1. Introduction
Annually, fungal infections are responsible for numerous deaths worldwide [
1]. Among the limitations presented by the antifungal agents used for systemic treatment, we can mention: (i) suboptimal efficacy; (ii) toxicity; (iii) drug interactions; and (iv) the emergence of resistant species [
2]. The increasing incidence of fungal infections highlighted the need to find new treatment alternatives [
1].
It is essential to study more effective drugs, which act more selectively on the fungal cell and require shorter treatment and to even explore compounds that act on distinct cellular targets rather than those of commercial antifungals, thus preventing the development of cross-resistance. An alternative strategy is to search for new antifungal candidates from available molecule libraries [
3]. In this study, we used the Pandemic Response Box library, developed by the Medicines for Malaria Venture (MMV) organization, which contains 400 molecules with known activity against fungi, bacteria, and viruses [
4]. Some of these molecules are commercially available drugs, while others are new compounds that showed promising biological activities.
Dimorphic fungi are less sensitive to antifungal treatment, which usually requires a long therapeutic regimen [
5]. These include sporotrichosis, the most common human subcutaneous mycosis globally, which also affects animals, especially cats [
6]. Sporotrichosis can be acquired as sapronosis or zoonosis, and zoonotic transmission is the main form observed in Brazil, with the species
Sporothrix brasiliensis being the most frequent [
6]. Zoonotic sporotrichosis, currently endemic in Brazil and causing hundreds of cases, is expanding to other Latin American countries [
7,
8].
There are a few options for sporotrichosis treatment, with itraconazole as the first choice. However, the treatment is lengthy and expensive and promotes considerable side-effects for patients (gastrointestinal and hepatotoxicity, for example) [
9]. In addition, therapeutic failures and identifying isolates with reduced sensitivity to itraconazole are increasingly frequent in Brazil [
7].
The main objective of our study was to evaluate the Pandemic Response Box library compounds against the medically relevant main causative agents of sporotrichosis: S. brasiliensis, Sporothrix globosa, and Sporothrix schenckii. In addition, we assessed the effects of the most promising compound on yeasts, its selectivity, and the interaction between keratinocytes and treated yeasts.
2. Materials and Methods
2.1. Isolates and Culture Conditions
The reference isolates S. brasiliensis ATCC MYA 4823, S. schenckii ATCC 32286, and S. globosa CBS 130104 were used in this study. Isolates were kept in a saline solution containing 10% glycerol and 10% glucose at −20 °C. S. brasiliensis and S. schenckii were initially cultivated in the mycelial form in Sabouraud broth ( BD Difco™, Franklin Lakes, NJ, USA), and an aliquot containing 105 CFU/mL was inoculated into brain heart infusion broth (BD Difco™) supplemented with 2% glucose (pH 7.8) for the conversion to the yeast phase. Both were incubated at 36 °C, with orbital shaking (150 rpm) for 7 days. S. globosa was initially cultivated in Sabouraud agar (BD Difco™) at 25 °C for 7 days and converted to the yeast phase by a successive passage on brain heart infusion agar (BD Difco™) at 35 °C in a 5% CO2 atmosphere for 7 days. The parasitic yeast phase was used in all assays.
2.2. Cells Line and Culture Conditions
Macrophage cell line (RAW 264.7) and keratinocyte cell line (HaCat) were maintained in DMEM medium (Sigma-Aldrich®, San Luis, MO, USA) with a pH 7.2 supplemented with 10% fetal bovine serum (BD Difco™) in 5% CO2 atmosphere at 37 °C.
2.3. Compounds
Medicines for Malaria Venture (MMV, Geneva, Switzerland) kindly provided the Pandemic Response Box library containing 400 compounds diluted in dimethyl sulfoxide (DMSO) at 10 mM [
4]. All compounds were diluted to 1 mM in DMSO and stored at −20 °C until use. Additional experiments were conducted using olorofim powder, also provided by MMV. Itraconazole (1 mM, Sigma-Aldrich®) in DMSO was used as a standard antifungal.
2.4. Screening the Pandemic Response Box
The reference isolate
S. brasiliensis ATCC MYA 4823 was used to screen the Pandemic Response Box compounds for inhibitors of fungal growth. Compounds were diluted in supplemented RPMI medium (RPMI 1640 supplemented with 2% glucose and buffered with 0.165 M MOPS to pH 7.2) (Sigma-Aldrich®) in flat-bottom 96-well microplates to a final concentration of 1 µM, following the MMV recommended guidelines for screening [
10]. Yeasts were counted in a hemocytometer, and a standardized yeast suspension of 1 × 10
5 CFU/mL was used in experiments. Yeasts were added to each well, and the microplate was incubated for 48 h at 35 °C in a 5% CO
2 atmosphere. After 48 h, fungal growth was analyzed by visual inspection using an inverted light microscope (Axiovert 100, ZEISS, Oberkochen, Germany) and quantified by spectrophotometric readings at 492 nm using a microtiter plate reader (EMax Plus, Molecular Devices, San José, CA, USA). The absorbance value for each well was subtracted from the value for the negative control (well containing only supplemented RPMI media). Inhibition of fungal growth (I) relative to untreated controls was calculated using the following equation: I = 100 − (A × 100/C), where A is the absorbance of treated wells, and C is the absorbance of untreated wells. As an additional control, 0.1% DMSO solution was included in all experiments. Inhibitions of more than 80% were defined as the cut-off to select the most promising compounds, corresponding to clearly visible growth prevention when samples were initially analyzed by visual inspection. Results are representative of three independent experiments performed in duplicate.
2.5. Determination of Minimum Inhibitory Concentration
The broth microdilution technique, adapted for
Sporothrix cells, was used to determine the minimum inhibitory concentration (MIC) values of the most active compounds [
11]. Briefly, serial 2-fold dilutions of the compounds were prepared in supplemented RPMI in flat-bottom 96-well microplates to obtain a final concentration ranging from 0.002 to 1 µM (except for luliconazole, whose final concentration ranged from 1 to 0.0002 µM). Yeasts were added to microplates at a final concentration of 1 × 10
5 CFU/mL and incubated at 35 °C for 48 h in a 5% CO
2 chamber. Fungal growth was analyzed by visual inspection using an inverted light microscope (Axiovert 100, ZEISS) and quantified by spectrophotometric readings at 492 nm (Emax Plus plate reader, Molecular Devices). Negative controls were included in experiments for the subtraction of absorbance values. Concentrations that inhibit at least 50% of fungal growth (IC
50) were calculated using the following equation: I = 100 − (A × 100/C), where A was the absorbance of treated wells, and C was the absorbance of untreated wells. Results are presented as the mean of two independent experiments performed in duplicate.
2.6. Killing Assay
Yeasts (10
5 CFU/mL starting inoculum) were exposed to distinct concentrations of olorofim or itraconazole (0, 1 µM, 10 µM, 50 µM, and 100 µM) in supplemented RPMI for 48 h at 35 °C in a 5% CO
2 atmosphere. Samples were homogenized, and 10 µL were plated on BHI agar and incubated for 5 days at 35 °C in a 5% CO
2 atmosphere. Images of agar plates were digitalized and processed using ImageJ 1.52a software (
https://imagej.nih.gov/ij/, accessed on 19 September 2022 ), and fungal growth was quantified regarding the total area of the colonies. Results are presented as the mean of two independent experiments performed in duplicate.
2.7. Effect of Olorofim on Mature Biofilms
To obtain Sporothrix biofilms, yeast suspensions (106 CFU/mL) in supplemented RPMI were transferred into 96-well microplates (100 µL) (Corning Inc., New York, NY, USA) and incubated for 5 days at 35 °C and 5% CO2. After removing the supernatant, 100 µL of olorofim was added to final concentrations ranging from 1 to 64 µM in supplemented RPMI. The same concentrations of itraconazole were tested in parallel. Biofilms were incubated for 48 h (at 35 °C and 5% CO2), and the metabolic activity was quantified using the XTT reduction assay, with color change measured by spectrophotometric readings at 492 nm (Emax Plus plate reader, Molecular Devices). Inhibition of biofilm metabolic activity was calculated according to the following equation: I = 100 − (A × 100/C), where A is the absorbance of treated biofilms, and C is the absorbance of untreated biofilms. Results are representative of three independent experiments performed in duplicate.
2.8. Fluorimetry Assays
S. brasiliensis yeasts (1 × 105 CFU/mL) were incubated with 0.015, 0.03, and 0.06 µM of olorofim in supplemented RPMI for 48 h at 36 °C in an orbital shaker. Untreated controls were grown in the absence of drugs. Cells were washed in sterile saline, fixed in 2% formaldehyde, counted, and 1 × 107 cells were incubated for 30 min at room temperature in the dark with the following fluorochromes: 20 μM SYTOX™ Blue; 25 μg/mL concanavalin A conjugate with Alexa Fluor™ 488 (Thermo Fisher Scientific, Waltham, Massachusetts, USA); 30 μg/mL aniline blue; or 25 μg/mL calcofluor white (Sigma-Aldrich®). Samples were washed in saline. Yeast suspensions were standardized again, and 100 µL/well was added to a 96-well clear-bottom dark-side microplate. The fluorescence intensity was measured using a Spectra-MAX 340 microplate reader (Molecular Devices), according to the following parameters: 480 nm (excitation at 444 nm) for SYTOX Blue; 519 nm (excitation at 495 nm) for concanavalin A; 502 nm (excitation at 398 nm) for aniline blue; and 432 nm (excitation at 350 nm) for calcofluor white. Results are representative of three independent experiments performed in triplicate.
2.9. Zeta Potential (ζ) and Conductance
S. brasiliensis yeasts were treated as described, washed, and resuspended with pyrogenic water, and 1 × 10
6 cells were used to measure the zeta potential and conductance in a zeta potential analyzer (NanoBrook Omni particle, Brookhaven Instruments Corporation, Holtsville, NY, USA) at 25 °C. Twenty measurements were performed in each experiment. Results are representative of three independent experiments [
12].
2.10. Scanning Electron Microscopy
Untreated or treated yeasts with 0.06 µM of olorofim were washed in sterile saline and fixed in 2.5% glutaraldehyde and 4% formaldehyde in 0.1 M cacodylate buffer for 1 h. Cells were washed in 0.1 M cacodylate buffer, adhered to poly-L-lysine-coated (Sigma-Aldrich®) glass coverslips, and post-fixed with 1% osmium tetroxide in 0.1 M cacodylate buffer containing 1.25% potassium ferrocyanide for 30 min. Samples were dehydrated in a graded ethanol (Merck KGaA, Darmstadt, Germany) series, critical-point-dried in CO2 (EM DPC 300, Leica, Wetzlar, Germany), and coated for sputter with gold/palladium (Au/Pd) (Balzers Union sputtering device FL-9496, Balzers Union, Balzers, Liechtenstein). Images were obtained using a Carl Zeiss Evo LS 10 scanning electron microscope (ZEISS) and processed using Photoshop software (Adobe, San José, CA, USA).
2.11. Transmission Electron Microscopy
Untreated and treated yeasts with 0.06 µM of olorofim were washed in sterile saline and fixed overnight (at 4 °C) in 2.5% glutaraldehyde and 4% formaldehyde in 0.1 M cacodylate buffer. Cells were washed in 0.1 M cacodylate buffer, post-fixed with 1% osmium tetroxide in 0.1 M cacodylate buffer containing 1.25% potassium ferrocyanide for 2 h (at 4 °C), and dehydrated in a graded ethanol series (30, 50, 70, 90, and 100% for 30 min each step at 4 °C). Samples were embedded in Spurr resin, and ultrathin sections were stained in uranyl acetate and lead citrate. Images were obtained using a JEOL 1200 EX transmission electron microscope (JEOL, Akishima, Tokyo, Japan) and processed using Photoshop software (Adobe). The cell wall thickness of 100 cells was measured using ImageJ 1.52a software (
https://imagej.nih.gov/ij/, accessed on 19 September 2022).
2.12. Cytotoxicity Assays
Cytotoxicity assays with olorofim were performed using the keratinocyte cell line HaCaT and the macrophage cell line RAW 264.7. Cells were treated with different concentrations of olorofim ranging from 0.1 to 100 μM and diluted in DMEM medium supplemented with 10% fetal bovine serum. After 48 h of incubation at 37 °C and 5% CO2, concentrations that elicited 50% cytotoxicity (CC50) were estimated according to the Neutral Red assay. The selectivity towards Sporothrix spp. was determined using the median of MIC values previously obtained. The selectivity index (SI) of olorofim was calculated using the following equation: SI = CC50/MIC median. Experiments were also performed in parallel with itraconazole as a control. Results are representative of three independent experiments performed in triplicate.
2.13. Interaction between Keratinocytes and Treated Yeasts
HaCaT cells (5 × 10
5 cells) were seeded in 24-well plates with glass coverslips in DMEM medium supplemented with 10% fetal bovine serum and incubated for 48 h at 37 °C and 5% CO
2. Before the interaction assay, untreated and treated yeasts with 0.06 µM of olorofim or 0.125 µM of itraconazole were washed in sterile saline, and 1 × 10
7 cells were resuspended in DMEM medium. Keratinocytes were exposed to
S. brasiliensis yeasts at a 5:1 ratio (fungus: cell) for 24 h. After incubation, the coverslips were washed with sterile saline and fixed with 4% formaldehyde (Sigma-Aldrich®) for 20 min. The coverslips were stained with Giemsa (Sigma-Aldrich®) for 1 h. Finally, these coverslips were washed in serial solutions of acetone and xylene (Sigma-Aldrich®) and adhered to the glass slide. The interaction rate was calculated using the following equation: Ir = A/B, where A is the number of keratinocytes with yeasts adhered to their surface after 24 h, and B is the total keratinocytes [
13]. The interaction was quantified by counting 100 keratinocytes in each coverslip. Results are representative of three independent experiments performed in duplicate.
2.14. Statistical Analyses
Statistical analysis was performed using Prism 9 software (GraphPad Software, San Diego, CA, USA), and p < 0.05 was considered statistically significant. Differences in fluorescent intensity, physicochemical properties, and interaction ratio were analyzed by one-way analysis of variance (with Dunnett’s post hoc test), while the student t-test (Mann–Whitney test) was used to examine differences in the cell wall thickness.
4. Discussion
Sporotrichosis was recently added to the list of Neglected Tropical Diseases by the World Health Organization, and efforts to understand its pathogenic agent have increased in recent years [
7,
16]. Here, we evaluated the anti-
Sporothrix activity of 400 compounds from the Pandemic Response Box library and demonstrated the high efficacy of olorofim, a new antifungal that belongs to the orotomide class.
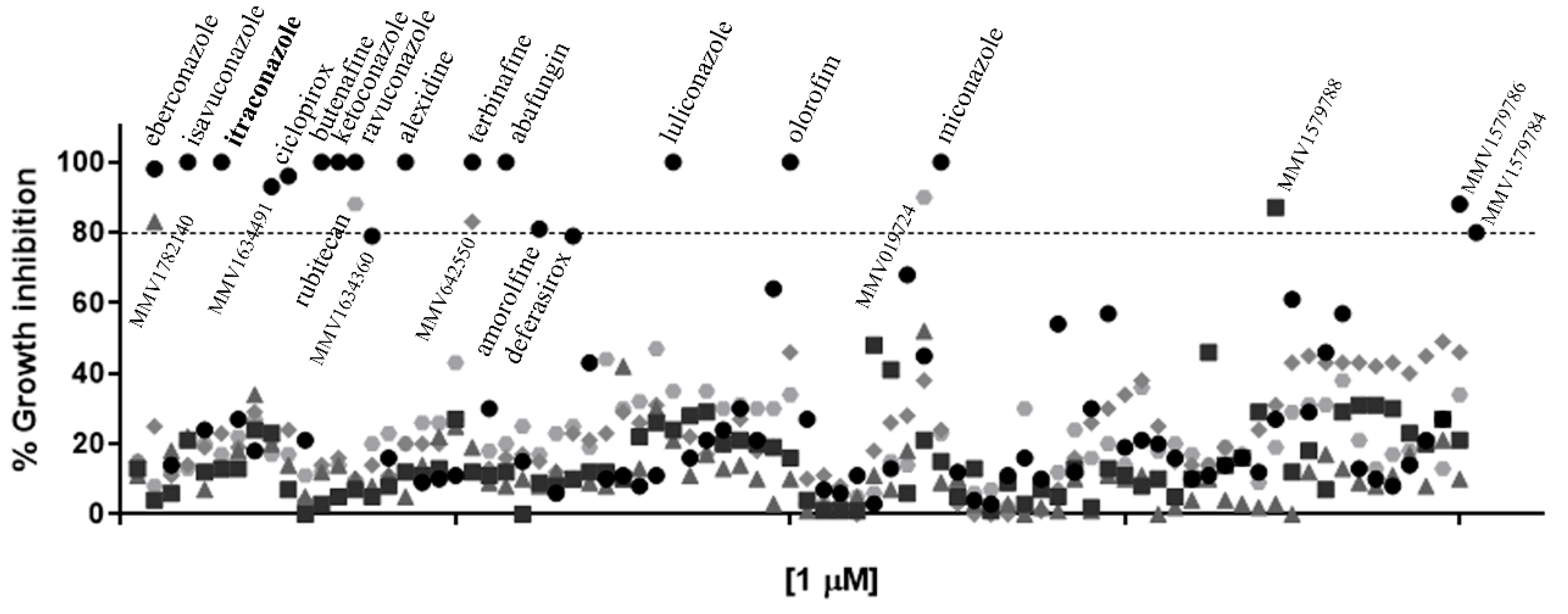
The initial screening showed that twenty-four compounds from the Pandemic Response Box library have in vitro activity against
S. brasiliensis (
Figure 1). Some of these compounds are commercial antifungals used in topical posology to treat fungal infections (abafungin, amorolfine, butenafine, ciclopirox, deferasirox, eberconazole, ketoconazole, luliconazole, miconazole, and terbinafine). Itraconazole and terbinafine presented in the library served as internal controls, confirming the validity of our screening technique because both antifungals are recommended for sporotrichosis treatment and exhibit low MIC values [
7].
Launched in 2005, luliconazole is an azole for the topical treatment of
Tinea pedis, candidiasis, and pityriasis versicolor [
14]. This compound exhibited the lowest MIC values during our tests (
Table 1); however, luliconazole is cytotoxic at low concentrations, prohibiting its systemic use as an antifungal [
14].
Alexidine, another topical drug, also showed anti-
Sporothrix activity. Initially developed as an anticancer drug, it is now used as an antibacterial agent in oral rinse and contact lens solutions [
17]. The antifungal activity of alexidine was previously shown against
Candida spp.,
Aspergillus fumigatus, and
Cryptococcus neoformans [
18]. Here, we demonstrated that alexidine exhibits in vitro activity against dimorphic fungi.
Rubitecan is an antitumoral drug that inhibits DNA topoisomerase I [
19]. This camptothecin derivative inhibits in vitro HIV replication in different cell types [
20]. The antifungal activity of rubitecan was not previously reported, and our results showed that only
S. brasiliensis and
S. schenckii were susceptible to this compound in concentrations lower than 1 µM (
Table 1).
Similar to rubitecan, it was possible to observe that some library compounds that inhibited
S. brasiliensis growth were not active against
S. schenckii or
S. globosa (
Table 1). According to our previous experience,
S. brasiliensis is usually more susceptible during in vitro evaluation than other
Sporothrix species [
21]. Therefore,
S. brasiliensis was selected for our initial screening with the 400 compounds. In general, the three species showed a distinct activity profile. It was interesting to note, for example, that the new azoles isavuconazole and ravuconazole were more active against
S. globosa, with lower MIC values than for
S. brasiliensis and
S. schenckii (
Table 1).
Regarding new compounds (named with “MMV” initials), none of the eight molecules identified as active against
S. brasiliensis was able to inhibit all three
Sporothrix species (
Table 1). MMV identified MMV1634360 and MMV1634491 as antifungal compounds [
10], and our results confirm their ability to inhibit fungal growth. Some of these compounds were described as exhibiting activity against other fungi. MMV1634491 showed in vitro antifungal activity against mycetoma agents and improved the survival rate of
Galleria mellonella infected with
Madurella mycetomatis, as well as the compound MMV019724 (previously described as an antiviral molecule [
10]) [
22]. MMV019724 inhibited the fungal growth of
Cryptococcus spp. and
Candida auris at 5 µM; however, it showed cytotoxicity at this concentration against RAW 264.7 macrophages [
23].
We selected olorofim for further experiments due to its great in vitro activity against the three
Sporothrix species and as a new antifungal already involved in phase III of human tests [
24]. Olorofim (formerly F901318, F2G Ltd., Princeton, NJ, USA) is being evaluated as an oral treatment for life-threatening systemic fungal infections, including invasive aspergillosis, invasive scedosporiosis, invasive lomentosporiosis, coccidioidomycosis, infections due to the
Scopulariopsis species, and invasive fusariosis. In 2022, olorofim commercialization was licensed in Asia and Europe [
15,
25].
The promising in vitro activity of olorofim was already reported for several species of filamentous fungi, with MIC values ranging from 0.03 to 1 µg/mL (0.06 to 2 µM) for
Aspergillus spp.,
Scedosporium spp., and
Fusarium spp., for example [
15]. Olorofim also exhibited potent activity against the dimorphic fungi
Blastomyces dermatitidis,
Coccidioides immitis, and
Histoplasma capsulatum. However, it has no action against the medically relevant yeasts
Candida spp. and
Cryptococcus spp. [
26].
According to the literature, olorofim displayed a fungistatic action profile [
27]; however, in our work, we showed a fungicidal effect at 10 µM against the three
Sporothrix pathogenic species (
Figure 2B). Olorofim inhibited 50% or more of the metabolic activity of the
Sporothrix mature biofilms at concentrations lower than 4 µM (
Figure 2C). It is noteworthy that olorofim could not inhibit the mature biofilms of
Aspergillus fumigatus and
Lomentospora prolificans [
28]. It was also verified that
S. globosa was more sensitive to olorofim, since its yeasts and biofilms were more susceptible to lower concentrations than against
S. brasiliensis and
S. schenckii.
In addition to exhibiting great antifungal activity and selectivity against
Sporothrix pathogenic species, olorofim induced profound alterations on the cell surface and cell cycle arrest in
S. brasiliensis yeasts (
Figure 3). Olorofim inhibits the biosynthesis of pyrimidine due to the reversible inhibition of the enzyme dihydroorotate dehydrogenase (DHODH) located in the mitochondria, causing a reduction in uridine-5′-monophosphate (UMP) and uridine-5′-triphosphate (UTP). UTP plays a central role in several metabolic pathways in eukaryotic cells; therefore, its reduction induces many disturbances inside the cell, such as: (i) a decrease in DNA replication because UTP is necessary to form DNA pyrimidine derivatives; (ii) the impairment of protein synthesis due to decreased RNA levels; and (iii) alterations on fungal cell walls due to the UTP requirement for the generation of UDP–sugars, which are substrates for glucans and chitin biosynthesis [
15]. UTP can also be converted into cytidine triphosphate (CTP), which acts in phospholipid synthesis [
29]. Thus, olorofim can also disturb the plasma membrane.
We observed a dose-dependent DNA accumulation in
S. brasiliensis yeasts with exposure to olorofim, indicating cell cycle arrest probably due to the inhibition of mitosis, as reported with
A. fumigatus [
30]. Olorofim also induced cell wall remodeling with increased chitin and mannans, with the latter exhibiting the most remarkable changes, whereas β-glucan was decreased, as observed with
A. fumigatus [
30] (
Figure 3). The
Sporothrix cell wall is externally coated by a peptido–rhamnomannans layer [
31], which is visualized in
Figure 3(Hiv) as the electron-dense layer forming the cell wall. Untreated yeasts showed a lower peptido-rhamnomannans layer as visualized by transmission electron microscopy (
Figure 3(Hi)), confirming the higher fluorescent stain with concanavalin A. The increase in the cell wall thickness observed due to olorofim treatment confirmed the fluorimetry results with concanavalin A and calcofluor white.
The cell wall also presented a granular appearance after olorofim exposure, which was corroborated by the decrease in cellular conductance. Cell wall remodeling modified the physicochemical properties of yeasts, reducing their electronegativity and conductance (properties related to cell surface aspects). These changes can compromise the ability of yeasts to adhere to a substrate. Based on our results, we hypothesize that olorofim inhibits dihydroorotate dehydrogenase in
Sporothrix cells by blocking pyrimidine biosynthesis (
Figure 5). We verified that these profound morphophysiological alterations in
S. brasiliensis yeasts impaired their ability to adhere to keratinocytes (
Figure 4). Further in vivo experiments should be performed to confirm the potential of olorofim in sporotrichosis treatment.