An Increase in Specialist Treatment for Onychomycosis: An Unexplained Tendency. A Retrospective Study of Patients Treated for Onychomycosis in Danish Hospitals from 1994 to 2018
Abstract
1. Introduction
2. Material and Methods
2.1. Cohort and Case Definition
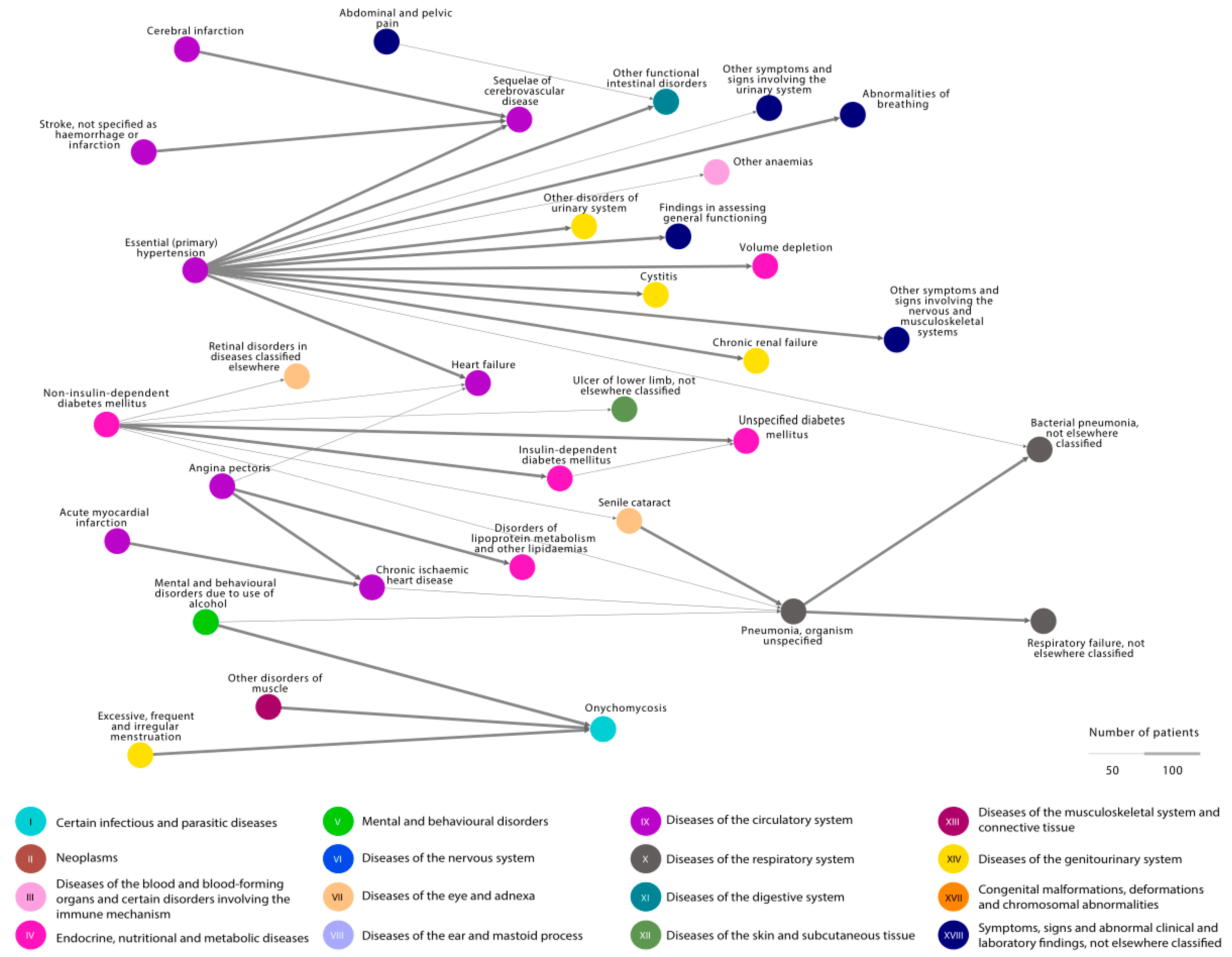
2.2. Disease Trajectories
2.3. Statistics
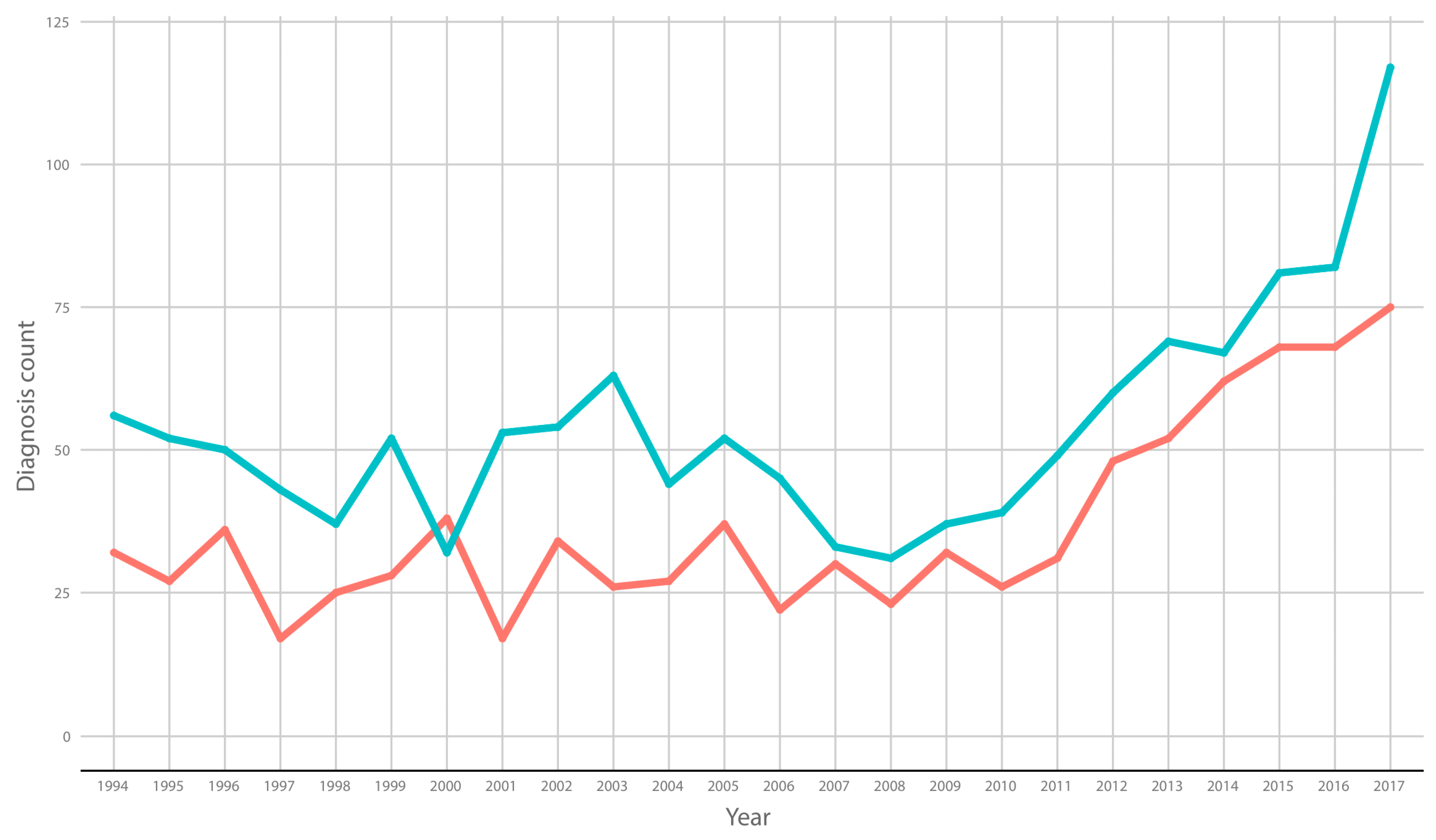
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vos, T.; Flaxman, A.D.; Naghavi, M.; Lozano, R.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; Aboyans, V.; et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2163–2196. [Google Scholar] [CrossRef]
- Andersen, P.L.; Jemec, G.B.E.; Loft, I.C.; Saunte, D.M.L.; Pedersen, O.B. Quality of Life in Danish Blood Donors Treated for Superficial Fungal Infections. Acta Derm.-Venereol. 2021, 101, adv00617. [Google Scholar] [CrossRef]
- Gupta, A.K.; Mays, R.R. The Impact of Onychomycosis on Quality of Life: A Systematic Review of the Available Literature. Ski. Appendage Disord. 2018, 4, 208–216. [Google Scholar] [CrossRef]
- Sigurgeirsson, B.; Baran, R. The prevalence of onychomycosis in the global population—A literature study. J. Eur. Acad. Dermatol. Venereol. 2013, 28, 1480–1491. [Google Scholar] [CrossRef]
- Gupta, A.K.; Versteeg, S.G.; Shear, N.H. Onychomycosis in the 21st Century: An Update on Diagnosis, Epidemiology, and Treatment. J. Cutan. Med. Surg. 2017, 21, 525–539. [Google Scholar] [CrossRef]
- Piraccini, B.M.; Starace, M.; Rubin, A.I.; Di Chiacchio, N.G.; Iorizzo, M.; Rigopoulos, D. A working group of the European Nail Society Onychomycosis: Recommendations for Diagnosis, Assessment of Treatment Efficacy, and Specialist Referral. The CONSONANCE Consensus Project. Dermatol. Ther. 2022, 12, 885–898. [Google Scholar] [CrossRef]
- Lipner, S.R. Onychomycosis: New Developments in Diagnosis, Treatment, and Antifungal Medication Safety. Cutis 2021, 107, 113–114. [Google Scholar] [CrossRef]
- Shen, J.J.; Jemec, G.B.; Arendrup, M.C.; Saunte, D.M.L. Photodynamic therapy treatment of superficial fungal infections: A systematic review. Photodiagnosis Photodyn. Ther. 2020, 31, 101774. [Google Scholar] [CrossRef]
- Schmidt, M.; Pedersen, L.; Sørensen, H.T. The Danish Civil Registration System as a tool in epidemiology. Eur. J. Epidemiol. 2014, 29, 541–549. [Google Scholar] [CrossRef]
- Jensen, A.B.; Moseley, P.L.; Oprea, T.I.; Ellesøe, S.G.; Eriksson, R.; Schmock, H.; Jensen, P.B.; Jensen, L.J.; Brunak, S. Temporal disease trajectories condensed from population-wide registry data covering 6.2 million patients. Nat. Commun. 2014, 5, 4022. [Google Scholar] [CrossRef]
- Henning, M.; Reguant, R.; Jørgensen, I.; Andersen, R.; Ibler, K.; Pedersen, O.; Jemec, G.; Brunak, S. The temporal association of hyperhidrosis and its comorbidities—A nationwide hospital-based cohort study. J. Eur. Acad. Dermatol. Venereol. 2022, 36, 2504–2511. [Google Scholar] [CrossRef]
- Andersen, R.K.; Jørgensen, I.F.; Reguant, R.; Jemec, G.B.E.; Brunak, S. Disease Trajectories for Hidradenitis Suppurativa in the Danish Population. JAMA Dermatol. 2020, 156, 780–787. [Google Scholar] [CrossRef]
- Svejgaard, E.L.; Nilsson, J. Onychomycosis in Denmark: Prevalence of fungal nail infection in general practice. Onychomykosen in Danemark: Die Haufigkeit von Nagelmykosen in der Allgemeinpraxis. Mycoses 2004, 47, 131–135. [Google Scholar] [CrossRef]
- Klaassen, K.; Dulak, M.; van de Kerkhof, P.; Pasch, M. The prevalence of onychomycosis in psoriatic patients: A systematic review. J. Eur. Acad. Dermatol. Venereol. 2014, 28, 533–541. [Google Scholar] [CrossRef]
- Statistics Denmark, Population Figures. 2022. Available online: https://www.dst.dk/en/Statistik/emner/borgere/befolkning/befolkningstal (accessed on 14 December 2022).
- Vasconcellos, C.; Pereira, C.Q.M.; Souza, M.C.; Pelegrini, A.; Freitas, R.S.; Takahashi, J.P. Identification of fungi species in the onychomycosis of institutionalized elderly. An. Bras. De Dermatol. 2013, 88, 377–380. [Google Scholar] [CrossRef]
- Gupta, A.K.; Venkataraman, M.; Talukder, M. Onychomycosis in Older Adults: Prevalence, Diagnosis, and Management. Drugs Aging 2022, 39, 191–198. [Google Scholar] [CrossRef]
- Statistics Denmark, Population 1. January 2017. 2022. Available online: https://extranet.dst.dk/pyramide/pyramide.htm#!y=2017&a=16,60&v=2&l=en&g (accessed on 14 December 2022).
- Statistics Denmark, Population 1. January 1994. 2022. Available online: https://extranet.dst.dk/pyramide/pyramide.htm#!y=1994&a=16,60&v=2&l=en&g (accessed on 14 December 2022).
- Gupta, A.; Daigle, D.; Foley, K. The prevalence of culture-confirmed toenail onychomycosis in at-risk patient populations. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 1039–1044. [Google Scholar] [CrossRef]
- Andersen, P.L.; Henning, M.; E Jemec, G.B.; Arendrup, M.C.; Saunte, D.M. Two Cases of Proximal Subungual Onychomycosis Caused by Trichophyton rubrum in HIV-negative Patients During Treatment with TNF-α Inhibitors Combined with Methotrexate. Acta Dermatovenerol. Croat. ADC 2018, 26, 304–306. [Google Scholar]
- Gupta, A.K.; Renaud, H.J.; Quinlan, E.M.; Shear, N.H.; Piguet, V. The Growing Problem of Antifungal Resistance in Onychomycosis and Other Superficial Mycoses. Am. J. Clin. Dermatol. 2021, 22, 149–157. [Google Scholar] [CrossRef]
- Saunte, D.; Pereiro-Ferreirós, M.; Rodríguez-Cerdeira, C.; Sergeev, A.; Arabatzis, M.; Prohić, A.; Piraccini, B.; Lecerf, P.; Nenoff, P.; Kotrekhova, L.; et al. Emerging antifungal treatment failure of dermatophytosis in Europe: Take care or it may become endemic. J. Eur. Acad. Dermatol. Venereol. 2021, 35, 1582–1586. [Google Scholar] [CrossRef]
- Shen, J.J.; Arendrup, M.C.; Jemec, G.B.; Saunte, D.M.L. Photodynamic therapy: A treatment option for terbinafine resistant Trichophyton species. Photodiagnosis Photodyn. Ther. 2021, 33, 102169. [Google Scholar] [CrossRef]
- Falotico, J.M.; Lipner, S.R. Updated Perspectives on the Diagnosis and Management of Onychomycosis. Clin. Cosmet. Investig. Dermatol. 2022, 15, 1933–1957. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lindsø Andersen, P.; Jørgensen, I.F.; Saunte, D.M.L.; Jemec, G.B.; Pedersen, O.B.; Brunak, S. An Increase in Specialist Treatment for Onychomycosis: An Unexplained Tendency. A Retrospective Study of Patients Treated for Onychomycosis in Danish Hospitals from 1994 to 2018. J. Fungi 2023, 9, 33. https://doi.org/10.3390/jof9010033
Lindsø Andersen P, Jørgensen IF, Saunte DML, Jemec GB, Pedersen OB, Brunak S. An Increase in Specialist Treatment for Onychomycosis: An Unexplained Tendency. A Retrospective Study of Patients Treated for Onychomycosis in Danish Hospitals from 1994 to 2018. Journal of Fungi. 2023; 9(1):33. https://doi.org/10.3390/jof9010033
Chicago/Turabian StyleLindsø Andersen, Pernille, Isabella Friis Jørgensen, Ditte Marie Lindhardt Saunte, Gregor Borut Jemec, Ole Birger Pedersen, and Søren Brunak. 2023. "An Increase in Specialist Treatment for Onychomycosis: An Unexplained Tendency. A Retrospective Study of Patients Treated for Onychomycosis in Danish Hospitals from 1994 to 2018" Journal of Fungi 9, no. 1: 33. https://doi.org/10.3390/jof9010033
APA StyleLindsø Andersen, P., Jørgensen, I. F., Saunte, D. M. L., Jemec, G. B., Pedersen, O. B., & Brunak, S. (2023). An Increase in Specialist Treatment for Onychomycosis: An Unexplained Tendency. A Retrospective Study of Patients Treated for Onychomycosis in Danish Hospitals from 1994 to 2018. Journal of Fungi, 9(1), 33. https://doi.org/10.3390/jof9010033






