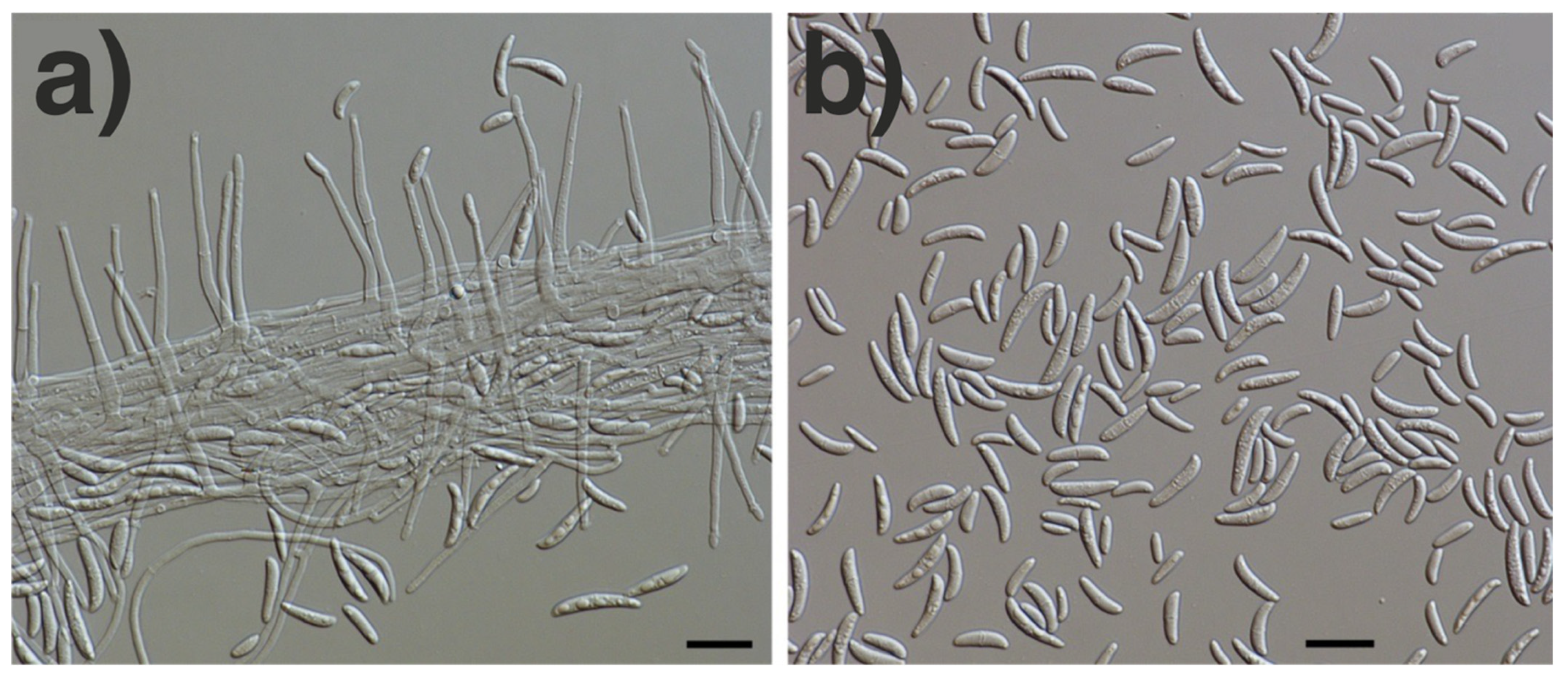
2.3. Microbiology
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- O’Donnell, K.; Ward, T.J.; Robert, V.A.R.G.; Crous, P.W.; Geiser, D.M.; Kang, S. DNA sequence-based identification of Fusarium: Current status and future directions. Phytoparasitica 2015, 43, 583–595. [Google Scholar] [CrossRef]
- Sandoval-Denis, M.; Crous, P.W. Removing chaos from confusion: Assigning names to common human and animal pathogens in neocosmospora. Pers. Mol. Phylogeny Evol. Fungi 2018, 41, 109–129. [Google Scholar] [CrossRef]
- Sandoval-Denis, M.; Lombard, L.; Crous, P.W. Back to the roots: A reappraisal of Neocosmospora. Pers. Mol. Phylogeny Evol. Fungi 2019, 43, 90–185. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, K.; Al-Hatmi, A.M.S.; Aoki, T.; Brankovics, B.; Cano-Lira, J.F.; Coleman, J.J.; de Hoog, G.S.; Di Pietro, A.; Frandsen, R.J.N.; Geiser, D.M.; et al. No to Neocosmospora: Phylogenomic and practical reasons for continued inclusion of the Fusarium solani species complex in the genus Fusarium. mSphere 2020, 5, e00810-20. [Google Scholar] [CrossRef] [PubMed]
- Geiser, D.M.; Al-Hatmi, A.; Aoki, T.; Arie, T.; Balmas, V.; Barnes, I.; Bergstrom, G.C.; Bhattacharyya, M.K.K.; Blomquist, C.L.; Bowden, R.; et al. Phylogenomic analysis of a 55.1 kb 19-gene dataset resolves a monophyletic Fusarium that includes the Fusarium solani Species Complex. Phytopathology 2021, 111, 1064–1079. [Google Scholar] [CrossRef] [PubMed]
- Sáenz, V.; Alvarez-Moreno, C.; Pape, P.L.; Restrepo, S.; Guarro, J.; Ramírez, A.M.C. A one health perspective to recognize Fusarium as important in clinical practice. J. Fungi 2020, 6, 235. [Google Scholar] [CrossRef]
- Hof, H. The medical relevance of Fusarium spp. J. Fungi 2020, 6, 117. [Google Scholar] [CrossRef]
- Walther, G.; Zimmermann, A.; Theuersbacher, J.; Kaerger, K.; von Lilienfeld-Toal, M.; Roth, M.; Kampik, D.; Geerling, G.; Kurzai, O. Eye infections caused by filamentous fungi: Spectrum and antifungal susceptibility of the prevailing agents in Germany. J. Fungi 2021, 7, 511. [Google Scholar] [CrossRef] [PubMed]
- Chang, D.C.; Grant, G.B.; O’Donnell, K.; Wannemuehler, K.A.; Noble-Wang, J.; Rao, C.Y.; Jacobson, L.M.; Crowell, C.S.; Sneed, R.S.; Lewis, F.M.T.; et al. Multistate outbreak of Fusarium keratitis associated with use of a contact lens solution. JAMA 2006, 296, 953–963. [Google Scholar] [CrossRef]
- Khor, W.B.; Aung, T.; Saw, S.M.; Wong, T.Y.; Tambyah, P.A.; Tan, A.L.; Beuerman, R.; Lim, L.; Chan, W.K.; Heng, W.J.; et al. An outbreak of Fusarium keratitis associated with contact lens wear in Singapore. J. Am. Med. Assoc. 2006, 295, 2867–2873. [Google Scholar] [CrossRef]
- Walther, G.; Stasch, S.; Kaerger, K.; Hamprecht, A.; Roth, M.; Cornely, O.A.; Geerling, G.; Mackenzie, C.R.; Kurzai, O.; Von Lilienfeld-Toal, M. Fusarium keratitis in Germany. J. Clin. Microbiol. 2017, 55, 2983–2995. [Google Scholar] [CrossRef]
- Lübke, J.; Auw-Hädrich, C.; Meyer-ter-Vehn, T.; Emrani, E.; Reinhard, T. Fusarium keratitis with dramatic outcome. Ophthalmologe 2017, 114, 462–465. [Google Scholar] [CrossRef] [PubMed]
- Azor, M.; Gené, J.; Cano, J.; Guarro, J. Universal in vitro antifungal resistance of genetic clades of the Fusarium solani species complex. Antimicrob. Agents Chemother. 2007, 51, 1500–1503. [Google Scholar] [CrossRef] [PubMed]
- Niu, L.; Liu, X.; Ma, Z.; Yin, Y.; Sun, L.; Yang, L.; Zheng, Y. Fungal keratitis: Pathogenesis, diagnosis and prevention. Microb. Pathog. 2020, 138, 103802. [Google Scholar] [CrossRef]
- Muraosa, Y.; Oguchs, M.; Yahsro, M.; Watanabe, A.; Yaguchs, T.; Kames, K. Epidemiological study of Fusarium species causing invasive and superficial fusariosis in Japan. Med. Mycol. J. 2017, 58, E5–E13. [Google Scholar] [CrossRef] [PubMed]
- Subcommittee on Antifungal Susceptibility Testing of the ESCMID European Committee for Antimicrobial Susceptibility Testing. EUCAST Technical Note on the method for determination of broth dilution minimum inhibitory concentrations of antifungal agents for conidia-forming moulds. Clin. Microbiol. Infect. 2008, 14, 982–984. [Google Scholar] [CrossRef] [PubMed]
- Lalitha, P.; Shapiro, B.L.; Srinivasan, M.; Prajna, N.V.; Acharya, N.R.; Fothergill, A.W.; Ruiz, J.; Chidambaram, J.D.; Maxey, K.J.; Hong, K.C.; et al. Antimicrobial Susceptibility of Fusarium, Aspergillus, and Other Filamentous Fungi Isolated From Keratitis. Arch. Ophthalmol. 2007, 125, 789–793. [Google Scholar] [CrossRef] [PubMed]
- Manikandan, P.; Abdel-Hadi, A.; Randhir, Y.; Singh, B.; Revathi, R.; Anita, R.; Banawas, S.; Aziz, A.; Dukhyil, B.; Alshehri, B.; et al. Antifungal susceptibilities of Fusarium and Aspergillus isolates from corneal scrapings. BioMed Res. Int. 2019, 2019, 103802. [Google Scholar] [CrossRef]
- Homa, M.; Galgóczy, L.; Manikandan, P.; Narendran, V.; Sinka, R.; Csernetics, Á.; Vágvölgyi, C.; Kredics, L.; Papp, T. South Indian isolates of the Fusarium solani species complex from clinical and environmental samples: Identification, antifungal susceptibilities, and virulence. Front. Microbiol. 2018, 9, 1052. [Google Scholar] [CrossRef]
- Roth, M.; Daas, L.; Renner-Wilde, A.; Cvetkova-Fischer, N.; Saeger, M.; Herwig-Carl, M.; Matthaei, M.; Fekete, A.; Kakkassery, V.; Walther, G.; et al. The German keratomycosis registry: Initial results of a multicenter survey. Ophthalmologe 2019, 116, 957–966. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, A.K.; Gupta, A.; Rudramurthy, S.M.; Paul, S.; Hallur, V.K.; Chakrabarti, A. Fungal Keratitis in North India: Spectrum of Agents, Risk Factors and Treatment. Mycopathologia 2016, 181, 843–850. [Google Scholar] [CrossRef]
- Xie, L.; Zhong, W.; Shi, W.; Sun, S. Spectrum of Fungal Keratitis in North China. Ophthalmology 2006, 113, 1943–1948. [Google Scholar] [CrossRef] [PubMed]
- Bugnicourt, F.; Guilliermond, A. Les Fusarium et Cylindrocarpon de L’indochine; P. Lechevalier: Paris, France, 1939. [Google Scholar]
- Laverde, S.; Moncada, L.H.; Restrepo, A.; Vera, C.L. Mycotic keratitis; 5 cases caused by unusual fungi. Sabouraudia 1973, 11, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Booth, C.; Clayton, Y.; Usherwood, M. Cylindrocarpon species associated with mycotic keratitis. Proc. Plant Sci. 1985, 94, 433–436. [Google Scholar] [CrossRef]
- O’Donnell, K.; Sarver, B.A.J.; Brandt, M.; Chang, D.C.; Noble-Wang, J.; Park, B.J.; Sutton, D.A.; Benjamin, L.; Lindsley, M.; Padhye, A.; et al. Phylogenetic diversity and microsphere array-based genotyping of human pathogenic fusaria, including isolates from the multistate contact lens-associated U.S. keratitis outbreaks of 2005 and 2006. J. Clin. Microbiol. 2007, 45, 2235–2248. [Google Scholar] [CrossRef]
- Raza, S.K.; Mallet, A.I.; Howell, S.A.; Thomas, P.A. An in-vitro study of the sterol content and toxin production of Fusarium isolates from mycotic keratitis. J. Med. Microbiol. 1994, 41, 204–208. [Google Scholar] [CrossRef]
- Hof, H.; Kupfahl, C. Gliotoxin in Aspergillus fumigatus: An example that mycotoxins are potential virulence factors. Mycotoxin Res. 2009, 25, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Hof, H. Mycotoxins: Pathogenicity factors or virulence factors? Mycoses 2008, 51, 93–94. [Google Scholar] [CrossRef]
- Lockwood, M.B.; Crescencio, J.C.R. Adventitious sporulation in Fusarium: The yeast that were not. IDCases 2016, 3, 5–7. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kidd, G.H.; Wolf, F.T. Dimorphism in a Pathogenic Fusarium. Mycologia 1973, 65, 1371–1375. [Google Scholar] [CrossRef] [PubMed]
- Behrens-Baumann, W.; Finis, D.; Mackenzie, C.; Roth, M.; Geerling, G. Keratomycosis–Therapy standards and new developments. Klin. Mon. Fur Augenheilkd. 2015, 232, 754–764. [Google Scholar] [CrossRef]
- Daas, L.; Viestenz, A.; Bischoff, M.; Hasenfus, A.; Seitz, B. Confocal microscopy for the diagnostics of fungal keratitis. Ophthalmologe 2016, 113, 767–771. [Google Scholar] [CrossRef]
- Daas, L.; Bischoff-Jung, M.; Viestenz, A.; Seitz, B.; Viestenz, A. Confocal microscopy as an early relapse marker after keratoplasty due to Fusarium solani keratitis. Ophthalmologe 2017, 114, 66–69. [Google Scholar] [CrossRef]
- Alfaro Rangel, R.; Szentmáry, N.; Lepper, S.; Milioti, G.; Daas, L.; Langenbucher, A.; Seitz, B. Large-diameter penetrating keratoplasties are mostly due to very severe infectious keratitis and cannot always prevent secondary enucleation. Klin. Mon. Für Augenheilkd. 2021, 6–13. [Google Scholar] [CrossRef] [PubMed]
- Al-Hatmi, A.M.S.; Meis, J.F.; de Hoog, G.S. Fusarium: Molecular Diversity and Intrinsic Drug Resistance. PLoS Pathog. 2016, 12, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Espinel-Ingroff, A.; Colombo, A.L.; Cordoba, S.; Dufresne, P.J.; Fuller, J.; Ghannoum, M.; Gonzalez, G.M.; Guarro, J.; Kidd, S.E.; Meis, J.F.; et al. International evaluation of MIC distributions and epidemiological cutoff value (ECV) definitions for Fusarium species identified by molecular methods for the CLSI broth microdilution method. Antimicrob. Agents Chemother. 2016, 60, 1079–1084. [Google Scholar] [CrossRef] [PubMed]
- Hoenigl, M.; Salmanton-García, J.; Walsh, T.J.; Nucci, M.; Neoh, C.F.; Jenks, J.D.; Lackner, M.; Sprute, R.; Al-Hatmi, A.M.S.; Bassetti, M.; et al. Global guideline for the diagnosis and management of rare mould infections: An initiative of the European Confederation of Medical Mycology in cooperation with the International Society for Human and Animal Mycology and the American Society for Microbiolo. Lancet. Infect. Dis. 2021, 21, e246–e257. [Google Scholar] [CrossRef]
- Te Welscher, Y.M.; Hendrik, H.; Balagué, M.M.; Souza, C.M.; Riezman, H.; de Kruijff, B.; Breukink, E. Natamycin Blocks Fungal Growth by Binding Specifically to Ergosterol without Permeabilizing the Membrane *. J. Biol. Chem. 2008, 283, 6393–6401. [Google Scholar] [CrossRef] [PubMed]
- te Welscher, Y.M.; Jones, L.; van Leeuwen, M.R.; Dijksterhuis, J.; de Kruijff, B.; Eitzen, G.; Breukink, E. Natamycin inhibits vacuole fusion at the priming phase via a specific interaction with ergosterol. Antimicrob. Agents Chemother. 2010, 54, 2618–2625. [Google Scholar] [CrossRef]
- Cvetkova, N.; Köstler, J.; Prahs, P.; Helbig, H.; Dietrich-Ntoukas, T. Prolonged topical natamycin 5 % therapy before and after keratoplasty for Fusarium keratitis. Ophthalmologe 2016, 113, 420–424. [Google Scholar] [CrossRef]
- Awwad, S.; Mohamed Ahmed, A.H.A.; Sharma, G.; Heng, J.S.; Khaw, P.T.; Brocchini, S.; Lockwood, A. Principles of pharmacology in the eye. Br. J. Pharmacol. 2017, 174, 4205–4223. [Google Scholar] [CrossRef] [PubMed]
- Fraunfelder, F.T. Extraocular fluid dynamics: How best to apply topical ocular medication. Trans. Am. Ophthalmol. Soc. 1977, 74, 457–487. [Google Scholar]
- Behrens-Baumann, W. Anti-infective drug therapy in ophthalmology—Part 1: Bacterial infections. Klin. Mon. Fur Augenheilkd. 2004, 221, 539–545. [Google Scholar] [CrossRef] [PubMed]
- Todokoro, D.; Suzuki, T.; Tamura, T.; Makimura, K.; Yamaguchi, H.; Inagaki, K.; Akiyama, H. Efficacy of Luliconazole against broad-range filamentous fungi Including Fusarium solani species complex causing fungal keratitis. Cornea 2019, 38, 238–242. [Google Scholar] [CrossRef] [PubMed]
- Behrens-Baumann, W.J. New Antimycotics in the Pipeline—For Ophthalmology Too? Klin. Mon. Für Augenheilkd. 2021, 238, 1108–1112. [Google Scholar] [CrossRef] [PubMed]
- Prakash, G.; Sharma, N.; Goel, M.; Titiyal, J.S.; Vajpayee, R.B. Evaluation of Intrastromal Injection of Voriconazole as a Therapeutic Adjunctive for the Management of Deep Recalcitrant Fungal Keratitis. Am. J. Ophthalmol. 2008, 146, 56–59.e2. [Google Scholar] [CrossRef]
- Troke, P.; Obenga, G.; Gaujoux, T.; Goldschmidt, P.; Bienvenu, A.L.; Cornet, M.; Grenouillet, F.; Pons, D.; Ranque, S.; Sitbon, K.; et al. The efficacy of voriconazole in 24 ocular Fusarium infections. Infection 2013, 41, 15–20. [Google Scholar] [CrossRef]
- Nucci, M.; Jenks, J.; Thompson, G.R.; Hoenigl, M.; Dos Santos, M.C.; Forghieri, F.; Rico, J.C.; Bonuomo, V.; López-Soria, L.; Lass-Flörl, C.; et al. Do high MICs predict the outcome in invasive fusariosis? J. Antimicrob. Chemother. 2021, 76, 1063–1069. [Google Scholar] [CrossRef]
- Cornely, O.A.; Chemnitz, J.; Brochhagen, H.G.; Lemmer, K.; Schütt, H.; Söhngen, D.; Staib, P.; Wickenhauser, C.; Diehl, V.; Tintelnot, K. Disseminated Neocosmospora vasinfecta infection in a patient with acute nonlymphocytic leukemia. Emerg. Infect. Dis. 2001, 7, 149–152. [Google Scholar] [CrossRef]
- Behrens-Baumann, W.J.; Hofmüller, W.; Tammer, I.; Tintelnot, K. Keratomycosis due to Tintelnotia destructans refractory to common therapy treated successfully with systemic and local terbinafine in combination with polyhexamethylene biguanide. Int. Ophthalmol. 2019, 39, 1379–1385. [Google Scholar] [CrossRef]



| Antifungal | MIC | Assessment * |
|---|---|---|
| Amphotericin B | 2 mg/L | presumably resistant |
| Natamycin | 4 mg/L | presumably susceptible |
| Caspofungin | >8 mg/L | presumably resistant |
| Anidulafungin | >8 mg/L | presumably resistant |
| Itraconazol | >8 mg/L | presumably resistant |
| Isavuconazol | >8 mg/L | presumably resistant |
| Posaconazol | >8 mg/L | presumably resistant |
| Voriconazol | 8 mg/L | presumably resistant |
| Terbinafin | >32 mg/L | presumably resistant |
| Mycotoxin | Group | Amount |
|---|---|---|
| Deoxynivalenol (also known as vomitoxin) | Trichothecene | <20 g/L (DL) |
| T2 Toxin (also known as fusariotoxin) | Trichothecene | <18 µg/L (DL) |
| Fumonisin B1 | Fumonisin | <0.05 mg/L (DL) |
| Zearalenone | Zearalenon | <2 µg/L (DL) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schrecker, J.; Seitz, B.; Berger, T.; Daas, L.; Behrens-Baumann, W.; Auw-Hädrich, C.; Schütt, S.; Kerl, S.; Rentner-Andres, S.; Hof, H. Malignant Keratitis Caused by a Highly-Resistant Strain of Fusarium Tonkinense from the Fusarium Solani Complex. J. Fungi 2021, 7, 1093. https://doi.org/10.3390/jof7121093
Schrecker J, Seitz B, Berger T, Daas L, Behrens-Baumann W, Auw-Hädrich C, Schütt S, Kerl S, Rentner-Andres S, Hof H. Malignant Keratitis Caused by a Highly-Resistant Strain of Fusarium Tonkinense from the Fusarium Solani Complex. Journal of Fungi. 2021; 7(12):1093. https://doi.org/10.3390/jof7121093
Chicago/Turabian StyleSchrecker, Jens, Berthold Seitz, Tim Berger, Loay Daas, Wolfgang Behrens-Baumann, Claudia Auw-Hädrich, Sabine Schütt, Sabine Kerl, Sascha Rentner-Andres, and Herbert Hof. 2021. "Malignant Keratitis Caused by a Highly-Resistant Strain of Fusarium Tonkinense from the Fusarium Solani Complex" Journal of Fungi 7, no. 12: 1093. https://doi.org/10.3390/jof7121093
APA StyleSchrecker, J., Seitz, B., Berger, T., Daas, L., Behrens-Baumann, W., Auw-Hädrich, C., Schütt, S., Kerl, S., Rentner-Andres, S., & Hof, H. (2021). Malignant Keratitis Caused by a Highly-Resistant Strain of Fusarium Tonkinense from the Fusarium Solani Complex. Journal of Fungi, 7(12), 1093. https://doi.org/10.3390/jof7121093







