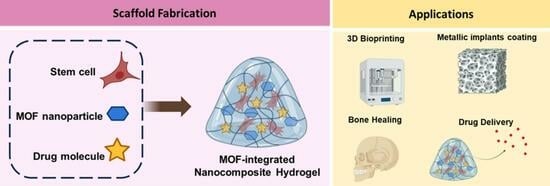
Metal Organic Framework-Incorporated Three-Dimensional (3D) Bio-Printable Hydrogels to Facilitate Bone Repair: Preparation and In Vitro Bioactivity Analysis
Abstract
:1. Introduction
2. Results and Discussion
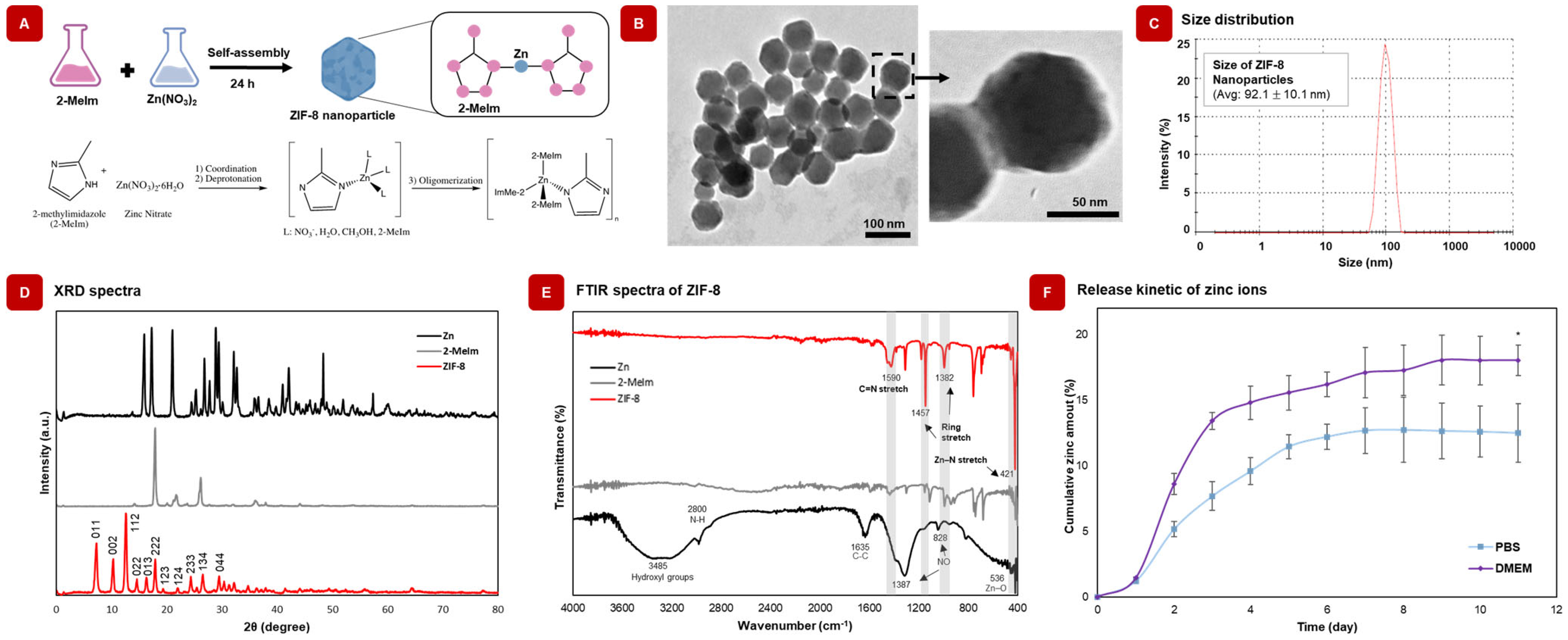
2.1. Physicochemical Characterization Confirms the Successful Synthesis of ZIF-8 Nanoparticles
2.2. ZIF-8 Nanoparticles Release Zn2+ Ions in Physiological Solutions
2.3. Composition of GelMA Plays a Key Role on the Printability of GelMA/ZIF-8 Hydrogels
2.4. Exposure Time and Power Have a Profound Effect on Shape Retention of 3D Printed GelMA/ZIF-8 Hydrogels
2.5. Integration of ZIF-8 Nanoparticles in GelMA Alters the Physicochemical Behavior of the Pristine Hydrogel
2.5.1. GelMA/ZIF-8 Hydrogels Display Lower Swelling Ratio When Compared to GelMA Hydrogels
2.5.2. GelMA/ZIF-8 Hydrogels Degraded Slower than GelMA Hydrogels
2.5.3. Presence of ZIF-8 in GelMA/ZIF-8 Hydrogel Was Confirmed Using FTIR Analysis
2.5.4. SEM Images and Elemental Mapping Demonstrated the Successful Integration of ZIF-8 in GelMA/ZIF-8 Hydrogel
2.5.5. Presence of ZIF-8 in GelMA/ZIF-8 Hydrogels Was Further Confirmed with EDX Analysis
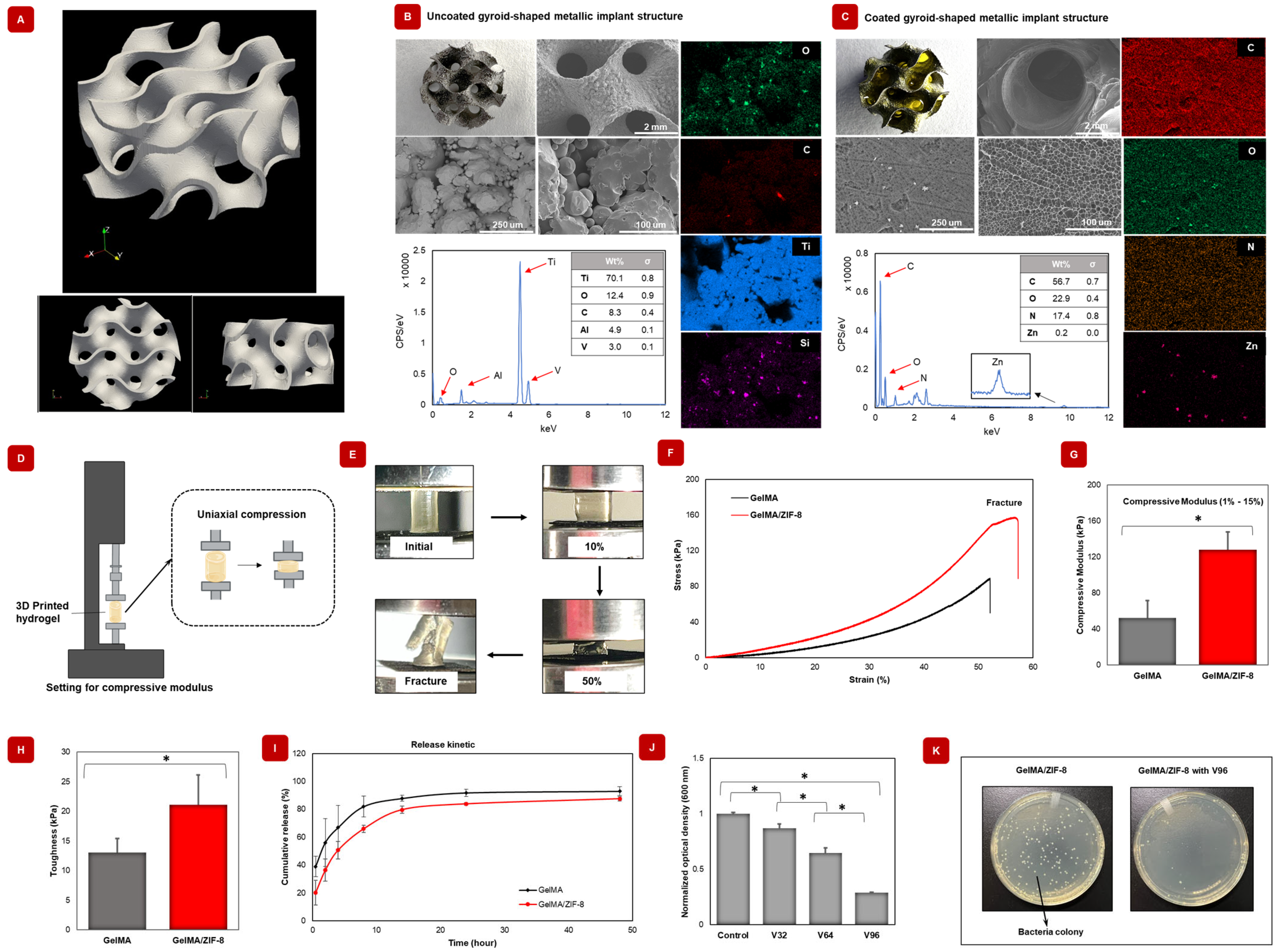
2.6. Orthopedic Metallic Implants Can Be Coated with GelMA/ZIF-8 Hydrogels
2.7. GelMA/ZIF-8 Hydrogels Displayed Superior Mechanical Strength and Toughness When Compared to GelMA Hydrogels
2.8. GelMA/ZIF-8 Hydrogels Sustain the Release of Model Antibiotic Vancomycin at Physiological Conditions
2.9. Antioxidant Agent-Loaded Nanocomposite Hydrogels Can Scavenge Free Radicals
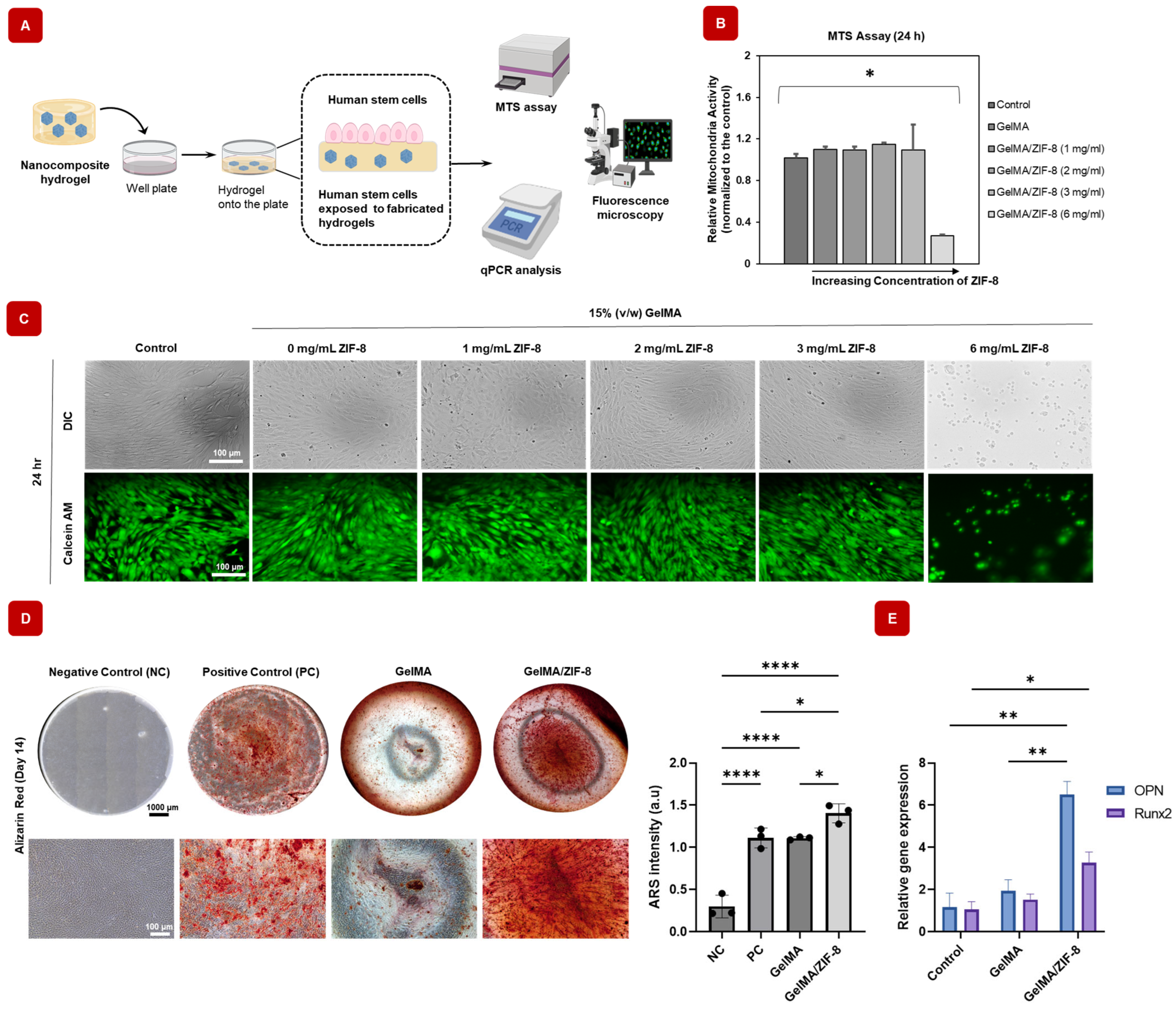
2.10. GelMA/ZIF-8 Hydrogels Show Excellent Cyto-Compatibility and Osteogenic Differentiation Abilities
2.10.1. In Vitro Cyto-Compatibility of Mineral-Based Nanocomposite Hydrogels
2.10.2. GelMA/ZIF-8 Hydrogels Can Differentiate hASCs toward Osteogenic Lineage
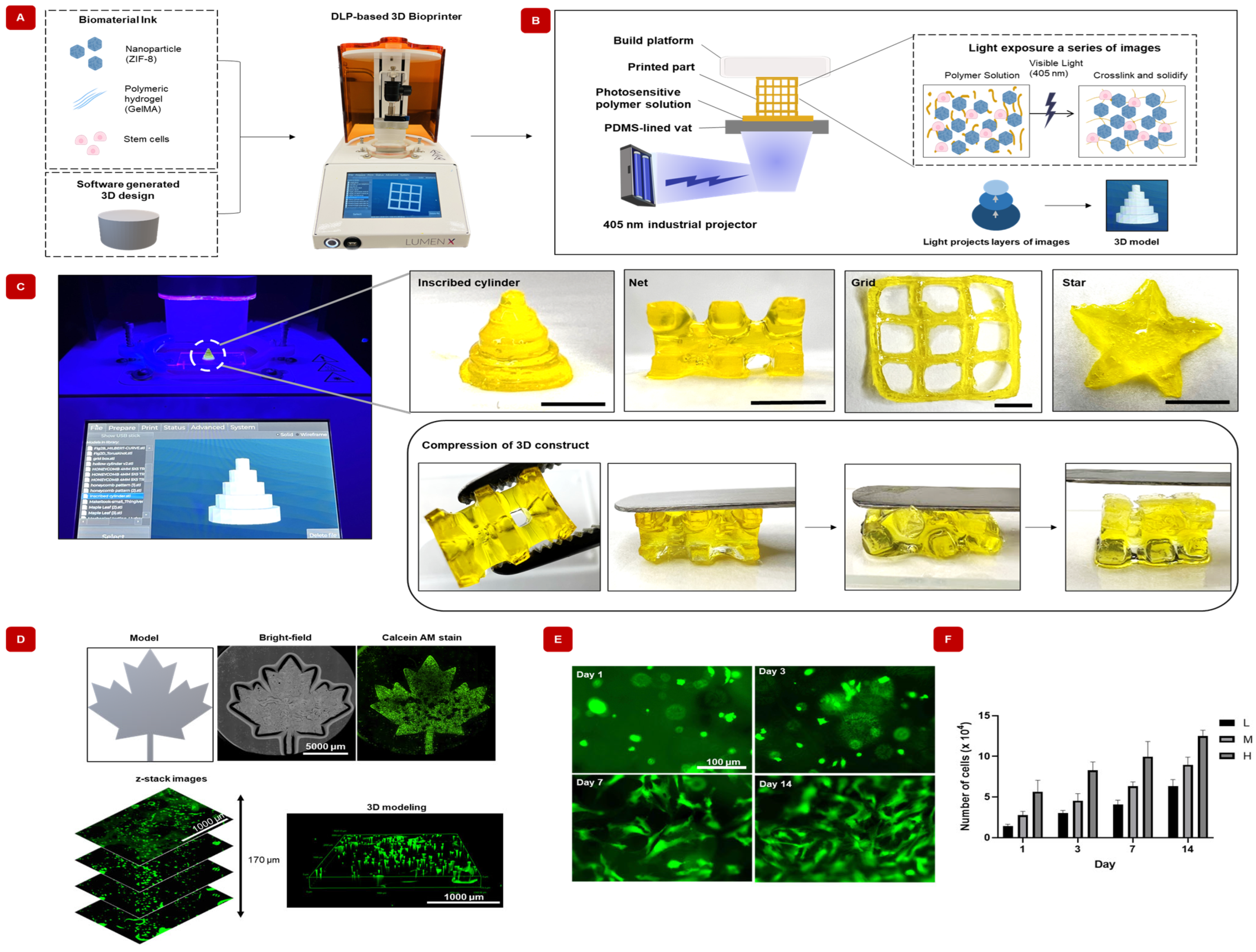
2.10.3. Complex Shapes of GelMA/ZIF-8 Hydrogels Can Be Fabricated Using DLP-Based 3D Bio-Printing
3. Conclusions
4. Materials and Methods
4.1. Preparation of GelMA Pregel Solution
4.2. Preparation of ZIF-8 Nanoparticles
4.3. Electron Microscopy to Determine Morphology of ZIF-8 Nanoparticles and GelMA/ZIF-8 Hydrogels
4.4. Zeta Potential and Dynamic Light Scattering (DLS) Analysis of ZIF-8 Nanoparticles
4.5. DLP-Based 3D Bio-Printing of GelMA/ZIF-8 Hydrogels
4.5.1. Preparation of Bio-ink
4.5.2. 3D Bio-Printing of GelMA/ZIF-8 Hydrogels Using LumenXTM
4.5.3. Lyophilization of Hydrogels
4.5.4. Physical Characterization: Swelling
- Equation (1): Swelling Ratio (%)
4.5.5. Physical Characterization: Degradation
- Equation (2): Degradation rate (%)
4.5.6. Chemical Characterization: Fourier Transformed Infrared (FTIR)
4.5.7. Mechanical Characterization of GelMA/ZIF-8 Hydrogels
- Equation (3): Toughness (kPa)
4.6. Zinc Ion Release from ZIF-8 Nanoparticles
4.7. Antioxidant Release from GelMA/ZIF-8 Hydrogels
- Equation (4): % scavenging activity of DPPH
4.8. Model Antibiotic Release from GelMA/ZIF-8 Hydrogel
- Equation (5): Cumulative drug release (%)
4.9. Antibacterial Efficacy of GelMA/ZIF-8 Hydrogel
4.10. Coating Titanium Implants with GelMA/ZIF-8 Hydrogels
4.10.1. Preparation of Gyroid-Shaped Titanium Implants
4.10.2. Coating of Gyroids with GelMA/ZIF-8 Hydrogels
4.11. Cyto-Compatibility and Bio-Functionality of GelMA/ZIF-8 Hydrogels
4.11.1. In Vitro Cell Culture
4.11.2. Cell Proliferation and Cyto-Compatibility
4.11.3. Determining Cell Viability by Calcein Acetoxymethyl (Calcein-AM) Staining
4.11.4. Determining Osteogenic Differentiation of Stem Cells Using Alizarin Red S (ARS) Staining
4.11.5. Quantifying the Ability of GelMA/ZIF-8 Hydrogels to Promote Osteogenic Differentiation of Stem Cells Using Real-Time Quantitative Polymerase Chain Reaction (RT-qPCR) Analysis
4.12. Evaluating Cell Viability in 3D Bio-printing through Live/Dead Cell Staining
4.13. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bai, X.; Gao, M.; Syed, S.; Zhuang, J.; Xu, X.; Zhang, X.Q. Bioactive Hydrogels for Bone Regeneration. Bioact. Mater. 2018, 3, 401–417. [Google Scholar] [CrossRef] [PubMed]
- Pedrosa, M.; Ferreira, M.T.; Luís, L.A.; Maria, M.P.; Curate, F. The Association of Osteochemometrics and Bone Mineral Density in Humans. Am. J. Phys. Anthropol. 2021, 176, 434–444. [Google Scholar] [CrossRef]
- Amini, A.R.; Laurencin, C.T.; Nukavarapu, S.P. Bone Tissue Engineering: Recent Advances and Challenges. Crit. Rev. Biomed. Eng. 2012, 40, 363. [Google Scholar] [CrossRef]
- McGovern, J.A.; Griffin, M.; Hutmacher, D.W. Animal Models for Bone Tissue Engineering and Modelling Disease. DMM Dis. Model. Mech. 2018, 11, dmm033084. [Google Scholar] [CrossRef] [PubMed]
- Xue, X.; Hu, Y.; Deng, Y.; Su, J. Recent Advances in Design of Functional Biocompatible Hydrogels for Bone Tissue Engineering. Adv. Funct. Mater. 2021, 31, 2009432. [Google Scholar] [CrossRef]
- Wang, W.; Yeung, K.W.K. Bone Grafts and Biomaterials Substitutes for Bone Defect Repair: A Review. Bioact. Mater. 2017, 2, 224–247. [Google Scholar] [CrossRef] [PubMed]
- Kinaci, A.; Neuhaus, V.; Ring, D.C. Trends in Bone Graft Use in the United States. Orthopedics 2014, 37, e783–e788. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.M.; Ibrahim, E.-S.H.; Dudek, N.; Lu, J.C.; Kalia, V.; Runge, M.; Srinivasan, A.; Stojanovska, J.; Agarwal, P.P. Improving MR Image Quality in Patients with Metallic Implants. Radiographics 2021, 41, E126–E137. [Google Scholar] [CrossRef]
- Roberts, T.T.; Rosenbaum, A.J. Bone Grafts, Bone Substitutes and Orthobiologics the Bridge between Basic Science and Clinical Advancements in Fracture Healing. Organogenesis 2012, 8, 114–124. [Google Scholar] [CrossRef]
- Cannio, M.; Bellucci, D.; Roether, J.A.; Boccaccini, D.N.; Cannillo, V. Bioactive Glass Applications: A Literature Review of Human Clinical Trials. Materials 2021, 14, 5440. [Google Scholar] [CrossRef]
- Dewi, A.H.; Ana, I.D. The Use of Hydroxyapatite Bone Substitute Grafting for Alveolar Ridge Preservation, Sinus Augmentation, and Periodontal Bone Defect: A Systematic Review. Heliyon 2018, 4, e00884. [Google Scholar] [CrossRef] [PubMed]
- Koshy, S.T.; Ferrante, T.C.; Lewin, S.A.; Mooney, D.J. Injectable, Porous, and Cell-Responsive Gelatin Cryogels. Biomaterials 2014, 35, 2477. [Google Scholar] [CrossRef] [PubMed]
- Choi, C.E.; Chakraborty, A.; Coyle, A.; Shamiya, Y.; Paul, A. Contact-Free Remote Manipulation of Hydrogel Properties Using Light-Triggerable Nanoparticles: A Materials Science Perspective for Biomedical Applications. Adv. Healthc. Mater. 2022, 11, 2102088. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, A.; Alexander, S.; Luo, W.; Al-Salam, N.; Mia, O.V.; Sudhir, R.H.; Chakrabarti, S.; Paul, A. Engineering Multifunctional Adhesive Hydrogel Patches for Biomedical Applications. Interdiscip. Med. 2023, 1, e20230008. [Google Scholar] [CrossRef]
- Waters, R.; Pacelli, S.; Maloney, R.; Medhi, I.; Ahmed, R.P.H.; Paul, A. Stem Cell Secretome-Rich Nanoclay Hydrogel: A Dual Action Therapy for Cardiovascular Regeneration. Nanoscale 2016, 8, 7371–7376. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, A.; Roy, A.; Ravi, S.P.; Paul, A. Exploiting the Role of Nanoparticles for Use in Hydrogel-Based Bioprinting Applications: Concept, Design, and Recent Advances. Biomater. Sci. 2021, 9, 6337–6354. [Google Scholar] [CrossRef] [PubMed]
- Del Valle, L.J.; Díaz, A.; Puiggalí, J. Hydrogels for Biomedical Applications: Cellulose, Chitosan, and Protein/Peptide Derivatives. Gels 2017, 3, 27. [Google Scholar] [CrossRef]
- Xavier, J.R.; Thakur, T.; Desai, P.; Jaiswal, M.K.; Sears, N.; Cosgriff-Hernandez, E.; Kaunas, R.; Gaharwar, A.K. Bioactive Nanoengineered Hydrogels for Bone Tissue Engineering: A Growth-Factor-Free Approach. ACS Nano 2015, 9, 3109–3118. [Google Scholar] [CrossRef]
- Merino, S.; Martín, C.; Kostarelos, K.; Prato, M.; Vázquez, E. Nanocomposite Hydrogels: 3D Polymer-Nanoparticle Synergies for on-Demand Drug Delivery. ACS Nano 2015, 9, 4686–4697. [Google Scholar] [CrossRef]
- Sharma, G.; Thakur, B.; Naushad, M.; Kumar, A.; Stadler, F.J.; Alfadul, S.M.; Mola, G.T. Applications of Nanocomposite Hydrogels for Biomedical Engineering and Environmental Protection. Environ. Chem. Lett. 2017, 16, 113–146. [Google Scholar] [CrossRef]
- Sun, M.; Sun, X.; Wang, Z.; Guo, S.; Yu, G.; Yang, H. Synthesis and Properties of Gelatin Methacryloyl (GelMA) Hydrogels and Their Recent Applications in Load-Bearing Tissue. Polymers 2018, 10, 1290. [Google Scholar] [CrossRef] [PubMed]
- Pablos, J.L.; Jiménez-Holguín, J.; Salcedo, S.S.; Salinas, A.J.; Corrales, T.; Vallet-Regí, M. New Photocrosslinked 3D Foamed Scaffolds Based on GelMA Copolymers: Potential Application in Bone Tissue Engineering. Gels 2023, 9, 403. [Google Scholar] [CrossRef]
- Yue, K.; Trujillo-de Santiago, G.; Alvarez, M.M.; Tamayol, A.; Annabi, N.; Khademhosseini, A. Synthesis, Properties, and Biomedical Applications of Gelatin Methacryloyl (GelMA) Hydrogels. Biomaterials 2015, 73, 254. [Google Scholar] [CrossRef] [PubMed]
- Klotz, B.J.; Gawlitta, D.; Rosenberg, A.J.W.P.; Malda, J.; Melchels, F.P.W. Gelatin-Methacryloyl Hydrogels: Towards Biofabrication-Based Tissue Repair. Trends Biotechnol. 2016, 34, 394. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Liu, M.; Zhang, Y.; Yin, J.; Pei, R. Nanocomposite Hydrogels for Tissue Engineering Applications. Nanoscale 2020, 12, 14976–14995. [Google Scholar] [CrossRef] [PubMed]
- Piao, Y.; You, H.; Xu, T.; Bei, H.P.; Piwko, I.Z.; Kwan, Y.Y.; Zhao, X. Biomedical Applications of Gelatin Methacryloyl Hydrogels. Eng. Regen. 2021, 2, 47–56. [Google Scholar] [CrossRef]
- Chakraborty, A.; Pacelli, S.; Alexander, S.; Huayamares, S.; Rosenkrans, Z.; Vergel, F.E.; Wu, Y.; Chakravorty, A.; Paul, A. Nanoparticle-Reinforced Tough Hydrogel as a Versatile Platform for Pharmaceutical Drug Delivery: Preparation and in Vitro Characterization. Mol. Pharm. 2023, 20, 767–774. [Google Scholar] [CrossRef]
- Basu, S.; Chakraborty, A.; Alkiswani, A.R.I.; Shamiya, Y.; Paul, A. Investigation of a 2D WS 2 Nanosheet-Reinforced Tough DNA Hydrogel as a Biomedical Scaffold: Preparation and in Vitro Characterization. Mater. Adv. 2022, 3, 946–952. [Google Scholar] [CrossRef]
- Jeong, J.; Kim, J.H.; Shim, J.H.; Hwang, N.S.; Heo, C.Y. Bioactive Calcium Phosphate Materials and Applications in Bone Regeneration. Biomater. Res. 2019, 23, 4. [Google Scholar] [CrossRef]
- Habibah, T.U.; Amlani, D.V.; Brizuela, M. Hydroxyapatite Dental Material; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Li, H.; Li, M.; Ran, X.; Cui, J.; Wei, F.; Yi, G.; Chen, W.; Luo, X.; Chen, Z. The Role of Zinc in Bone Mesenchymal Stem Cell Differentiation. Cell. Reprogram. 2022, 24, 80–94. [Google Scholar] [CrossRef]
- Ciosek, Ż.; Kot, K.; Rotter, I. Iron, Zinc, Copper, Cadmium, Mercury, and Bone Tissue. Int. J. Environ. Res. Public Health 2023, 20, 2197. [Google Scholar] [CrossRef]
- Sun, T.W.; Yu, W.L.; Zhu, Y.J.; Chen, F.; Zhang, Y.G.; Jiang, Y.Y.; He, Y.H. Porous Nanocomposite Comprising Ultralong Hydroxyapatite Nanowires Decorated with Zinc-Containing Nanoparticles and Chitosan: Synthesis and Application in Bone Defect Repair. Chem.-A Eur. J. 2018, 24, 8809–8821. [Google Scholar] [CrossRef] [PubMed]
- Liang, N.; Ren, N.; Feng, Z.; Sun, Z.; Dong, M.; Wang, W.; Liu, F.; Sun, C.; Zhou, W.; Xing, Z.; et al. Biomimetic Metal−Organic Frameworks as Targeted Vehicles to Enhance Osteogenesis. Adv. Healthc. Mater. 2022, 11, 2102821. [Google Scholar] [CrossRef] [PubMed]
- Tyagi, N.; Wijesundara, Y.H.; Gassensmith, J.J.; Popat, A. Clinical Translation of Metal–Organic Frameworks. Nat. Rev. Mater. 2023, 8, 701–703. [Google Scholar] [CrossRef]
- Öztürk, Z.; Filez, M.; Weckhuysen, B.M. Decoding Nucleation and Growth of Zeolitic Imidazolate Framework Thin Films with Atomic Force Microscopy and Vibrational Spectroscopy. Chem.–A Eur. J. 2017, 23, 10915–10924. [Google Scholar] [CrossRef] [PubMed]
- Cravillon, J.; Schröder, C.A.; Bux, H.; Rothkirch, A.; Caro, J.; Wiebcke, M. Formate Modulated Solvothermal Synthesis of ZIF-8 Investigated Using Time-Resolved in Situ X-Ray Diffraction and Scanning Electron Microscopy. CrystEngComm 2011, 14, 492–498. [Google Scholar] [CrossRef]
- Kaur, H.; Mohanta, G.C.; Gupta, V.; Kukkar, D.; Tyagi, S. Synthesis and Characterization of ZIF-8 Nanoparticles for Controlled Release of 6-Mercaptopurine Drug. J. Drug Deliv. Sci. Technol. 2017, 41, 106–112. [Google Scholar] [CrossRef]
- Luzuriaga, M.A.; Benjamin, C.E.; Gaertner, M.W.; Lee, H.; Herbert, F.C.; Mallick, S.; Gassensmith, J.J. ZIF-8 Degrades in Cell Media, Serum, and Some—But Not All—Common Laboratory Buffers. Supramol. Chem. 2019, 31, 485–490. [Google Scholar] [CrossRef]
- Spitsyna, A.S.; Poryvaev, A.S.; Sannikova, N.E.; Yazikova, A.A.; Kirilyuk, I.A.; Dobrynin, S.A.; Chinak, O.A.; Fedin, M.V.; Krumkacheva, O.A. Stability of ZIF-8 Nanoparticles in Most Common Cell Culture Media. Molecules 2022, 27, 3240. [Google Scholar] [CrossRef]
- Velásquez-Hernández, M.D.J.; Ricco, R.; Carraro, F.; Limpoco, F.T.; Linares-Moreau, M.; Leitner, E.; Wiltsche, H.; Rattenberger, J.; Schröttner, H.; Frühwirt, P.; et al. Degradation of ZIF-8 in Phosphate Buffered Saline Media. CrystEngComm 2019, 21, 4538–4544. [Google Scholar] [CrossRef]
- Liu, Y.; Li, T.; Sun, M.; Cheng, Z.; Jia, W.; Jiao, K.; Wang, S.; Jiang, K.; Yang, Y.; Dai, Z.; et al. ZIF-8 Modified Multifunctional Injectable Photopolymerizable GelMA Hydrogel for the Treatment of Periodontitis. Acta Biomater. 2022, 146, 37–48. [Google Scholar] [CrossRef] [PubMed]
- Yao, T.; Asayama, Y. Animal-Cell Culture Media: History, Characteristics, and Current Issues. Reprod. Med. Biol. 2017, 16, 99–117. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Sun, X.; Yildirimer, L.; Lang, Q.; Lin, Z.Y.; Zheng, R.; Zhang, Y.; Cui, W.; Annabi, N.; Khademhosseini, A. Cell Infiltrative Hydrogel Fibrous Scaffolds for Accelerated Wound Healing. Acta Biomater. 2017, 49, 66. [Google Scholar] [CrossRef] [PubMed]
- Xiang, L.; Cui, W. Biomedical Application of Photo-Crosslinked Gelatin Hydrogels. J. Leather Sci. Eng. 2021, 3, 1–24. [Google Scholar] [CrossRef]
- Gibbs, D.M.R.; Black, C.R.M.; Dawson, J.I.; Oreffo, R.O.C. A Review of Hydrogel Use in Fracture Healing and Bone Regeneration. J. Tissue Eng. Regen. Med. 2016, 10, 187–198. [Google Scholar] [CrossRef] [PubMed]
- Akbari, M.; Khademhosseini, A. Tissue Bioprinting for Biology and Medicine. Cell 2022, 185, 2644–2648. [Google Scholar] [CrossRef] [PubMed]
- Mantha, S.; Pillai, S.; Khayambashi, P.; Upadhyay, A.; Zhang, Y.; Tao, O.; Pham, H.M.; Tran, S.D. Smart Hydrogels in Tissue Engineering and Regenerative Medicine. Materials 2019, 12, 3323. [Google Scholar] [CrossRef]
- Liu, Y.; Zhu, Z.; Pei, X.; Zhang, X.; Cheng, X.; Hu, S.; Gao, X.; Wang, J.; Chen, J.; Wan, Q. ZIF-8-Modified Multifunctional Bone-Adhesive Hydrogels Promoting Angiogenesis and Osteogenesis for Bone Regeneration. ACS Appl. Mater. Interfaces 2020, 12, 36978–36995. [Google Scholar] [CrossRef]
- Liu, C.; Zeng, H.; Chen, Z.; Ge, Z.; Wang, B.; Liu, B.; Fan, Z. Sprayable Methacrylic Anhydride-Modified Gelatin Hydrogel Combined with Bionic Neutrophils Nanoparticles for Scar-Free Wound Healing of Diabetes Mellitus. Int. J. Biol. Macromol. 2022, 202, 418–430. [Google Scholar] [CrossRef]
- Shin, S.R.; Bae, H.; Cha, J.M.; Mun, J.Y.; Chen, Y.C.; Tekin, H.; Shin, H.; Farshchi, S.; Dokmeci, M.R.; Tang, S.; et al. Carbon Nanotube Reinforced Hybrid Microgels as Scaffold Materials for Cell Encapsulation. ACS Nano 2012, 6, 362–372. [Google Scholar] [CrossRef]
- Xavier Mendes, A.; Moraes Silva, S.; O’Connell, C.D.; Duchi, S.; Quigley, A.F.; Kapsa, R.M.I.; Moulton, S.E. Enhanced Electroactivity, Mechanical Properties, and Printability through the Addition of Graphene Oxide to Photo-Cross-Linkable Gelatin Methacryloyl Hydrogel. ACS Biomater. Sci. Eng. 2021, 7, 2279–2295. [Google Scholar] [CrossRef]
- Kurian, A.G.; Singh, R.K.; Patel, K.D.; Lee, J.H.; Kim, H.W. Multifunctional GelMA Platforms with Nanomaterials for Advanced Tissue Therapeutics. Bioact. Mater. 2022, 8, 267–295. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Zheng, H.; Poh, P.S.P.; Machens, H.G.; Schilling, A.F. Hydrogels for Engineering of Perfusable Vascular Networks. Int. J. Mol. Sci. 2015, 16, 15997–16016. [Google Scholar] [CrossRef] [PubMed]
- Ahearne, M. Introduction to Cell–Hydrogel Mechanosensing. Interface Focus 2014, 4, 20130038. [Google Scholar] [CrossRef] [PubMed]
- Heta, S.; Robo, I. The Side Effects of the Most Commonly Used Group of Antibiotics in Periodontal Treatments. Med. Sci. 2018, 6, 6. [Google Scholar] [CrossRef] [PubMed]
- Xin, W.; Gao, Y.; Yue, B. Recent Advances in Multifunctional Hydrogels for the Treatment of Osteomyelitis. Front. Bioeng. Biotechnol. 2022, 10, 865250. [Google Scholar] [CrossRef] [PubMed]
- Pacelli, S.; Chakravarti, A.R.; Modaresi, S.; Subham, S.; Burkey, K.; Kurlbaum, C.; Fang, M.; Neal, C.A.; Mellott, A.J.; Chakraborty, A.; et al. Investigation of Human Adipose-Derived Stem-Cell Behavior Using a Cell-Instructive Polydopamine-Coated Gelatin–Alginate Hydrogel. J. Biomed. Mater. Res. Part A 2021, 109, 2597–2610. [Google Scholar] [CrossRef] [PubMed]
- Dreiss, C.A. Hydrogel Design Strategies for Drug Delivery. Curr. Opin. Colloid Interface Sci. 2020, 48, 1–17. [Google Scholar] [CrossRef]
- Hu, Y.; Li, H.; Lv, X.; Xu, Y.; Xie, Y.; Yuwen, L.; Song, Y.; Li, S.; Shao, J.; Yang, D. Stimuli-Responsive Therapeutic Systems for the Treatment of Diabetic Infected Wounds. Nanoscale 2022, 14, 12967–12983. [Google Scholar] [CrossRef]
- Paul, A.; Manoharan, V.; Krafft, D.; Assmann, A.; Uquillas, J.A.; Shin, S.R.; Hasan, A.; Hussain, M.A.; Memic, A.; Gaharwar, A.K.; et al. Nanoengineered Biomimetic Hydrogels for Guiding Human Stem Cell Osteogenesis in Three Dimensional Microenvironments. J. Mater. Chem. B 2016, 4, 3544–3554. [Google Scholar] [CrossRef]
- Hoop, M.; Walde, C.F.; Riccò, R.; Mushtaq, F.; Terzopoulou, A.; Chen, X.Z.; de Mello, A.J.; Doonan, C.J.; Falcaro, P.; Nelson, B.J.; et al. Biocompatibility Characteristics of the Metal Organic Framework ZIF-8 for Therapeutical Applications. Appl. Mater. Today 2018, 11, 13–21. [Google Scholar] [CrossRef]
- Brokesh, A.M.; Gaharwar, A.K. Inorganic Biomaterials for Regenerative Medicine. ACS Appl. Mater. Interfaces 2020, 12, 5319–5344. [Google Scholar] [CrossRef] [PubMed]
- Balasubramanian, P.; Strobel, L.A.; Kneser, U.; Boccaccini, A.R. Zinc-Containing Bioactive Glasses for Bone Regeneration, Dental and Orthopedic Applications. Biomed. Glas. 2015, 1, 51–69. [Google Scholar] [CrossRef]
- O’Connor, J.P.; Kanjilal, D.; Teitelbaum, M.; Lin, S.S.; Cottrell, J.A. Zinc as a Therapeutic Agent in Bone Regeneration. Materials 2020, 13, 2211. [Google Scholar] [CrossRef] [PubMed]
- Zeng, H.; Ran, J.; Shi, B. Rational Design of a Stable, Effective, and Sustainable Dexamethasone Delivery Platform on Ti Implant—An Innovative Application of Metal Organic Framework in Bone Implants. Clin. Oral Implant. Res. 2018, 29, 204. [Google Scholar] [CrossRef]
- Yao, S.; Chi, J.; Wang, Y.; Zhao, Y.; Luo, Y.; Wang, Y. Zn-MOF Encapsulated Antibacterial and Degradable Microneedles Array for Promoting Wound Healing. Adv. Healthc. Mater. 2021, 10, 2100056. [Google Scholar] [CrossRef] [PubMed]
- Kocyła, A.; Pomorski, A.; Krężel, A. Molar Absorption Coefficients and Stability Constants of Zincon Metal Complexes for Determination of Metal Ions and Bioinorganic Applications. J. Inorg. Biochem. 2017, 176, 53–65. [Google Scholar] [CrossRef]
- Mukherjee, S.; Pawar, N.; Kulkarni, O.; Nagarkar, B.; Thopte, S.; Bhujbal, A.; Pawar, P. Evaluation of Free-Radical Quenching Properties of Standard Ayurvedic Formulation Vayasthapana Rasayana. BMC Complement. Altern. Med. 2011, 11, 38. [Google Scholar] [CrossRef]
- Jin, Y.; Kong, H.; Zhou, X.; Li, G.; Du, J. Design and Characterization of Sheet-Based Gyroid Porous Structures with Bioinspired Functional Gradients. Materials 2020, 13, 3844. [Google Scholar] [CrossRef]
- Tsao, Y.T.; Huang, Y.J.; Wu, H.H.; Liu, Y.A.; Liu, Y.S.; Lee, O.K. Osteocalcin Mediates Biomineralization during Osteogenic Maturation in Human Mesenchymal Stromal Cells. Int. J. Mol. Sci. 2017, 18, 159. [Google Scholar] [CrossRef]


| Desired ZIF-8 Conc. in GelMA Hydrogel Formulation (mg/mL) | Amount of 10 mg/mL ZIF-8 Solution Required (µL) |
|---|---|
| 0.5 | 15 |
| 1 | 30 |
| 2 | 60 |
| 3 | 90 |
| Components | Stock Conc. (% w/v) | Component Conc. in Hydrogel (% v/v) | ||
|---|---|---|---|---|
| GelMA | 20 | 5 | 10 | 15 |
| LAP | 8 | 1 | 1 | 1 |
| Tartrazine | 1 | 0.1 | 0.1 | 0.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, C.-E.; Chakraborty, A.; Adzija, H.; Shamiya, Y.; Hijazi, K.; Coyle, A.; Rizkalla, A.; Holdsworth, D.W.; Paul, A. Metal Organic Framework-Incorporated Three-Dimensional (3D) Bio-Printable Hydrogels to Facilitate Bone Repair: Preparation and In Vitro Bioactivity Analysis. Gels 2023, 9, 923. https://doi.org/10.3390/gels9120923
Choi C-E, Chakraborty A, Adzija H, Shamiya Y, Hijazi K, Coyle A, Rizkalla A, Holdsworth DW, Paul A. Metal Organic Framework-Incorporated Three-Dimensional (3D) Bio-Printable Hydrogels to Facilitate Bone Repair: Preparation and In Vitro Bioactivity Analysis. Gels. 2023; 9(12):923. https://doi.org/10.3390/gels9120923
Chicago/Turabian StyleChoi, Cho-E, Aishik Chakraborty, Hailey Adzija, Yasmeen Shamiya, Khaled Hijazi, Ali Coyle, Amin Rizkalla, David W. Holdsworth, and Arghya Paul. 2023. "Metal Organic Framework-Incorporated Three-Dimensional (3D) Bio-Printable Hydrogels to Facilitate Bone Repair: Preparation and In Vitro Bioactivity Analysis" Gels 9, no. 12: 923. https://doi.org/10.3390/gels9120923
APA StyleChoi, C.-E., Chakraborty, A., Adzija, H., Shamiya, Y., Hijazi, K., Coyle, A., Rizkalla, A., Holdsworth, D. W., & Paul, A. (2023). Metal Organic Framework-Incorporated Three-Dimensional (3D) Bio-Printable Hydrogels to Facilitate Bone Repair: Preparation and In Vitro Bioactivity Analysis. Gels, 9(12), 923. https://doi.org/10.3390/gels9120923