Abstract
Whole-body cryotherapy (WBC) is a therapeutic practice involving brief exposure to extreme cold, typically lasting one to four minutes. Given that WBC sessions often occur in groups, there is a hypothesis that cumulative heat dissipation from the group significantly affects the thermo-aerodynamic conditions of the cryotherapy chamber. Computational fluid dynamics (CFD) is employed to investigate thermal exchanges between three subjects (one man, two women) and a cryotherapy chamber at −92 °C during a 3-minute session. The investigation reveals that collective body heat loss significantly influences temperature fields within the cabin, causing global modifications in aerodynamic and thermal conditions. For example, a temperature difference of 6.7 °C was calculated between the average temperature in a cryotherapy chamber with a single subject and that with three subjects. A notable finding is that, under an identical protocol, the thermal response varies among individuals based on their position in the chamber. The aerodynamic and thermal characteristics of the cryotherapy chamber impact the heat released at the body’s surface and the skin-cooling rate needed to achieve recommended analgesic thresholds. This study highlights the complexity of physiological responses in WBC and emphasizes the importance of considering individual positions within the chamber for optimizing therapeutic benefits.
1. Introduction
Whole-body cryotherapy (WBC) is a therapeutic technique that involves exposing the body to extremely cold temperatures (−60° to −140 °C) for a brief period, typically lasting one to four minutes [1,2]. Recent research has revealed various benefits of cryotherapy, including physiological, psychological, and physical improvements [3]. It is widely used to alleviate pain associated with rheumatic and inflammatory conditions, such as rheumatoid arthritis, ankylosing spondylitis, fibromyalgia, and multiple sclerosis [4,5,6,7,8,9,10,11]. Additionally, athletes use cryotherapy to enhance muscle recovery and reduce post-exercise muscle soreness [12,13,14]. Beyond physical applications, cryotherapy has shown efficacy in reducing symptoms of psychiatric disorders like anxiety and depression while also improving sleep quality and overall well-being [15,16,17].
The fundamental concept of cryotherapy revolves around exposing the body to cold, inducing a thermal shock that activates thermosensitive skin receptors. This activation plays a crucial role in cryostimulation, triggering regulatory mechanisms to maintain a consistent central temperature. The changes in skin temperature become a pivotal parameter in the cryostimulation process. The efficacy of the thermal shock depends on the thermal gradient between the body and the external environment, along with the aerothermal factor influencing the patient’s perception of cold [18]. In this context, it is essential to thoroughly assess all parameters that could influence the temperature within the cryotherapy chamber, particularly focusing on the heat generated by the patient’s body. Thermal transfers between the body and its surroundings have the potential to alter temperatures within the cryotherapy chamber, either in localized areas or on a broader scale. Given the variable size of the chamber, designed for one to five patients, accurately determining the specific impact of these heat sources on the actual temperature inside the chamber poses a considerable challenge. Adjustments to the protocol duration or the set temperature may be necessary based on the number of patients present in the cryotherapy chamber.
In a recent study, we investigated the impact of the body heat loss of a single male subject on the thermal and aerodynamic conditions within a whole-body cryotherapy chamber [19]. Our findings notably highlighted that body heat losses lead to substantial alterations in temperature fields within the chamber, prompting overall adjustments in aerodynamic and thermal conditions [19,20]. However, most whole-body cryotherapy sessions take place in groups to achieve a collective cooling effect. This practice leads us to hypothesize that the cumulative heat input dissipated by this group may alter the aerodynamic and thermal conditions of the chamber.
In this study, we aim to deepen our understanding of the impact of the simultaneous presence of three subjects, comprising one man and two women, on the thermal and aerodynamic aspects of the airflow inside the whole-body cryotherapy (WBC) chamber. Through the computational fluid dynamics (CFD) methodology, these in-depth investigations will provide further insights into the cumulative effect of body heat on the internal conditions of the cryotherapy chamber when occupied by multiple individuals. The obtained results could offer crucial insights for adjusting cryotherapy protocols accordingly, thereby maximizing therapeutic benefits while accommodating variations induced by the simultaneous presence of multiple subjects.
2. Materials and Methods
2.1. Geometry and Computational Domain
The initial stage of the numerical process involves defining the geometry, encompassing the whole-body cryotherapy (WBC) chamber with three patients. For this purpose, the computer-aided design (CAD) software ANSYS Workbench© Design Modeler (ANSYS 2020 R2, ANSYS, Inc., Canonsburg, PA, USA) was utilized. The dimensions of the cryotherapy chamber are based on the actual dimensional characteristics of a commercial model (interior dimensions of 2.1 m by 2.15 m, total height of 2.25 m). The geometries of the male (height ≈ 1.9 m) and female patients (height ≈ 1.7 m) were obtained through the 3D scanning of individuals wearing cryotherapy-specific protective clothing (gloves, caps, clogs). This study focuses on the air circulation and heat transfer among the three human bodies, modeled as a heat transfer surface, and their environment, without delving into the intricate biological mechanisms of the human body.
2.2. Boundary Conditions
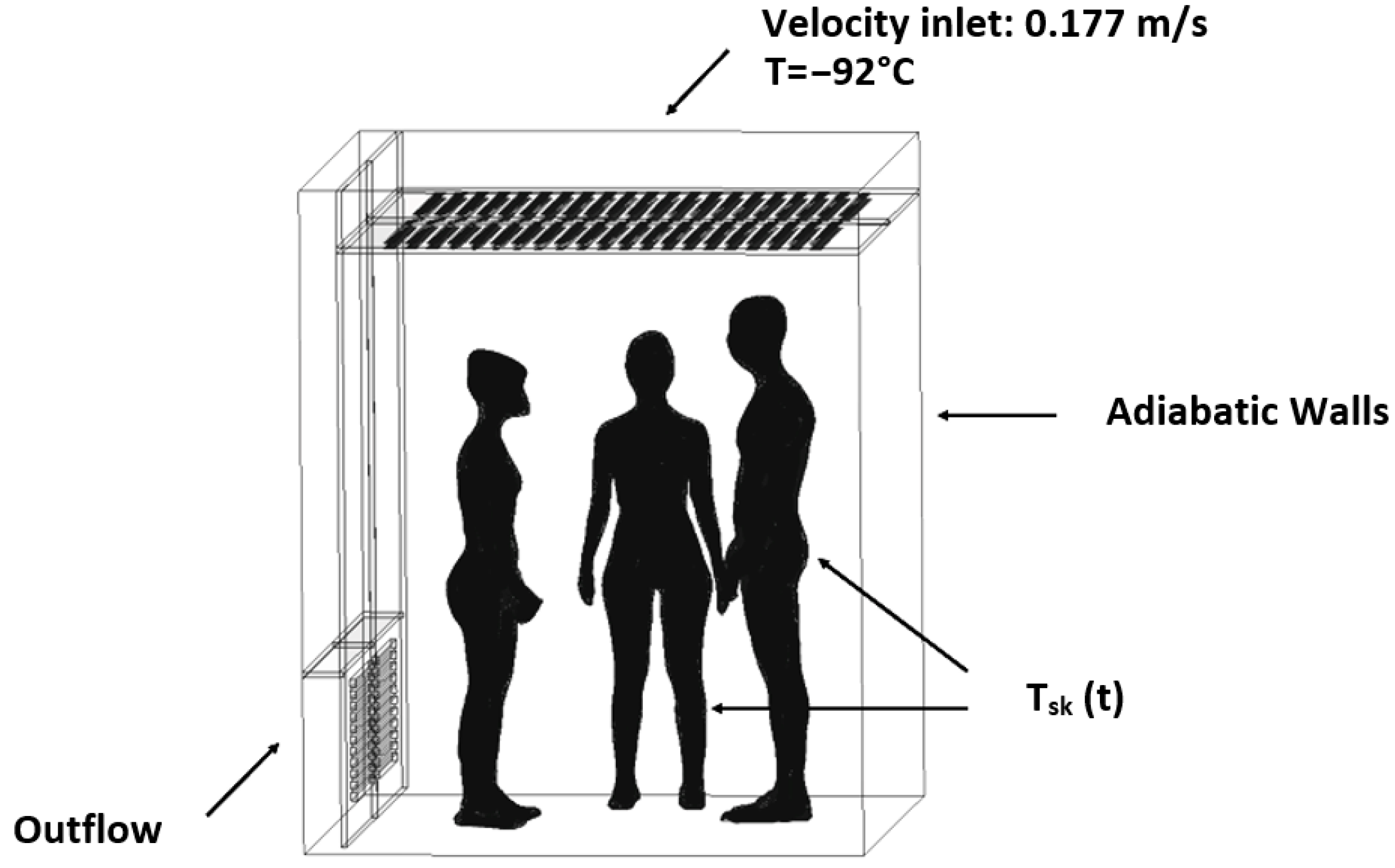
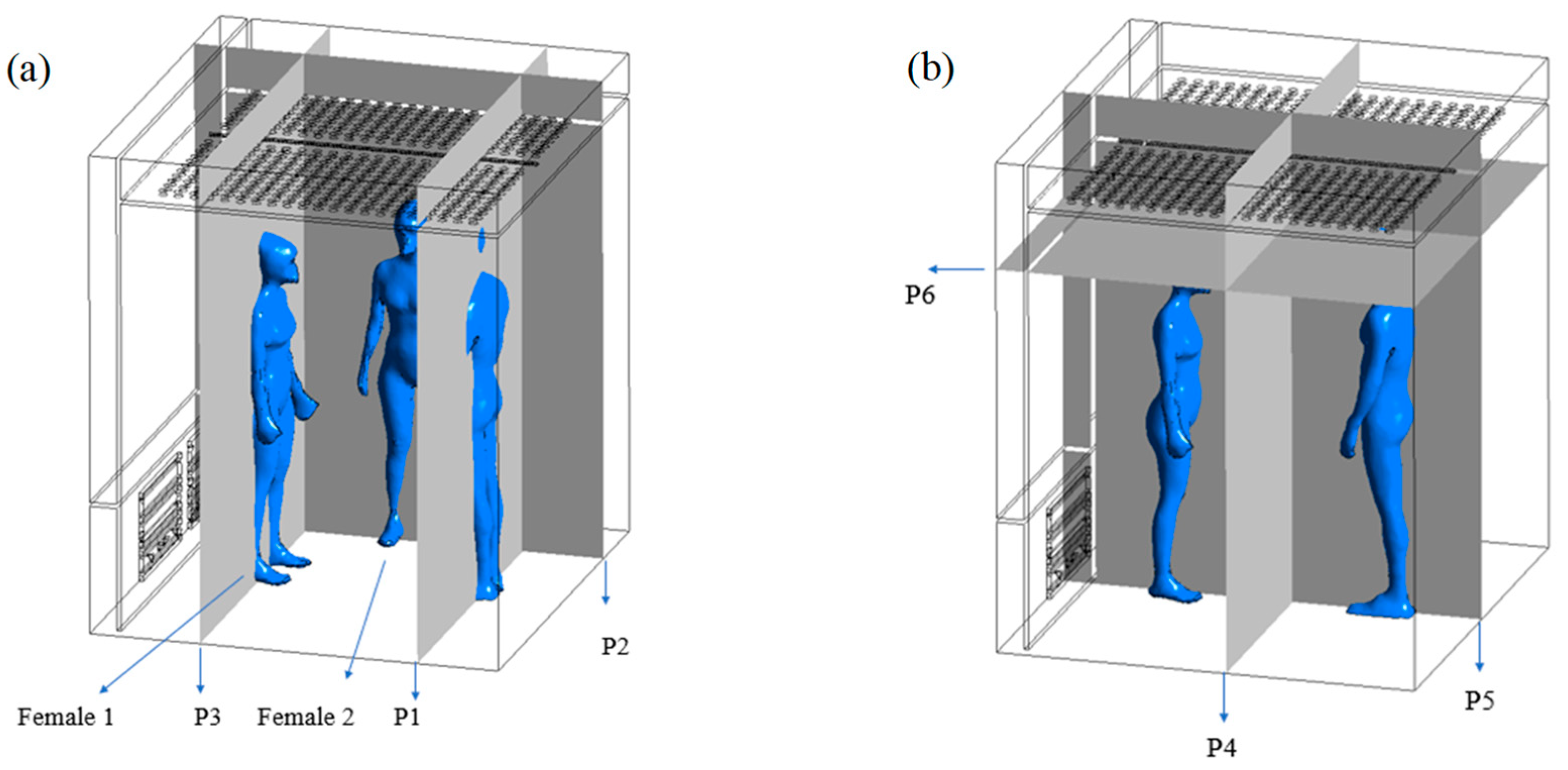
Figure 1 illustrates the computational domain and boundary conditions of the system under investigation. Specifically, cold air is introduced from the ceiling of the whole-body cryotherapy (WBC) chamber at a temperature of −92 °C and a constant velocity of 0.177 m/s. An outflow condition is implemented at the ventilation grilles located on a wall at the bottom of the chamber. To streamline computation time, adiabatic conditions are assumed for the chamber walls. To simulate variations in skin temperature throughout a whole-body cryotherapy session, a thermal boundary condition is applied to the body’s surface. This condition is represented by an equation developed from experimental data characterizing the evolution of skin temperature during a WBC session [18].
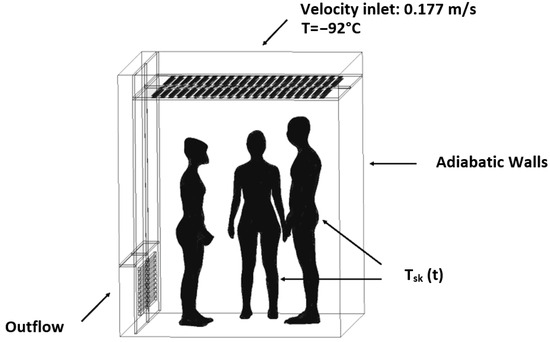
Figure 1.
Geometry and boundary conditions.
Equation (1) delineates the evolution of skin temperature during a WBC session. This mathematical model, describing the kinetics of skin cooling, was developed based on experimental data [13]. Assuming an exponential behavior for the initial transient phase [16] within the time range t ∈ [0;30], followed by a transition to a linear trend during the latter part of the transient phase from t ∈ [30;β], the time-varying skin temperature can be represented as follows:
where K, a, A, and B are constants to be analytically determined using both thermal boundary conditions and a C1-continuous junction between these two functions.
The resulting analytical expression of the skin temperature is:
Tsk0, Tsk1, and C0 are, respectively, the baseline skin temperature, the skin temperature at the end of the session, and the rate of cooling and β corresponds to the end of the session. To account for variations in the thermophysical properties of air with temperature, polynomial laws have been incorporated into the computational code. These laws enable the calculation of density, dynamic viscosity, thermal conductivity, and specific heat at each time step within the temperature range of interest (−110 °C to 33 °C). The iterative calculation is then performed to simulate a 3-min cryotherapy session with a time step of 0.03 s. It is worth noting that the time step was chosen to maximize computational efficiency while ensuring that the Courant number remains below the limit of 1.
2.3. Computational Grid
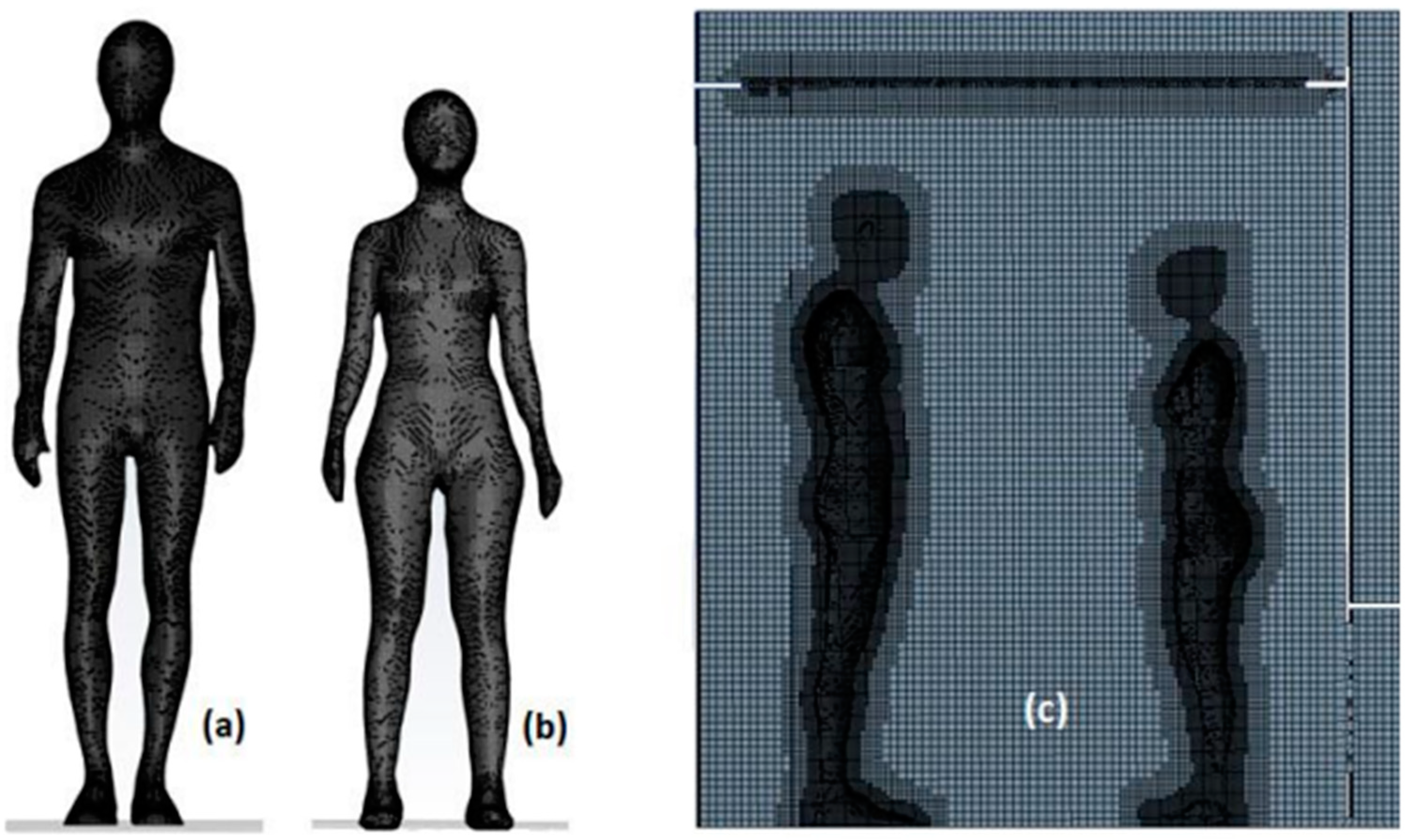
Firstly, a surface mesh is generated for the three bodies, followed by a Cartesian volumetric mesh within the fluid domain around the bodies. The maximum cell dimension within the computational domain does not exceed 0.023 m. To ensure the independence of the mesh size from the results, a grid dependency test was conducted; the results are presented in a previous study [19]. The cell dimensions around the bodies ensure a fine resolution of the boundary layer and provide adequate accuracy for thermal transfer calculations. Additionally, the use of a structured Cartesian mesh enhances result convergence and constrains the total number of mesh cells. In total, the mesh consists of approximately 3.5 million cells. Figure 2 illustrates the surface (a, b) and volumetric mesh in a plane cutting through the bodies in their symmetry plane (c).
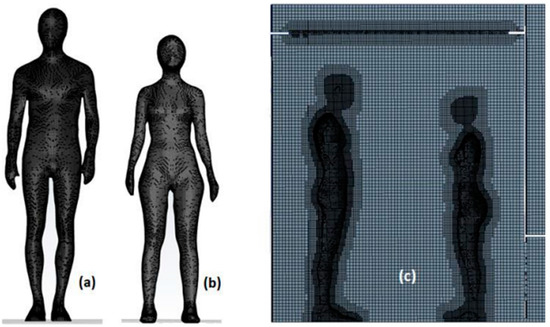
Figure 2.
Surface mesh on the male scan (a), Surface mesh on the female scan (b), Cartesian mesh of the computational domain (c).
2.4. Numerical Methods
For this study, we employed the ANSYS Fluent® 2020 R2 commercial computational code, utilizing the finite volume method for solving the governing fluid flow equations. This CFD calculation code facilitated the analysis of a three-dimensional, time-dependent, and non-isothermal numerical approach. The pressure–velocity coupling was resolved using the SIMPLE algorithm, implementing a first-order discretization scheme [21]. The standard k-ε turbulence model was chosen to accurately close the Reynolds-averaged Navier–Stokes equations over time. The following equations were utilized to describe heat and mass transfer through convection:
Mass conservation equation:
Momentum conservation equation:
Energy conservation equation (heat transfer):
where is the pressure, is the fluid density, is the time, is the fluid velocity vector, is the pressure, is the viscous stress tensor, is the specific internal energy, is the conductive heat flux vector, and represents the turbulent heat flux vector.
3. Results
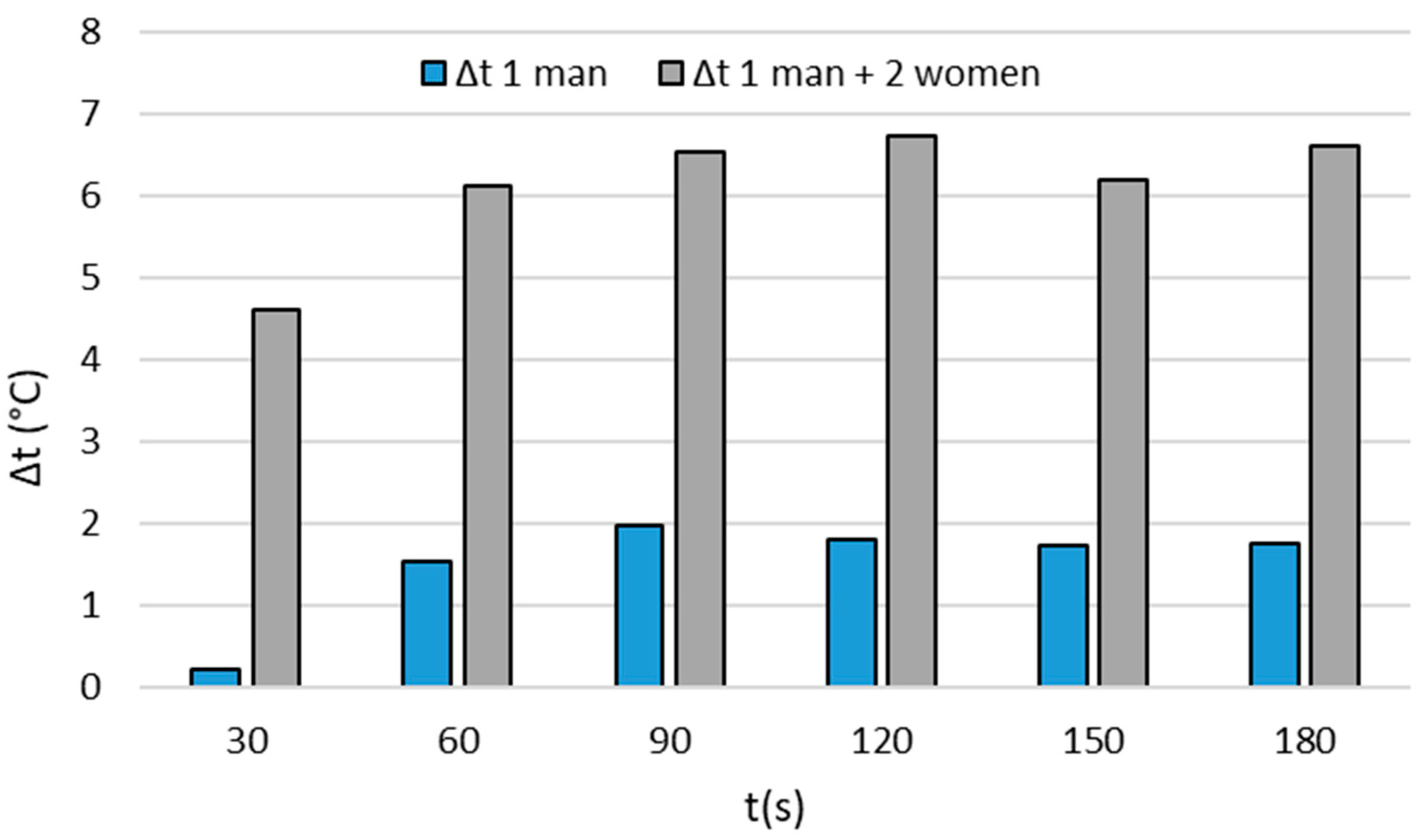
Primarily, our objective was to evaluate the influence of patients, regarded as heat sources, on the average temperature within the cryotherapy chamber. To achieve this, we leveraged findings from a prior study [19], wherein we monitored the average temperature within the empty cryotherapy chamber, serving as the reference case. Subsequently, we conducted a comparative analysis with the results obtained for a single individual (a man) and three individuals (one man and two women). The outcomes, depicted in histogram format, are illustrated in Figure 3.
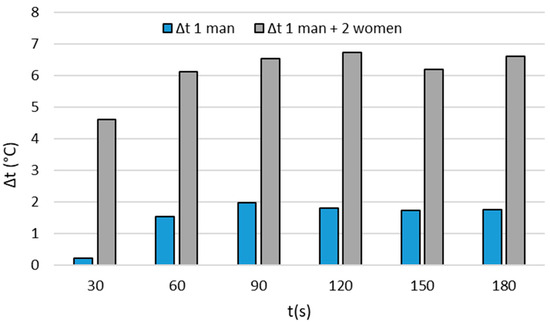
Figure 3.
Temperature difference Δt (expressed in °C) between the average temperature measured within the empty chamber and the average temperature measured within the chamber with one person (one man alone) and the chamber with three people (one man and two women).
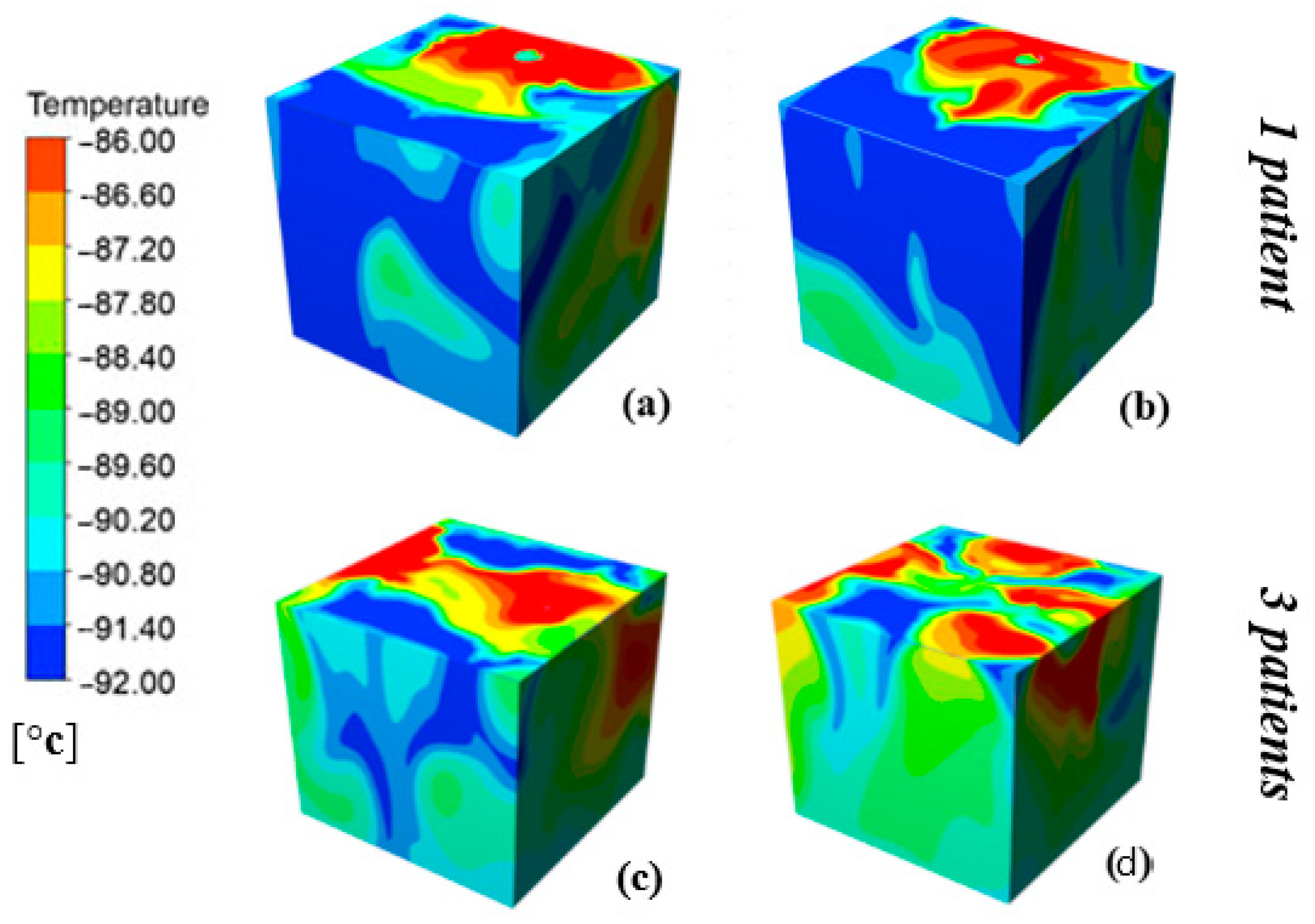
Notably, we observe that the temperature difference (Δt), expressed in °C, increases with the number of people simultaneously occupying the chamber. Hence, following the 3-min cryotherapy session, the average temperature difference between the empty chamber and the chamber with one person approaches nearly 2 °C while it reaches approximately 7 °C with three people in the chamber. This significant result underscores the impact of the human body, acting as a heat source, on the “actual” temperature within the cryotherapy chamber. To visually depict how the human body influences the temperature within the cryotherapy chamber, Figure 4 illustrates the volumetric distribution of temperatures inside the chamber when occupied by one patient and three patients at t = 120 s and t = 180 s. First and foremost, the figure clearly delineates the positions of patients within the cryotherapy chamber. The human body, exposed to extreme negative temperatures, emits a substantial amount of heat, manifesting as a temperature peak depicted in Figure 4 as red-colored patches. Additionally, there is noticeable heterogeneity in the temperature distribution, whether with one or three patients in the cryotherapy chamber. This heterogeneity arises from the heat contribution of the human bodies and the intensified convective movements resulting from the injection of cold air into the cryotherapy chamber. Significantly, there exists a temperature disparity between the chamber occupied by a single patient and the one occupied by three patients. It is evident that the presence of the coldest air (in dark blue) is more diminished with three patients. Furthermore, when comparing the results obtained at 120 s with those at the end of a 180 s cryotherapy session, it is discernible that the overall temperatures within the treatment space continue to rise.
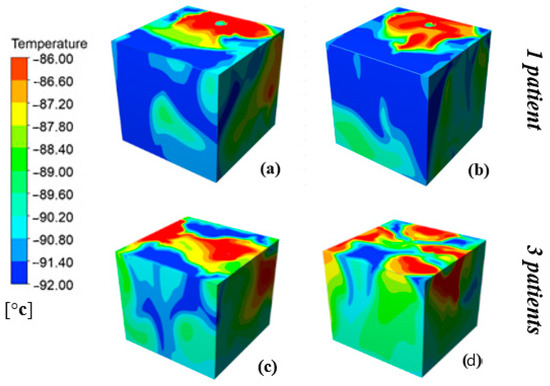
Figure 4.
Distribution of temperatures inside the cryotherapy chamber when occupied by one person (a,b) and then three people (c,d), respectively, at t = 2 min and t = 3 min.
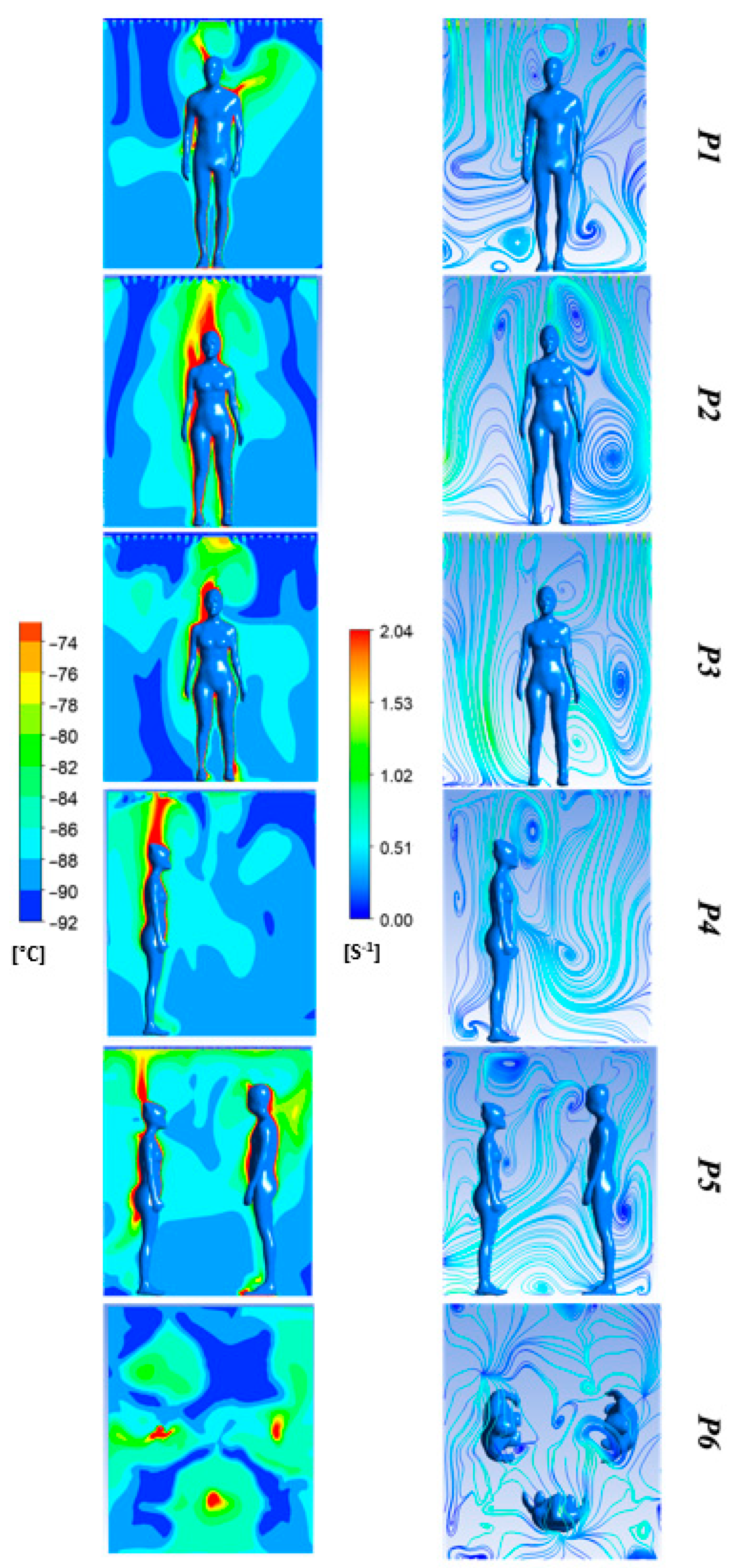
Certainly, owing to its functioning, the whole-body cryotherapy chamber produces a continual stream of cold air that actively impacts the thermodynamic dynamics of the human body. Consequently, there exists a reciprocal interaction between the human body and its immediate environment, the thermodynamic characteristics of which are also dynamically changing. In this scenario, it becomes imperative to examine not solely the thermal aspect but also the aerodynamic aspect; they are inherently interconnected. To address this, we employed distinct cross-sectional views that enabled the representation of both thermal and aerodynamic facets. The diverse sectional perspectives are illustrated in Figure 5. Figure 6 portrays both temperature distributions and streamline patterns color-coded by velocity across six different planes for t = 3 min. To emphasize even the subtlest temperature or velocity gradients, we constrained the temperature range between −92 °C and −72 °C and the velocity between 0 and 2 m/s.
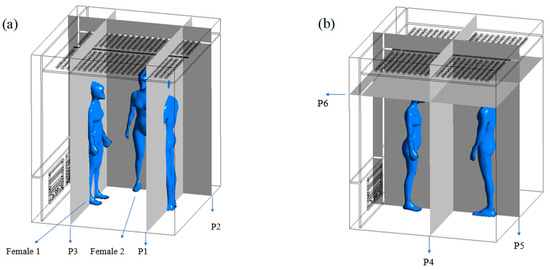
Figure 5.
Plane positions. (a) Three planes passing through the human bodies; (b) Three other planes crossing the cabin through its symmetry planes.
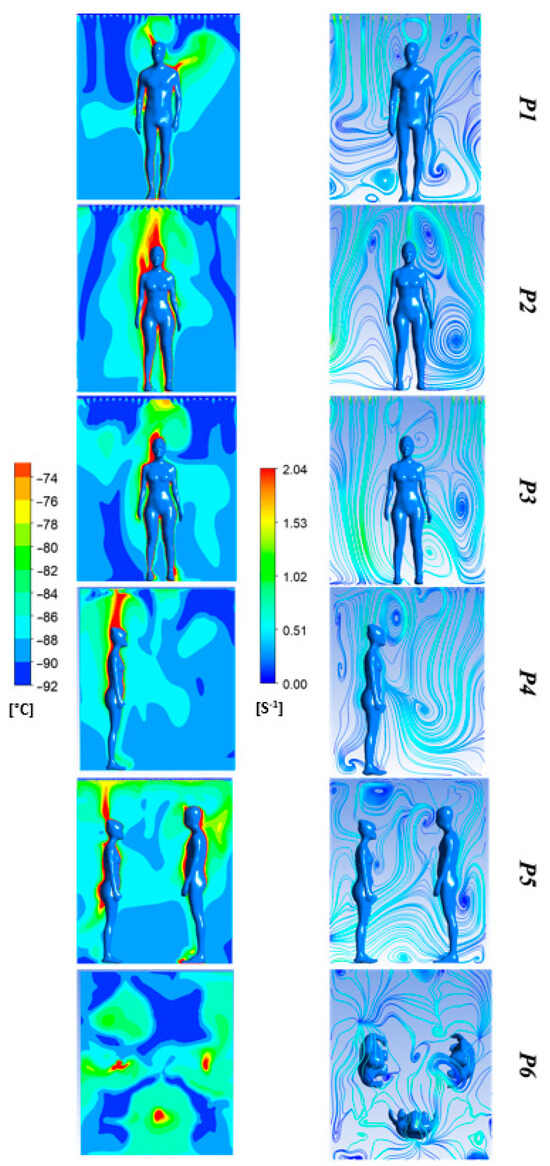
Figure 6.
Temperature fields and velocity-coded streamlines for Planes 1–6 at t = 180 s.
Whatever the subject is, a notable temperature gradient is observed between the incoming air temperature into the cryotherapy chamber and the maximum temperature, surpassing −72 °C above the human bodies. This temperature gradient is characterized by the emergence of thermal plumes that form above and around the head of each patient. The fluctuating dynamics of the natural convection plume depend significantly on the temperature disparity between the patient’s skin and the air temperature, as well as on the body surface area, which varies between the man and the two women (≈2 m2 vs. 1.7 m2). Additionally, the positioning of the patients in the cryotherapy chamber will influence heat transfers and the development of the thermal plume. Turning our attention to the airflow velocity in the cryotherapy chamber, noteworthy variations are observed with elevated velocities around the bodies and above the head, associated with the formation of the thermal plume. In this region, the velocity exceeds 1 m/s. The flow topology is intricate, featuring multiple vortex instabilities. The vortices observed above the patients’ heads result from the development of the convective thermal boundary layer induced by the temperature gradient. This boundary layer transitions into a fully turbulent flow at the upper level of the body, constituting the thermal plume. Human bodies serve a dual role as obstacles to the flow and heat sources, initiating air motion through natural convection. On Plane 5, the airflow trajectory toward the outlet is clearly discernible. It can be reasonably assumed that the patient’s position in the cryotherapy chamber will markedly influence heat transfers between the human body and its environment, thereby impacting the therapeutic efficacy of the cryotherapy session.
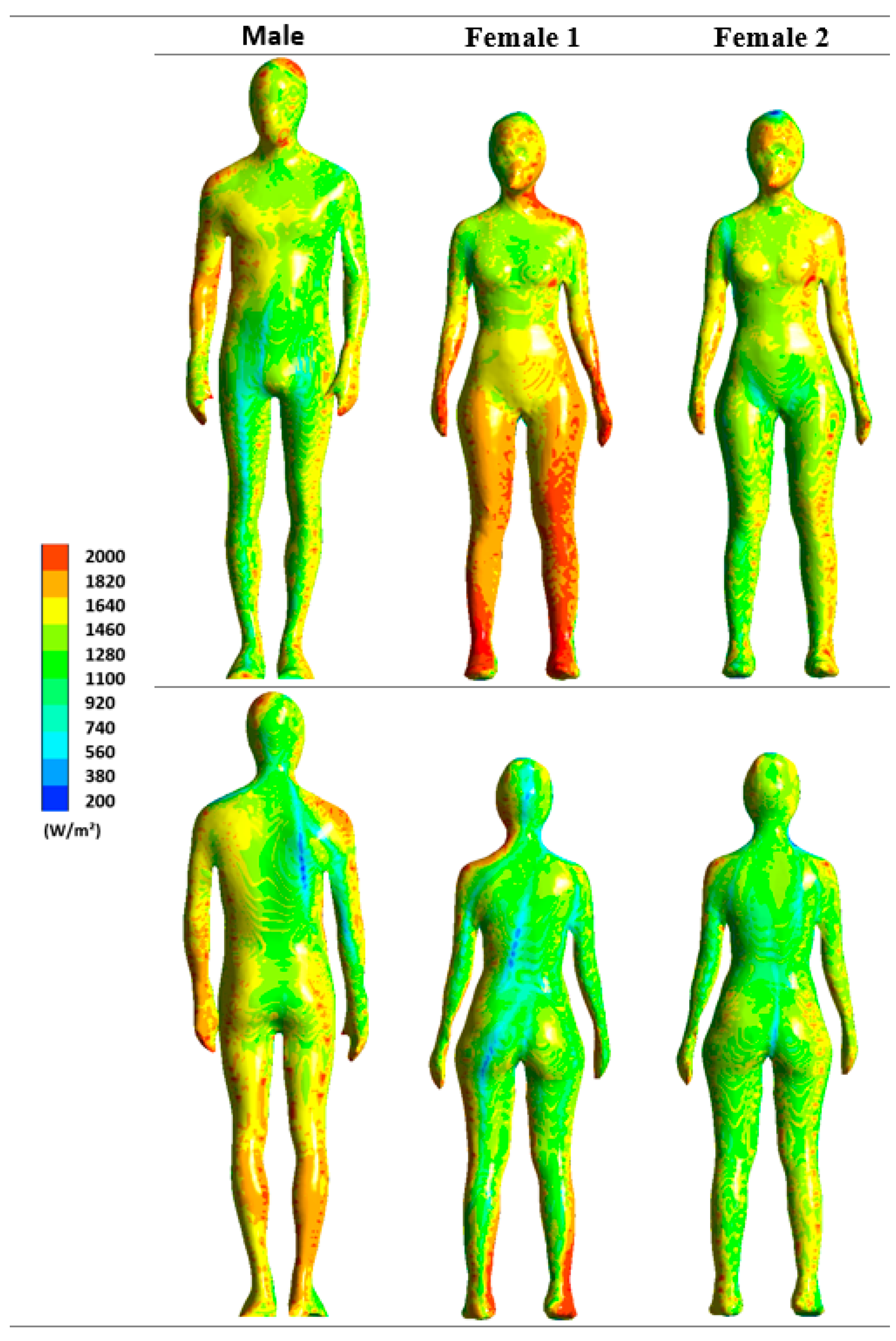
To underscore the influence of airflow and temperature distribution on the human body, we depict the distribution of surface heat flux on the bodies of the man and the two women in Figure 7. Once again, we constrained the range of heat flux to better emphasize even subtle differences. Initially, Figure 7 underscores an uneven distribution of flux on the body surface, alongside distinctions among the three patients.
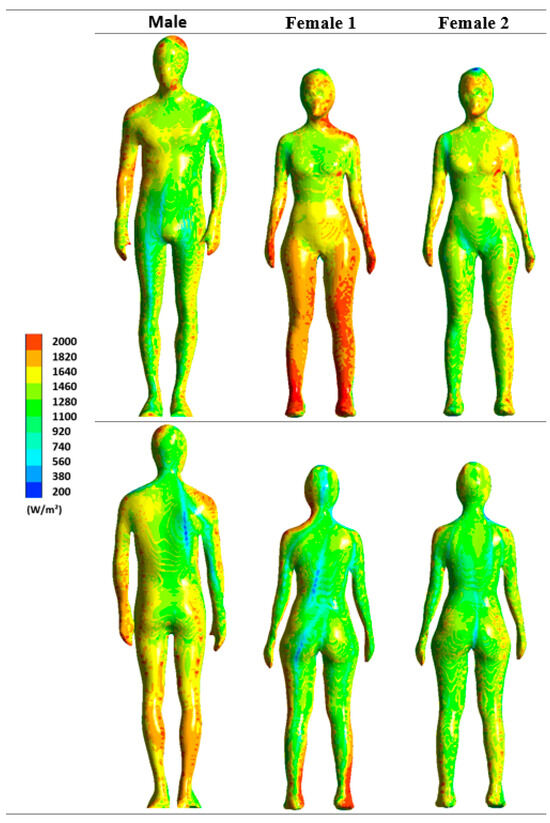
Figure 7.
Surface heat flux dissipated at t = 180 s for male and female patients.
For example, in the case of Woman 1, the arms and legs exhibit significantly higher heat dissipation, with values surpassing 2000 W/m2. Conversely, in the man, it is the back of the body that serves as the primary source of heat dissipation. When comparing the results for the three patients, it becomes evident that heat dissipation is markedly influenced by the patient’s positioning within the cryotherapy chamber. Notably, the surface flux for Woman 1 in the lower part of the body is considerably higher than for the other two patients. This discrepancy arises because Woman 1’s legs are positioned in front of the cryotherapy chamber’s air outlet, where forced convection combines with natural convection, intensifying thermal losses. There is also a discernible cause-and-effect relationship between the airflow dynamics and the distribution of heat flux on the human body’s surface. The higher the air velocity, the more pronounced the surface flux. Another critical factor is the patient’s size; the larger it is, the more time the thermal boundary layer has to develop, thereby accentuating transfers between the body and its environment. Therefore, the body surface area is crucial as a larger area facilitates greater heat exchange.
4. Discussion
The initial findings of this study underscore how patients, functioning as heat sources, affect the thermal conditions within the whole-body cryotherapy (WBC) chamber during a session. Indeed, as the ambient temperature drops below the skin temperature, the human body experiences heat loss to the surroundings due to temperature gradients [22,23]. This presence of multiple patients disrupts the initial thermal homogeneity, leading to an overall temperature increase inside the enclosure. Previous research has suggested a correlation between the presence of a patient in the cryotherapy chamber and a general rise in average temperature [19]. As cold air is denser than warm air, a thermal stratification phenomenon occurs in the cryotherapy chamber. When a patient enters a cryotherapy chamber, the temperature gradient between the patient’s body, contributing a significant amount of heat, and the internal volume of the cryotherapy chamber rapidly alters the initially created thermal stratification, leading to a sudden increase in overall temperature. Consequently, a convection phenomenon occurs, resulting in the formation of a convective thermal boundary layer enveloping the human body and a thermal plume above the head. The upward motion of heated air within the boundary layer reaches positions where it disturbs the boundary layers, expelling sizable unsteady eddies into the surrounding space, away from the human body. These combined effects contribute to a significant increase in temperature in specific areas of the body, as observed above the patients’ heads and in the upper part of the cryotherapy chamber (refer to Figure 6). Settles and Craven [24] studied the development of a thermal plume induced by the presence of an individual (with an average surface temperature of 26.6 °C) in an indoor environment (a closed and unventilated room with an air temperature of T = 21.6 °C); experimental and numerical results showed a flow velocity of 0.24 m/s above the subject’s head. In a similar vein, Liu et al. [25] conducted a computational fluid dynamics (CFD) study at an environmental temperature of 24 °C, revealing a maximum velocity of 0.23 m/s over the top of the head.
Other studies have highlighted the formation of a thermal plume around patients during WBC sessions [19,20,21] or partial-body cryotherapy (PBC) sessions [3]. In whole-body cryotherapy (WBC), Marreiro et al. [21] estimated the velocity of the thermal plume to be approximately 1.5 m/s for a target temperature of −110 °C. In a recent study, we estimated the thermal plume velocity to be around 1.3 m/s for an air injection temperature of −92 °C [19]. The results of the current study, involving the simultaneous presence of multiple patients in the cryotherapy chamber, align with the previously mentioned studies. The findings demonstrate that as the number of patients participating in the cryotherapy session simultaneously increases, the overall temperature within the treatment space will be higher. An analogy can be drawn with a room heated by electric heaters—the more heaters, the warmer the room.
This study also highlights that the positioning of patients within the room significantly impacts the distribution of surface flux, indicating the amount of heat dissipated by the human body. Indeed, the increase in heat transfer is primarily driven by a notable decrease in skin temperature, as underscored by Blokker et al. [26] in their examination of the effects of cold ambient temperature on elite biathletes.
When individuals are suddenly exposed to extreme cold, the physiological response involves a thermal shock, resulting in a decrease in skin temperature. This decrease initiates the activation of mechanisms aimed at preserving body heat and enhancing heat production, as elucidated by Kenny and Flouris [27].
The conclusions drawn from this study suggest a correlation between the number of patients simultaneously present in the cryotherapy chamber and cutaneous cooling, which is associated with the distribution of surface thermal flux. In situations of extreme cold exposure, such as in cryotherapy, the human body amplifies heat dissipation to reach significant thresholds. For example, Burkov et al. [28] estimated the heat flux from the human body to range between 1650 W/m2 and 2500 W/m2, values that align closely with our estimates in this study.
Based on experimental data from previous studies [18,21], we established a strong correlation between skin temperatures and set temperatures:
According to this equation, we can estimate the impact of the number of individuals inside the cryotherapy chamber on the average skin temperature for an equal exposure duration of 3 min and a given exposure temperature. Referring to Figure 3, the temperature difference between the chamber with one person and the one with three people is approximately 6.7 °C. Thus, utilizing Equation (7), we estimate that the average skin temperature will be 0.4 °C lower when a person is alone in the cryotherapy chamber compared to when three individuals are present. While a temperature difference of 0.4 °C may appear insignificant, it is crucial to consider the cryotherapy protocol’s purpose: achieving target skin temperature values corresponding to analgesic thresholds. The skin cooling process defines the effectiveness of whole-body cryostimulation (WBC) in achieving localized analgesic thresholds and avoiding undesirable effects [29,30,31,32].
Recent revisions to the 2010 guidelines, issued by the Association of Chartered Physiotherapists in Sports and Exercise Medicine (ACPSEM) and endorsed by the Chartered Society of Physiotherapists (London), emphasize that the recognized threshold for effective local analgesia is reached when the absolute skin temperature is reduced below 13 °C.
The duration of the cryotherapy protocol, the actual temperature inside the cryotherapy chamber, and, as demonstrated by this study, the number of individuals participating simultaneously in a cryotherapy session all influence the therapeutic efficacy of the cryotherapy protocol. Additionally, both thermo-aerodynamic aspects related to whole-body cryostimulation chambers and physiological and anthropometric aspects related to users need to be considered. The optimal benefit of the dose-response ratio is associated with the optimal match between exposure temperature and specific exposure duration for a given category of individuals. The exposure temperature, representing the actual temperature to which the body is exposed, currently poses a challenging variable to determine precisely. Moreover, the present study demonstrates that particular attention should be given to the influence of individuals’ positions in the whole-body cryotherapy chamber, especially regarding the intensity of skin cooling, which is at the core of the therapeutic process. The spatial arrangement of individuals can impact the efficacy of skin cooling by influencing the distribution of cold around their bodies. For instance, the proximity or distance between individuals in the chamber can affect the cold distribution on their body surface. Certain areas of the body may be more exposed to the cold than others based on individuals’ positions and the aerodynamic conditions within the chamber (see Figure 6 and Figure 7). To optimize protocols, it might be advisable for individuals to change positions throughout the cryotherapy session to enhance the kinetics of skin cooling.
Furthermore, the simultaneous presence of multiple subjects in the cryotherapy chamber can lead to a significant increase in the temperature inside the cabin. This rise in the average exposure temperature may compromise the effectiveness of skin cooling, questioning the anticipated therapeutic outcomes of cryotherapy. A more nuanced understanding of the spatial arrangement’s effect on thermal exchanges among individuals could further optimize cryotherapy protocols. This optimization is crucial to ensure maximum therapeutic efficacy and ensure that variations in skin temperature remain consistent with therapeutic goals.
5. Conclusions
The aim of this study was to explore the influence of the number of patients on the thermal and aerodynamic conditions within a whole-body cryotherapy chamber at −92 °C during a 3-minute session. To achieve this, a 3-min cryotherapy session was simulated using computational fluid dynamics (CFD). Drawing from the findings of a preceding study, we assessed the impact of heat transfer between the human body and its surroundings. A comparative analysis was conducted among the outcomes obtained for an empty cryotherapy chamber, a chamber with one patient, and a chamber with three patients. The main findings of this study are as follows:
- The simultaneous presence of multiple patients disrupts thermal homogeneity, resulting in an overall rise in temperature within the enclosure;
- This disruption is associated with the thermal stratification induced by the density disparity between cold and warm air, leading to a convection phenomenon and the formation of a convective thermal boundary layer enveloping the human body;
- The results suggest a temperature difference of approximately 6.7 °C between an empty cryotherapy chamber and one with three patients;
- Based on a mathematical model derived from experimental data, it is estimated that, compared to the reference case, the average skin temperature would be higher by approximately 0.4 °C with three patients;
- This study highlights the importance of patients’ positions in the chamber, influencing the non-uniform distribution of surface thermal flux;
- This variability can lead to noteworthy differences in skin cooling, a critical aspect for achieving recommended analgesic thresholds.
These results underscore the importance of considering these factors to optimize cryotherapy protocols, ensuring maximum therapeutic effectiveness while maintaining consistency in skin temperature variations, aligning with specific therapeutic goals.
The implications of these findings extend to the optimal design of cryotherapy protocols, underscoring the necessity for precise management of temperature and the number of individuals present simultaneously to ensure consistent therapeutic outcomes. In conclusion, this study highlights the need for a holistic approach, taking into account both thermo-aerodynamic aspects and physiological and anthropometric factors related to users. The optimization of cryotherapy protocols should aim to ensure maximum therapeutic effectiveness while maintaining consistency in skin temperature variations, aligning with specific therapeutic goals.
Limitations
It is important to interpret the findings of this study while considering several inherent limitations. Firstly, the numerical model does not incorporate the physiological intricacies of the human body. The interaction between the human body and the chamber predominantly occurs at the skin level, with skin temperature reflecting the intricate interplay between heat dissipation to the environment and heat generation by metabolically active tissues. Additionally, the thermal boundary condition applied to the human body assumes a uniform distribution of surface temperature at time t = 0 whereas, in reality, the thermal response varies across different body segments. Lastly, the model assumes a static patient whereas real-world scenarios involve patient movement, introducing disruptions in the flow field and localized alterations in heat transfers.
Author Contributions
Conceptualization, R.E. and G.P.; methodology, F.B. and F.L.; software, R.E.; validation, B.A., G.P., and B.B.; formal analysis, F.B.; investigation, G.P.; resources, B.B.; data curation, B.A. and F.L.; writing—original draft preparation, F.B.; writing—review and editing, R.E.; visualization, G.P. and F.L.; supervision, B.A.; project administration, B.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Ethical review and approval were waived for this study because this numerical article does not encompass any studies involving real human subjects.
Data Availability Statement
The datasets generated during the current study are available from the first author upon reasonable request.
Conflicts of Interest
Author Bastien Bouchet was employed by the company Cryotera. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Bouzigon, R.; Grappe, F.; Ravier, G.; Dugue, B. Whole- and Partial-Body Cryostimulation/Cryotherapy: Current Technologies and Practical Applications. J. Therm. Biol. 2016, 61, 67–81. [Google Scholar] [CrossRef]
- Westerlund, T.; Oksa, J.; Smolander, J.; Mikkelsson, M. Thermal Responses During and After Whole-Body Cryotherapy (−110 °C). J. Therm. Biol. 2003, 28, 601–608. [Google Scholar] [CrossRef]
- Legrand, F.D.; Dugué, B.; Costello, J.; Bleakley, C.; Miller, E.; Broatch, J.R.; Polidori, G.; Lubkowska, A.; Louis, J.; Lombardi, G.; et al. Evaluating Safety Risks of Whole-Body Cryotherapy/Cryostimulation (WBC): A Scoping Review from an International Consortium. Eur. J. Med. Res. 2023, 28, 387. [Google Scholar] [CrossRef]
- Sadura-Sieklucka, T.; Sołtysiuk, B.; Karlicka, A.; Sokołowska, B.; Kontny, E.; Księżopolska-Orłowska, K. Effects of Whole-Body Cryotherapy in Patients with Rheumatoid Arthritis Considering Immune Parameters. Rheumatology 2019, 57, 320–325. [Google Scholar] [CrossRef]
- Księżopolska-Orłowska, K.; Pacholec, A.; Jędryka-Góral, A.; Bugajska, J.; Sadura-Sieklucka, T.; Kowalik, K.; Pawłowska-Cyprysiak, K.; Łastowiecka-Moras, E. Complex Rehabilitation and the Clinical Condition of Working Rheumatoid Arthritis Patients: Does Cryotherapy Always Overtop Traditional Rehabilitation? Disabil. Rehabil. 2016, 38, 1034–1040. [Google Scholar] [CrossRef]
- Gizińska, M.; Rutkowski, R.; Romanowski, W.; Lewandowski, J.; Straburzyńska-Lupa, A. Effects of Whole-Body Cryotherapy in Comparison with Other Physical Modalities Used with Kinesitherapy in Rheumatoid Arthritis. BioMed. Res. Int. 2015, 2015, e409174. [Google Scholar] [CrossRef]
- Stanek, A.; Cholewka, J.; Gadula, J.; Drzazga, Z.; Sieron, A.; Sieron-Stoltny, K. Can Whole-Body Cryotherapy with Subsequent Kinesiotherapy Procedures in Closed Type Cryogenic Chamber Improve BASDAI, BASFI, and Some Spine Mobility Parameters and Decrease Pain Intensity in Patients with Ankylosing Spondylitis? BioMed. Res. Int. 2015, 2015, e404259. [Google Scholar] [CrossRef] [PubMed]
- Stanek, A.; Cholewka, A.; Wielkoszyński, T.; Romuk, E.; Sieroń, A. Decreased Oxidative Stress in Male Patients with Active Phase Ankylosing Spondylitis Who Underwent Whole-Body Cryotherapy in Closed Cryochamber. Oxid. Med. Cell. Longev. 2018, 2018, e7365490. [Google Scholar] [CrossRef] [PubMed]
- Straburzyńska-Lupa, A.; Kasprzak, M.P.; Romanowski, M.W.; Kwaśniewska, A.; Romanowski, W.; Iskra, M.; Rutkowski, R. The Effect of Whole-Body Cryotherapy at Different Temperatures on Proinflammatory Cytokines, Oxidative Stress Parameters, and Disease Activity in Patients with Ankylosing Spondylitis. Oxid. Med. Cell. Longev. 2018, 2018, e2157496. [Google Scholar] [CrossRef] [PubMed]
- Vitenet, M.; Tubez, F.; Marreiro, A.; Polidori, G.; Taiar, R.; Legrand, F.; Boyer, F. Effect of Whole Body Cryotherapy Interventions on Health-Related Quality of Life in Fibromyalgia Patients: A Randomized Controlled Trial. Complement. Ther. Med. 2018, 36, 6–8. [Google Scholar] [CrossRef] [PubMed]
- Miller, E.; Kostka, J.; Włodarczyk, T.; Dugué, B. Whole-Body Cryostimulation (Cryotherapy) Provides Benefits for Fatigue and Functional Status in Multiple Sclerosis Patients. A Case–Control Study. Acta Neurol. Scand. 2016, 134, 420–426. [Google Scholar] [CrossRef]
- Pournot, H.; Bieuzen, F.; Louis, J.; Fillard, J.-R.; Barbiche, E.; Hausswirth, C. Time-Course of Changes in Inflammatory Response after Whole-Body Cryotherapy Multi Exposures following Severe Exercise. PLoS ONE 2011, 6, e22748. [Google Scholar] [CrossRef]
- Ziemann, E.; Olek, R.A.; Grzywacz, T.; Kaczor, J.J.; Antosiewicz, J.; Skrobot, W.; Kujach, S.; Laskowski, R. Whole-Body Cryostimulation as an Effective Way of Reducing Exercise-Induced Inflammation and Blood Cholesterol in Young Men. Eur. Cytokine Netw. 2014, 25, 14–23. [Google Scholar] [CrossRef]
- Ferreira-Junior, J.B.; Bottaro, M.; Vieira, A.; Siqueira, A.F.; Vieira, C.A.; Durigan, J.L.Q.; Cadore, E.L.; Coelho, L.G.M.; Simões, H.G.; Bemben, M.G. One Session of Partial-Body Cryotherapy (−110 °C) Improves Muscle Damage Recovery. Scand. J. Med. Sci. Sports 2015, 25, e524–e530. [Google Scholar] [CrossRef]
- Rymaszewska, J.; Tulczynski, A.; Zagrobelny, Z.; Kiejna, A.; Hadrys, T. Influence of Whole Body Cryotherapy on Depressive Symptoms—Preliminary Report. Acta Neuropsychiatr. 2003, 15, 122–128. [Google Scholar] [CrossRef][Green Version]
- Rymaszewska, J.; Ramsey, D.; Chładzińska-Kiejna, S. Whole-Body Cryotherapy as Adjunct Treatment of Depressive and Anxiety Disorders. Arch. Immunol. Ther. Exp. 2008, 56, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Douzi, W.; Dupuy, O.; Tanneau, M.; Boucard, G.; Bouzigon, R.; Dugué, B. 3-Min Whole Body Cryotherapy/Cryostimulation after Training in the Evening Improves Sleep Quality in Physically Active Men. Eur. J. Sport Sci. 2019, 19, 860–867. [Google Scholar] [CrossRef] [PubMed]
- Polidori, G.; Elfahem, R.; Abbes, B.; Bogard, F.; Legrand, F.; Bouchet, B.; Beaumont, F. Preliminary Study on the Effect of Sex on Skin Cooling Response During Whole Body Cryostimulation (−110 °C): Modeling and Prediction of Exposure Durations. Cryobiology 2020, 97, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Elfahem, R.; Bouchet, B.; Abbes, B.; Polidori, G.; Beaumont, F. Influence of Body Heat Loss on Temperature and Velocity Fields in a Whole-Body Cryotherapy Chamber. Fluids 2023, 8, 9. [Google Scholar] [CrossRef]
- Elfahem, R.; Abbes, B.; Bouchet, B.; Murer, S.; Bogard, F.; Moussa, T.; Beaumont, F.; Polidori, G. Whole-Body Cryostimulation: New Insights in Thermo-Aeraulic Fields Inside Chambers. Inventions 2023, 8, 4. [Google Scholar] [CrossRef]
- Marreiro, F.; Beaumont, F.; Taïar, R.; Polidori, G. Application des Techniques d’Imagerie Thermique Infrarouge et de Mécanique des Fluides Numérique à la Cryothérapie Corps Entier (CCE). Instrum. Mes. Métrologie 2017, 6, 11–32. [Google Scholar]
- Gagge, A.P.; Gonzalez, R.R. Mechanisms of heat exchange: Biophysics and physiology. In Handbook of Physiology. Section 4: Environmental Physiology; Fregley, M.J., Blatteis, C.M., Eds.; Oxford University Press: New York, NY, USA, 1996; pp. 45–84. [Google Scholar]
- Parsons, K.C. Human Thermal Environments, 2nd ed.; Taylor & Francis: London, UK, 2003. [Google Scholar]
- Craven, B.A.; Settles, G.S. A Computational and Experimental Investigation of the Human Thermal Plume. J. Fluids Eng. 2006, 128, 1251–1258. [Google Scholar] [CrossRef]
- Liu, Y.; Liu, Z.; Luo, J. Numerical Investigation of the Unsteady Thermal Plume Around Human Body in Closed Space. Procedia Eng. 2015, 121, 1919–1926. [Google Scholar] [CrossRef]
- Blokker, T.; Bucher, E.; Steiner, T.; Wehrlin, J.P. Effect of cold ambient temperature on heat flux, skin temperature, and thermal sensation at different body parts in elite biathletes. Front. Sports Act. Living 2022, 4, 966203. [Google Scholar] [CrossRef] [PubMed]
- Kenny, G.P.; Flouris, A.D. The human thermoregulatory system and its response to thermal stress. In Protective Clothing; Wang, F., Gao, C., Eds.; Woodhead Publishing Series in Textiles; Woodhead Publishing: Sawston, UK, 2014; pp. 319–365. [Google Scholar]
- Burkov, I.A.; Kolishkin, L.M.; Pushkarev, A.V.; Shakurov, A.V.; Tsiganov, D.I.; Zherdev, A.A. Experimental and computational thermal analysis of partial-body cryotherapy. Int. J. Heat Mass Transf. Part C 2022, 183, 122194. [Google Scholar] [CrossRef]
- Costello, J.T.; McInerney, C.D.; Bleakley, C.M.; Selfe, J.; Donnelly, A.E. The Use of Thermal Imaging in Assessing Skin Temperature Following Cryotherapy: A Review. J. Therm. Biol. 2012, 37, 103–110. [Google Scholar] [CrossRef]
- Mourot, L.; Cluzeau, C.; Regnard, J. Hyperbaric gaseous cryotherapy: Effects on skin temperature and systemic vasoconstriction. Arch. Phys. Med. Rehabil. 2007, 88, 1339–1343. [Google Scholar] [CrossRef]
- Cholewka, A.; Stanek, A.; Sieroń; A; Drzazga, Z. Thermography study of skin response due to whole-body cryotherapy. Skin Res. Technol. 2012, 18, 180–187. [Google Scholar] [CrossRef]
- Bleakley, C.M.; Hopkins, J.T. Is it possible to achieve optimal levels of tissue cooling in cryotherapy? Phys. Ther. Rev. 2010, 15, 344–350. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).