In Vitro Physicochemical and Pharmacokinetic Properties of Bevacizumab Dissolved in Silicone Oils Compared to Hydrogel-Substitutes and Porcine Vitreous Bodies
Abstract
:1. Introduction
2. Results and Discussion
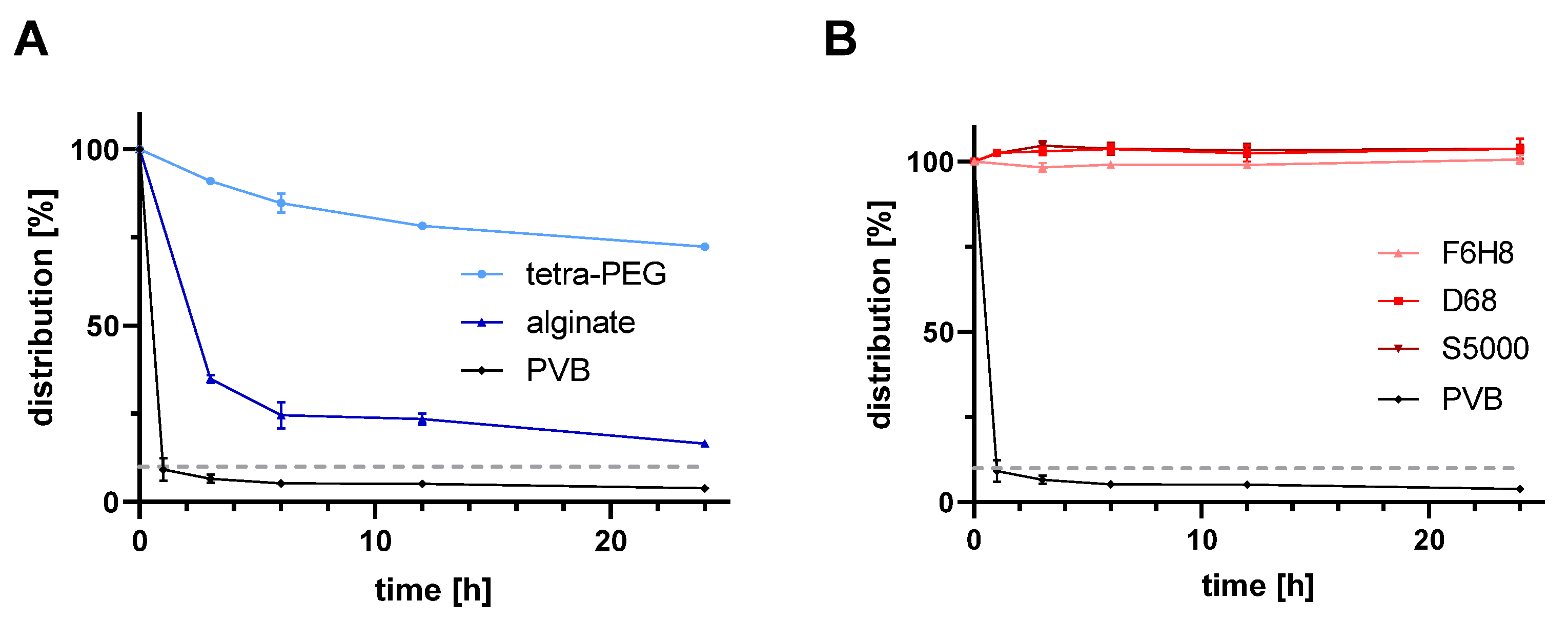
2.1. In Vitro Pharmacokinetics of Bevacizumab for All Tested Vitreous Body Substitutes
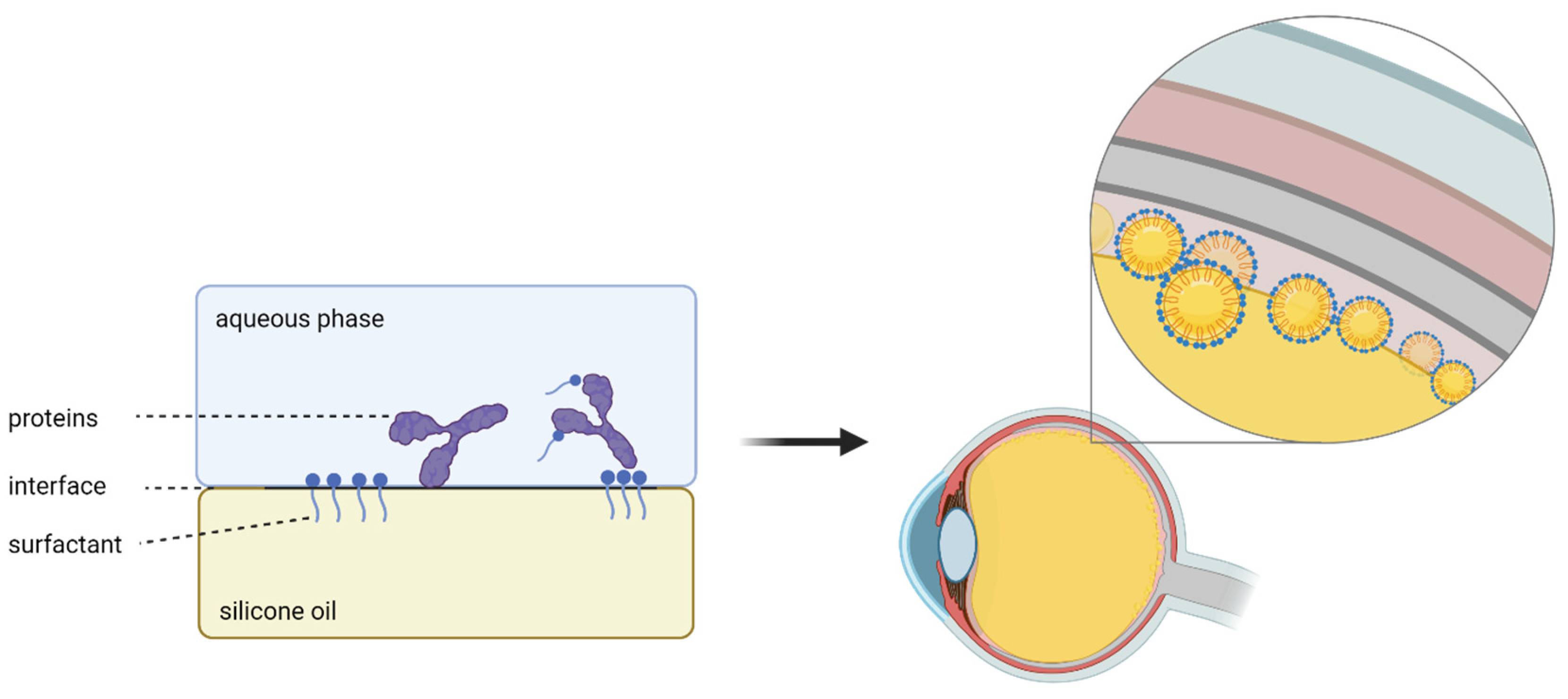
2.2. Influence of Bevacizumab on the Interfacial Tension between the Aqueous Phase and Light and Heavy Silicone Oils
2.3. Discussion
2.3.1. Summary of Results
2.3.2. Silicone Oil and Intravitreal Injections
2.3.3. Interfacial Tension between Silicone Oil and Aqueous Phase
2.3.4. Bevacizumab and Hydrogels
3. Conclusions
4. Materials and Methods
4.1. Preparation of the Aqueous Phase
4.2. In Vitro Posterior Segment Model
4.3. Quantification of Bevacizumab Concentrations
4.4. Synthesis of Hydrogels
4.4.1. Second-Generation Vitreous Body Replacement Hydrogel
4.4.2. Third-Generation Vitreous Body Replacement Hydrogel
4.5. Surface Tension Measurement
4.6. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hammer, M.; Schickhardt, S.; Munro, D.J.; Scheuerle, A.; Mayer, C.S.; Auffarth, G.U. Physicochemical Properties of Explanted Silicone Oil after Use as an Intraocular Tamponade. Transl. Vis. Sci. Technol. 2022, 11, 3. [Google Scholar] [CrossRef] [PubMed]
- Hammer, M.; Schickhardt, S.; Munro, D.; Scheuerle, A.; Khoramnia, R.; Uhl, P.; Auffarth, G.U. New approaches to explanting high-viscosity silicone oil in retinal surgery—Polyimide cannulas vs extraction sleeves vs a luer-trocar. Int. J. Retin. Vitr. 2023, 9, 43. [Google Scholar] [CrossRef]
- Hammer, M.; Schickhardt, S.K.; Munro, D.; Khoramnia, R.; Scheuerle, A.; Mayer, C.S.; Auffarth, G.U. The novel use of high-flow polyimide cannulas to improve silicone oil injectability in vitreoretinal surgery. Retina 2022, 42, 1170–1175. [Google Scholar] [CrossRef] [PubMed]
- Hammer, M.; Schickhardt, S.K.; Merz, P.R.; Khoramnia, R.; Scheuerle, A.F.; Mier, W.; Uhl, P.; Auffarth, G.U. Intravitreal Application: Physicochemical Properties of Drugs Dissolved in Silicone Oils of Different Density in Comparison to the Porcine Vitreous Body. Pharmaceutics 2022, 14, 1364. [Google Scholar] [CrossRef] [PubMed]
- Hammer, M.; Herth, J.; Muuss, M.; Schickhardt, S.; Scheuerle, A.; Khoramnia, R.; Łabuz, G.; Uhl, P.; Auffarth, G.U. Forward Light Scattering of First to Third Generation Vitreous Body Replacement Hydrogels after Surgical Application Compared to Conventional Silicone Oils and Vitreous Body. Gels 2023, 9, 837. [Google Scholar] [CrossRef] [PubMed]
- Chirila, T.V.; Harkin, D.G. (Eds.) Biomaterials and Regenerative Medicine in Ophthalmology, 2nd ed.; Woodhead Publishing Series in Biomaterials; Woodhead Publishing: Cambridge, UK, 2016; pp. xiii–xviii. [Google Scholar]
- Schulz, A.; Januschowski, K.; Szurman, P. Novel vitreous substitutes: The next frontier in vitreoretinal surgery. Curr. Opin. Ophthalmol. 2021, 32, 288–293. [Google Scholar] [CrossRef] [PubMed]
- Calciu-Rusu, D.; Rothfuss, E.; Eckelt, J.; Haase, T.; Dick, H.B.; Wolf, B.A. Rheology of Sodium Hyaluronate Saline Solutions for Ophthalmic Use. Biomacromolecules 2007, 8, 1287–1292. [Google Scholar] [CrossRef] [PubMed]
- Baino, F. Towards an ideal biomaterial for vitreous replacement: Historical overview and future trends. Acta Biomater. 2011, 7, 921–935. [Google Scholar] [CrossRef]
- Lin, Q.; Lim, J.Y.C.; Xue, K.; Su, X.; Loh, X.J. Polymeric hydrogels as a vitreous replacement strategy in the eye. Biomaterials 2021, 268, 120547. [Google Scholar] [CrossRef]
- Prinz, A.; Fennes, C.; Buehl, W.; Findl, O. Efficacy of ophthalmic viscosurgical devices in maintaining corneal epithelial hydration and clarity: In vitro assessment. J. Cataract Refract. Surg. 2012, 38, 2154–2159. [Google Scholar] [CrossRef]
- Arshinoff, S.A. Dispersive-cohesive viscoelastic soft shell technique. J. Cataract Refract. Surg. 1999, 25, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Poyer, J.F.; Chan, K.Y.; Arshinoff, S.A. Quantitative method to determine the cohesion of viscoelastic agents by dynamic aspiration. J. Cataract Refract. Surg. 1998, 24, 1130–1135. [Google Scholar] [CrossRef] [PubMed]
- Schnichels, S.; Schneider, N.; Hohenadl, C.; Hurst, J.; Schatz, A.; Januschowski, K.; Spitzer, M.S. Efficacy of two different thiol-modified crosslinked hyaluronate formulations as vitreous replacement compared to silicone oil in a model of retinal detachment. PLoS ONE 2017, 12, e0172895. [Google Scholar] [CrossRef] [PubMed]
- Hurst, J.; Rickmann, A.; Heider, N.; Hohenadl, C.; Reither, C.; Schatz, A.; Schnichels, S.; Januschowski, K.; Spitzer, M.S. Long-Term Biocompatibility of a Highly Viscously Thiol-Modified Cross-Linked Hyaluronate as a Novel Vitreous Body Substitute. Front. Pharmacol. 2022, 13, 817353. [Google Scholar] [CrossRef] [PubMed]
- Schulz, A.; Rickmann, A.; Wahl, S.; Germann, A.; Stanzel, B.V.; Januschowski, K.; Szurman, P. Alginate-and hyaluronic acid–based hydrogels as vitreous substitutes: An in vitro evaluation. Transl. Vis. Sci. Technol. 2020, 9, 34. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, K.; Okamoto, F.; Hoshi, S.; Katashima, T.; Zujur, D.C.; Li, X.; Shibayama, M.; Gilbert, E.P.; Chung, U.-I.; Ohba, S.; et al. Fast-forming hydrogel with ultralow polymeric content as an artificial vitreous body. Nat. Biomed. Eng. 2017, 1, 0044. [Google Scholar] [CrossRef]
- Schramm, C.; Spitzer, M.S.; Henke-Fahle, S.; Steinmetz, G.; Januschowski, K.; Heiduschka, P.; Geis-Gerstorfer, J.; Biedermann, T.; Bartz-Schmidt, K.U.; Szurman, P. The Cross-linked Biopolymer Hyaluronic Acid as an Artificial Vitreous Substitute. Investig. Ophthalmol. Vis. Sci. 2012, 53, 613–621. [Google Scholar] [CrossRef] [PubMed]
- Tram, N.K.; Jiang, P.; Torres-Flores, T.C.; Jacobs, K.M.; Chandler, H.L.; Swindle-Reilly, K.E. A Hydrogel Vitreous Substitute that Releases Antioxidant. Macromol. Biosci. 2020, 20, 1900305. [Google Scholar] [CrossRef]
- Osawa, S.; Oshima, Y. 27-Gauge Vitrectomy. In Microincision Vitrectomy Surgery: Emerging Techniques and Technology; Oh, H., Oshima, Y., Eds.; S. Karger AG: Basel, Switzerland, 2014; Volume 54. [Google Scholar] [CrossRef]
- Charles, S.; Ho, A.C.; Dugel, P.U.; Riemann, C.D.; Berrocal, M.H.; Gupta, S.; Hamilton, C.; Abulon, D.J.K. Clinical comparison of 27-gauge and 23-gauge instruments on the outcomes of pars plana vitrectomy surgery for the treatment of vitreoretinal diseases. Curr. Opin. Ophthalmol. 2020, 31, 185–191. [Google Scholar] [CrossRef]
- Barth, H.; Crafoord, S.; Andréasson, S.; Ghosh, F. A cross-linked hyaluronic acid hydrogel (Healaflow®) as a novel vitreous substitute. Graefe’s Arch. Clin. Exp. Ophthalmol. 2016, 254, 697–703. [Google Scholar] [CrossRef]
- Barth, H.; Crafoord, S.; Ghosh, F. A New Retinal Detachment Treatment Model for Evaluation of Vitreous Tamponades. Curr. Eye Res. 2021, 46, 373–379. [Google Scholar] [CrossRef] [PubMed]
- Ren, X.J.; Bu, S.C.; Wu, D.; Liu, B.S.; Yang, F.H.; Hu, B.J.; Liu, J.P.; Zhang, X.M.; Dong, L.J.; Zheng, C.Z.; et al. PATCHING RETINAL BREAKS WITH HEALAFLOW IN 27-GAUGE VITRECTOMY FOR THE TREATMENT OF RHEGMATOGENOUS RETINAL DETACHMENT. Retina 2020, 40, 1900–1908. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Peng, Y.; Yang, C.; Liu, W.; Han, B. The feasibility study of an in situ marine polysaccharide-based hydrogel as the vitreous substitute. J. Biomed. Mater. Res. Part A 2018, 106, 1997–2006. [Google Scholar] [CrossRef] [PubMed]
- Su, W.-Y.; Chen, K.-H.; Chen, Y.-C.; Lee, Y.-H.; Tseng, C.-L.; Lin, F.-H. An Injectable Oxidated Hyaluronic Acid/Adipic Acid Dihydrazide Hydrogel as a Vitreous Substitute. J. Biomater. Sci. Polym. Ed. 2011, 22, 1777–1797. [Google Scholar] [CrossRef]
- Ferrara, N. Vascular Endothelial Growth Factor: Basic Science and Clinical Progress. Endocr. Rev. 2004, 25, 581–611. [Google Scholar] [CrossRef]
- Keating, G.M. Bevacizumab: A Review of Its Use in Advanced Cancer. Drugs 2014, 74, 1891–1925. [Google Scholar] [CrossRef] [PubMed]
- Pindrus, M.; Shire, S.J.; Kelley, R.F.; Demeule, B.; Wong, R.; Xu, Y.; Yadav, S. Solubility Challenges in High Concentration Monoclonal Antibody Formulations: Relationship with Amino Acid Sequence and Intermolecular Interactions. Mol. Pharm. 2015, 12, 3896–3907. [Google Scholar] [CrossRef] [PubMed]
- Roche Registration GmbH. Fachinformation Avastin® 008726-86807. Available online: https://www.fachinfo.de/api/public/fachinfo/pdf/008726 (accessed on 27 July 2024).
- Falavarjani, K.G.; Modarres, M.; Nazari, H. Therapeutic effect of bevacizumab injected into the silicone oil in eyes with neovascular glaucoma after vitrectomy for advanced diabetic retinopathy. Eye 2010, 24, 717–719. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; You, Y.; Du, W.; Zhao, C.; Li, J.; Mao, J.; Chen, H.; Cheng, L. Ocular Pharmacokinetics of Bevacizumab in Vitrectomized Eyes with Silicone Oil Tamponade. Investig. Opthalmology Vis. Sci. 2012, 53, 5221. [Google Scholar] [CrossRef]
- Leung, E.H.; Stout, J.T. Antibiotics and antifungals in silicone oil. Int. J. Retin. Vitr. 2019, 5, 50. [Google Scholar] [CrossRef]
- Hira, D.; Kitagawa, T.; Imamura, T.; Kakinoki, M.; Ueshima, S.; Okano, T.; Ohji, M.; Kakumoto, M.; Terada, T. Impact of silicone oil tamponade on intravitreally injected vancomycin pharmacokinetics in cynomolgus monkey eyes. Int. J. Pharm. 2021, 609, 121185. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Kearns, V.R.; Zhou, L.; Sandinha, T.; Lam, W.C.; Steel, D.H.; Chan, Y.K. Silicone oil in vitreoretinal surgery: Indications, complications, new developments and alternative long-term tamponade agents. Acta Ophthalmol. 2021, 99, 240–250. [Google Scholar] [CrossRef] [PubMed]
- Nepita, I.; Repetto, R.; Pralits, J.O.; Romano, M.R.; Ravera, F.; Santini, E.; Liggieri, L. The Role of Endogenous Proteins on the Emulsification of Silicone Oils Used in Vitreoretinal Surgery. BioMed Res. Int. 2020, 2020, 2915010. [Google Scholar] [CrossRef]
- Chan, Y.K.; Ng, C.O.; Knox, P.C.; Garvey, M.J.; Williams, R.L.; Wong, D. Emulsification of Silicone Oil and Eye Movements. Investig. Ophthalmol. Vis. Sci. 2011, 52, 9721–9727. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Zhao, X. Alginate hydrogel dressings for advanced wound management. Int. J. Biol. Macromol. 2020, 162, 1414–1428. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.-Y.; Pang, W.-J.; Wen, Z.-N.; Xiang, W.-P. Changes in human umbilical vein endothelial cells induced by endothelial nitric oxide synthase traffic inducer. J. Huazhong Univ. Sci. Technol. Med. Sci. 2013, 33, 272–276. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Xu, X.; Yao, F.; Luo, Z.; Jin, L.; Xie, B.; Shi, S.; Ma, H.; Li, X.; Chen, H. In situ covalently cross-linked PEG hydrogel for ocular drug delivery applications. Int. J. Pharm. 2014, 470, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Ayazi, H.; Akhavan, O.; Raoufi, M.; Varshochian, R.; Hosseini Motlagh, N.S.; Atyabi, F. Graphene aerogel nanoparticles for in-situ loading/pH sensitive releasing anticancer drugs. Colloids Surf. B Biointerfaces 2020, 186, 110712. [Google Scholar] [CrossRef] [PubMed]
- Hammer, M.; Muuss, M.; Herbster, L.; Herth, J.; Scheuerle, A.; Khoramnia, R.; Łabuz, G.; Uhl, P.; Auffarth, G.U. Viscoelastic, Optical, and Surgical Properties of Vitreous Body Replacement Hydrogels After Aging Compared to Porcine Vitreous Bodies And Silicone Oils. Transl. Vis. Sci. Technol. 2024, 13, 5. [Google Scholar] [CrossRef]
- CIBIS, P.A.; BECKER, B.; OKUN, E.; CANAAN, S. The Use of Liquid Silicone in Retinal Detachment Surgery. Arch. Ophthalmol. 1962, 68, 590–599. [Google Scholar] [CrossRef]
- Russo, R.; Malinconico, M.; Santagata, G. Effect of Cross-Linking with Calcium Ions on the Physical Properties of Alginate Films. Biomacromolecules 2007, 8, 3193–3197. [Google Scholar] [CrossRef] [PubMed]





Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hammer, M.; Herth, J.; Herbster, L.; Böhmann, M.B.; Muuss, M.; Khoramnia, R.; Scheuerle, A.; Mier, W.; Wohlfart, S.; Auffarth, G.U.; et al. In Vitro Physicochemical and Pharmacokinetic Properties of Bevacizumab Dissolved in Silicone Oils Compared to Hydrogel-Substitutes and Porcine Vitreous Bodies. Gels 2024, 10, 501. https://doi.org/10.3390/gels10080501
Hammer M, Herth J, Herbster L, Böhmann MB, Muuss M, Khoramnia R, Scheuerle A, Mier W, Wohlfart S, Auffarth GU, et al. In Vitro Physicochemical and Pharmacokinetic Properties of Bevacizumab Dissolved in Silicone Oils Compared to Hydrogel-Substitutes and Porcine Vitreous Bodies. Gels. 2024; 10(8):501. https://doi.org/10.3390/gels10080501
Chicago/Turabian StyleHammer, Maximilian, Jonathan Herth, Lorenz Herbster, Manuel Ben Böhmann, Marcel Muuss, Ramin Khoramnia, Alexander Scheuerle, Walter Mier, Sabrina Wohlfart, Gerd Uwe Auffarth, and et al. 2024. "In Vitro Physicochemical and Pharmacokinetic Properties of Bevacizumab Dissolved in Silicone Oils Compared to Hydrogel-Substitutes and Porcine Vitreous Bodies" Gels 10, no. 8: 501. https://doi.org/10.3390/gels10080501






