Effects of Printing Angle and Post-Curing Time on the Color and Translucency of 3D-Printed Temporary Restoration
Abstract
1. Introduction
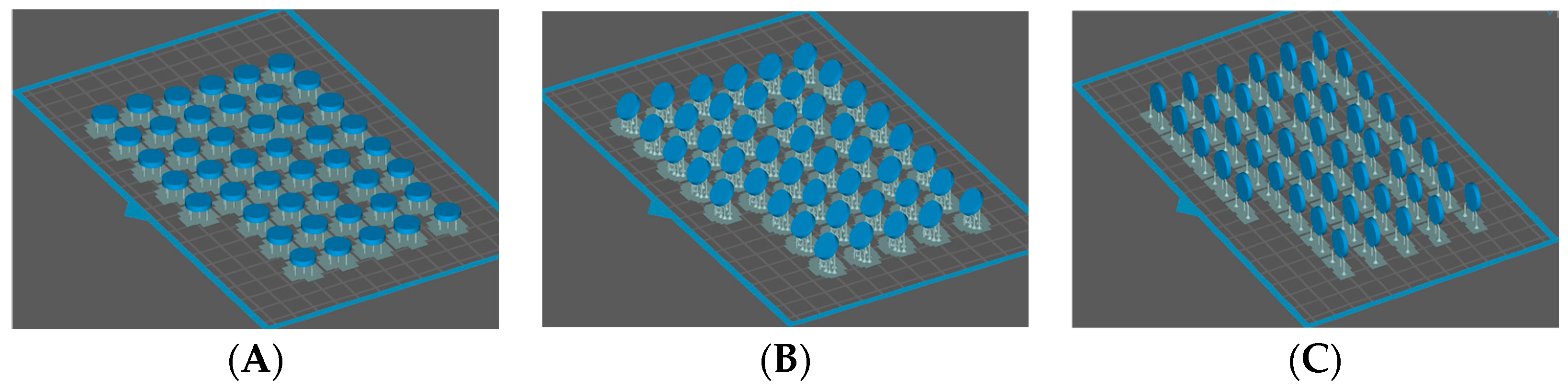
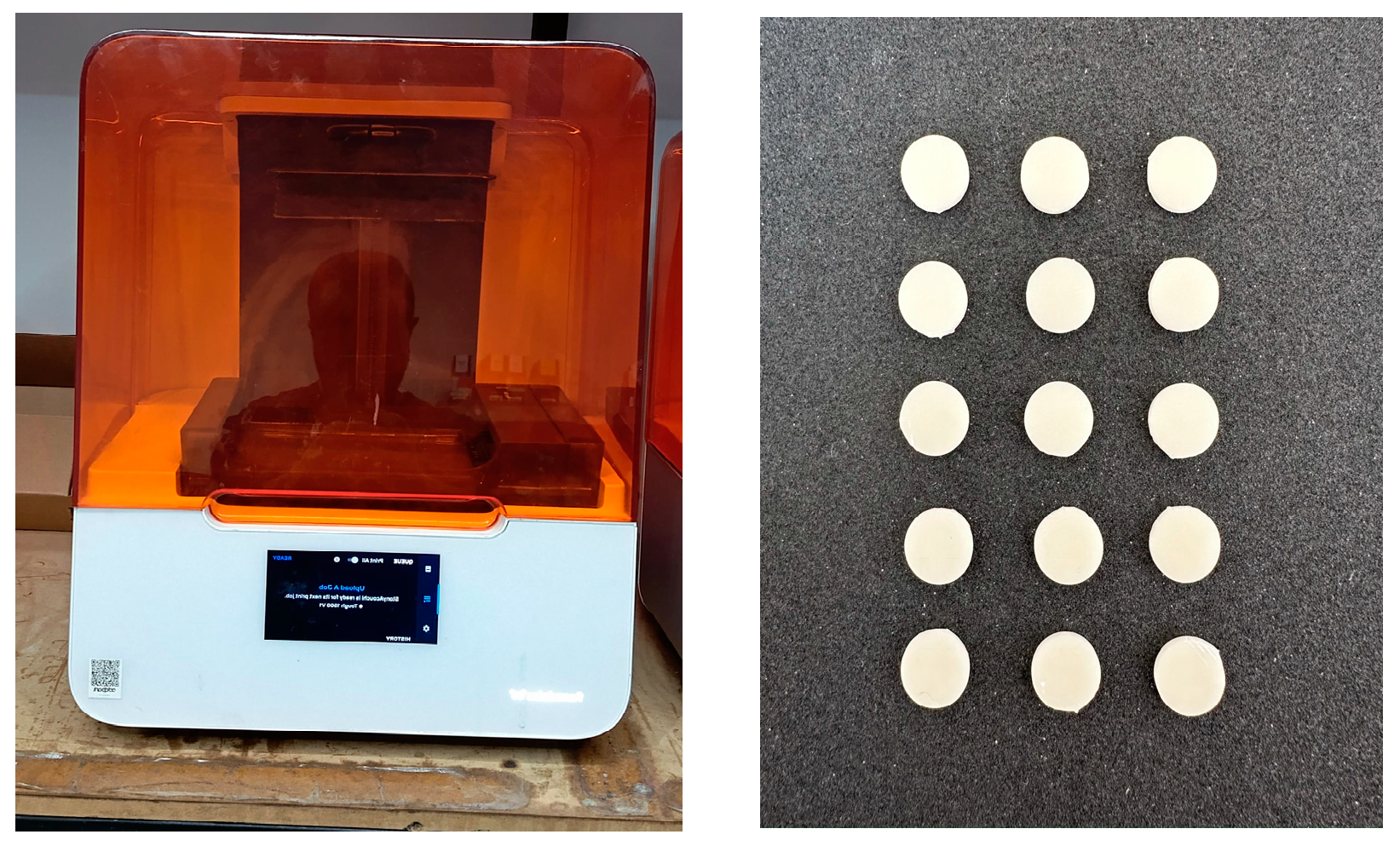
2. Materials and Methods
2.1. Color Measurement
2.2. Translucency Measurement
2.3. Statistical Analysis
3. Results
3.1. Color Change Results
3.2. Translucency Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Song, S.Y.; Shin, Y.H.; Lee, J.Y.; Shin, S.W. Color stability of provisional restorative materials with different fabrication methods. J. Adv. Prosthodont. 2020, 12, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Abdulmohsen, B.; Parker, S.; Braden, M.; Patel, M.P. A study to investigate and compare the physicomechanical properties of experimental and commercial temporary crown and bridge materials. Dent. Mater. 2016, 32, 200–210. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R.; Wismeijer, D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J. Prosthet. Dent. 2016, 115, 760–767. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.W.; Kim, J.E.; Choi, Y.J.; Shin, S.H.; Nam, N.E.; Shim, J.S.; Lee, K.W. Evaluation of the color stability of 3D-printed crown and bridge materials against various sources of discoloration: An in vitro study. Materials 2020, 13, 5359. [Google Scholar] [CrossRef] [PubMed]
- Stansbury, J.W.; Idacavage, M.J. 3D printing with polymers: Challenges among expanding options and opportunities. Dent. Mater. 2016, 32, 54–64. [Google Scholar] [CrossRef]
- Bellocchio, A.M.; Ciancio, E.; Ciraolo, L.; Barbera, S.; Nucera, R. Three-Dimensional Printed Attachments: Analysis of Reproduction Accuracy Compared to Traditional Attachments. Appl. Sci. 2024, 14, 3837. [Google Scholar] [CrossRef]
- Baytur, S.; Diken Turksayar, A.A. Effects of post-polymerization conditions on color properties, surface roughness, and flexural strength of 3D-printed permanent resin material after thermal aging. J. Prosthodont. 2024, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Della Bona, A.; Cantelli, V.; Britto, V.T.; Collares, K.F.; Stansbury, J.W. 3D printing restorative materials using a stereolithographic technique: A systematic review. Dent. Mater. 2021, 37, 336–350. [Google Scholar] [CrossRef]
- Della Bona, A. Color and Appearance in Dentistry, 1st ed.; Springer: Cham, Switzerland, 2020. [Google Scholar]
- Espinar, C.; Della Bona, A.; Pérez, M.M.; Pulgar, R. Color and optical properties of 3D printing restorative polymer-based materials: A scoping review. J. Esthet. Restor. Dent. 2022, 34, 853–864. [Google Scholar] [CrossRef]
- Kim, D.; Shim, J.S.; Lee, D.; Shin, S.H.; Nam, N.E.; Park, K.H.; Kim, J.E. Effects of post-curing time on the mechanical and color properties of three-dimensional printed crown and bridge materials. Polymers 2020, 12, 2762. [Google Scholar] [CrossRef]
- Chang, J.; Choi, Y.; Moon, W.; Chung, S.H. Impact of postpolymerization devices and locations on the color, translucency, and mechanical properties of 3D-printed interim resin materials. J. Prosthet. Dent. 2022, in press. [Google Scholar] [CrossRef] [PubMed]
- Revilla-Leon, M.; Ozcan, M. Additive manufacturing technologies used for processing polymers: Current status and potential application in prosthetic dentistry. J. Prosthodont. 2019, 28, 146–158. [Google Scholar] [CrossRef] [PubMed]
- Schweiger, J.; Edelhoff, D.; Guth, J.F. 3D printing in digital prosthetic dentistry: An overview of recent developments in additive manufacturing. J. Clin. Med. 2021, 10, 2010. [Google Scholar] [CrossRef] [PubMed]
- Puebla, K.; Arcaute, K.; Quintana, R.; Wicker, R.B. Effects of environmental conditions, aging, and build orientations on the mechanical properties of ASTM type I specimens manufactured via stereolithography. Rapid Prototyp. J. 2012, 18, 374–388. [Google Scholar] [CrossRef]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef]
- Zhang, Z.C.; Li, P.L.; Chu, F.T.; Shen, G. Influence of the three-dimensional printing technique and printing layer thickness on model accuracy. J. Orofac. Orthop. Fortschr. Kieferorthop. 2019, 80, 194–204. [Google Scholar] [CrossRef] [PubMed]
- Dimitrov, D.; Schreve, K.; De Beer, N. Advances in three dimensional printing—State of the art and future perspectives. Rapid Prototyp. J. 2006, 12, 136–147. [Google Scholar] [CrossRef]
- Coon, C.; Pretzel, B.; Lomax, T.; Strlič, M. Preserving rapid prototypes: A review. Herit. Sci. 2016, 4, 40. [Google Scholar] [CrossRef]
- Winter, R. Visualizing the natural dentition. J. Esthet. Dent. 1993, 5, 102–117. [Google Scholar] [CrossRef]
- Johnston, W.M.; Ma, T.; Kienle, B.H. Translucency parameter of colorants for maxillofacial prostheses. Int. J. Prosthodont. 1995, 8, 79–86. [Google Scholar]
- Lee, Y.K. Influence of scattering/absorption characteristics on the color of resin composites. Dent. Mater. 2007, 23, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Umorin, M.; Özcan, M.; Piedra-Cascón, W. Color dimensions of additive manufactured interim restorative dental material. J. Prosthet. Dent. 2020, 123, 754–760. [Google Scholar] [CrossRef] [PubMed]
- Revilla-león, M.; Morillo, J.A.; Att, W.; Özcan, M. Chemical composition, knoop hardness, surface roughness, and adhesion aspects of additively manufactured dental interim materials. J. Prosthodont. 2021, 30, 698–705. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Meyers, M.J.; Zandinejad, A.; Özcan, M. A review on chemical composition, mechanical properties, and manufacturing work flow of additively manufactured current polymers for interim dental restorations. J. Esthet. Restor. Dent. 2019, 31, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Kessler, A.; Hickel, R.; Reymus, M. 3D printing in dentistry-state of the art. Oper. Dent. 2020, 45, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Pfeifer, C.S. Polymer-based direct filling materials. Dent. Clin. North. Am. 2017, 61, 733–750. [Google Scholar] [CrossRef]
- Fronza, B.M.; Ayres, A.P.A.; Pacheco, R.R.; Rueggeberg, F.A.; Dias, C.T.D.S.; Giannini, M. Characterization of inorganic filler content, mechanical properties, and light transmission of bulk-fill resin composites. Oper. Dent. 2017, 42, 445–455. [Google Scholar] [CrossRef] [PubMed]
- Fronza, B.M.; Rueggeberg, F.A.; Braga, R.R.; Mogilevych, B.; Soares, L.E.S.; Martin, A.A.A.; Giannini, M. Monomer conversion, microhardness, internal marginal adaptation, and shrinkage stress of bulk- fill resin composites. Dent. Mater. 2015, 31, 1542–1551. [Google Scholar] [CrossRef] [PubMed]
- Kang, X.; Liu, S.; Dai, Z.; He, Y.; Song, X.; Tan, Z. Titanium dioxide: From engineering to applications. Catalysts 2019, 9, 191. [Google Scholar] [CrossRef]
- Albuquerque, P.P.A.C.; Moreira, A.D.L.; Moraes, R.R.; Schneider, L.F.J.; Cavalcante, L.M. Color stability, conversion, water sorption and solubility of dental composites formulated with different photoinitiator systems. J. Dent. 2013, 41, 67–72. [Google Scholar] [CrossRef]
- Revilla-León, M.; Jordan, D.; Methani, M.M.; Piedra-Cascón, W.; Özcan, M.; Zandinejad, A. Influence of printing angulation on the surface roughness of additive manufactured clear silicone indices: An in vitro study. J. Prosthet. Dent. 2021, 125, 462–468. [Google Scholar] [CrossRef] [PubMed]
- Reymus, M.; Fabritius, R.; Keßler, A.; Hickel, R.; Edelhoff, D.; Stawarczyk, B. Fracture load of 3D-printed fixed dental prostheses compared with milled and conventionally fabricated ones: The impact of resin material, build direction, post-curing, and artificial aging—An in vitro study. Clin. Oral. Investig. 2020, 24, 701–710. [Google Scholar] [CrossRef]
- Mayer, J.; Reymus, M.; Wiedenmann, F.; Edelhoff, D.; Hickel, R.; Stawarczyk, B. Temporary 3D printed fixed dental prosthesis materials: Impact of post printing cleaning methods on degree of conversion as well as surface and mechanical properties. Int. J. Prosthodont. 2021, 34, 1–29. [Google Scholar] [CrossRef] [PubMed]
- Mayer, J.; Stawarczyk, B.; Vogt, K.; Hickel, R.; Edelhoff, D.; Reymus, M. Influence of cleaning methods after 3D printing on two- body wear and fracture load of resin-based temporary crown and bridge material. Clin. Oral. Investig. 2021, 25, 5987–5996. [Google Scholar] [CrossRef] [PubMed]
- Perea-Lowery, L.; Gibreel, M.; Vallittu, P.K.; Lassila, L. Evaluation of the mechanical properties and degree of conversion of 3D printed splint material. J. Mech. Behav. Biomed. Mater. 2021, 115, 104254. [Google Scholar] [CrossRef] [PubMed]
- Reymus, M.; Stawarczyk, B. In vitro study on the influence of postpolymerization and aging on the Martens parameters of 3D-printed occlusal devices. J. Prosthet. Dent. 2020, 125, 817–823. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.E.; Choi, W.H.; Lee, D.; Shin, Y.; Park, S.H.; Roh, B.D.; Kim, D. Color and translucency stability of three-dimensional printable dental materials for crown and bridge restorations. Materials 2021, 14, 650. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, N.; Alharbi, A.; Osman, R. Stain susceptibility of 3D-printed nanohybrid composite restorative material and the efficacy of different stain removal techni- ques: An in vitro study. Materials 2021, 14, 5621. [Google Scholar] [CrossRef] [PubMed]
- Almejrad, L.; Yang, C.C.; Morton, D.; Lin, W.S. The effects of beverages and surface treatments on the color stability of 3D-printed interim restorations. J. Prosthodont. 2022, 31, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.H.; Ahn, J.S.; Lim, Y.J.; Kwon, H.B.; Kim, M.J. Effect of post-curing time on the color stability and related properties of a tooth-colored 3D-printed resin material. J. Mech. Behav. Biomed. Mater. 2022, 126, 104993. [Google Scholar] [CrossRef]
- Soto-Montero, J.; de Castro, E.F.; Romano, B.C.; Nima, G.; Shimokawa, C.A.K.; Giannini, M. Color alterations, flexural strength, and microhardness of 3D printed resins for fixed provisional restoration using different post-curing times. Dent. Mater. 2022, 38, 1271–1282. [Google Scholar] [CrossRef]
- Espinar, C.; Della Bona, A.; Pérez, M.M.; Tejada-Casado, M.; Pulgar, R. The influence of printing angle on color and translucency of 3D printed resins for dental restorations. Dent. Mater. 2023, 39, 410–417. [Google Scholar] [CrossRef]
- Salas, M.; Lucena, C.; Herrera, L.J.; Yebra, A.; Della Bona, A.; Perez, M.M. Translucency thresholds for dental materials. Dent. Mater. 2018, 34, 1168–1174. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.H.; Ahn, J.S.; Lim, Y.J.; Kwon, H.B.; Kim, M.J. Effect of layer thickness and printing orientation on the color stability and stainability of a 3D-printed resin material. J. Prosthet. Dent. 2022, 127, 784.e1–784.e7. [Google Scholar] [CrossRef] [PubMed]
- de Castro, E.F.; Nima, G.; Rueggeberg, F.A.; Araújo-Neto, V.G.; Faraoni, J.J.; Palma-Dibb, R.G.; Giannini, M. Effect of build orientation in gloss, roughness and color of 3D-printed resins for provisional indirect restorations. Dent. Mater. 2023, 39, e1–e11. [Google Scholar] [CrossRef]
- Espinar, C.; Della Bona, A.; Tejada-Casado, M.; Pulgar, R.; Pérez, M.M. Optical behavior of 3D-printed dental restorative resins: Influence of thickness and printing angle. Dent. Mater. 2023, 39, 894–902. [Google Scholar] [CrossRef] [PubMed]
- Terry, D.A.; Geller, W.; Tric, O.; Anderson, M.J.; Tourville, M.; Kobashigawa, A. Anatomical form defines color: Function, form, and aesthetics. Pract. Proced. Aesthet. Dent. 2002, 14, 59–67. [Google Scholar] [PubMed]
- Pecho, O.E.; Ghinea, R.; do Amaral, E.A.; Cardona, J.C.; Della Bona, A.; Pérez, M.M. Relevant optical properties for direct restorative materials. Dent. Mater. 2016, 32, e105–e112. [Google Scholar] [CrossRef] [PubMed]
- Perez, M.M.; Hita-Iglesias, C.; Ghinea, R.; Yebra, A.; Pecho, O.E.; Ionescu, A.M.; Hita, E. Optical properties of supra-nano spherical filled resin composites compared to nanofilled, nano-hybrid and micro-hybrid composites. Dent. Mater. J. 2016, 35, 353–359. [Google Scholar] [CrossRef]
- Arikawa, H.; Kanie, T.; Fujii, K.; Takahashi, H.; Ban, S. Effect of filler properties in composite resins on light transmittance characteristics and color. Dent. Mater. J. 2007, 26, 38–44. [Google Scholar] [CrossRef]
- Kolb, C.; Gumpert, K.; Wolter, H.; Sextl, G. Highly translucent dental resin composites through refractive index adaption using zirconium dioxide nanoparticles and organic functionalization. Dent. Mater. 2020, 36, 1332–1342. [Google Scholar] [CrossRef] [PubMed]
- Hébert, M.; Hersch, R.D.; Becker, J.M. Compositional reflectance and transmittance model for multilayer specimens. JOSA A 2007, 24, 2628–2644. [Google Scholar] [CrossRef] [PubMed]
- Unkovskiy, A.; Bui, P.H.; Schille, C.; Geis-Gerstorfer, J.; Huettig, F.; Spintzyk, S. Objects build orientation, positioning, and curing influence dimensional accuracy and flexural properties of stereolithographically printed resin. Dent. Mater. 2018, 34, e324–e333. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.H.; Lin, Y.M.; Lai, Y.L.; Lee, S.Y. Mechanical properties, accuracy, and cytotoxicity of UV-polymerized 3D printing resins composed of Bis-EMA, UDMA, and TEGDMA. J. Prosthet. Dent. 2020, 123, 349–354. [Google Scholar] [CrossRef] [PubMed]
- Bayarsaikhan, E.; Lim, J.H.; Shin, S.H.; Park, K.H.; Park, Y.B.; Lee, J.H.; Kim, J.E. Effects of Postcuring Temperature on the Mechanical Properties and Biocompatibility of Three-Dimensional Printed Dental Resin Material. Polymers 2021, 13, 1180. [Google Scholar] [CrossRef] [PubMed]
- dos Santos, R.L.; de Sampaio, G.A.; de Carvalho, F.G.; Pithon, M.M.; Guenes, G.M.; Alves, P.M. Influence of degree of conversion on the biocompatibility of different composites in vivo. J. Adhes. Dent. 2014, 16, 15–20. [Google Scholar] [PubMed]
- Andrady, A.L.; Heikkilä, A.M.; Pandey, K.K.; Bruckman, L.S.; White, C.C.; Zhu, M.; Zhu, L. Effects of UV radiation on natural and synthetic materials. Photochem. Photobiol. Sci. 2023, 22, 1177–1202. [Google Scholar] [CrossRef] [PubMed]
- Ng, W.L.; Lee, J.M.; Zhou, M.; Chen, Y.W.; Lee, K.X.A.; Yeong, W.Y.; Shen, Y.F. Vat polymerization-based bioprinting—Process, materials, applications and regulatory challenges. Biofabrication 2020, 12, 022001. [Google Scholar] [CrossRef]
- Shin, D.H.; Rawls, H.R. Degree of conversion and color stability of the light curing resin with new photoinitiator systems. Dent. Mater. 2009, 25, 1030–1038. [Google Scholar] [CrossRef]
- Galindo, D.; Soltys, J.L.; Graser, G.N. Long-term reinforced fixed provisional restorations. J. Prosthet. Dent. 1998, 79, 698–701. [Google Scholar] [CrossRef]
- Hadis, M.; Shortall, A.C.; Palin, W. Competitive light absorbers in photoactive dental resin-based materials. Dent. Mater. 2012, 28, 831–841. [Google Scholar] [CrossRef] [PubMed]
- Rubayo, D.D.; Phasuk, K.; Vickery, J.M.; Morton, D.; Lin, W.S. Influences of build angle on the accuracy, printing time, and material consumption of additively manufactured surgical templates. J. Prosthet. Dent. 2021, 126, 658–663. [Google Scholar] [CrossRef] [PubMed]
- Reymus, M.; Stawarczyk, B. Influence of Different Postpolymerization Strategies and Artificial Aging on Hardness of 3D-Printed Resin Materials: An In Vitro Study. Int. J. Prosthodont. 2020, 33, 634–640. [Google Scholar] [CrossRef] [PubMed]
- Scherer, M.D.; Barmak, B.A.; Özcan, M.; Revilla-León, M. Influence of post- polymerization methods and artificial aging procedures on the fracture resistance and flexural strength of a vat-polymerized interim dental material. J. Prosthet. Dent. 2022, 128, 1085–1093. [Google Scholar] [CrossRef]
- Katheng, A.; Kanazawa, M.; Iwaki, M.; Arakida, T.; Hada, T.; Minakuchi, S. Evaluation of trueness and precision of stereolithography-fabricated photo-polymer-resin dentures under different postpolymerization conditions: An in vitro study. J. Prosthet. Dent. 2022, 128, 514–520. [Google Scholar] [CrossRef]

| Printing Angle | Post-Curing Times between Which ΔE Was Measured | Mean | Std. Deviation | N |
|---|---|---|---|---|
| 0° | 20–40 min | 2.2200 | 1.10342 | 15 |
| 20–60 min | 1.5800 | 0.87820 | 15 | |
| 40–60 min | 1.5387 | 1.52961 | 15 | |
| 45° | 20–40 min | 2.1960 | 1.55907 | 15 |
| 20–60 min | 1.4833 | 0.83184 | 15 | |
| 40–60 min | 1.9347 | 1.45855 | 15 | |
| 90° | 20–40 min | 3.2693 | 1.28991 | 15 |
| 20–60 min | 2.1320 | 1.37863 | 15 | |
| 40–60 min | 2.3033 | 1.18075 | 15 |
| Post-Curing Time | Angles between Which ΔE Was Measured | Mean | Std. Deviation | N |
|---|---|---|---|---|
| 20 min | 0°–45° | 1.9747 | 1.03028 | 15 |
| 45°–90° | 1.9473 | 1.04465 | 15 | |
| 0°–90° | 1.6567 | 1.03923 | 15 | |
| 40 min | 0°–45° | 2.1447 | 1.72213 | 15 |
| 45°–90° | 2.3313 | 2.10046 | 15 | |
| 0°–90° | 1.7067 | 1.08973 | 15 | |
| 60 min | 0°–45° | 1.1847 | 0.81700 | 15 |
| 45°–90° | 2.1073 | 1.27027 | 15 | |
| 0°–90° | 1.9873 | 1.32617 | 15 |
| (I) Curing Times at Which ΔE Was Measured | (J) Curing Times at Which ΔE Was Measured | Mean Difference (I–J) | Std. Error | Sig. | 95% Confidence Interval | |
|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||
| 20–40 min | 40–60 min | 0.6362 * | 0.26793 | 0.050 | 0.0008 | 1.2717 |
| 20–60 min | 20–40 min | −0.8300 * | 0.26793 | 0.007 | −1.4655 | −0.1945 |
| 40–60 min | 20–60 min | 0.1938 | 0.26793 | 0.750 | −0.4417 | 0.8292 |
| (I) Printing Angles at Which ΔE Was Measured | (J) Printing Angles at Which ΔE Was Measured | |||||
| 0°–45° | 45°–90° | −0.3607 | 0.27966 | 0.404 | −1.0240 | 0.3026 |
| 45°–90° | 0°–90° | 0.3451 | 0.27966 | 0.435 | −0.3182 | 1.0084 |
| 0°–90° | 0°–45° | 0.0156 | 0.27966 | 0.998 | −0.6477 | 0.6788 |
| Printing Angle | Post-Curing Time | Mean | Standard Deviation | n |
|---|---|---|---|---|
| 0° | 20 min | 4.8833 | 0.46449 | 15 |
| 40 min | 4.5400 | 0.45902 | 15 | |
| 60 min | 4.8107 | 0.48075 | 15 | |
| 45° | 20 min | 5.6767 | 0.41636 | 15 |
| 40 min | 5.4513 | 0.49666 | 15 | |
| 60 min | 5.3847 | 0.28168 | 15 | |
| 90° | 20 min | 5.8767 | 0.49928 | 15 |
| 40 min | 5.1613 | 0.52565 | 15 | |
| 60 min | 5.4973 | 0.37167 | 15 |
| (I) Post-Cure Time | (J) Post-Cure Time | Mean Difference (I–J) | Std. Error | Sig. | 95% Confidence Interval | |
|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||
| 20 min | 40 min | 0.4280 * | 0.09482 | 0.000 | 0.2031 | 0.6529 |
| 40 min | 60 min | −0.1800 | 0.09482 | 0.143 | −0.4049 | 0.0449 |
| 60 min | 20 min | −0.2480 * | 0.09482 | 0.027 | −0.4729 | −0.0231 |
| (I) Printing Angle | (J) Printing Angle | |||||
| 0° | 45° | −0.7596 * | 0.09482 | 0.000 | −0.9844 | −0.5347 |
| 45° | 90° | −0.0076 | 0.09482 | 0.997 | −0.2324 | 0.2173 |
| 90° | 0° | 0.7671 * | 0.09482 | 0.000 | 0.5422 | 0.9920 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Temizci, T.; Kölüş, T. Effects of Printing Angle and Post-Curing Time on the Color and Translucency of 3D-Printed Temporary Restoration. Biomimetics 2024, 9, 420. https://doi.org/10.3390/biomimetics9070420
Temizci T, Kölüş T. Effects of Printing Angle and Post-Curing Time on the Color and Translucency of 3D-Printed Temporary Restoration. Biomimetics. 2024; 9(7):420. https://doi.org/10.3390/biomimetics9070420
Chicago/Turabian StyleTemizci, Tuğba, and Türkay Kölüş. 2024. "Effects of Printing Angle and Post-Curing Time on the Color and Translucency of 3D-Printed Temporary Restoration" Biomimetics 9, no. 7: 420. https://doi.org/10.3390/biomimetics9070420
APA StyleTemizci, T., & Kölüş, T. (2024). Effects of Printing Angle and Post-Curing Time on the Color and Translucency of 3D-Printed Temporary Restoration. Biomimetics, 9(7), 420. https://doi.org/10.3390/biomimetics9070420





