Invasive Fungal Infections: The Early Killer after Liver Transplantation
Abstract
:1. Introduction
2. Materials and Methods
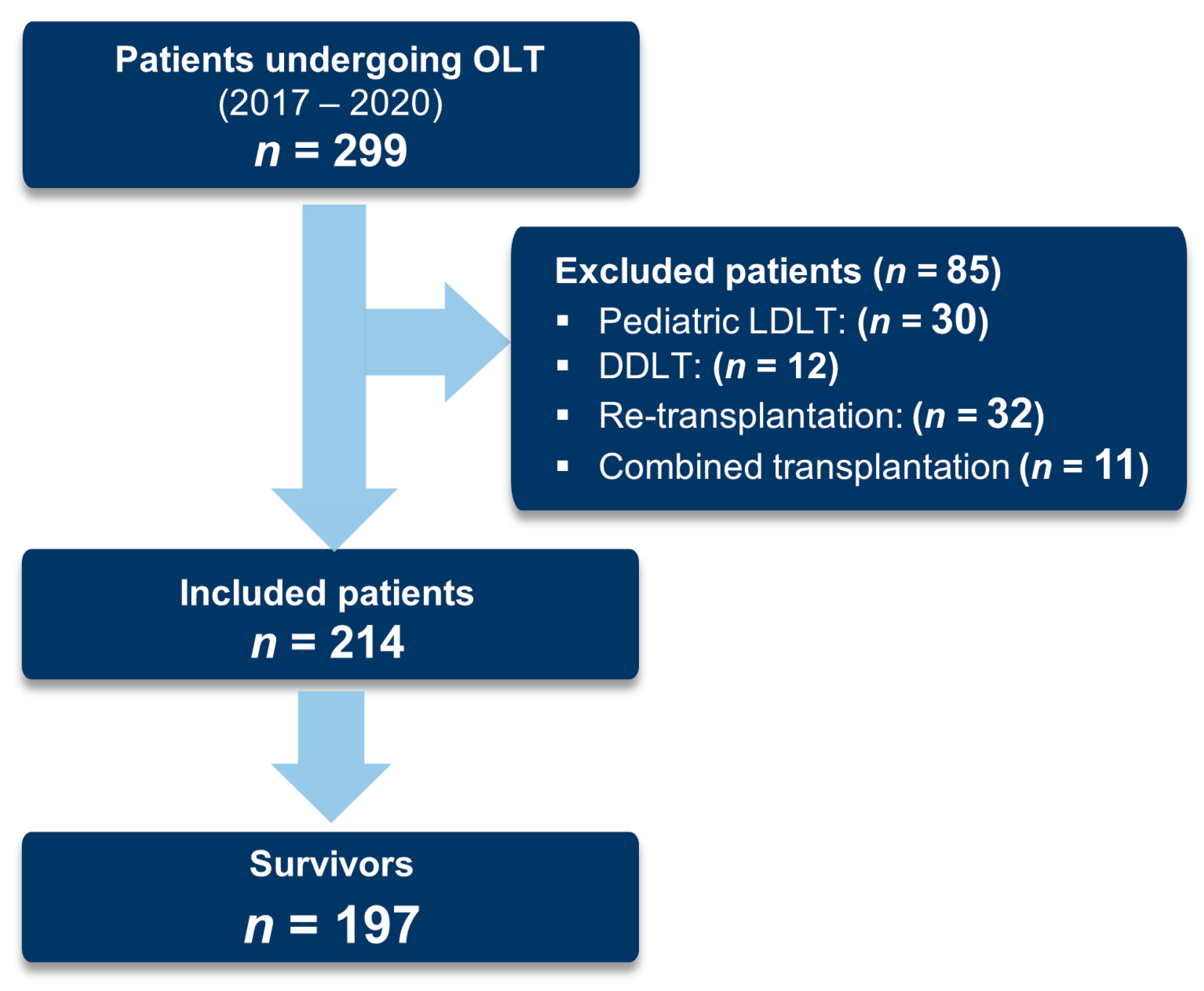
2.1. Patient Selection
2.2. Data Collection and Study Endpoints
2.3. Surgical Technique and Outcomes Definition
Outcome Definitions
2.4. Immunosuppressive Regimen and Prophylaxis
2.5. Statistical Analyses
3. Results
3.1. Study Population and Baseline Characteristics
3.2. Postoperative Complications
3.3. Mortality
3.3.1. One-Year Mortality
3.3.2. Infection-Attributed Mortality
3.4. Risk Factors for Early Postoperative Mortality
4. Discussion
4.1. Mortality
Infection-Attributed Mortality
4.2. Risk Factors for Early Postoperative Mortality
4.3. Limitations
4.4. Future Perspectives
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Starzl, T.E.; Marchioro, T.L.; Porter, K.A.; Brettschneider, L. Homotransplantation of the Liver. Transplantation 1967, 5, 790–803. [Google Scholar] [CrossRef]
- Zarrinpar, A.; Busuttil, R.W. Liver Transplantation: Past, Present and Future. Nat. Rev. Gastroenterol. Hepatol. 2013, 10, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Müller, P.C.; Kabacam, G.; Vibert, E.; Germani, G.; Petrowsky, H. Current Status of Liver Transplantation in Europe. Int. J. Surg. 2020, 82, 22–29. [Google Scholar] [CrossRef]
- Linecker, M.; Krones, T.; Berg, T.; Niemann, C.U.; Steadman, R.H.; Dutkowski, P.; Clavien, P.A.; Busuttil, R.W.; Truog, R.D.; Petrowsky, H. Potentially Inappropriate Liver Transplantation in the Era of the “Sickest First” Policy—A Search for the Upper Limits. J. Hepatol. 2018, 68, 798–813. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Halldorson, J.B.; Paarsch, H.J.; Dodge, J.L.; Segre, A.M.; Lai, J.; Roberts, J.P. Center Competition and Outcomes Following Liver Transplantation. Wiley Online Libr. 2013, 19, 96–104. [Google Scholar] [CrossRef] [Green Version]
- Fox, A.N.; Vagefi, P.A.; Stock, P.G. Liver Transplantation in HIV Patients. Semin. Liver Dis. 2012, 32, 177–185. [Google Scholar] [CrossRef]
- Lomero, M.; Gardiner, D.; Coll, E.; Haase-Kromwijk, B.; Procaccio, F.; Immer, F.; Gabbasova, L.; Antoine, C.; Jushinskis, J.; Lynch, N.; et al. Donation after Circulatory Death Today: An Updated Overview of the European Landscape. Wiley Online Libr. 2020, 33, 76–88. [Google Scholar] [CrossRef] [Green Version]
- Orman, E.S.; Barritt, A.S.; Wheeler, S.B.; Hayashi, P.H. Declining Liver Utilization for Transplantation in the United States and the Impact of Donation after Cardiac Death. Wiley Online Libr. 2013, 19, 59–68. [Google Scholar] [CrossRef] [Green Version]
- Marsh, J.; Gray, E.; Ness, R.; Starzl, T.E. Complications of Right Lobe Living Donor Liver Transplantation. J. Hepatol. 2009, 51, 715–724. [Google Scholar] [CrossRef] [Green Version]
- Belli, L.S.; Perricone, G.; Adam, R.; Cortesi, P.A.; Strazzabosco, M.; Facchetti, R.; Karam, V.; Salizzoni, M.; Andujar, R.L.; Fondevila, C.; et al. Impact of DAAs on Liver Transplantation: Major Effects on the Evolution of Indications and Results. An ELITA Study Based on the ELTR Registry. J. Hepatol. 2018, 69, 810–817. [Google Scholar] [CrossRef]
- Adam, R.E.; Karam, V.; Erie Cailliez, V.; Grady, J.G.O.; Mirza, D.; Cherqui, D.; Klempnauer, J.; Salizzoni, M.; Pratschke, J.; Jamieson, N.; et al. 2018 Annual Report of the European Liver Transplant Registry (ELTR)–50-year Evolution of Liver Transplantation. Wiley Online Libr. 2018, 31, 1293–1317. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rea, D.J.; Rosen, C.B.; Nagorney, D.M.; Heimbach, J.K.; Gores, G.J. Transplantation for Cholangiocarcinoma: When and for Whom? Surg. Oncol. Clin. N. Am. 2009, 18, 325–337. [Google Scholar] [CrossRef] [PubMed]
- Rosado, B.; Gores, G.J. Liver Transplantation for Neuroendocrine Tumors: Progress and Uncertainty. Liver Transpl. 2004, 10, 712–713. [Google Scholar] [CrossRef] [PubMed]
- Bennett-Guerrero, E.; Feierman, D.E.; Barclay, G.R.; Parides, M.K.; Sheiner, P.A.; Mythen, M.G.; Levine, D.M.; Parker, T.S.; Carroll, S.F.; White, M.L.; et al. Preoperative and Intraoperative Predictors of Postoperative Morbidity, Poor Graft Function, and Early Rejection in 190 Patients Undergoing Liver Transplantation. Arch. Surg. 2001, 136, 1177–1183. [Google Scholar] [CrossRef] [Green Version]
- Gil, E.; Kim, J.M.; Jeon, K.; Park, H.; Kang, D.; Cho, J.; Suh, G.Y.; Park, J. Recipient Age and Mortality after Liver Transplantation: A Population-Based Cohort Study. Transplantation 2018, 102, 2025–2032. [Google Scholar] [CrossRef]
- Zhang, X.-M.; Fan, H.; Wu, Q.; Zhang, X.-X.; Lang, R.; He, Q. In-Hospital Mortality of Liver Transplantation and Risk Factors: A Single-Center Experience. Ann. Transl. Med. 2021, 9, 369. [Google Scholar] [CrossRef]
- Rana, A.; Gruessner, A.; Agopian, V.G.; Khalpey, Z.; Riaz, I.B.; Kaplan, B.; Halazun, K.J.; Busuttil, R.W.; Gruessner, R.W.G. Survival Benefit of Solid-Organ Transplant in the United States. JAMA Surg. 2015, 150, 252–259. [Google Scholar] [CrossRef] [Green Version]
- Adam, R.; Karam, V.; Delvart, V.; O’Grady, J.; Mirza, D.; Klempnauer, J.; Castaing, D.; Neuhaus, P.; Jamieson, N.; Salizzoni, M.; et al. Evolution of Indications and Results of Liver Transplantation in Europe. A Report from the European Liver Transplant Registry (ELTR). J. Hepatol. 2012, 57, 675–688. [Google Scholar] [CrossRef] [Green Version]
- Baganate, F.; Beal, E.W.; Tumin, D.; Azoulay, D.; Mumtaz, K.; Black, S.M.; Washburn, K.; Pawlik, T.M. Early Mortality after Liver Transplantation: Defining the Course and the Cause. Surgery 2018, 164, 694–704. [Google Scholar] [CrossRef]
- Senoner, T.; Breitkopf, R.; Treml, B.; Rajsic, S. Invasive Fungal Infections after Liver Transplantation. J. Clin. Med. 2023, 12, 3238. [Google Scholar] [CrossRef]
- Peter Donnelly, J.; Chen, S.C.; Kauffman, C.A.; Steinbach, W.J.; Baddley, J.W.; Verweij, P.E.; Clancy, C.J.; Wingard, J.R.; Lockhart, S.R.; Groll, A.H.; et al. Revision and Update of the Consensus Definitions of Invasive Fungal Disease from the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clin. Infect. Dis. 2020, 71, 1367–1376. [Google Scholar] [CrossRef] [Green Version]
- Bassetti, M.; Azoulay, E.; Kullberg, B.J.; Ruhnke, M.; Shoham, S.; Vazquez, J.; Giacobbe, D.R.; Calandra, T. EORTC/MSGERC Definitions of Invasive Fungal Diseases: Summary of Activities of the Intensive Care Unit Working Group. Clin. Infect. Dis. 2021, 72, S121–S127. [Google Scholar] [CrossRef]
- Cornely, O.A.; Hoenigl, M.; Lass-Flörl, C.; Chen, S.C.A.; Kontoyiannis, D.P.; Morrissey, C.O.; Thompson, G.R. Defining Breakthrough Invasive Fungal Infection-Position Paper of the Mycoses Study Group Education and Research Consortium and the European Confederation of Medical Mycology. Mycoses 2019, 62, 716–729. [Google Scholar] [CrossRef]
- Breitkopf, R.; Treml, B.; Simmet, K.; Bukumirić, Z.; Fodor, M.; Senoner, T.; Rajsic, S. Incidence of Invasive Fungal Infections in Liver Transplant Recipients under Targeted Echinocandin Prophylaxis. J. Clin. Med. 2023, 12, 1520. [Google Scholar] [CrossRef]
- Breitkopf, R.; Treml, B.; Senoner, T.; Bukumirić, Z.; Rajsic, S. Invasive Fungal Breakthrough Infections under Targeted Echinocandin Prophylaxis in High-Risk Liver Transplant Recipients. J. Fungi 2023, 9, 272. [Google Scholar] [CrossRef]
- Righi, E. Management of Bacterial and Fungal Infections in End Stage Liver Disease and Liver Transplantation: Current Options and Future Directions. World J. Gastroenterol. 2018, 24, 4311. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Available online: https://scholar.google.com/scholar_lookup?title=Surveillance+of+Surgical+Site+Infections+and+Prevention+Indicators+in+European+Hospitals-HAI-Net+SSI+Protocol&publication_year=2017& (accessed on 6 June 2023).
- The European Committee on Antimicrobial Susceptibility. Available online: https://scholar.google.com/scholar?q=The%20European%20Committee%20on%20Antimicrobial%20Susceptibility%20Testing.%20Breakpoint%20tables%20for%20interpretation%20of%20MICs%20and%20zone%20diameters.%20Version%209.0,%202019.%20Available%20at:%20http:www.eucast.org.%20Accessed%20November%201,%202019 (accessed on 6 June 2023).
- Plachouras, D.; Lepape, A.; Suetens, C. ECDC Definitions and Methods for the Surveillance of Healthcare-Associated Infections in Intensive Care Units. Intensive Care Med. 2018, 44, 2216–2218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, D.J.; Lee, S.K.; Jo, J.W.; Kim, S.J.; Kwon, C.H.D.; Park, J.W.; Han, Y.S.; Park, J.B. Prognosis after Liver Transplantation Predicted by Preoperative MELD Score. Transpl. Proc. 2006, 38, 2095–2096. [Google Scholar] [CrossRef]
- Bruns, H.; Lozanovski, V.J.; Schultze, D.; Hillebrand, N.; Hinz, U.; Büchler, M.W.; Schemmer, P. Prediction of Postoperative Mortality in Liver Transplantation in the Era of MELD-Based Liver Allocation: A Multivariate Analysis. PLoS ONE 2014, 9, e98782. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Serrano, M.T.; Sabroso, S.; Esteban, L.M.; Berenguer, M.; Fondevila, C.; Lorente, S.; Cortés, L.; Sanchez-Antolin, G.; Nuño, J.; De la Rosa, G.; et al. Mortality and Causes of Death after Liver Transplantation: Analysis of Sex Differences in a Large Nationwide Cohort. Transpl. Int. 2022, 35, 91. [Google Scholar] [CrossRef]
- Lewsey, J.D.; Dawwas, M.; Copley, L.P.; Gimson, A.; Van Der Meulen, J.H.P. Developing a Prognostic Model for 90-Day Mortality after Liver Transplantation Based on Pretransplant Recipient Factors. Transplantation 2006, 82, 898–907. [Google Scholar] [CrossRef] [PubMed]
- Levesque, E.; Winter, A.; Noorah, Z.; Daurès, J.P.; Landais, P.; Feray, C.; Azoulay, D. Impact of Acute-on-Chronic Liver Failure on 90-Day Mortality Following a First Liver Transplantation. Liver Int. 2017, 37, 684–693. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Kim, B.W.; Choi, H.J.; Hong, S.H.; Park, C.S.; Choi, J.H.; Chae, M.S. Risk Stratification for Early Bacteremia after Living Donor Liver Transplantation: A Retrospective Observational Cohort Study. BMC Surg. 2020, 20, 2. [Google Scholar] [CrossRef] [PubMed]
- Kim, S., II. Bacterial Infection after Liver Transplantation. World J. Gastroenterol. WJG 2014, 20, 6211. [Google Scholar] [CrossRef]
- Singh, N.; Limaye, A.P. Infections in Solid-Organ Transplant Recipients. Mand. Douglas Bennetts Princ. Pract. Infect. Dis. 2015, 2, 3440. [Google Scholar] [CrossRef]
- Fishman, J.A.; Rubin, R.H. Infection in Organ-Transplant Recipients. N. Engl. J. Med. 1998, 338, 1741–1751. [Google Scholar] [CrossRef]
- Raghuram, A.; Restrepo, A.; Safadjou, S.; Cooley, J.; Orloff, M.; Hardy, D.; Butler, S.; Koval, C.E. Invasive Fungal Infections Following Liver Transplantation: Incidence, Risk Factors, Survival, and Impact of Fluconazole-Resistant Candida Parapsilosis (2003–2007). Liver Transplant. 2012, 18, 1100–1109. [Google Scholar] [CrossRef]
- Pappas, P.G.; Alexander, B.D.; Andes, D.R.; Hadley, S.; Kauffman, C.A.; Freifeld, A.; Anaissie, E.J.; Brumble, L.M.; Herwaldt, L.; Lto, J.; et al. Invasive Fungal Infections among Organ Transplant Recipients: Results of the Transplant-Associated Infection Surveillance Network (TRANSNET). Clin. Infect. Dis. 2010, 50, 1101–1111. [Google Scholar] [CrossRef]
- Saliba, F.; Pascher, A.; Cointault, O.; Laterre, P.F.; Cervera, C.; De Waele, J.J.; Cillo, U.; Langer, R.M.; Lugano, M.; Göran-Ericzon, B.; et al. Randomized Trial of Micafungin for the Prevention of Invasive Fungal Infection in High-Risk Liver Transplant Recipients. Clin. Infect. Dis. 2015, 60, 997–1006. [Google Scholar] [CrossRef]
- Sun, H.Y.; Cacciarelli, T.V.; Singh, N. Micafungin versus Amphotericin B Lipid Complex for the Prevention of Invasive Fungal Infections in High-Risk Liver Transplant Recipients. Transplantation 2013, 96, 573–578. [Google Scholar] [CrossRef]
- Winston, D.J.; Limaye, A.P.; Pelletier, S.; Safdar, N.; Morris, M.I.; Meneses, K.; Busuttil, R.W.; Singh, N. Randomized, Double-Blind Trial of Anidulafungin versus Fluconazole for Prophylaxis of Invasive Fungal Infections in High-Risk Liver Transplant Recipients. Am. J. Transpl. 2014, 14, 2758–2764. [Google Scholar] [CrossRef] [Green Version]
- Perrella, A.; Esposito, C.; Amato, G.; Perrella, O.; Migliaccio, C.; Pisaniello, D.; Calise, F.; Cuomo, O.; Santaniello, W. Antifungal Prophylaxis with Liposomal Amphotericin B and Caspofungin in High-Risk Patients after Liver Transplantation: Impact on Fungal Infections and Immune System. Infect. Dis. 2016, 48, 161–166. [Google Scholar] [CrossRef]
- Neyra, K.M.; Brizendine, K.D. Retrospective Study Evaluating the Performance of Risk Factors for Invasive Mold Infections in Liver Transplantation. Transpl. Infect. Dis. 2020, 22, e13223. [Google Scholar] [CrossRef] [PubMed]
- Kang, W.H.; Song, G.W.; Lee, S.G.; Suh, K.S.; Lee, K.W.; Yi, N.J.; Joh, J.W.; Kwon, C.H.D.; Kim, J.M.; Choi, D.L.; et al. A Multicenter, Randomized, Open-Label Study to Compare Micafungin with Fluconazole in the Prophylaxis of Invasive Fungal Infections in Living-Donor Liver Transplant Recipients. J. Gastrointest. Surg. 2020, 24, 832–840. [Google Scholar] [CrossRef] [PubMed]
- Rinaldi, M.; Bartoletti, M.; Ferrarese, A.; Franceschini, E.; Campoli, C.; Coladonato, S.; Pascale, R.; Tedeschi, S.; Gatti, M.; Cricca, M.; et al. Breakthrough Invasive Fungal Infection after Liver Transplantation in Patients on Targeted Antifungal Prophylaxis: A Prospective Multicentre Study. Transpl. Infect. Dis. 2021, 23, e13608. [Google Scholar] [CrossRef]
- Fortún, J.; Muriel, A.; Martín-Dávila, P.; Montejo, M.; Len, O.; Torre-Cisneros, J.; Carratalá, J.; Muñoz, P.; Fariñas, C.; Moreno, A.; et al. Caspofungin versus Fluconazole as Prophylaxis of Invasive Fungal Infection in High-Risk Liver Transplantation Recipients: A Propensity Score Analysis. Liver Transpl. 2016, 22, 427–435. [Google Scholar] [CrossRef] [Green Version]
- Eschenauer, G.A.; Lam, S.W.; Carver, P.L. Antifungal Prophylaxis in Liver Transplant Recipients. Liver Transpl. 2009, 15, 842–858. [Google Scholar] [CrossRef] [Green Version]
- Singh, N.; Pruett, T.L.; Houston, S.; Muñoz, P.; Cacciarelli, T.V.; Wagener, M.M.; Husain, S. Invasive Aspergillosis in the Recipients of Liver Retransplantation. Liver Transplant. 2006, 12, 1205–1209. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.; Avery, R.K.; Munoz, P.; Pruett, T.L.; Alexander, B.; Jacobs, R.; Tollemar, J.G.; Dominguez, E.A.; Yu, C.M.; Paterson, D.L.; et al. Trends in Risk Profiles for and Mortality Associated with Invasive Aspergillosis among Liver Transplant Recipients. Clin. Infect. Dis. 2003, 36, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Husain, S.; Tollemar, J.; Dominguez, E.A.; Baumgarten, K.; Humar, A.; Paterson, D.L.; Wagener, M.M.; Kusne, S.; Singh, N. Changes in the Spectrum and Risk Factors for Invasive Candidiasis in Liver Transplant Recipients: Prospective, Multicenter, Case-Controlled Study. Transplantation 2003, 75, 2023–2029. [Google Scholar] [CrossRef]
- Dewi, I.M.; Janssen, N.A.; Rosati, D.; Bruno, M.; Netea, M.G.; Brüggemann, R.J.; Verweij, P.E.; van de Veerdonk, F.L. Invasive Pulmonary Aspergillosis Associated with Viral Pneumonitis. Curr. Opin. Microbiol. 2021, 62, 21–27. [Google Scholar] [CrossRef]
- De Boer, J.D.; Braat, A.E.; Putter, H.; De Vries, E.; Strassburg, C.H.; Máthé, Z.; Van Hoek, B.; Braun, F.; Van Den Berg, A.P.; Mikulic, D.; et al. Outcome of Liver Transplant Patients with High Urgent Priority: Are We Doing the Right Thing? Transplantation 2019, 103, 1181–1190. [Google Scholar] [CrossRef]
- Bongomin, F.; Gago, S.; Oladele, R.O.; Denning, D.W. Global and Multi-National Prevalence of Fungal Diseases—Estimate Precision. J. Fungi 2017, 3, 57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saliba, F.; Delvart, V.; Ichaï, P.; Kassis, N.; Botterel, F.; Mihaila, L.; Azoulay, D.; Adam, R.; Castaing, D.; Bretagne, S.; et al. Fungal Infections after Liver Transplantation: Outcomes and Risk Factors Revisited in the MELD Era. Clin. Transpl. 2013, 27, E454–E461. [Google Scholar] [CrossRef] [PubMed]
- Viehman, J.A.; Clancy, C.J.; Clarke, L.; Shields, R.K.; Silveira, F.P.; Kwak, E.J.; Vergidis, P.; Hughes, C.; Humar, A.; Nguyen, M.H. Surgical Site Infections after Liver Transplantation: Emergence of Multidrug-Resistant Bacteria and Implications for Prophylaxis and Treatment Strategies. Transplantation 2016, 100, 2107–2114. [Google Scholar] [CrossRef] [PubMed]
- Winston, D.J.; Pakrasi, A.; Busuttil, R.W. Prophylactic Fluconazole in Liver Transplant Recipients. A Randomized, Double-Blind, Placebo-Controlled Trial. Ann. Intern. Med. 1999, 131, 729–737. [Google Scholar] [CrossRef]
- Rogers, J.; Rohal, S.; Carrigan, D.R.; Kusne, S.; Knox, K.K.; Gayowski, T.; Wagener, M.M.; Fung, J.J.; Singh, N. Human Herpesvirus-6 in Liver Transplant Recipients: Role in Pathogenesis of Fungal Infections, Neurologic Complications, and Outcome. Transplantation 2000, 69, 2566–2573. [Google Scholar] [CrossRef]
- Evans, J.D.W.; Morris, P.J.; Knight, S.R. Antifungal Prophylaxis in Liver Transplantation: A Systematic Review and Network Meta-Analysis. Am. J. Transplant. 2014, 14, 2765–2776. [Google Scholar] [CrossRef]
- Aslam, S.; Rotstein, C. Candida Infections in Solid Organ Transplantation: Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin. Transpl. 2019, 33, e13623. [Google Scholar] [CrossRef]
- Fortún, J.; Martín-Dávila, P.; Montejo, M.; Muñoz, P.; Cisneros, J.M.; Ramos, A.; Aragón, C.; Blanes, M.; San Juan, R.; Gavaldá, J.; et al. Prophylaxis with Caspofungin for Invasive Fungal Infections in High-Risk Liver Transplant Recipients. Transplantation 2009, 87, 424–435. [Google Scholar] [CrossRef]
- Glöckner, A. Treatment and Prophylaxis of Invasive Candidiasis with Anidulafungin, Caspofungin and Micafungin—Review of the Literature. Eur. J. Med. Res. 2011, 16, 167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shields, R.K.; Nguyen, M.H.; Press, E.G.; Clancya, C.J. Abdominal Candidiasis Is a Hidden Reservoir of Echinocandin Resistance. Antimicrob. Agents Chemother. 2014, 58, 7601. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, X.; Liu, D.; Pan, Y.; Li, Y. Pharmacokinetic/Pharmacodynamics Variability of Echinocandins in Critically Ill Patients: A Systematic Review and Meta-Analysis. J. Clin. Pharm. 2020, 45, 1207–1217. [Google Scholar] [CrossRef]
- Arendrup, M.C. Epidemiology of Invasive Candidiasis. Curr. Opin. Crit. Care 2010, 16, 445–452. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, J.; Fisher, M.C. Global Epidemiology of Emerging Candida Auris. Curr. Opin. Microbiol. 2019, 52, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Blum, G.; Perkhofer, S.; Grif, K.; Mayr, A.; Kropshofer, G.; Nachbaur, D.; Kafka-Ritsch, R.; Dierich, M.P.; Lass-Flörl, C. A 1-Year Aspergillus Terreus Surveillance Study at the University Hospital of Innsbruck: Molecular Typing of Environmental and Clinical Isolates. Clin. Microbiol. Infect. 2008, 14, 1146–1151. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fisher, M.C.; Denning, D.W. The WHO Fungal Priority Pathogens List as a Game-Changer. Nat. Rev. Microbiol. 2023, 21, 211–212. [Google Scholar] [CrossRef]
- Singer, M.; Deutschman, C.S.; Seymour, C.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801. [Google Scholar] [CrossRef]


| Patient Characteristics | All Patients (n = 214) | Survivors (n = 197) | Non-Survivors (n = 17) | p-Value | Missing (n/Total) | |
|---|---|---|---|---|---|---|
| Age (years) | 57.3 ± 11.1 | 57.4 ± 11.0 | 55.9 ± 13.2 | 0.582 | 0/214 | |
| Male sex | 163 (76.2) | 152 (77.2) | 11 (64.7) | 0.346 | 0/214 | |
| Height (cm) | 174.2 ± 8.5 | 174.4 ± 8.4 | 171.7 ± 9.9 | 0.209 | 0/214 | |
| Weight (kg) | 81.4 ± 16.3 | 81.9 ± 16.1 | 75.4 ± 18.6 | 0.114 | 0/214 | |
| Body mass index (kg/m2) | 26.8 ± 5.0 | 26.9 ± 4.9 | 25.4 ± 5.3 | 0.236 | 0/214 | |
| SAPS III score | 44.8 ± 8.5 | 44.6 ± 8.6 | 47.3 ± 7.7 | 0.240 | 6/214 | |
| MELD score | 13 (6–40) | 13 (6–40) | 13.5 (6–39) | 0.846 | 10/214 | |
| Charlson comorbidity index | 4 (0–10) | 4 (0–10) | 5.5 (1–9) | 0.213 | 2/214 | |
| Underlying Disease | 0.033 | 0/214 | ||||
| Acute liver failure | 10 (4.7) | 7 (3.6) | 3 (17.6) | 0.035 | ||
| Tumors | 89 (41.6) | 84 (42.6) | 5 (29.4) | 0.319 | ||
| Hepatocellular carcinoma | 82 (92.1) | 77 (91.7) | 5 (100.0) | 0.604 | ||
| Cholangiocellular carcinoma | 3 (3.4) | 3 (3.6) | 0 (0.0) | 1.000 | ||
| Neuroendocrine tumor | 3 (3.4) | 3 (3.6) | 0 (0.0) | 1.000 | ||
| Polycystic liver disease | 1 (1.1) | 1 (1.2) | 0 (0.0) | 1.000 | ||
| Cirrhosis | 68 (31.8) | 64 (32.5) | 4 (23.5) | 0.591 | ||
| Alcoholic cirrhosis | 51 (23.8) | 49 (24.9) | 2 (11.8) | 0.372 | ||
| Virus related cirrhosis | 9 (4.2) | 9 (4.6) | 0 (0.0) | 1.000 | ||
| Autoimmune cirrhosis | 8 (3.7) | 6 (3.0) | 2 (11.8) | 0.125 | ||
| Cholestatic disease | 15 (7.0) | 14 (7.1) | 1 (5.9) | 1.000 | ||
| Nonalcoholic steatohepatitis | 14 (6.5) | 12 (6.1) | 2 (11.8) | 0.307 | ||
| Metabolic disease | 10 (4.7) | 9 (4.6) | 1 (5.9) | 0.571 | ||
| Budd–Chiari syndrome | 6 (2.8) | 6 (3.0) | 0 (0.0) | 1.000 | ||
| Other | 2 (0.9) | 1 (0.5) | 1 (5.9) | 0.153 | ||
| Operative Characteristics | All Patients (n = 214) | Survivors (n = 197) | Non-Survivors (n = 17) | p-Value | Missing (n/Total) | |
|---|---|---|---|---|---|---|
| Operation duration (minutes) | 355 (173–783) | 353 (173–783) | 363 (175–783) | 0.435 | 0/214 | |
| Cold ischemia time (minutes) | 435 (125–1199) | 441 (125–1199) | 413 (240–1040) | 0.867 | 0/214 | |
| Intraoperative blood transfusion (mL) | 2412 (0–32,740) | 2358 (0–21,200) | 3300 (455–32,740) | 0.066 | 0/214 | |
| Type of graft | 0/214 | |||||
| Whole liver | 208 (97.2) | 192 (97.5) | 16 (94.1) | 0.395 | ||
| Split liver | 6 (2.8) | 5 (2.5) | 1 (5.9) | |||
| Type of biliary anastomosis | 0/214 | |||||
| Duct-to-duct | 199 (93.0) | 185 (93.9) | 14 (82.4) | 0.104 | ||
| Roux-y-choledochojejunostomy | 15 (7.0) | 12 (6.1) | 3 (17.6) | |||
| Type of venous anastomosis | 0/214 | |||||
| Retrocaval resection | 205 (97.2) | 190 (97.9) | 15 (88.2) | 0.076 | ||
| Piggyback | 6 (2.8) | 4 (2.1) | 2 (11.8) | |||
| Donation and preservation characteristics | ||||||
| Type of donation | 0/214 | |||||
| Standard criteria donation | 46 (21.5) | 42 (21.3) | 4 (23.5) | 0.765 | ||
| Extended criteria donation | 168 (78.5) | 155 (78.7) | 13 (76.5) | |||
| Type of donor death | 0/214 | |||||
| DBD | 196 (91.6) | 182 (92.4) | 14 (82.4) | 0.160 | ||
| DCD | 18 (8.4) | 15 (7.6) | 3 (17.6) | |||
| Preservation | 0/214 | |||||
| Static cold storage | 144 (67.3) | 135 (68.5) | 9 (52.9) | 0.191 | ||
| Normothermic machine perfusion | 70 (32.7) | 62 (31.5) | 8 (47.1) | |||
| Allocation | ||||||
| Local | 42 (20.2) | 39 (20.4) | 3 (17.6) | 6/208 | ||
| Regional | 109 (52.4) | 102 (53.4) | 7 (41.2) | 0.435 | ||
| National | 57 (27.4) | 50 (26.2) | 7 (41.2) | |||
| Postoperative Complications | All Patients (n = 214) | Survivors (n = 197) | Non-Survivors (n = 17) | p-Value | Missing (n/Total) | |
|---|---|---|---|---|---|---|
| Length of ICU stay (days) | 5 (1–117) | 2 (1–117) | 6 (1–40) | 0.211 | 1/214 | |
| Graft dysfunction | 0/214 | |||||
| Primary non-function | 2 (1.1) | 2 (1.2) | 0 (0.0) | 1.000 | ||
| Early allograft dysfunction | 56 (30.9) | 50 (30.5) | 6 (35.3) | 0.784 | ||
| Immunologic complications | 0/214 | |||||
| Acute rejection | 10 (5.8) | 8 (5.1) | 2 (11.8) | 0.256 | ||
| Graft-versus-host disease | 4 (2.3) | 2 (1.3) | 2 (11.8) | 0.049 | ||
| Vascular complications | 0/214 | |||||
| Hepatic artery thrombosis | 7 (3.4) | 6 (3.2) | 1 (6.3) | 0.442 | ||
| Portal vein thrombosis | 6 (3.6) | 4 (2.5) | 2 (18.2) | 0.051 | ||
| Hepatic vein thrombosis | 9 (5.4) | 8 (5.1) | 1 (9.1) | 0.465 | ||
| Bile stricture | 4 (2.2) | 2 (1.2) | 2 (11.8) | 0.043 | 0/214 | |
| Reoperation | 74 (34.6) | 63 (32.0) | 11 (64.7) | 0.014 | 0/214 | |
| Bile leak | 20 (10.8) | 18 (10.7) | 2 (11.8) | 1.000 | ||
| Hemorrhage | 31 (16.8) | 23 (13.7) | 8 (47.1) | 0.002 | ||
| Re-transplantation | 6 (3.0) | 6 (2.8) | 0 (0.0) | 1.000 | ||
| Other | 8 (4.4) | 7 (4.1) | 1 (7.1) | 0.478 | ||
| Acute kidney injury | 94 (43.9) | 82 (41.6) | 12 (70.6) | 0.039 | 0/214 | |
| Sepsis | 14 (8.1) | 4 (2.6) | 10 (58.8) | <0.001 | 0/214 | |
| CMV viremia | 61 (28.5) | 52 (26.4) | 9 (52.9) | 0.027 | 0/214 | |
| Invasive fungal infection | 26 (12.1) | 17 (8.6) | 9 (52.9) | <0.001 | 0/214 | |
| Complication | Number of Patients |
|---|---|
| Myocardial infarction | 2 (2) |
| Posterior reversible encephalopathy syndrome and central pontine myelinolysis | 1 |
| Cerebrovascular accident | 2 (2) |
| Acute kidney failure | 12 |
| Pancreatitis | 1 |
| Gastrointestinal perforation | 1 |
| Primary non-function | 0 |
| Early allograft dysfunction | 6 |
| Acute cellular rejection | 2 |
| Graft-versus-host-disease | 2 |
| Hospital-acquired and ventilator-associated pneumonia | 6 (2) |
| Surgical site infection | 7 (2) |
| Catheter-associated urinary tract infection | 1 (1) |
| Central line-related bloodstream infection | 5 |
| Complicated skin and soft tissue infection | 1 |
| Sepsis | 10 (10) |
| Invasive fungal infection | 8 (5) |
| CMV viremia | 9 |
| Reoperation | 11 |
| Bile leak | 2 |
| Hemorrhage | 8 |
| Hepatic artery thrombosis | 2 (2) |
| Portal vein thrombosis | 3 |
| Hepatic vein thrombosis | 1 |
| Primary Infection | Co-Infections | ||
|---|---|---|---|
| VAP (A. fumigatus) | IAC + BSI (C. dubliensis) | VAP (Influenza) | SSI (Citrobacter/MDR) |
| VAP (A. fumigatus) | IAC + BSI (C. orthopsilosis, C. krusei) | VAP (Influenza) | VAP (E. coli/MDR) |
| VAP (A. fumigatus) | UTI (C. glabrata) | - | - |
| VAP (A. fumigatus) | - | - | - |
| VAP (A. fumigatus) | VAP (Fusarium spp., Penicillium spp.) | VAP/Colitis (CMV) | - |
| Non-Dependent Variable | B-Coefficient | p-Value | HR | 95% Confidence Interval | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Underlying disease (reference category: malignancy and other tumors) | ||||||
| Alcoholic Cirrhosis | −0.694 | 0.478 | 0.50 | 0.07 | 3.40 | |
| Virus related Cirrhosis | - | - | - | - | - | |
| Nonalcoholic Steatohepatitis | 1.541 | 0.089 | 4.67 | 0.79 | 27.52 | |
| Budd-Chiari Syndrome | - | - | - | - | - | |
| Acute Liver Failure | 1.146 | 0.252 | 3.14 | 0.44 | 22.33 | |
| Cholestatic Disease | 0.098 | 0.932 | 1.10 | 0.12 | 10.54 | |
| Autoimmune Cirrhosis | 1.033 | 0.328 | 2.81 | 0.36 | 22.24 | |
| Metabolic Disease | 0.904 | 0.420 | 2.47 | 0.28 | 22.21 | |
| Other | 0.038 | 0.979 | 1.04 | 0.06 | 17.18 | |
| Invasive Fungal Infection | 1.534 | 0.032 | 4.64 | 1.14 | 18.78 | |
| Roux-Y-Choledochojejunostomy | −0.133 | 0.807 | 0.88 | 0.30 | 2.56 | |
| Piggyback-Anastomosis | 1.469 | 0.226 | 4.35 | 0.40 | 46.87 | |
| Relaparotomy | 0.157 | 0.823 | 1.17 | 0.30 | 4.62 | |
| Postoperative dialysis | 0.460 | 0.457 | 1.58 | 0.47 | 5.32 | |
| CMV viremia | 0.407 | 0.495 | 1.50 | 0.47 | 4.84 | |
| Graft-versus-host disease | 1.011 | 0.381 | 2.75 | 0.29 | 26.34 | |
| Bile stricture | 0.926 | 0.354 | 2.53 | 0.36 | 17.89 | |
| Portal vein thrombosis | 0.784 | 0.385 | 2.19 | 0.37 | 12.84 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Breitkopf, R.; Treml, B.; Bukumiric, Z.; Innerhofer, N.; Fodor, M.; Rajsic, S. Invasive Fungal Infections: The Early Killer after Liver Transplantation. J. Fungi 2023, 9, 655. https://doi.org/10.3390/jof9060655
Breitkopf R, Treml B, Bukumiric Z, Innerhofer N, Fodor M, Rajsic S. Invasive Fungal Infections: The Early Killer after Liver Transplantation. Journal of Fungi. 2023; 9(6):655. https://doi.org/10.3390/jof9060655
Chicago/Turabian StyleBreitkopf, Robert, Benedikt Treml, Zoran Bukumiric, Nicole Innerhofer, Margot Fodor, and Sasa Rajsic. 2023. "Invasive Fungal Infections: The Early Killer after Liver Transplantation" Journal of Fungi 9, no. 6: 655. https://doi.org/10.3390/jof9060655
APA StyleBreitkopf, R., Treml, B., Bukumiric, Z., Innerhofer, N., Fodor, M., & Rajsic, S. (2023). Invasive Fungal Infections: The Early Killer after Liver Transplantation. Journal of Fungi, 9(6), 655. https://doi.org/10.3390/jof9060655







