Smart Nursing Wheelchairs: A New Trend in Assisted Care and the Future of Multifunctional Integration
Abstract
:1. Introduction
2. Analysis of the Current Status of Nursing Wheelchair Research
- Publication Date: Only studies published within the last five years were considered to ensure the timeliness and relevance of the technological information.
- Publication Type: Research published in peer-reviewed journals was selected to ensure the scientific integrity and authority of the referenced information.
- Relevance of Content: The literature must provide detailed descriptions of the technological applications or research development processes of nursing wheelchairs.
- Exclusion of conference abstracts and non-peer-reviewed literature, as these sources typically lack rigorous scientific validation.
- Studies not directly related to smart nursing wheelchair technologies were excluded to maintain the focus and accuracy of the research.
- Research published more than five years ago was excluded, unless it had significant historical impact on current technologies.
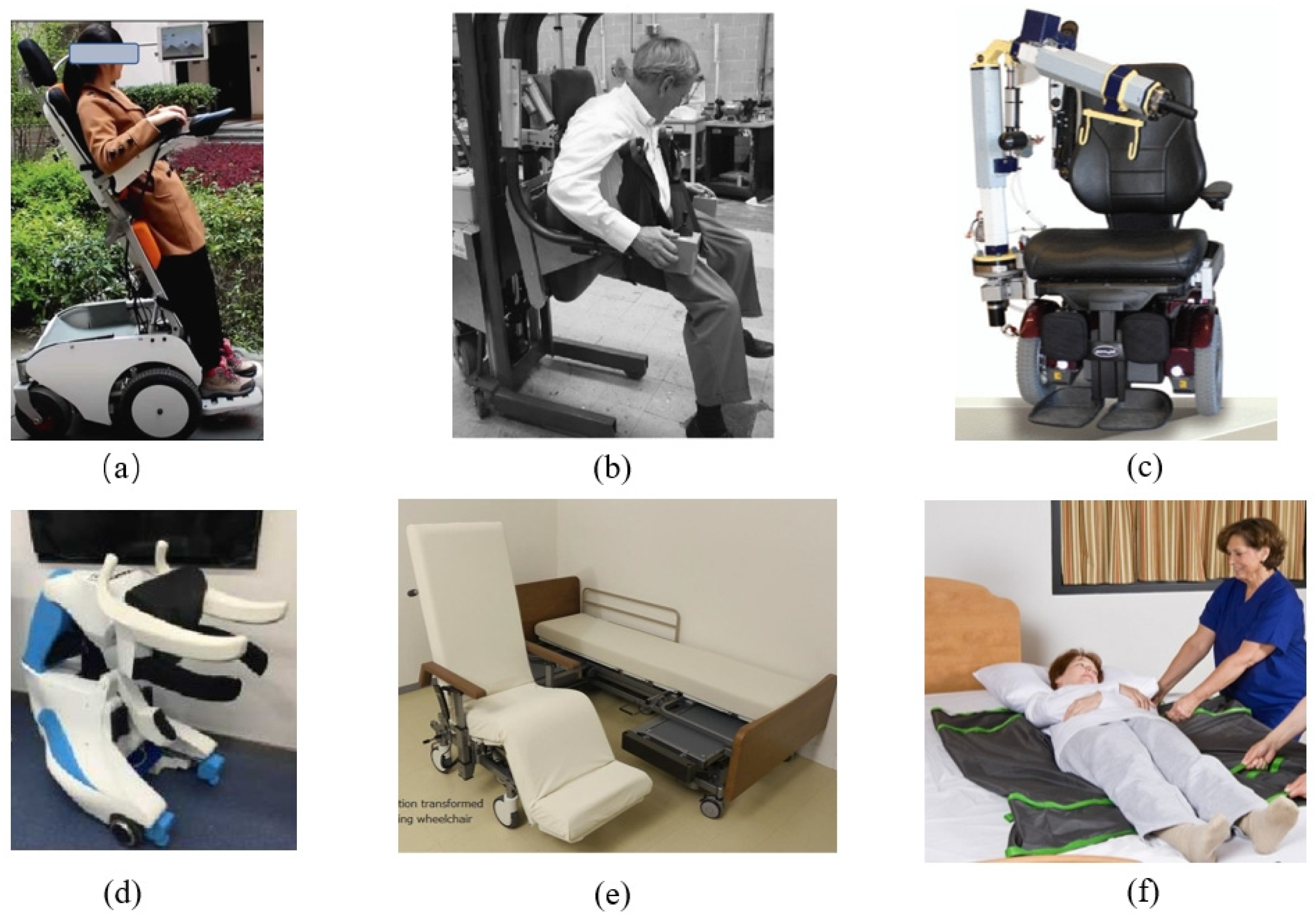
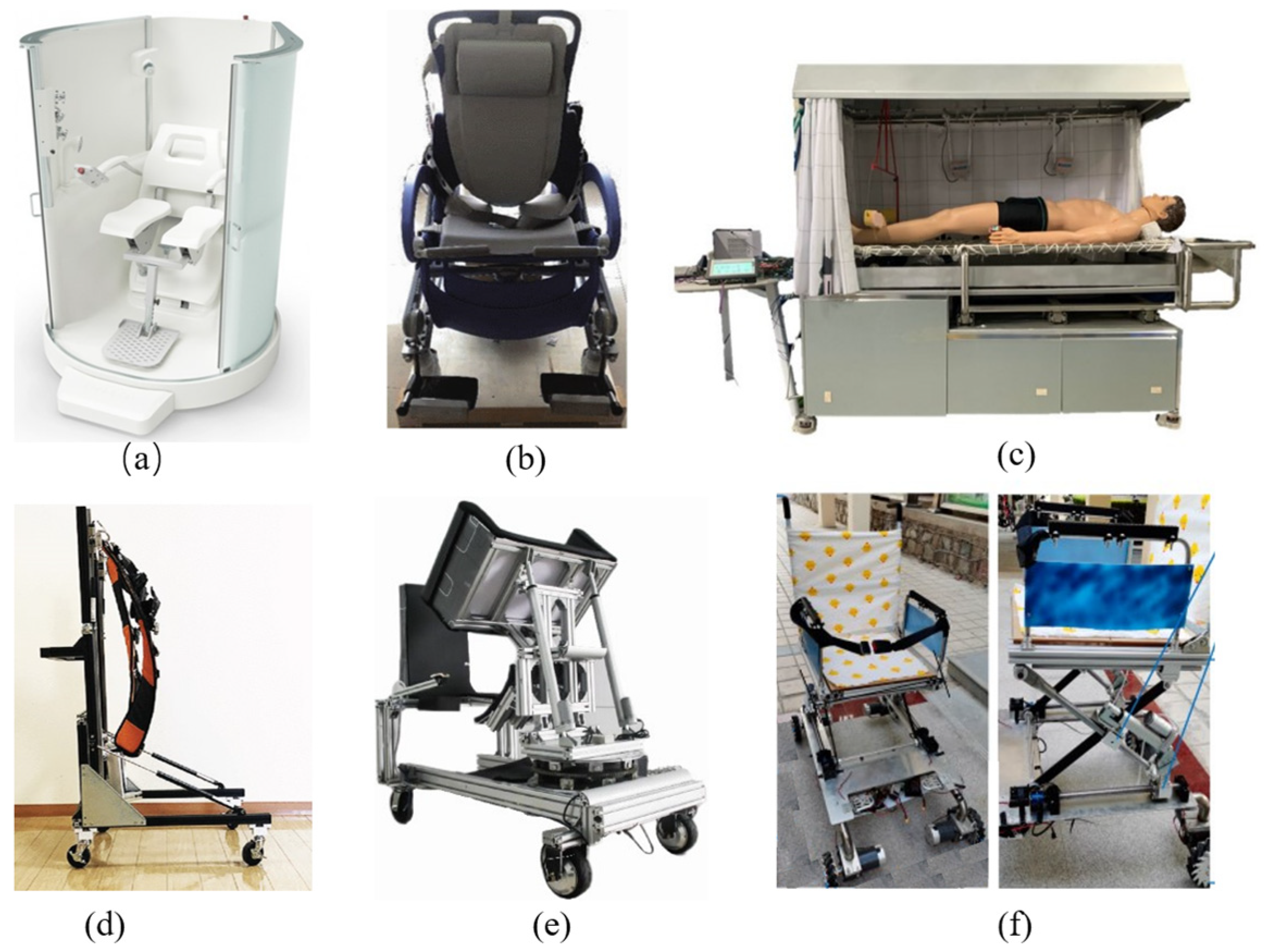
2.1. Supportive Care Functions
- Limited Nursing Functions: Most nursing devices are designed to address specific nursing needs, necessitating the transfer of elderly individuals between devices when faced with different care requirements. This increases potential safety risks during the transfer process.
- Bulky Size: Home nursing devices often have a large footprint, requiring substantial operating space, which poses high spatial demands on home environments and limits the adaptability of the equipment.
- Space Modification Requirements: The use of nursing equipment often demands significant modifications to the user’s living space, resulting in additional costs for the user.
- Limited Maneuverability: The majority of electric nursing devices employ differential drive systems for chassis movement, leading to a large turning radius during mobility. This is not conducive to navigating through narrow indoor environments.
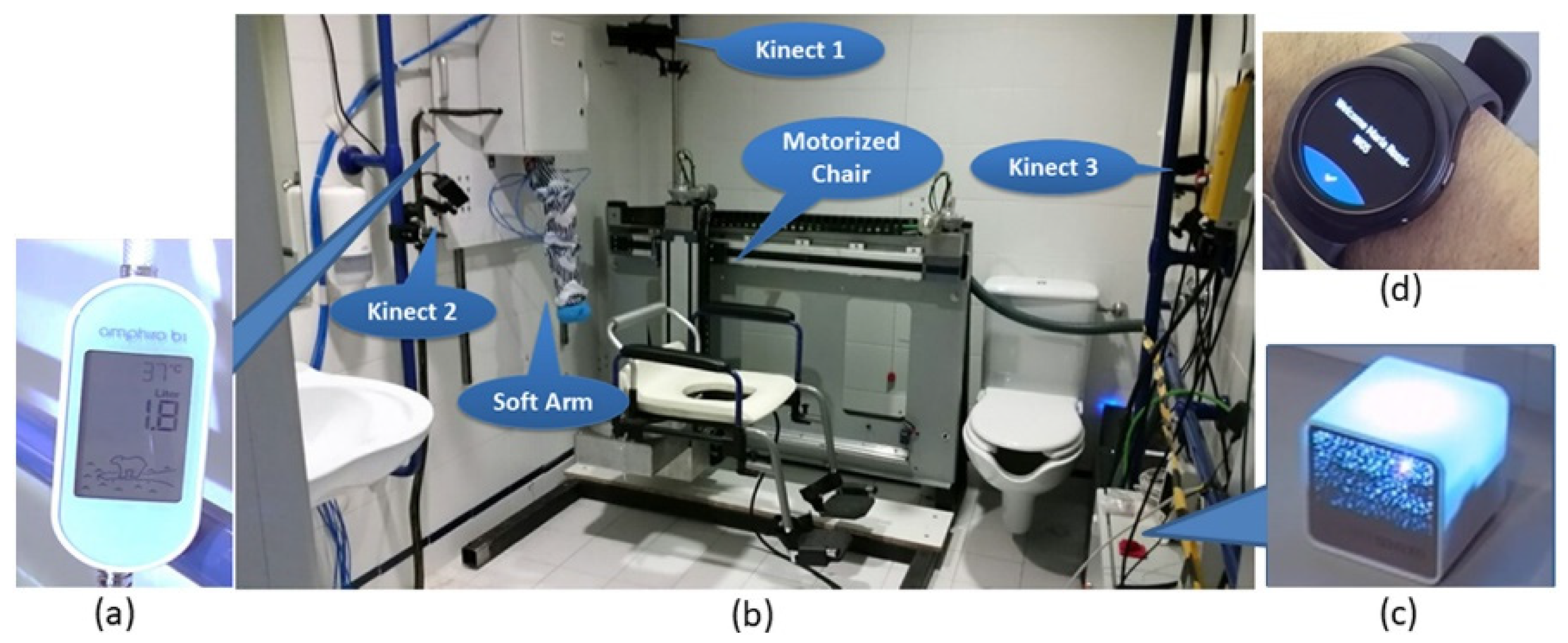
2.2. Multiple Sensor Fusion Technology
- Simulation Testing: Simulated environments are created to test the initial functionality and performance of the sensor fusion algorithms.
- Field Testing: Real-world environments are used to test the nursing wheelchairs in practical scenarios, evaluating their ability to navigate and avoid obstacles.
- User Trials: Trials with actual users, including healthcare professionals and patients, are conducted to gather feedback on usability and effectiveness.
- Performance Metrics: Metrics such as accuracy, response time, and reliability are measured to ensure the technology meets the required standards.
- The environmental awareness capabilities of nursing wheelchairs are relatively limited in terms of intelligent navigation, making it difficult to accurately detect obstacles and the terrain in crowded indoor environments.
- Traditional care wheelchairs lack autonomy, often requiring manual control in common care scenarios such as bedside chair docking and toileting, resulting in inconvenience for both patients and caregivers.
- Future improvements in nursing wheelchairs should include the integration of advanced sensing technologies such as laser radar, cameras, and ultrasonic sensors to improve environmental awareness and improve the accuracy of obstacle detection. In addition, the development of smarter navigation and positioning algorithms should be promoted to give nursing wheelchairs more autonomy and navigation capabilities. This, in turn, would better support nurses in carrying out their nursing tasks, reduce nurses’ workload, and provide better nursing services to patients.
2.3. Human–Machine Interaction Functions
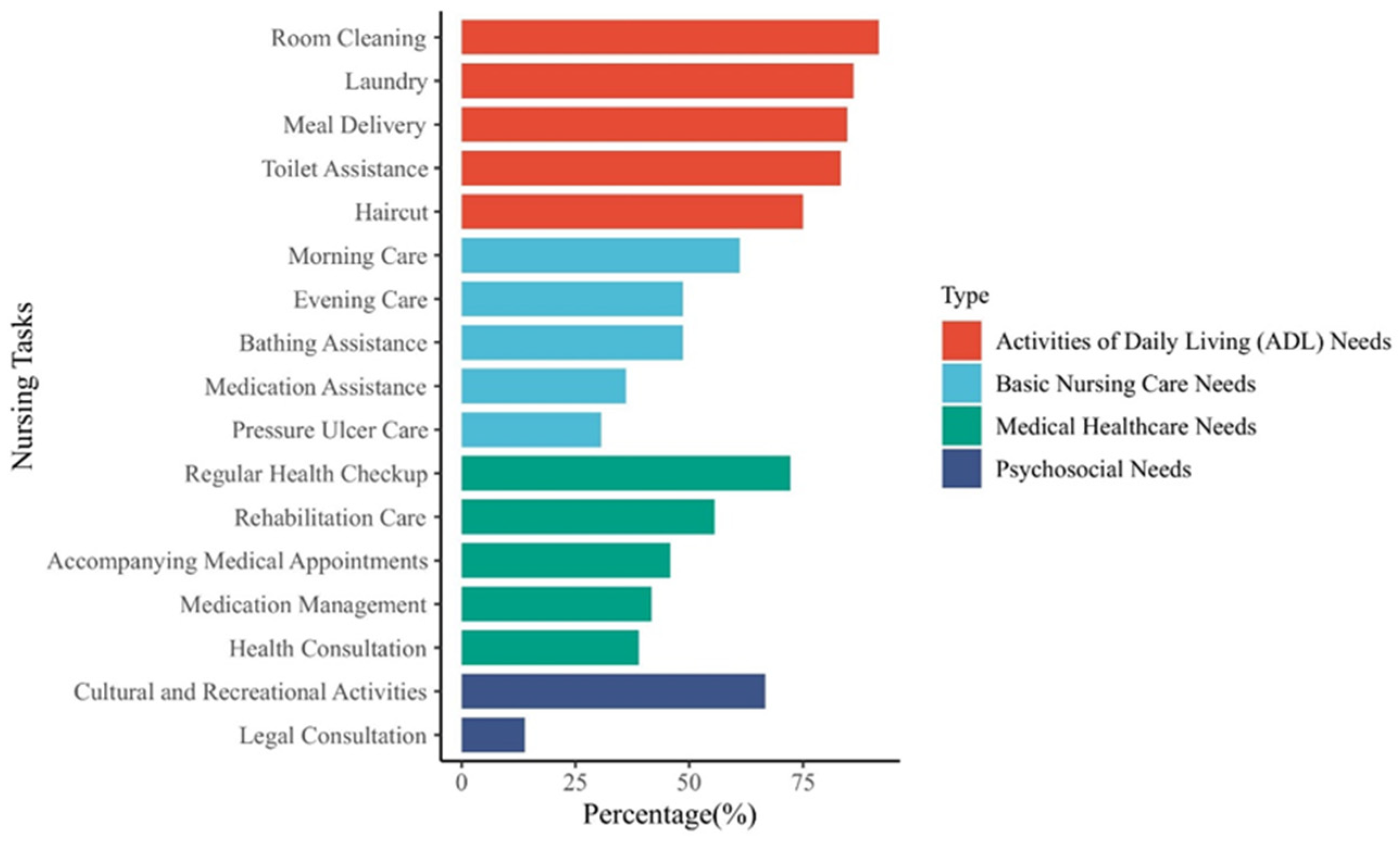
3. The Importance Analysis of Integrated Functionality in Nursing Wheelchairs
4. Future Trends in Nursing Wheelchair Development
- Multi-functional integration: Integration of multiple assistive care functions such as multi-posture change, transfer, bathing, and toileting.
- Intelligent and automated: able to navigate autonomously, avoid obstacles automatically, and perform care tasks such as standing, lifting, bathing, and toileting according to the patient’s needs.
- Individualized design and customization: future nursing wheelchairs will have greater ability to be individually configured, with customized settings based on the patient’s physical condition, needs, and preferences.
- Remote monitoring and cloud-connected technology: the nursing wheelchair will integrate sensors for vital signs monitoring, such as heart rate, blood pressure, blood glucose, etc., to monitor the patient’s health in real time.
- Diversity of human–computer interfaces: future nursing wheelchairs will offer a variety of human–computer interfaces, which may include smarter voice recognition, more intuitive touchscreens, more convenient head controls, and virtual reality interfaces.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. World Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Bedaf, S.; Gelderblom, G.J.; De Witte, L. Overview and categorization of robots supporting independent living of elderly people: What activities do they support and how far have they developed. Assist. Technol. 2015, 27, 88–100. [Google Scholar] [CrossRef]
- Khaksar, W.; Saplacan, D.; Bygrave, L.A.; Torresen, J. Robotics in Elderly Healthcare: A Review of 20 Recent Research Projects. arXiv 2023, arXiv:2302.04478. [Google Scholar]
- Johansson-Pajala, R.M.; Thommes, K.; Hoppe, J.A.; Tuisku, O.; Hennala, L.; Pekkarinen, S.; Melkas, H.; Gustafsson, C. Care robot orientation: What, who and how? Potential users’ perceptions. Int. J. Soc. Robot. 2020, 12, 1103–1117. [Google Scholar] [CrossRef]
- Matsumoto, H.; Ueki, M.; Uehara, K.; Noma, H.; Nozawa, N.; Osaki, M.; Hagino, H. Comparison of healthcare workers transferring patients using either conventional or robotic wheelchairs: Kinematic, electromyographic, and electrocardiographic analyses. J. Healthc. Eng. 2016, 2016, 5963432. [Google Scholar] [CrossRef]
- Sivakanthan, S.; Candiotti, J.L.; Sundaram, S.A.; Duvall, J.A.; Sergeant, J.J.G.; Cooper, R.; Satpute, S.; Turner, R.L.; Cooper, R.A. Mini-review: Robotic wheelchair taxonomy and readiness. Neurosci. Lett. 2022, 772, 136482. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, B.; Wei, S. Investigation and analysis of assistive device use in elderly patients with stroke disability. J. Nurs. 2017, 32, 85–88. [Google Scholar]
- Xiaochu LI, U.; Kunyan, W.E.I.; Li, G.U.; Mei, J.U. Attributes and influencing factors of service demand for the elderly in medical-nursing combined institutions. Chin. Nurs. Res. 2020, 3373. [Google Scholar] [CrossRef]
- Kamenov, K.; Mills, J.A.; Chatterji, S.; Cieza, A. Needs and unmet needs for rehabilitation services: A scoping review. Disabil. Rehabil. 2019, 41, 1227–1237. [Google Scholar] [CrossRef]
- De Vries, N.; Lavreysen, O.; Boone, A.; Bouman, J.; Szemik, S.; Baranski, K.; Godderis, L.; De Winter, P. Retaining healthcare workers: A systematic review of strategies for sustaining power in the workplace. Healthcare 2023, 11, 1887. [Google Scholar] [CrossRef]
- Sang, L.; Yamamura, M.; Dong, F.; Gan, Z.; Fu, J.; Wang, H.; Tian, Y. Analysis, design, and experimental research of a novel wheelchair-stretcher assistive robot. Appl. Sci. 2019, 10, 264. [Google Scholar] [CrossRef]
- Knibbe, J.J.; Friele, R.D. The use of logs to assess exposure to manual handling of patients, illustrated in an intervention study in home care nursing. Int. J. Ind. Ergon. 1999, 24, 445–454. [Google Scholar] [CrossRef]
- Keir, P.J.; MacDonell, C.W. Muscle activity during patient transfers: A preliminary study on the influence of lift assists and experience. Ergonomics 2004, 47, 296–306. [Google Scholar] [CrossRef]
- Ribeiro, T.; Serranheira, F.; Loureiro, H. Work related musculoskeletal disorders in primary health care nurses. Appl. Nurs. Res. 2017, 33, 72–77. [Google Scholar] [CrossRef]
- Labbé, D.; Yao, D.G.; Miller, W.C.; Routhier, F.; Rushton, P.W.; Demers, L.; Mortenson, W.B. Positive and negative experiences of caregivers helping power wheelchair users: A mixed-method study. Disabil. Rehabil. Assist. Technol. 2024, 1–12. [Google Scholar] [CrossRef]
- Rayssiguie, E.; Erden, M.S. A review of exoskeletons considering nurses. Sensors 2022, 22, 7035. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Work-Related Musculoskeletal Disorders and Ergonomics; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2020.
- Sivaprakasam, A.; Wang, H.; Cooper, R.A.; Koontz, A.M. Innovation in transfer assist technologies for persons with severe disabilities and their caregivers. IEEE Potentials 2017, 36, 34–41. [Google Scholar] [CrossRef]
- Wang, H.; Tsai, C.Y.; Jeannis, H.; Chung, C.S.; Kelleher, A.; Grindle, G.G.; Cooper, R.A. Stability analysis of electrical powered wheelchair-mounted robotic-assisted transfer device. J. Rehabil. Res. Dev. 2014, 51, 761–774. [Google Scholar] [CrossRef]
- Simpson, R.C.; LoPresti, E.F.; Cooper, R.A. How many people would benefit from a smart wheelchair? J. Rehabil. Res. Dev. 2008, 45, 53–72. [Google Scholar] [CrossRef]
- Naaris, M.; Konings, M.; Ortibus, E.; Monbaliu, E. Wheelchair skills training improves power mobility and participation in young people with cerebral palsy. Dev. Med. Child Neurol. 2024. online ahead of print. [Google Scholar] [CrossRef]
- Leaman, J.; La, H.M. A comprehensive review of smart wheelchairs: Past, present, and future. IEEE Trans. Hum.-Mach. Syst. 2017, 47, 486–499. [Google Scholar] [CrossRef]
- Ortiz, J.S.; Palacios-Navarro, G.; Andaluz, V.H.; Guevara, B.S. Virtual reality-based framework to simulate control algorithms for robotic assistance and rehabilitation tasks through a standing wheelchair. Sensors 2021, 21, 5083. [Google Scholar] [CrossRef] [PubMed]
- Cooper, R.A.; Cooper, R. Rehabilitation Engineering: A perspective on the past 40-years and thoughts for the future. Med. Eng. Phys. 2019, 72, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Candiotti, J.L.; Kamaraj, D.C.; Daveler, B.; Chung, C.S.; Grindle, G.G.; Cooper, R.; Cooper, R.A. Usability evaluation of a novel robotic power wheelchair for indoor and outdoor navigation. Arch. Phys. Med. Rehabil. 2019, 100, 627–637. [Google Scholar] [CrossRef] [PubMed]
- Cao, W.; Yu, H.; Wu, X.; Li, S.; Meng, Q.; Chen, C. Development and evaluation of a rehabilitation wheelchair with multiposture transformation and smart control. Complexity 2021, 2021, 6628802. [Google Scholar] [CrossRef]
- Thongpance, N.; Chotikunnan, P. Design and Construction of Electric Wheelchair with Mecanum Wheel. J. Robot. Control JRC 2023, 4, 71–82. [Google Scholar] [CrossRef]
- Zhang, L.; Yang, Y.; Yang, Y.; Chen, W. Intelligent Robot Design to Assistance the Elderly in Toilet. In Proceedings of the 2022 International Conference on Computer Science, Information Engineering and Digital Economy (CSIEDE 2022), Guangzhou, China, 28–30 October 2022; Atlantis Press: Amsterdam, The Netherlands, 2022; pp. 363–368. [Google Scholar]
- Koyama, S.; Tanabe, S.; Otaka, Y.; Kato, T.; Furuzawa, S.; Tatemoto, T.; Kumazawa, N.; Yoshimuta, H.; Torii, K.; Tsukada, S.; et al. Novel lateral transfer assist robot decreases the difficulty of transfer in post-stroke hemiparesis patients: A pilot study. Disabil. Rehabil. Assist. Technol. 2022, 17, 828–832. [Google Scholar] [CrossRef]
- Kume, Y.; Tsukada, S.; Kawakami, H. Design and evaluation of rise assisting bed “Resyone®” based on ISO 13482. J. Robot. Soc. Jpn. 2015, 33, 781–788. [Google Scholar] [CrossRef]
- Zlatintsi, A.; Dometios, A.C.; Kardaris, N.; Rodomagoulakis, I.; Koutras, P.; Papageorgiou, X.; Maragos, P.; Tzafestas, C.S.; Vartholomeos, P.; Hauer, K.; et al. I-Support: A robotic platform of an assistive bathing robot for the elderly population. Robot. Auton. Syst. 2020, 126, 103451. [Google Scholar] [CrossRef]
- He, Z.; Yuan, F.; Chen, D.; Wang, M. Ergonomic design of multi-functional bathing robot. In Proceedings of the 2019 IEEE International Conference on Real-Time Computing and Robotics (RCAR), Irkutsk, Russia, 4–9 August 2019; pp. 580–585. [Google Scholar]
- Shi, X.; Lu, H.; Chen, Z. Design and analysis of an intelligent toilet wheelchair based on planar 2DOF parallel mechanism with coupling branch chains. Sensors 2021, 21, 2677. [Google Scholar] [CrossRef]
- Zhang, Z.; Lu, J.L.; Ochiai, Y. Indoor Auto-Navigate System for Electric Wheelchairs in a Nursing Home. In Universal Access in Human-Computer Interaction. Novel Design Approaches and Technologies. HCII 2022; Antona, M., Stephanidis, C., Eds.; Lecture Notes in Computer Science; Springer: Cham, Switzerland, 2022; Volume 13308. [Google Scholar] [CrossRef]
- Haddad, M.J.; Sanders, D.A. Selecting a best compromise direction for a powered wheelchair using PROMETHEE. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 228–235. [Google Scholar] [CrossRef]
- Sevastopoulos, C.; Acharya, S.; Makedon, F. An RGB-D Fusion System for Indoor Wheelchair Navigation. In Proceedings of the 16th International Conference on PErvasive Technologies Related to Assistive Environments, Corfu, Greece, 5–7 July 2023; pp. 187–191. [Google Scholar]
- Wang, C.; Xia, M.; Meng, M.Q.H. Stable autonomous robotic wheelchair navigation in the environment with slope way. IEEE Trans. Veh. Technol. 2020, 69, 10759–10771. [Google Scholar] [CrossRef]
- Xie, Y.; Guo, S.; Li, Y.; Zhang, X. Automatic docking optimization method of bed and chair based on multi-sensor information fusion. J. Internet Technol. 2022, 23, 99–108. [Google Scholar]
- Correia, D.; Pereira, A.; Pedrosa, E. Semantic Navigation Applied to Narrow Passages for Intelligent Wheelchairs. In Proceedings of the 2023 IEEE International Conference on Autonomous Robot Systems and Competitions (ICARSC), Tomar, Portugal, 26–27 April 2023; pp. 151–156. [Google Scholar]
- Megalingam, R.K.; Rajendraprasad, A.; Raj, A.; Raghavan, D.; Teja, C.R.; Sreekanth, S.; Sankaran, R. Self-E: A self-driving wheelchair for elders and physically challenged. Int. J. Intell. Robot. Appl. 2021, 5, 477–493. [Google Scholar] [CrossRef]
- Iskanderani, A.I.; Tamim, F.R.; Rana, M.M.; Ahmed, W.; Mehedi, I.M.; Aljohani, A.J.; Latif, A.; Shaikh, S.A.L.; Shorfuzzaman, M.; Akther, F.; et al. Voice Controlled Artificial Intelligent Smart Wheelchair. In Proceedings of the 2020 8th International Conference on Intelligent and Advanced Systems (ICIAS), Kuching, Malaysia, 13–15 July 2021; pp. 1–5. [Google Scholar]
- Sunny, M.S.H.; Zarif, M.I.I.; Rulik, I.; Sanjuan, J.; Rahman, M.H.; Ahamed, S.I.; Wang, I.; Schultz, K.; Brahmi, B. Eye-gaze control of a wheelchair mounted 6DOF assistive robot for activities of daily living. J. NeuroEng. Rehabil. 2021, 18, 173. [Google Scholar] [CrossRef] [PubMed]
- Rabhi, Y.; Mrabet, M.; Fnaiech, F. A facial expression controlled wheelchair for people with disabilities. Comput. Methods Programs Biomed. 2018, 165, 89–105. [Google Scholar] [CrossRef]
- Maciel, G.M.; Pinto, M.F.; Júnior, I.C.D.S.; Coelho, F.O.; Marcato, A.L.; Cruzeiro, M.M. Shared control methodology based on head positioning and vector fields for people with quadriplegia. Robotica 2022, 40, 348–364. [Google Scholar] [CrossRef]
- Li, Z.; Zhao, S.; Duan, J.; Su, C.Y.; Yang, C.; Zhao, X. Human cooperative wheelchair with brain–machine interaction based on shared control strategy. IEEE/ASME Trans. Mechatron. 2016, 22, 185–195. [Google Scholar] [CrossRef]
- Hosni, S.M.; Shedeed, H.A.; Mabrouk, M.S.; Tolba, M.F. EEG-EOG based virtual keyboard: Toward hybrid brain computer interface. Neuroinformatics 2019, 17, 323–341. [Google Scholar] [CrossRef] [PubMed]
- Rosero-Montalvo, P.D.; Peluffo-Ordóñez, D.H.; Batista, V.F.L.; Serrano, J.; Rosero, E.A. Intelligent system for identification of wheelchair user’s posture using machine learning techniques. IEEE Sens. J. 2018, 19, 1936–1942. [Google Scholar] [CrossRef]
- Cui, J.; Cui, L.; Huang, Z.; Li, X.; Han, F. IoT wheelchair control system based on multi-mode sensing and human-machine interaction. Micromachines 2022, 13, 1108. [Google Scholar] [CrossRef]
- Kabir, A.T.; Saha, P.K.; Sarowar, M.G.; Saha, R.; Ahmad, I.; Zishan, M.S.R. Smart Wheelchair for COVID-19 Patients with Mobile Application Based Health Monitoring System. In Proceedings of the 2023 3rd International Conference on Robotics, Electrical and Signal Processing Techniques (ICREST), Dhaka, Bangladesh, 7–8 January 2023; pp. 336–340. [Google Scholar]
- Trinkoff, A.M.; Lipscomb, J.A.; Geiger-Brown, J.; Brady, B. Musculoskeletal problems of the neck, shoulder, and back and functional consequences in nurses. Am. J. Ind. Med. 2002, 41, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Pancholi, S.; Wachs, J.P.; Duerstock, B.S. Use of artificial intelligence techniques to assist individuals with physical disabilities. Annu. Rev. Biomed. Eng. 2024, 26, 1–24. [Google Scholar] [CrossRef]
- Gomes, B.; Torres, J.; Sobral, P.; Sousa, A.; Reis, L.P. Stereo Based 3D Perception for Obstacle Avoidance in Autonomous Wheelchair Navigation. In Proceedings of the Iberian Robotics Conference, Zaragoza, Spain, 23–25 November 2022; Springer International Publishing: Cham, Switzerland, 2022; pp. 321–332. [Google Scholar]
- Bakouri, M.; Alsehaimi, M.; Ismail, H.F.; Alshareef, K.; Ganoun, A.; Alqahtani, A.; Alharbi, Y. Steering a robotic wheelchair based on voice recognition system using convolutional neural networks. Electronics 2022, 11, 168. [Google Scholar] [CrossRef]
- Kozlowski, A.; Bryce, T.; Dijkers, M. Time and effort required by persons with spinal cord injury to learn to use a powered exoskeleton for assisted walking. Top. Spinal Cord Inj. Rehabil. 2015, 21, 110–121. [Google Scholar] [CrossRef] [PubMed]
- King, E.C.; Holliday, P.J.; Andrews, G.J. Care Challenges in the Bathroom: The Views of Professional Care Providers Working in Clients’ Homes. J. Appl. Gerontol. 2018, 37, 493–515. [Google Scholar] [CrossRef]
- Bostelman, R.; Ryu, J.C.; Chang, T.; Johnson, J.; Agrawal, S.K. An advanced patient lift and transfer device for the home. J. Med. Devices 2010, 4, 011004. [Google Scholar] [CrossRef]
- Abdul Halim, N.S.S.; Mohd Ripin, Z.; Yusuf, A.; Ridzwan, M.I.Z. Efficacy of lifting devices for wheelchair transfers: A systematic review and meta-analysis. Ergonomics 2024, 1–12. [Google Scholar] [CrossRef]
- Liu, Y.; Yin, Y.; Jiang, Z.; Guo, S. Motion Analysis and Tactile-Based Impedance Control of the Chest Holder of a Piggyback Patient Transfer Robot. J. Healthc. Eng. 2021, 2021, 9918019. [Google Scholar] [CrossRef]
- Rice, M.S.; Woolley, S.M.; Waters, T.R. Comparison of required operating forces between floor-based and overhead-mounted patient lifting devices. Ergonomics 2009, 52, 112–120. [Google Scholar] [CrossRef]
- Mukai, T.; Hirano, S.; Yoshida, M.; Nakashima, H.; Guo, S.; Hayakawa, Y. Tactile-based motion adjustment for the nursing-care assistant robot RIBA. In Proceedings of the 2011 IEEE International Conference on Robotics and Automation, Shanghai, China, 9–13 May 2011; pp. 5435–5441. [Google Scholar]
- Ding, M.; Ikeura, R.; Mori, Y.; Mukai, T.; Hosoe, S. Lift-up motion generation of nursing-care assistant robot based on human muscle force and body softness estimation. In Proceedings of the 2014 IEEE/ASME International Conference on Advanced Intelligent Mechatronics, Besacon, France, 8–11 July 2014; pp. 1302–1307. [Google Scholar]
- Honarvar, M.H.; Suzuki, T.; Sato, S.; Nakamura, Y. 4-D body posture in sagittal plane for care-receiver patient can be estimated by using only two low-reolution tactile sensors mounted on robot arms. In Proceedings of the 2014 Second RSI/ISM International Conference on Robotics and Mechatronics (ICRoM), Tehran, Iran, 15–17 October 2014; pp. 684–689. [Google Scholar]
- Baptiste, A.; Boda, S.V.; Nelson, A.L.; Lloyd, J.D.; Lee, W.E., III. Friction-reducing devices for lateral patient transfers: A clinical evaluation. Aaohn J. 2006, 54, 173–180. [Google Scholar] [CrossRef]
- Zhang, J.; Zhao, X.; Ma, L.; Li, J. Research Status of Bathing Aids for the Elderly. In Proceedings of the 2022 12th International Conference on CYBER Technology in Automation, Control, and Intelligent Systems (CYBER), Baishan, China, 27–31 July 2022; pp. 712–717. [Google Scholar] [CrossRef]
- Wang, W.; Chen, Y.; Zou, X.; Wang, S.; Ferreira, J.P.; Liu, T. Development of Bath Auxiliary Robot for the Disabled Elderly. In Proceedings of the 2021 IEEE International Conference on Intelligence and Safety for Robotics (ISR), Tokoname, Japan, 4–6 March 2021; pp. 85–88. [Google Scholar] [CrossRef]
- Jin, J.; Jin, S.; Zhao, D.; Li, C. Self-Reliance Transfer Support Robot for Home-Based Care. In Proceedings of the 2022 7th International Conference on Robotics and Automation Engineering (ICRAE), Singapore, 18–20 November 2022; pp. 206–209. [Google Scholar]
- Simpson, R.C.; Levine, S.P.; Bell, D.A.; Jaros, L.A.; Koren, Y.; Borenstein, J. NavChair: An assistive wheelchair navigation system with automatic adaptation. In Assistive Technology and Artificial Intelligence: Applications in Robotics, User Interfaces and Natural Language Processing; Springer: Berlin/Heidelberg, Germany, 1998; pp. 235–255. [Google Scholar]
- Kader, M.A.; Alam, M.E.; Jahan, N.; Bhuiyan MA, B.; Alam, M.S.; Sultana, Z. Design and im-plementation of a head motion-controlled semi-autonomous wheelchair for quadriplegic patients based on 3-axis accel-erometer. In Proceedings of the 2019 22nd International Conference on Computer and Information Technology (ICCIT), Dhaka, Bangladesh, 18–20 December 2019; pp. 1–6. [Google Scholar]
- Hemmati, A.; Rahmani, A.M. The Internet of Autonomous Things applications: A taxonomy, technologies, and future directions. Internet Things 2022, 20, 100635. [Google Scholar] [CrossRef]
- Nardi, F.; Lázaro, M.T.; Iocchi, L.; Grisetti, G. Generation of laser-quality 2D navigation maps from RGB-D sensors. In RoboCup 2018: Robot World Cup XXII 22; Springer International Publishing: Cham, Switzerland, 2019; pp. 238–250. [Google Scholar]
- Sanders, D.A. Using self-reliance factors to decide how to share control between human powered wheelchair drivers and ultrasonic sensors. IEEE Trans. Neural Syst. Rehabil. Eng. 2016, 25, 1221–1229. [Google Scholar] [CrossRef] [PubMed]
- Diao, C.; Jia, S.; Zhang, G.; Sun, Y.; Zhang, X.; Xue, Y.; Li, X. Design and realization of a novel obstacle avoidance algorithm for intelligent wheelchair bed using ultrasonic sensors. In Proceedings of the 2017 Chinese Automation Congress (CAC), Jinan, China, 20–22 October 2017; pp. 4153–4158. [Google Scholar]
- Huang, J.; Junginger, S.; Liu, H.; Thurow, K. Indoor Positioning Systems of Mobile Robots: A Review. Robotics 2023, 12, 47. [Google Scholar] [CrossRef]
- Szaj, W.; Fudali, P.; Wojnarowska, W.; Miechowicz, S. Mechatronic anti-collision system for electric wheelchairs based on 2D LiDAR laser scan. Sensors 2021, 21, 8461. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, N.; Azzan, S.; Jaitoo, V.; Durairajah, V.; Gobee, S. Smart Wheelchair Navigation Using ROS with Collision Avoidance and 2D Map. In Proceedings of the International Conference for Innovation in Biomedical Engineering and Life Sciences, Kuala Lumpur, Malaysia, 10–13 December 2022; Springer Nature: Cham, Switzerland, 2022; pp. 135–143. [Google Scholar]
- Yu, Y.; Liu, Y.; Jiang, J.; Yin, E.; Zhou, Z.; Hu, D. An asynchronous control paradigm based on sequential motor imagery and its application in wheelchair navigation. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 2367–2375. [Google Scholar] [CrossRef]
- Abe, Y.; Hirose, T. Construction of a high-accuracy point cloud map for the automatic driving of an electric wheelchair. SEATUC J. Sci. Eng. 2020, 1, 1–6. [Google Scholar]
- Castagno, J.; Atkins, E. Polylidar3d-fast polygon extraction from 3d data. Sensors 2020, 20, 4819. [Google Scholar] [CrossRef] [PubMed]
- Cojocaru, D.; Manta, L.F.; Pană, C.F.; Dragomir, A.; Mariniuc, A.M.; Vladu, I.C. The design of an intelligent robotic wheelchair supporting people with special needs, including for their visual system. Healthcare 2021, 10, 13. [Google Scholar] [CrossRef] [PubMed]
- Xiao, H.; Li, Z.; Yang, C.; Yuan, W.; Wang, L. RGB-D sensor-based visual target detection and tracking for an intelligent wheelchair robot in indoors environments. Int. J. Control Autom. Syst. 2015, 13, 521–529. [Google Scholar] [CrossRef]
- Wang, H.; Sun, Y.; Fan, R.; Liu, M. S2P2: Self-supervised goal-directed path planning using RGB-D data for robotic wheelchairs. In Proceedings of the 2021 IEEE International Conference on Robotics and Automation (ICRA), Xi’an, China, 30 May–5 June 2021; pp. 11422–11428. [Google Scholar]
- Ngo, B.V.; Nguyen, T.H.; Vu, C.C. Automatic Labeling of Natural Landmarks for Wheelchair Motion Planning. Electronics 2023, 12, 3093. [Google Scholar] [CrossRef]
- Haddad, M.; Sanders, D.; Tewkesbury, G.; Langner, M.; Simandjuntak, S. Intelligent user interface to control a powered wheelchair using infrared sensors. In Intelligent Systems and Applications: Proceedings of the 2021 Intelligent Systems Conference (IntelliSys); Springer International Publishing: Cham, Switzerland, 2022; Volume 1, pp. 640–649. [Google Scholar]
- Malek, N. Safety Wheelchair Navigation System. J. Microcontrol. Eng. Appl. 2020, 7, 6–11. [Google Scholar]
- Mahdin, M.E.; Ornob, T.M.; Akhter, M.E.; Mullick, S.A.; Arnob, S.S.; Palit, R.; Habib, A.B. Hand gesture controlled smart wheelchair with gps tracking and deep learning based object detection for collision avoidance. In Proceedings of the 2022 IEEE International Women in Engineering (WIE) Conference on Electrical and Computer Engineering (WIECON-ECE), Naya Raipur, India, 30–31 December 2022; pp. 147–152. [Google Scholar]
- Qinghua, C.; Taihu, Z.; Yihong, X.; Hongyu, S. Design and Realization of Intelligent Wheelchair Based on STM32. J. Phys. Conf. Ser. 2020, 1678, 012114. [Google Scholar] [CrossRef]
- Favey, C.; Farcy, R.; Bogaert, L.; Berthe, I.; Jordan, L. Sensors and Strategy for Anticollision Function dedicated to Augmented Electric Wheelchair. arXiv 2024. [Google Scholar] [CrossRef]
- Sayied Haque, M.S.; Tanvir Rahman, M.; Tasin Khan, R.; Shibli Kaysar, M. Voice Assistant and Touch Screen Operated Intelligent Wheelchair for Physically Challenged People. In Proceedings of International Conference on Trends in Computational and Cognitive Engineering: Proceedings of TCCE 2020; Springer: Singapore, 2021; pp. 405–415. [Google Scholar]
- Choi, J.W.; Park, J.; Huh, S.; Jo, S. Asynchronous Motor Imagery BCI and LiDAR-based Shared Control System for Intuitive Wheelchair Navigation. IEEE Sens. J. 2023, 23, 16252–16263. [Google Scholar] [CrossRef]
- Zhang, R.; Li, Y.; Yan, Y.; Zhang, H.; Wu, S.; Yu, T.; Gu, Z. Control of a wheelchair in an indoor environment based on a brain–computer interface and automated navigation. IEEE Trans. Neural Syst. Rehabil. Eng. 2015, 24, 128–139. [Google Scholar] [CrossRef]
- Cao, L.; Li, J.; Ji, H.; Jiang, C. A hybrid brain computer interface system based on the neurophysiological protocol and brain-actuated switch for wheelchair control. J. Neurosci. Methods 2014, 229, 33–43. [Google Scholar] [CrossRef] [PubMed]
- Dahmani, M.; Chowdhury, M.E.; Khandakar, A.; Rahman, T.; Al-Jayyousi, K.; Hefny, A.; Kiranyaz, S. An intelligent and low-cost eye-tracking system for motorized wheelchair control. Sensors 2020, 20, 3936. [Google Scholar] [CrossRef] [PubMed]
- Cruz, R.; Souza, V.; Bastos Filho, T.; Lucena, V. Electric powered wheelchair command by information fusion from eye tracking and bci. In Proceedings of the 2019 IEEE International Conference on Consumer Electronics (ICCE), Las Vegas, NV, USA, 11–13 January 2019; pp. 1–2. [Google Scholar]
- Wołoszyn, N.; Grzegorczyk, J.; Wiśniowska-Szurlej, A.; Kilian, J.; Kwolek, A. Psychophysical health factors and its correlations in elderly wheelchair users who live in nursing homes. Int. J. Environ. Res. Public Health 2020, 17, 1706. [Google Scholar] [CrossRef]
- Rulik, I.; Sunny, M.S.H.; Sanjuan De Caro, J.D.; Zarif, M.I.I.; Brahmi, B.; Ahamed, S.I.; Schultz, K.; Wang, I.; Leheng, T.; Peng, J.; et al. Control of a wheelchair-mounted 6DOF assistive robot with Chin and finger joysticks. Front. Robot. AI 2022, 9, 885610. [Google Scholar] [CrossRef]
- Kim, J.; Park, H.; Bruce, J.; Rowles, D.; Holbrook, J.; Nardone, B.; West, D.P.; Laumann, A.; Roth, E.J.; Ghovanloo, M. Assessment of the tongue-drive system using a computer, a smartphone, and a powered-wheelchair by people with tetraplegia. IEEE Trans. Neural Syst. Rehabil. Eng. 2015, 24, 68–78. [Google Scholar] [CrossRef]
- Cojocaru, D.; Manta, L.F.; Vladu, I.C.; Dragomir, A.; Mariniuc, A.M. Using an eye gaze new combined approach to control a wheelchair movement. In Proceedings of the 2019 23rd International Conference on System Theory, Control and Computing (ICSTCC), Sinaia, Romania, 9–11 October 2019; pp. 626–631. [Google Scholar]
- Tang, J.; Liu, Y.; Hu, D.; Zhou, Z. Towards BCI-actuated smart wheelchair system. Biomed. Eng. Online 2018, 17, 111. [Google Scholar] [CrossRef] [PubMed]
- Tonin, L.; Perdikis, S.; Kuzu, T.D.; Pardo, J.; Orset, B.; Lee, K.; Aach, M.; Schildhauer, T.A.; Martínez-Olivera, R.; Millán, J.D.R. Learning to control a BMI-driven wheelchair for people with severe tetraplegia. Iscience 2022, 25, 105418. [Google Scholar] [CrossRef] [PubMed]
- Andersen, L.L.; Burdorf, A.; Fallentin, N.; Persson, R.; Jakobsen, M.D.; Mortensen, O.S.; Clausen, T.; Holtermann, A. Patient transfers and assistive devices: Prospective cohort study on the risk for occupational back injury among healthcare workers. Scandinavian journal of work. Environ. Health 2014, 40, 74–81. [Google Scholar] [CrossRef]
- Quinn, M.M.; Markkanen, P.K.; Galligan, C.J.; Sama, S.R.; Lindberg, J.E.; Edwards, M.F. Healthy aging requires a healthy home care workforce: The occupational safety and health of home care aides. Curr. Environ. Health Rep. 2021, 8, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Sahoo, S.K.; Choudhury, B.B. AI advances in wheelchair navigation and control: A comprehensive review. J. Process Manag. New Technol. 2023, 11, 115–132. [Google Scholar] [CrossRef]

| Paper | Nursing Care Functions | Multiple Sensor Fusion Technology | Human–Machine Interaction (HMI) |
|---|---|---|---|
| [10] Sang, L. (2019) | Transfer assist, lift assists, auxiliary toilet | None | Remote control |
| [25] Candiotti, J. (2019) | Assistive standing | None | Joystick control, navigation display screen |
| [26] Cao, W. (2021) | Assistive Standing, Multi-position adjustment | None | Joystick control, Voice control |
| [27] Thongpance, N. (2023) | N | None | Holonomic motion control |
| [28] Zhang, L. (2022) | Transfer assist, assistive standing | None | Remote control |
| [29] Koyama, S. (2022) | Bed-to-chair transfer assistance | None | Holonomic motion control |
| [30] Kume, Y. (2015) | Bed-to-chair transfer assistance | None | Remote control |
| [31] Zlatintsi, A. (2020) | Assistive bathing, transfer assist | None | Voice control, Gesture recognition control |
| [32] He, Z. (2019) | Assistive bathing | None | Intelligent AI recognition, Ergonomic design |
| [33] Shi, X. (2021) | Auxiliary toilet, assistive standing | None | Holonomic motion control |
| [34] Zhang, Z. (2022) | None | RGB-D | Navigation display screen, Joystick control |
| [35] Haddad, M.J. (2019) | None | Ultrasonic Sensor | Joystick control |
| [36] Sevastopoulos, C.(2023) | None | RGB-D | None |
| [37] Wang, C. (2020) | None | 3D-LIDAR, IMU | None |
| [38] Xie, Y. (2022) | Bed-to-chair transfer assistance, multi-position adjustment | 3D-LIDAR, RGB-D | None |
| [39] Correia, D. (2023) | None | LIDAR | Navigation display screen, Joystick control |
| [40] Megalingam, R.K. (2021) | None | LIDAR, IMU | Touchscreen navigation control |
| [41] Iskanderani, A.I. (2021) | None | Google Map | Voice control |
| [42] Sunny, M.S.H. (2021) | Robotic arm-assisted object retrieval | RGB | Eye-gaze control, Touchscreen navigation |
| [43] Rabhi, I. (2018) | None | Camera | Expression control |
| [44] Maciel, G.M. (2022) | None | RGB-D, IMU | head position control |
| [45,46] Li, Z. (2016) | None | Laser Sensor, EEG, RGB | BMI control |
| [47] Rosero-Montalvo, P.D. (2018) | Sitting posture monitoring | None | None |
| [48] Cui, J. (2022) | Vital signs monitoring, location detection, mobile environment detection | GPS, LIDAR, WIFI | Remote control, Gesture recognition control |
| [49] Kabir, A.T. (2023) | Vital signs monitoring, location detection | GPS, Infrared Sensor | Joystick control |
| Assistive Function | Description | Advantages | Disadvantages | Evaluation Criteria |
|---|---|---|---|---|
| Assistive Bathing [31,32,65] | Automated systems to aid patients in bathing activities. | Enhances independence; reduces caregiver strain. | High cost; complex maintenance requirements. | Cost-effectiveness: How the benefits align with costs. User impact: Effect on independence and caregiver reliance. |
| Bed-to-Chair Transfer [18,29,56,57,58] | Mechanisms facilitating transfers between beds and chairs. | Reduces physical exertion and risk of injuries. | Equipment cost and space requirements. | Operational ease: Simplicity of use. Safety: Risk of injuries to users. |
| Assistive Toileting [28,30,33,55,66] | Features facilitating the toileting process, such as automated seat adjustments. | Promotes patient dignity and independence. | Complexity in cleaning and maintenance. | Usability: Ease of cleaning and operation. Hygiene standards: Compliance with health and sanitation requirements. |
| Assistive Standing [26,27,53,54] | Support systems to aid users in standing up. | Supports rehabilitation and mobility. | Requires robust mechanical systems; potential safety risks. | Functionality: Support in daily activities. User safety: Ensuring the system is safe under all conditions. |
| Multi-Posture Adjustment [26,57,59] | Enables various seating adjustments to enhance comfort and health. | Prevents pressure ulcer; customizable to user needs. | Mechanism complexity leads to potential failures. | Reliability: Consistency and longevity of the mechanism. User comfort: Impact on user’s physical comfort and health. |
| Vital Signs Monitoring [31] | Sensors to monitor physiological parameters such as heart rate and temperature. | Allows continuous health monitoring; can alert to medical issues. | Increases cost; may raise privacy concerns. | Health impact: Effectiveness in improving patient monitoring. Privacy considerations: Handling of sensitive data. |
| Assistive Retrieval [60,61,62] | Robotic arms or similar mechanisms to help users retrieve objects. | Reduces dependency on caregivers for common tasks. | High initial and ongoing costs; complex mechanics. | Effectiveness: Ability to accurately perform intended tasks. Cost-efficiency: Economic viability given the benefits. |
| Sensor Type | Feature | Advantage/Disadvantage | Evaluation Methods |
|---|---|---|---|
| 2D LiDAR [23,70,74,75] | Facilitates flat map creation; utilized for obstacle navigation | Relatively cost-effective; Limited by the absence of vertical information, leading to blind spots in intricate 3D environments. | Field Testing: Real-world performance in varied environments. Accuracy Assessment: Measurement of detection precision and range. |
| 3D LiDAR [52,76,77,78,79] | Enables the generation of detailed 3D maps; adept at detecting and circumventing intricate obstacles | Provides a holistic environmental structure suitable for intricate navigation scenarios; Demands substantial computational resources for processing 3D. | Simulation Testing: Use in virtual environments to predict functionality. Integration Testing: Compatibility with other navigation systems. |
| RGB-D [36,70,80,81,82] | Offers visual information and delineates the 3D structure of the scene | Delivers high-resolution color imagery and depth data; Susceptible to lighting conditions, potential performance degradation in low-light or non-uniform lighting scenarios | Operational Testing: Evaluation in controlled environments to measure reliability and range. User Feedback: Collection of practical usage data from operators. |
| Ultrasonic Sensor [71,72] | Employed for short-range obstacle detection and avoidance | Economical solution; unaffected by lighting conditions; limited precision. | Comparative Analysis: Benchmark against other sensor types for object recognition accuracy. Environmental Testing: Assess performance across different lighting conditions. |
| Infrared Sensor [83,84] | Utilized for detecting distance, temperature, and related parameters | Cost-effective; Influenced by lighting and environmental temperature. | Precision Mapping: Evaluation of positioning accuracy in diverse geographic settings. Durability Testing: Long-term reliability and signal consistency. |
| GPS [85,86] | Designed for outdoor large-scale navigation and positioning | Exhibits high precision in outdoor navigation; Inapplicable for indoor navigation. | Precision Mapping: Evaluation of positioning accuracy in diverse geographic settings. Durability Testing: Long-term reliability and signal consistency. |
| IMU | Employed for attitude estimation, motion control, and navigation | High-frequency data updates; adaptable to dynamic scenarios; cumulative errors over time result in drift. | performance Metrics: Analysis of drift and correction mechanisms. Sensor Fusion Analysis: Effectiveness in integration with other technologies like GPS or LiDAR. |
| Sonar Sensor [68,87,88] | Utilized for distance measurement, obstacle detection, and positioning | Utilized for distance measurement, obstacle detection, and positioning. | Range Testing: Evaluate effective operational range and sensitivity. Robustness Analysis: Assess performance against environmental variables like humidity or temperature. |
| Interaction Mode | Description | Advantages | Disadvantages |
|---|---|---|---|
| Touchscreen [40,88] | Interface that allows users to interact with the system via touch inputs. | Intuitive and user-friendly; suitable for routine operations. | May be difficult to use under direct sunlight or in brightly lit conditions. |
| Voice Recognition System [40,42,89] | Technology that allows the wheelchair to be controlled through spoken commands. | Allows hands-free operation; convenient for voice commands. | May be affected by ambient noise; sensitive to accents and speech variations. |
| Remote Control [6,7,11,25,30] | A device or system that enables the wheelchair to be controlled from a distance. | Enables users or caregivers to control the wheelchair remotely. | Requires carrying a remote; risk of signal interference. |
| Brain–Machine Interface (BMI) [45,48,89,90,91] | An interface that translates neuronal information into commands capable of controlling the wheelchair. | Suitable for users with severe mobility restrictions. | Requires specific training; high cost; practicality depends on technological advancement. |
| Body Part Control (e.g., gestures, foot) [47] | Systems that allow wheelchair control using different body parts like feet or other gestures. | Allows users with limited hand mobility to control using other body parts. | Requires some physical coordination ability; may not be suitable for all users. |
| Eye Movement Control [42,92,93,94] | Technology that tracks eye movements to control the wheelchair. | Provides an efficient control method for users with extreme mobility limitations. | Requires high precision technology; may need time for users to adapt. |
| Facial Expression Control [43] | Systems that use facial expression recognition to control the wheelchair. | Controls through user facial expressions, so no need for hand or voice operation. | Needs highly sensitive sensors and advanced algorithms. |
| Head Movement Control [44,95,96] | Interfaces that use the direction and angle of the head for wheelchair control. | Allows users to control direction and speed by moving their head. | May not be suitable for users with neck injuries or conditions. |
| Health-Monitoring Interaction [97] | Systems that integrate health monitoring sensors to manage and respond to physiological data. | Monitors vital parameters like heart rate, ensuring safety. | Requires ongoing data processing and privacy protection measures. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Z.; Xu, P.; Wu, C.; Yu, H. Smart Nursing Wheelchairs: A New Trend in Assisted Care and the Future of Multifunctional Integration. Biomimetics 2024, 9, 492. https://doi.org/10.3390/biomimetics9080492
Zhang Z, Xu P, Wu C, Yu H. Smart Nursing Wheelchairs: A New Trend in Assisted Care and the Future of Multifunctional Integration. Biomimetics. 2024; 9(8):492. https://doi.org/10.3390/biomimetics9080492
Chicago/Turabian StyleZhang, Zhewen, Peng Xu, Chengjia Wu, and Hongliu Yu. 2024. "Smart Nursing Wheelchairs: A New Trend in Assisted Care and the Future of Multifunctional Integration" Biomimetics 9, no. 8: 492. https://doi.org/10.3390/biomimetics9080492






