The Use of Hydrogel-Based Materials for Radioprotection
Abstract
:1. Introduction
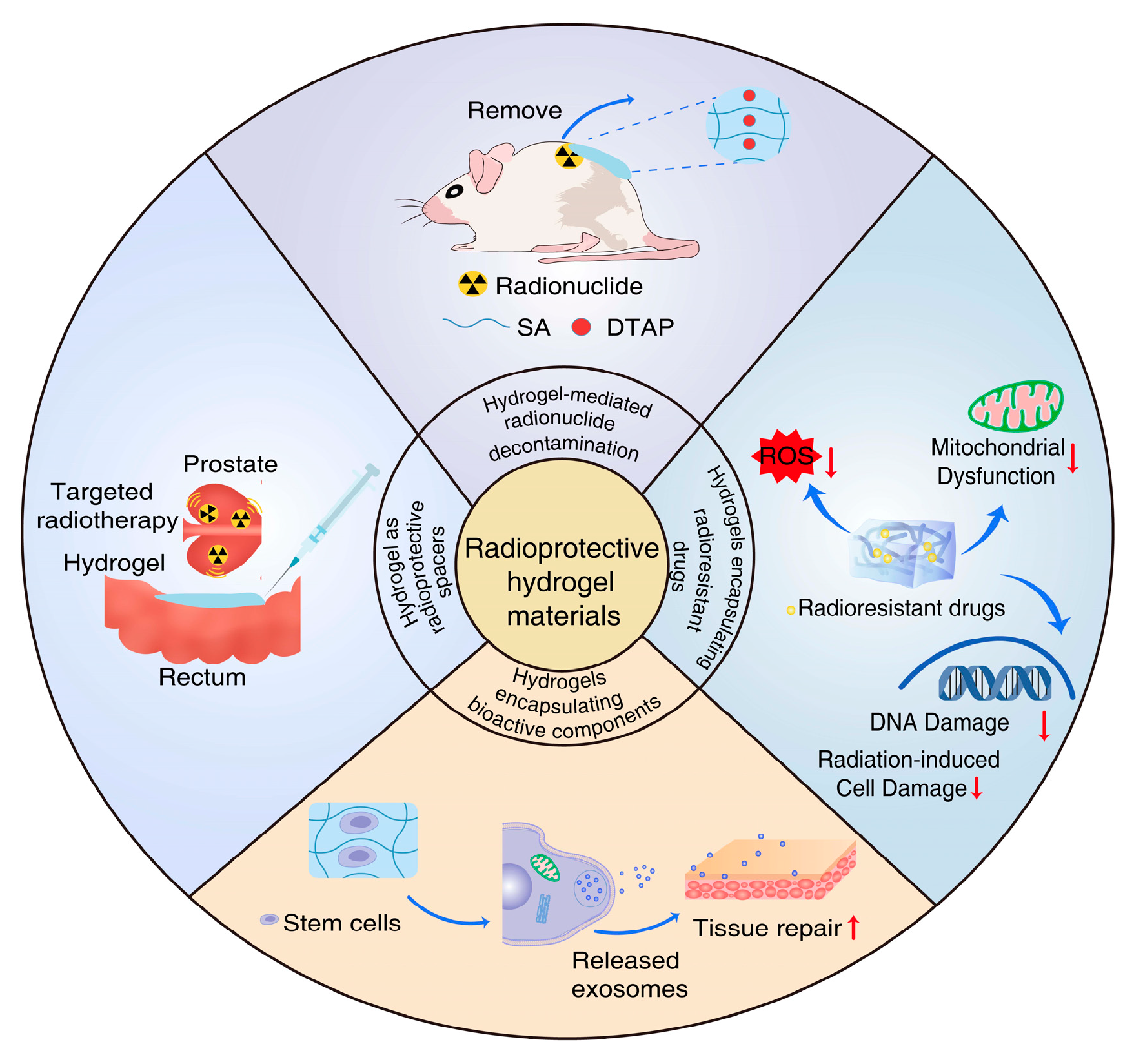
2. Approaches to the Design of Radioprotective Hydrogels
2.1. Hydrogel-Mediated Radionuclide Decontamination
2.2. Hydrogels Encapsulating Radioresistant Drug
2.3. Hydrogels Encapsulating Bioactive Components
2.4. Hydrogels as Radioprotective Spacers
3. The use of Hydrogels for the Treatment of Radiation-Related Disease
3.1. Radiation-Induced Skin Injury
3.2. Osteoradionecrosis
3.3. Radiation-Induced Damage to Adjacent Healthy Tissues
3.3.1. PEG Hydrogels
3.3.2. HA Hydrogels
3.3.3. Collagen Hydrogels
3.4. Other Radiation-Induced Diseases
4. Conclusions and Future Prospects
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Toon, O.B.; Bardeen, C.G.; Robock, A.; Xia, L.; Kristensen, H.; McKinzie, M.; Peterson, R.J.; Harrison, C.S.; Lovenduski, N.S.; Turco, R.P. Rapidly expanding nuclear arsenals in Pakistan and India portend regional and global catastrophe. Sci. Adv. 2019, 5, y5478. [Google Scholar] [CrossRef] [PubMed]
- Ohba, T.; Liutsko, L.; Schneider, T.; Barquinero, J.F.; Crouaïl, P.; Fattibene, P.; Kesminiene, A.; Laurier, D.; Sarukhan, A.; Skuterud, L.; et al. The SHAMISEN Project: Challenging historical recommendations for preparedness, response and surveillance of health and well-being in case of nuclear accidents: Lessons learnt from Chernobyl and Fukushima. Environ. Int. 2021, 146, 106200. [Google Scholar] [CrossRef] [PubMed]
- Schaue, D.; McBride, W.H. Opportunities and challenges of radiotherapy for treating cancer. Nat. Rev. Clin. Oncol. 2015, 12, 527–540. [Google Scholar] [CrossRef]
- Allen, C.; Her, S.; Jaffray, D.A. Radiotherapy for Cancer: Present and Future. Adv. Drug Deliver. Rev. 2017, 109, 1–2. [Google Scholar] [CrossRef]
- Grdina, D.J.; Murley, J.S.; Kataoka, Y. Radioprotectants: Current status and new directions. Oncology 2002, 63 (Suppl. 2), 2–10. [Google Scholar] [CrossRef] [PubMed]
- Mettler, F.A.; Brenner, D.; Coleman, C.N.; Kaminski, J.M.; Kennedy, A.R.; Wagner, L.K. Can radiation risks to patients be reduced without reducing radiation exposure? The status of chemical radioprotectants. Am. J. Roentgenol. 2011, 196, 616–618. [Google Scholar] [CrossRef]
- Yao, Y.; Zheng, Z.; Song, Q. Mesenchymal stem cells: A double-edged sword in radiation-induced lung injury. Thorac. Cancer 2018, 9, 208–217. [Google Scholar] [CrossRef]
- Zuo, R.; Liu, M.; Wang, Y.; Li, J.; Wang, W.; Wu, J.; Sun, C.; Li, B.; Wang, Z.; Lan, W.; et al. BM-MSC-derived exosomes alleviate radiation-induced bone loss by restoring the function of recipient BM-MSCs and activating Wnt/β-catenin signaling. Stem Cell Res. Ther. 2019, 10, 30. [Google Scholar] [CrossRef]
- Freyman, T.; Polin, G.; Osman, H.; Crary, J.; Lu, M.; Cheng, L.; Palasis, M.; Wilensky, R.L.; Freyman, T.; Polin, G.; et al. A quantitative, randomized study evaluating three methods of mesenchymal stem cell delivery following myocardial infarction. Eur. Heart J. 2006, 27, 1114–1122. [Google Scholar] [CrossRef]
- Berthiaume, F.; Maguire, T.J.; Yarmush, M.L. Tissue engineering and regenerative medicine: History, progress, and challenges. Annu. Rev. Chem. Biomol. 2011, 2, 403–430. [Google Scholar] [CrossRef]
- Dobrzyński, P.; Pamuła, E. Polymeric Scaffolds: Design, Processing, and Biomedical Application. Int. J. Mol. Sci. 2021, 22, 4552. [Google Scholar] [CrossRef] [PubMed]
- Dimatteo, R.; Darling, N.J.; Segura, T. In situ forming injectable hydrogels for drug delivery and wound repair. Adv. Drug Deliver. Rev. 2018, 127, 167–184. [Google Scholar] [CrossRef] [PubMed]
- Ganguly, S.; Margel, S. A Review on Synthesis Methods of Phyllosilicate- and Graphene-Filled Composite Hydrogels. J. Compos. Sci. 2022, 6, 15. [Google Scholar] [CrossRef]
- Zhao, C.; Zhou, L.; Chiao, M.; Yang, W. Antibacterial hydrogel coating: Strategies in surface chemistry. Adv. Colloid Interface Sci. 2020, 285, 102280. [Google Scholar] [CrossRef]
- Huang, Q.; Zou, Y.; Arno, M.C.; Chen, S.; Wang, T.; Gao, J.; Dove, A.P.; Du, J. Hydrogel scaffolds for differentiation of adipose-derived stem cells. Chem. Soc. Rev. 2017, 46, 6255–6275. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Z.; Zheng, X.; An, Y.; Wang, K.; Zhang, J.; He, H.; Wu, J. Zwitterionic hydrogel for sustained release of growth factors to enhance wound healing. Biomater. Sci. 2021, 9, 882–891. [Google Scholar] [CrossRef] [PubMed]
- Lei, T.; Liu, Y.; Deng, S.; Xiao, Z.; Yang, Y.; Zhang, X.; Bi, W.; Du, H. Hydrogel supplemented with human platelet lysate enhances multi-lineage differentiation of mesenchymal stem cells. J. Nanobiotechnol. 2022, 20, 176. [Google Scholar] [CrossRef]
- Kikuchi, I.S.; Galante, R.S.C.; Dua, K.; Malipeddi, V.R.; Awasthi, R.; Ghisleni, D.D.M.; Pinto, T.D.J.A. Hydrogel Based Drug Delivery Systems: A Review with Special Emphasis on Challenges Associated with Decontamination of Hydrogels and Biomaterials. Curr. Drug Deliv. 2017, 14, 917–925. [Google Scholar] [CrossRef]
- Hadigal, S.R.; Gupta, A.K. Application of Hydrogel Spacer SpaceOAR Vue for Prostate Radiotherapy. Tomography 2022, 8, 2648–2661. [Google Scholar] [CrossRef]
- Li, Z.; Zhao, T.; Ding, J.; Gu, H.; Wang, Q.; Wang, Y.; Zhang, D.; Gao, C. A reactive oxygen species-responsive hydrogel encapsulated with bone marrow derived stem cells promotes repair and regeneration of spinal cord injury. Bioact. Mater. 2023, 19, 550–568. [Google Scholar] [CrossRef]
- Zhang, D.; Chang, R.; Ren, Y.; He, Y.; Guo, S.; Guan, F.; Yao, M. Injectable and reactive oxygen species-scavenging gelatin hydrogel promotes neural repair in experimental traumatic brain injury. Int. J. Biol. Macromol. 2022, 219, 844–863. [Google Scholar] [CrossRef] [PubMed]
- Boerma, M.; Sridharan, V.; Mao, X.-W.; Nelson, G.A.; Cheema, A.K.; Koturbash, I.; Singh, S.P.; Tackett, A.J.; Hauer-Jensen, M. Effects of ionizing radiation on the heart. Mutat. Res. Mol. Mech. Mutagen. 2016, 770, 319–327. [Google Scholar] [CrossRef]
- Ullah, F.; Othman, M.B.H.; Javed, F.; Ahmad, Z.; Akil, H.M. Classification, processing and application of hydrogels: A review. Mater. Sci. Eng. C 2015, 57, 414–433. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, E.M. Hydrogel: Preparation, characterization, and applications: A review. J. Adv. Res. 2015, 6, 105–121. [Google Scholar] [CrossRef]
- Sharma, S.; Tiwari, S. A review on biomacromolecular hydrogel classification and its applications. Int. J. Biol. Macromol. 2020, 162, 737–747. [Google Scholar] [CrossRef] [PubMed]
- Yue, K.; Trujillo-de Santiago, G.; Alvarez, M.M.; Tamayol, A.; Annabi, N.; Khademhosseini, A. Synthesis, properties, and biomedical applications of gelatin methacryloyl (GelMA) hydrogels. Biomaterials 2015, 73, 254–271. [Google Scholar] [CrossRef] [PubMed]
- Saldin, L.T.; Cramer, M.C.; Velankar, S.S.; White, L.J.; Badylak, S.F. Extracellular matrix hydrogels from decellularized tissues: Structure and function. Acta Biomater. 2017, 49, 1–15. [Google Scholar] [CrossRef]
- Aaseth, J.; Nurchi, V.M.; Andersen, O. Medical Therapy of Patients Contaminated with Radioactive Cesium or Iodine. Biomolecules 2019, 9, 856. [Google Scholar] [CrossRef]
- Rump, A.; Becker, B.; Eder, S.; Lamkowski, A.; Abend, M.; Port, M. Medical management of victims contaminated with radionuclides after a “dirty bomb” attack. Mil. Med. Res. 2018, 5, 27. [Google Scholar] [CrossRef]
- Cui, F.; Wu, Z.; Zhao, R.; Chen, Q.; Liu, Z.; Zhao, Y.; Yan, H.; Shen, G.; Tu, Y.; Zhou, D.; et al. Development and Characterization of a Novel Hydrogel for the Decontaminating of Radionuclide-Contaminated Skin Wounds. Macromol. Biosci. 2021, 21, e2000399. [Google Scholar] [CrossRef]
- Xu, K.; Ge, W.; Liang, G.; Wang, L.; Yang, Z.; Wang, Q.; Hsing, I.-M.; Xu, B. Bisphosphonate-containing supramolecular hydrogels for topical decorporation of uranium-contaminated wounds in mice. Int. J. Radiat. Biol. 2008, 84, 353–362. [Google Scholar] [CrossRef] [PubMed]
- Prise, K.M.; O’Sullivan, J.M. Radiation-induced bystander signalling in cancer therapy. Nat. Rev. Cancer 2009, 9, 351–360. [Google Scholar] [CrossRef] [PubMed]
- Baskar, R.; Dai, J.; Wenlong, N.; Yeo, R.; Yeoh, K.-W. Biological response of cancer cells to radiation treatment. Front. Mol. Biosci. 2014, 1, 24. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.; Meng, L.; Hou, X.; Qu, C.; Wang, B.; Xin, Y.; Jiang, X. Radiation-induced skin reactions: Mechanism and treatment. Cancer Manag. Res. 2019, 11, 167–177. [Google Scholar] [CrossRef]
- Oliai, C.; Yang, L.X. Radioprotectants to reduce the risk of radiation-induced carcinogenesis. Int. J. Radiat. Biol. 2014, 90, 203–213. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Li, J.; Ma, H.; Zhen, M.; Guo, J.; Wang, L.; Jiang, L.; Shu, C.; Wang, C. Biocompatible [60]/[70] Fullerenols: Potent Defense against Oxidative Injury Induced by Reduplicative Chemotherapy. Acs. Appl. Mater. Inter. 2017, 9, 35539–35547. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.; Wang, C.; Xie, J.; Ji, C.; Gu, Z. Eco-Friendly and Scalable Synthesis of Fullerenols with High Free Radical Scavenging Ability for Skin Radioprotection. Small 2021, 17, e2102035. [Google Scholar] [CrossRef]
- Zhang, J.; Zhu, Y.; Zhang, Y.; Lin, W.; Ke, J.; Liu, J.; Zhang, L.; Liu, J. A balanced charged hydrogel with anti-biofouling and antioxidant properties for treatment of irradiation-induced skin injury. Mater. Sci. Eng. C 2021, 131, 112538. [Google Scholar] [CrossRef]
- Farhat, W.; Hasan, A.; Lucia, L.; Becquart, F.; Ayoub, A.; Kobeissy, F. Hydrogels for Advanced Stem Cell Therapies: A Biomimetic Materials Approach for Enhancing Natural Tissue Function. Ieee. Rev. Biomed. Eng. 2019, 12, 333–351. [Google Scholar] [CrossRef]
- Bercea, M. Bioinspired Hydrogels as Platforms for Life-Science Applications: Challenges and Opportunities. Polymers 2022, 14, 2365. [Google Scholar] [CrossRef]
- Nie, S.; Ren, C.; Liang, X.; Cai, H.; Sun, H.; Liu, F.; Ji, K.; Wang, Y.; Liu, Q. Supramolecular Hydrogel-Wrapped Gingival Mesenchymal Stem Cells in Cutaneous Radiation Injury. Cells 2022, 11, 3089. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Wu, P.; Sun, H.; Zhou, H.; Zhang, Y.; Xiao, Z. Lung tissue extracellular matrix-derived hydrogels protect against radiation-induced lung injury by suppressing epithelial-mesenchymal transition. J. Cell Physiol. 2020, 235, 2377–2388. [Google Scholar] [CrossRef] [PubMed]
- Iervolino, V.; Di Costanzo, G.; Azzaro, R.; Diodato, A.; Di Macchia, C.A.; Di Meo, T.; Petruzziello, A.; Loquercio, G.; Muto, P.; Apice, G.; et al. Platelet gel in cutaneous radiation dermatitis. Support. Care Cancer 2013, 21, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Piccin, A.; Di Pierro, A.M.; Tagnin, M.; Russo, C.; Fustos, R.; Corvetta, D.; Primerano, M.; Magri, E.; Conci, V.; Gentilini, I.; et al. Healing of a soft tissue wound of the neck and jaw osteoradionecrosis using platelet gel. Regen. Med. 2016, 11, 459–463. [Google Scholar] [CrossRef]
- Tang, Q.; Zhao, F.; Yu, X.; Wu, L.; Lu, Z.; Yan, S. The role of radioprotective spacers in clinical practice: A review. Quant. Imag. Med. Surg. 2018, 8, 514–524. [Google Scholar] [CrossRef]
- Pinkawa, M.; Corral, N.E.; Caffaro, M.; Piroth, M.D.; Holy, R.; Djukic, V.; Otto, G.; Schoth, F.; Eble, M.J. Application of a spacer gel to optimize three-dimensional conformal and intensity modulated radiotherapy for prostate cancer. Radiother. Oncol. 2011, 100, 436–441. [Google Scholar] [CrossRef]
- Ng, M.; Brown, E.; Williams, A.; Chao, M.; Lawrentschuk, N.; Chee, R. Fiducial markers and spacers in prostate radiotherapy: Current applications. BJU Int. 2014, 113 (Suppl. 2), 13–20. [Google Scholar] [CrossRef]
- Rao, A.D.; Coquia, S.; De Jong, R.; Gourin, C.; Page, B.; Latronico, D.; Dah, S.; Su, L.; Clarke, S.; Schultz, J.; et al. Effects of biodegradable hydrogel spacer injection on contralateral submandibular gland sparing in radiotherapy for head and neck cancers. Radiother. Oncol. 2018, 126, 96–99. [Google Scholar] [CrossRef]
- Murakami, N.; Nakamura, S.; Kashihara, T.; Kato, T.; Shibata, Y.; Takahashi, K.; Inaba, K.; Okuma, K.; Igaki, H.; Nakayama, Y.; et al. Hyaluronic acid gel injection in rectovaginal septum reduced incidence of rectal bleeding in brachytherapy for gynecological malignancies. Brachytherapy 2020, 19, 154–161. [Google Scholar] [CrossRef]
- Yang, X.; Ren, H.; Guo, X.; Hu, C.; Fu, J. Radiation-induced skin injury: Pathogenesis, treatment, and management. Aging 2020, 12, 23379–23393. [Google Scholar] [CrossRef]
- Rose, P. Radiation-induced skin toxicity: Prophylaxis or management? J. Med. Radiat. Sci. 2020, 67, 168–169. [Google Scholar] [CrossRef] [PubMed]
- Suman, S.; Domingues, A.; Ratajczak, J.; Ratajczak, M.Z. Potential Clinical Applications of Stem Cells in Regenerative Medicine. Adv. Exp. Med. Biol. 2019, 1201, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Hoang, D.M.; Pham, P.T.; Bach, T.Q.; Ngo, A.T.L.; Nguyen, Q.T.; Phan, T.T.K.; Nguyen, G.H.; Le, P.T.T.; Hoang, V.T.; Forsyth, N.R.; et al. Stem cell-based therapy for human diseases. Signal Transduct. Target. Ther. 2022, 7, 272. [Google Scholar] [CrossRef]
- olarevic, V.; Arsenijevic, N.; Lukic, M.L.; Stojkovic, M. Concise review: Mesenchymal stem cell treatment of the complications of diabetes mellitus. Stem Cells 2011, 29, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.; Blasco-Morente, G.; Cuende, N.; Arias-Santiago, S. Mesenchymal stromal cells: Properties and role in management of cutaneous diseases. J. Eur. Acad. Dermatol. 2017, 31, 414–423. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Tavakoli, S.; Parvathaneni, R.P.; Nawale, G.N.; Oommen, O.P.; Hilborn, J.; Varghese, O.P. Dynamic covalent crosslinked hyaluronic acid hydrogels and nanomaterials for biomedical applications. Biomater. Sci. 2022, 1, 6399–6412. [Google Scholar] [CrossRef]
- Tavakoli, S.; Kisiel, M.A.; Biedermann, T.; Klar, A.S. Immunomodulation of Skin Repair: Cell-Based Therapeutic Strategies for Skin Replacement (A Comprehensive Review). Biomedicines 2022, 10, 118. [Google Scholar] [CrossRef]
- Lee, C.; Shim, S.; Jang, H.; Myung, H.; Lee, J.; Bae, C.-H.; Myung, J.K.; Kim, M.-J.; Lee, S.B.; Jang, W.-S.; et al. Human umbilical cord blood-derived mesenchymal stromal cells and small intestinal submucosa hydrogel composite promotes combined radiation-wound healing of mice. Cytotherapy 2017, 19, 1048–1059. [Google Scholar] [CrossRef]
- Lamalice, L.; Le Boeuf, F.; Huot, J. Endothelial cell migration during angiogenesis. Circ. Res. 2007, 100, 782–794. [Google Scholar] [CrossRef]
- Lin, X.; Robinson, M.; Petrie, T.; Spandler, V.; Boyd, W.D.; Sondergaard, C.S. Small intestinal submucosa-derived extracellular matrix bioscaffold significantly enhances angiogenic factor secretion from human mesenchymal stromal cells. Stem Cell Res. Ther. 2015, 6, 164. [Google Scholar] [CrossRef]
- Park, S.J.; Cho, W.; Kim, M.S.; Gu, B.K.; Kang, C.M.; Khang, G.; Kim, C. Substance-P and transforming growth factor-β in chitosan microparticle-pluronic hydrogel accelerates regenerative wound repair of skin injury by local ionizing radiation. J. Tissue Eng. Regen M 2018, 12, 890–896. [Google Scholar] [CrossRef] [PubMed]
- Kulshrestha, S.; Chawla, R.; Singh, S.; Yadav, P.; Sharma, N.; Goel, R.; Ojha, H.; Kumar, V.; Adhikari, J. Protection of sildenafil citrate hydrogel against radiation-induced skin wounds. Burns 2020, 46, 1157–1169. [Google Scholar] [CrossRef] [PubMed]
- Hao, J.; Sun, M.; Li, D.; Zhang, T.; Li, J.; Zhou, D. An IFI6-based hydrogel promotes the healing of radiation-induced skin injury through regulation of the HSF1 activity. J. Nanobiotechnol. 2022, 20, 288. [Google Scholar] [CrossRef]
- Aysan, E.; Idiz, U.O.; Elmas, L.; Saglam, E.K.; Akgun, Z.; Yucel, S.B. Effects of Boron-Based Gel on Radiation-Induced Dermatitis in Breast Cancer: A Double-Blind, Placebo-Controlled Trial. J. Investig. Surg. 2017, 30, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Sahin, F.; Pirouzpanah, M.B.; Bijanpour, H.; Mohammadzadeh, M.; Zamiri, R.E.; Jangjoo, A.G.; Nasiri, B.; Saboori, H.; Doğan, A.; Demirci, S.; et al. The Preventive Effects of Boron-Based Gel on Radiation Dermatitis in Patients Being Treated for Breast Cancer: A Phase III Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Oncol. Res. Treat. 2022, 45, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; He, J.; Guo, B. Functional Hydrogels as Wound Dressing to Enhance Wound Healing. ACS Nano 2021, 15, 12687–12722. [Google Scholar] [CrossRef] [PubMed]
- Heggie, S.; Bryant, G.P.; Tripcony, L.; Keller, J.; Rose, P.; Glendenning, M.; Heath, J. A Phase III study on the efficacy of topical aloe vera gel on irradiated breast tissue. Cancer Nurs. 2002, 25, 442–451. [Google Scholar] [CrossRef]
- Gollins, S.; Gaffney, C.; Slade, S.; Swindell, R. RCT on gentian violet versus a hydrogel dressing for radiotherapy-induced moist skin desquamation. J. Wound Care 2008, 17, 268–270, 272, 274–275. [Google Scholar] [CrossRef]
- Kouloulias, V.; Asimakopoulos, C.; Tolia, M.; Filippou, G.; Platoni, K.; Dilvoi, M.; Beli, I.; Georgakopoulos, J.; Patatoukas, G.; Kelekis, N. Sucralfate gel as a radioprotector against radiation induced dermatitis in a hypo-fractionated schedule: A non-randomized study. Hippokratia 2013, 17, 126–129. [Google Scholar]
- Iacovelli, N.A.; Naimo, S.; Bonfantini, F.; Cavallo, A.; Bossi, P.; Fallai, C.; Pignoli, E.; Alfieri, S.; Bergamini, C.; Favales, F.; et al. Preemptive treatment with Xonrid®, a medical device to reduce radiation induced dermatitis in head and neck cancer patients receiving curative treatment: A pilot study. Support. Care Cancer 2017, 25, 1787–1795. [Google Scholar] [CrossRef]
- Ferreira, E.B.; Ciol, M.A.; De Meneses, A.G.; Bontempo, P.D.S.M.; Hoffman, J.M.; Dos Reis, P.E.D. Chamomile Gel versus Urea Cream to Prevent Acute Radiation Dermatitis in Head and Neck Cancer Patients: Results from a Preliminary Clinical Trial. Integr. Cancer Ther. 2020, 19, 1872180606. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.; Sung, K.; Kim, H.J.; Choi, Y.E.; Lee, Y.K.; Kim, J.S.; Lee, S.K.; Roh, J.-Y. Reducing Radiation Dermatitis Using a Film-forming Silicone Gel During Breast Radiotherapy: A Pilot Randomized-controlled Trial. Vivo 2020, 34, 413–422. [Google Scholar] [CrossRef]
- Tungkasamit, T.; Chakrabandhu, S.; Samakgarn, V.; Kunawongkrit, N.; Jirawatwarakul, N.; Chumachote, A.; Chitapanarux, I. Reduction in severity of radiation-induced dermatitis in head and neck cancer patients treated with topical aloe vera gel: A randomized multicenter double-blind placebo-controlled trial. Eur. J. Oncol. Nurs. 2022, 59, 102164. [Google Scholar] [CrossRef] [PubMed]
- Pacheco, R.; Stock, H. Effects of radiation on bone. Curr. Osteoporos. Rep. 2013, 11, 299–304. [Google Scholar] [CrossRef] [PubMed]
- O’Dell, K.; Sinha, U. Osteoradionecrosis. Oral Maxil. Surg. Clin. 2011, 23, 455–464. [Google Scholar] [CrossRef] [PubMed]
- Chronopoulos, A.; Zarra, T.; Ehrenfeld, M.; Otto, S. Osteoradionecrosis of the jaws: Definition, epidemiology, staging and clinical and radiological findings. A concise review. Int. Dent. J. 2018, 68, 22–30. [Google Scholar] [CrossRef]
- Marx, R.E. Osteoradionecrosis: A new concept of its pathophysiology. J. Oral Maxil. Surg. 1983, 41, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Delanian, S.; Lefaix, J.L. The radiation-induced fibroatrophic process: Therapeutic perspective via the antioxidant pathway. Radiother. Oncol. 2004, 73, 119–131. [Google Scholar] [CrossRef]
- Rice, N.; Polyzois, I.; Ekanayake, K.; Omer, O.; Stassen, L. The management of osteoradionecrosis of the jaws--a review. Surg. J. R Coll. Surg. E 2015, 13, 101–109. [Google Scholar] [CrossRef]
- Haroun, K.; Coblens, O.M. Reconstruction of the mandible for osteoradionecrosis. Curr. Opin. Otolaryngo. 2019, 27, 401–406. [Google Scholar] [CrossRef]
- Springer, I.N.; Niehoff, P.; Açil, Y.; Marget, M.; Lange, A.; Warnke, P.H.; Pielenz, H.; Roldán, J.C.; Wiltfang, J. BMP-2 and bFGF in an irradiated bone model. J. Cranio. Maxill. Surg. 2008, 36, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Lagarrigue, P.; Soulié, J.; Chabrillac, E.; Darcos, V.; Grossin, D.; Vergez, S.; Combes, C.; Dupret-Bories, A. Biomaterials and osteoradionecrosis of the jaw: Review of the literature according to the SWiM methodology. Eur. Ann. Otorhinolary 2022, 139, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Gundestrup, A.K.; Lynggaard, C.D.; Forner, L.; Heino, T.J.; Jakobsen, K.K.; Fischer-Nielsen, A.; Grønhøj, C.; von Buchwald, C. Mesenchymal Stem Cell Therapy for Osteoradionecrosis of the Mandible: A Systematic Review of Preclinical and Human Studies. Stem Cell Rev. Rep. 2020, 16, 1208–1221. [Google Scholar] [CrossRef] [PubMed]
- Jin, I.G.; Kim, J.H.; Wu, H.-G.; Kim, S.K.; Park, Y.; Hwang, S.J. Effect of bone marrow-derived stem cells and bone morphogenetic protein-2 on treatment of osteoradionecrosis in a rat model. J. Cranio. Maxill. Surg. 2015, 43, 1478–1486. [Google Scholar] [CrossRef] [PubMed]
- Park, H.S.; Lee, J.; Kim, J.-W.; Kim, H.Y.; Jung, S.Y.; Lee, S.M.; Park, C.H.; Kim, H.S. Preventive effects of tonsil-derived mesenchymal stem cells on osteoradionecrosis in a rat model. Head Neck 2018, 40, 526–535. [Google Scholar] [CrossRef]
- Ehrhart, N.P.; Hong, L.; Morgan, A.L.; Eurell, J.A.; Jamison, R.D. Effect of transforming growth factor-beta1 on bone regeneration in critical-sized bone defects after irradiation of host tissues. Am. J. Vet. Res. 2005, 66, 1039–1045. [Google Scholar] [CrossRef]
- Scala, M.; Gipponi, M.; Mereu, P.; Strada, P.; Corvo, R.; Muraglia, A.; Massa, M.; Bertoglio, S.; Santi, P.; Cafiero, F. Regeneration of mandibular osteoradionecrosis defect with platelet rich plasma gel. Vivo 2010, 24, 889–893. [Google Scholar]
- Leiker, A.J.; Desai, N.B.; Folkert, M.R. Rectal radiation dose-reduction techniques in prostate cancer: A focus on the rectal spacer. Future Oncol. 2018, 14, 2773–2788. [Google Scholar] [CrossRef]
- Harvey, M.; Ong, W.L.; Chao, M.; Udovicich, C.; McBride, S.; Bolton, D.; Eastham, J.; Perera, M. Comprehensive review of the use of hydrogel spacers prior to radiation therapy for prostate cancer. BJU Int. 2022, 131, 280–287. [Google Scholar] [CrossRef]
- Iijima, K.; Murakami, N.; Nakamura, S.; Nishioka, S.; Chiba, T.; Kuwahara, J.; Takemori, M.; Nakayama, H.; Kashihara, T.; Okuma, K.; et al. Configuration analysis of the injection position and shape of the gel spacer in gynecologic brachytherapy. Brachytherapy 2021, 20, 95–103. [Google Scholar] [CrossRef]
- Yasin, A.; Ren, Y.; Li, J.; Sheng, Y.; Cao, C.; Zhang, K. Advances in Hyaluronic Acid for Biomedical Applications. Front. Bioeng. Biotech. 2022, 10, 910290. [Google Scholar] [CrossRef] [PubMed]
- Karsh, L.I.; Gross, E.T.; Pieczonka, C.M.; Aliotta, P.J.; Skomra, C.J.; Ponsky, L.E.; Nieh, P.T.; Han, M.; Hamstra, D.A.; Shore, N.D. Absorbable Hydrogel Spacer Use in Prostate Radiotherapy: A Comprehensive Review of Phase 3 Clinical Trial Published Data. Urology 2018, 115, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Yu, L.; Ding, J. PEG-based thermosensitive and biodegradable hydrogels. Acta Biomater. 2021, 128, 42–59. [Google Scholar] [CrossRef] [PubMed]
- Pinkawa, M.; Berneking, V.; Schlenter, M.; Krenkel, B.; Eble, M.J. Quality of life after radiotherapy for prostate cancer with a hydrogel spacer—Five year results. Int. J. Radiat. Oncol. Biol. Phys. 2017, 99, 374–377. [Google Scholar] [CrossRef] [PubMed]
- Uhl, M.; Herfarth, K.; Eble, M.J.; Pinkawa, M.; Van Triest, B.; Kalisvaart, R.; Weber, D.C.; Miralbell, R.; Song, D.Y.; Deweese, T.L. Absorbable hydrogel spacer use in men undergoing prostate cancer radiotherapy: 12 month toxicity and proctoscopy results of a prospective multicenter phase II trial. Radiat. Oncol. 2014, 9, 96. [Google Scholar] [CrossRef]
- Highley, C.B.; Prestwich, G.D.; Burdick, J.A. Recent advances in hyaluronic acid hydrogels for biomedical applications. Curr. Opin. Biotech. 2016, 40, 35–40. [Google Scholar] [CrossRef]
- Wilder, R.B.; Barme, G.A.; Gilbert, R.F.; Holevas, R.E.; Kobashi, L.I.; Reed, R.R.; Solomon, R.S.; Walter, N.L.; Chittenden, L.; Mesa, A.V.; et al. Cross-Linked Hyaluronan Gel Reduces the Acute Rectal Toxicity of Radiotherapy for Prostate Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2010, 77, 824–830. [Google Scholar] [CrossRef]
- Kishi, K.; Iida, T.; Ojima, T.; Sonomura, T.; Shirai, S.; Nakai, M.; Sato, M.; Yamaue, H. Esophageal gel-shifting technique facilitating eradicative boost or reirradiation to upper mediastinal targets of recurrent nerve lymph node without damaging esophagus. J. Radiat. Res. 2013, 54, 748–754. [Google Scholar] [CrossRef]
- Xu, Q.; Torres, J.E.; Hakim, M.; Babiak, P.M.; Pal, P.; Battistoni, C.M.; Nguyen, M.; Panitch, A.; Solorio, L.; Liu, J.C. Collagen- and hyaluronic acid-based hydrogels and their biomedical applications. Mat. Sci. Eng. R 2021, 146, 100641. [Google Scholar] [CrossRef]
- Noyes, W.R.; Hosford, C.C.; Schultz, S.E. Human collagen injections to reduce rectal dose during radiotherapy. Int. J. Radiat. Oncol. 2012, 82, 1918–1922. [Google Scholar] [CrossRef]
- Rajan, R.R.; Chandrasekharan, G. Pulmonary injury associated with radiation therapy—Assessment, complications and therapeutic targets. Biomed. Pharmacother. 2017, 89, 1092–1104. [Google Scholar] [CrossRef] [PubMed]
- Giridhar, P.; Mallick, S.; Rath, G.K.; Julka, P.K. Radiation induced lung injury: Prediction, assessment and management. Asian Pac. J. Cancer Prev. 2015, 16, 2613–2617. [Google Scholar] [CrossRef] [PubMed]
- Pati, F.; Jang, J.; Ha, D.-H.; Kim, S.W.; Rhie, J.-W.; Shim, J.-H.; Kim, D.-H.; Cho, D.-W. Printing three-dimensional tissue analogues with decellularized extracellular matrix bioink. Nat. Commun. 2014, 5, 3935. [Google Scholar] [CrossRef] [PubMed]
- Murro, D.; Jakate, S. Radiation esophagitis. Arch. Pathol. Lab. Med. 2015, 139, 827–830. [Google Scholar] [CrossRef]
- Ha, D.-H.; Chae, S.; Lee, J.Y.; Kim, J.Y.; Yoon, J.; Sen, T.; Lee, S.-W.; Kim, H.J.; Cho, J.H.; Cho, D.-W. Therapeutic effect of decellularized extracellular matrix-based hydrogel for radiation esophagitis by 3D printed esophageal stent. Biomaterials 2021, 266, 120477. [Google Scholar] [CrossRef] [PubMed]
- Kim, I.G.; Cho, H.; Shin, J.; Cho, J.H.; Cho, S.-W.; Chung, E.-J. Regeneration of irradiation-damaged esophagus by local delivery of mesenchymal stem-cell spheroids encapsulated in a hyaluronic-acid-based hydrogel. Biomater. Sci. 2021, 9, 2197–2208. [Google Scholar] [CrossRef]
- Hauer-Jensen, M.; Denham, J.W.; Andreyev, H.J. Radiation enteropathy--pathogenesis, treatment and prevention. Nat. Rev. Gastro. Hepat. 2014, 11, 470–479. [Google Scholar] [CrossRef] [PubMed]
- Marshall, J. Radiation and the ageing eye. Ophthal. Physl. Opt. 1985, 5, 241–263. [Google Scholar] [CrossRef]
- Grumetto, L.; DEL Prete, A.; Ortosecco, G.; Barbato, F.; Del Prete, S.; Borrelli, A.; Schiattarella, A.; Mancini, R.; Mancini, A. Study on the Protective Effect of a New Manganese Superoxide Dismutase on the Microvilli of Rabbit Eyes Exposed to UV Radiation. Biomed. Res. Int. 2015, 2015, 973197. [Google Scholar] [CrossRef]
- Zhao, H.; Huang, J.; Li, Y.; Lv, X.; Zhou, H.; Wang, H.; Xu, Y.; Wang, C.; Wang, J.; Liu, Z. ROS-scavenging hydrogel to promote healing of bacteria infected diabetic wounds. Biomaterials 2020, 258, 120286. [Google Scholar] [CrossRef]




| Study | Hydrogel Type | Characteristics | Stowage | Function | Model Type | Radiation Type |
|---|---|---|---|---|---|---|
| Zhao 2021 [37] | NaHA hydrogels | Unique viscoelasticity, good water retention, tissue compatibility, and non-immunogenicity | Fullerenols | Protect epidermal stem cells | RISI in rat | Electron rays (6 MeV) |
| Zhang 2021 [38] | Alginate/HA/polysine hydrogels | Anti-biofouling and antioxidant | Curcumin and epigallocatechin gallate | Alleviate inflammation, scavenge ROS, and promote angiogenesis. | RISI in rat | X-ray (40 Gy) |
| Nie 2022 [41] | Self-assembled peptide hydrogel | Biodegradable and biocompatible, bioadhesion properties | Gingiva-derived MSCs | Improve wound healing | RISI in rat | 137Cs γ-ray (50 Gy) |
| LEE 2017 [58] | Small intestinal dreived-ECM hydrogel | Biocompatibility | Human umbilical cord blood-derived-MSCs | Enhanced wound healing and the angiogenesis | Combined radiation-wound in rat | X-ray (5 Gy) |
| Park 2018 [61] | Chitosan microparticlepluronic F127 hydrogel | Thermo-responsive | Substance P and transforming growth factor-β1 | Accelerates regenerative wound repair | RISI in rat | 60Co γ-ray (40 Gy) |
| Kulshrestha 2020 [62] | Citrate-Based Hydrogel | Combined property of lipid based drug delivery | Sildenafil | Improve delayed wound healing | RISI in rat | 60Co γ-ray (45 Gy) |
| Hao 2022 [63] | Graphene oxide/Sodium alginate Based(GO/SA) hydrogels | Biocompatibility, antibacterial, radioresistance, sprayable | Interferon-alpha inducible protein 6, Polydopamine | Improve inflammation and induce granulation tissue formation, angiogenesis | RISI in rat | Electron rays (6 MeV) |
| Study | Research Type | Patients Type | Number of Patients | Hydrogel Type | Characteristics of Hydrogel | Controls | Resuts |
|---|---|---|---|---|---|---|---|
| Aysan 2017 [64] | RCT | BC | 47 | Boron-based gel | Antioxidant properties | Placebo | Positive |
| Tungkasamit 2022 [65] | RCT | HNC | 120 | Aloe vera gel | Anti-inflammatory | Placebo gel | Positive |
| Heggie 2002 [67] | RCT | BC | 225 | Aloe Vera Gel | Anti-inflammatory and antibacterial. | Aqueous cream | Negative |
| Gollins 2008 [68] | RCT | HNC or BC | 30 | Cross-linked polyethylene oxide hydrogel | NA | Gentian violet | Positive |
| Kouloulias 2013 [69] | Single arm study | BC | 30 | Sucralfate gel | Promotes angiogenesis, anti-inflammatory | Historical controls | Positive |
| Iacovelli 2017 [70] | Single arm study | HNC | 41 | Hyaluronic acid gel (Xonrid®) | Hygroscopic moisturizing effect; emollient, softening, nourishing properties. | Historical controls | Positive |
| Ahn 2020 [71] | RCT | BC | 56 | Silicone gel(Strata XRT®) | Promote a moist wound-healing environment. | Moisturizing cream(X-derm®) | Positive |
| Ferreira 2020 [72] | RCT | HNC | 48 | Chamomile gel | Anti-inflammatory | Cream of urea | Positive |
| Sahin 2022 [73] | RCT | BC | 257 | Boron-Based Gel | NA | Placebo gel | Positive |
| Study | Hydrogel Type | Characteristics | Stowage | Model Type | Evaluation Indicator | Radiation Type |
|---|---|---|---|---|---|---|
| Jin 2015 [84] | HA-based hydrogel | MMP-sensitive, | Rat MSCs and bone morphogenetic protein-2 | Osteoradionecrosis in the rat mandible | BV and BMD | X-ray(30 Gy) |
| Park 2017 [85] | Matrigel® matrix | Promote bone regeneration | Tonsil-derived MSCs | Osteoradionecrosis in a rat model | BMD, BV, BV/TV, and TTV | X-ray(20 Gy) |
| Ehrhart 2005 [86] | Gelatin hydrogel | Localized and sustained drug release | Transforming growth factor-β1 | Irradiated long-bone defects in rabbit | The amounts of bone formation | 60Co γ-ray (50 Gy) |
| Study | Hydrogel Type | Characteristics | Mode of Presentation | Stowage | Model Type | Evaluation Indicator |
|---|---|---|---|---|---|---|
| Zhou 2019 [42] | Lung tissue ECM hydrogel | Affect cell behavior and influence remodeling outcomes | Endotracheal injection | - | Radiation-induced lung injury in mice | Lung histopathology injury and pulmonary edema |
| Ha 2021 [105] | Esophagus-derived dECM hydrogel | Promote tissue regeneration | Loaded in esophageal stents | - | Radiation esophagitis rat model | Histological morphology and inflammatory responses |
| Kim 2021 [106] | HA hydrogel | Promote tissue adhesion and cell retention | Esophagus injection | Human mesenchymal stem-cell spheroids | Radiation-induced esophageal fibrosis in rat model | Histological morphology and inflammatory responses |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.; Liu, H.; Ding, Y.; Li, W.; Zhang, Y.; Luo, S.; Xiang, Q. The Use of Hydrogel-Based Materials for Radioprotection. Gels 2023, 9, 301. https://doi.org/10.3390/gels9040301
Li Y, Liu H, Ding Y, Li W, Zhang Y, Luo S, Xiang Q. The Use of Hydrogel-Based Materials for Radioprotection. Gels. 2023; 9(4):301. https://doi.org/10.3390/gels9040301
Chicago/Turabian StyleLi, Yang, Han Liu, Yaqun Ding, Wanyu Li, Yuansong Zhang, Shenglin Luo, and Qiang Xiang. 2023. "The Use of Hydrogel-Based Materials for Radioprotection" Gels 9, no. 4: 301. https://doi.org/10.3390/gels9040301
APA StyleLi, Y., Liu, H., Ding, Y., Li, W., Zhang, Y., Luo, S., & Xiang, Q. (2023). The Use of Hydrogel-Based Materials for Radioprotection. Gels, 9(4), 301. https://doi.org/10.3390/gels9040301






