Cerebral Venous Thrombosis: A Challenging Diagnosis; A New Nonenhanced Computed Tomography Standardized Semi-Quantitative Method
Abstract
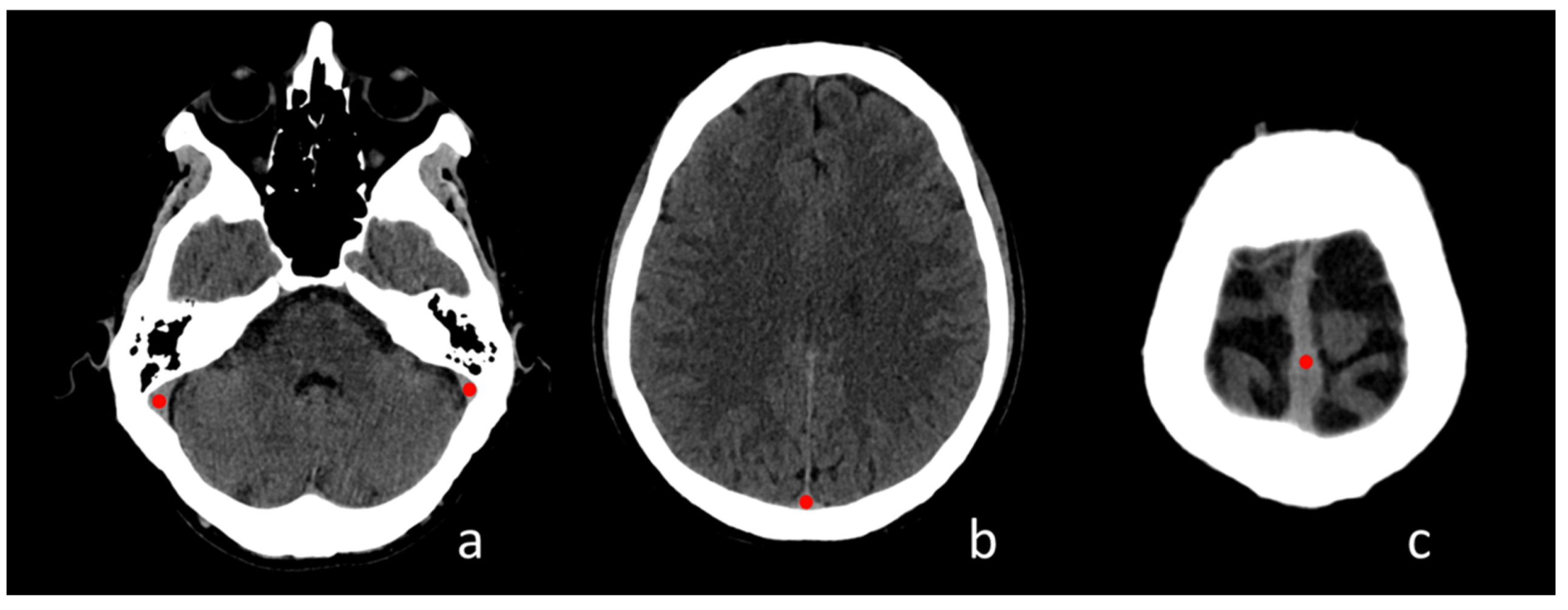
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Inclusion Criteria
- Clinical suspicion of CVST.
- No history of previous venous sinus thrombosis.
- Plain CT and CTV performed <24 h from clinical onset.
2.3. Exclusion Criteria
- Coexistence of other acute intracranial brain diseases.
- Presence of significant artifacts on CT images.
2.4. CT Protocol
2.5. Image Analysis
2.6. Statistical Analysis
3. Results
3.1. Subject Population
3.2. Data Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Guenther, G.; Arauz, A. Cerebral Venous Thrombosis: A Diagnostic and Treatment Update. Neurología 2011, 26, 488–498. [Google Scholar] [CrossRef]
- Saposnik, G.; Barinagarrementeria, F.; Brown, R.D.; Bushnell, C.D.; Cucchiara, B.; Cushman, M.; Deveber, G.; Ferro, J.M.; Tsai, F.Y. Diagnosis and Management of Cerebral Venous Thrombosis: A Statement for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 2011, 42, 1158–1192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bousser, M.G.; Ferro, J.M. Cerebral Venous Thrombosis: An Update. Lancet Neurol. 2007, 6, 162–170. [Google Scholar] [CrossRef]
- Canhão, P.; Ferro, J.M.; Lindgren, A.G.; Bousser, M.G.; Stam, J.; Barinagarrementeria, F. Causes and Predictors of Death in Cerebral Venous Thrombosis. Stroke 2005, 36, 1720–1725. [Google Scholar] [CrossRef] [Green Version]
- Stam, J. Thrombosis of the Cerebral Veins and Sinuses. N. Engl. J. Med. 2005, 352, 1791–1798. [Google Scholar] [CrossRef] [Green Version]
- Wagner, M.W.; Bosemani, T.; Oshmyansky, A.; Poretti, A.; Huisman, T.A.G.M. Neuroimaging Findings in Pediatric Cerebral Sinovenous Thrombosis. Child’s Nerv. Syst. 2015, 31, 705–712. [Google Scholar] [CrossRef]
- Poon, C.S.; Chang, J.K.; Swarnkar, A.; Johnson, M.H.; Wasenko, J. Radiologic Diagnosis of Cerebral Venous Thrombosis: Pictorial Review. Am. J. Roentgenol. 2007, 189, 64–75. [Google Scholar] [CrossRef] [PubMed]
- Leach, J.L.; Fortuna, R.B.; Jones, B.V.; Gaskill-Shipley, M.F. Imaging of Cerebral Venous Thrombosis: Current Techniques, Spectrum of Findings, and Diagnostic Pitfalls. Radiographics 2006, 26, 19–42. [Google Scholar] [CrossRef] [Green Version]
- Piazza, G. Cerebral Venous Thrombosis. Circulation 2012, 125, 1704–1709. [Google Scholar] [CrossRef] [Green Version]
- de la Vega Muns, G.; Quencer, R.; Ezuddin, N.S.; Saigal, G. Utility of Hounsfield Unit and Hematocrit Values in the Diagnosis of Acute Venous Sinus Thrombosis in Unenhanced Brain CTs in the Pediatric Population. Pediatric Radiol. 2019, 49, 234–239. [Google Scholar] [CrossRef]
- DeVeber, G.; Andrew, M.; Adams, C.; Bjornson, B.; Booth, F.; Buckley, D.J.; Camfield, C.S.; David, M.; Humphreys, P.; Langevin, P.; et al. Cerebral Sinovenous Thrombosis in Children. N. Engl. J. Med. 2001, 345, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Ferro, J.M.; Canhão, P.; Stam, J.; Bousser, M.G.; Barinagarrementeria, F. Prognosis of Cerebral Vein and Dural Sinus Thrombosis: Results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke 2004, 35, 664–670. [Google Scholar] [CrossRef] [Green Version]
- Roland, T.; Jacobs, J.; Rappaport, A.; Vanheste, R.; Wilms, G.; Demaerel, P. Unenhanced Brain CT Is Useful to Decide on Further Imaging in Suspected Venous Sinus Thrombosis. Clin. Radiol. 2010, 65, 34–39. [Google Scholar] [CrossRef]
- Linn, J.; Pfefferkorn, T.; Ivanicova, K.; Müller-Schunk, S.; Hartz, S.; Wiesmann, M.; Dichgans, M.; Brückmann, H. Noncontrast CT in Deep Cerebral Venous Thrombosis and Sinus Thrombosis: Comparison of Its Diagnostic Value for Both Entities. Am. J. Neuroradiol. 2009, 30, 728–735. [Google Scholar] [CrossRef]
- Pasquini, L.; Rossi Espagnet, M.C.; Napolitano, A.; Longo, D.; Bertaina, A.; Visconti, E.; Tomà, P. Dentate Nucleus T1 Hyperintensity: Is It Always Gadolinium All That Glitters? Radiol. Med. 2018, 123, 469–473. [Google Scholar] [CrossRef]
- Rossi Espagnet, M.C.; Bernardi, B.; Pasquini, L.; Figà-Talamanca, L.; Tomà, P.; Napolitano, A. Signal Intensity at Unenhanced T1-Weighted Magnetic Resonance in the Globus Pallidus and Dentate Nucleus after Serial Administrations of a Macrocyclic Gadolinium-Based Contrast Agent in Children. Pediatric Radiol. 2017, 47, 1345–1352. [Google Scholar] [CrossRef] [PubMed]
- Pasquini, L.; Napolitano, A.; Visconti, E.; Longo, D.; Romano, A.; Tomà, P.; Espagnet, M.C.R. Gadolinium-Based Contrast Agent-Related Toxicities. CNS Drugs 2018, 32, 229–240. [Google Scholar] [CrossRef]
- Faucon, A.L.; Bobrie, G.; Clément, O. Nephrotoxicity of Iodinated Contrast Media: From Pathophysiology to Prevention Strategies. Eur. J. Radiol. 2019, 116, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Bottino, F.; Lucignani, M.; Napolitano, A.; Dellepiane, F.; Visconti, E.; Espagnet, M.C.R.; Pasquini, L. In Vivo Brain Gsh: Mrs Methods and Clinical Applications. Antioxidants 2021, 10, 1407. [Google Scholar] [CrossRef]
- Fanous, R.; Leung, A.; Karlik, S. Quantitative Assessment of the Superior Sagittal Sinus on Unenhanced Computed Tomography. Eur. J. Radiol. 2010, 75, 336–342. [Google Scholar] [CrossRef]
- Al-Ryalat, N.T.; AlRyalat, S.A.S.; Malkawi, L.W.; Al-Zeena, E.F.; Najar, M.S.A.; Hadidy, A.M. Factors Affecting Attenuation of Dural Sinuses on Noncontrasted Computed Tomography Scan. J. Stroke Cerebrovasc. Dis. 2016, 25, 2559–2565. [Google Scholar] [CrossRef]
- Black, D.F.; Rad, A.E.; Gray, L.A.; Campeau, N.G.; Kallmes, D.F. Cerebral Venous Sinus Density on Noncontrast CT Correlates with Hematocrit. Am. J. Neuroradiol. 2011, 32, 1354–1357. [Google Scholar] [CrossRef] [Green Version]
- Buyck, P.J.; De Keyzer, F.; Vanneste, D.; Wilms, G.; Thijs, V.; Demaerel, P. CT Density Measurement and H:H Ratio Are Useful in Diagnosing Acute Cerebral Venous Sinus Thrombosis. Am. J. Neuroradiol. 2013, 34, 1568–1572. [Google Scholar] [CrossRef] [Green Version]
- Avsenik, J.; Oblak, J.P.; Popovic, K.S. Non-Contrast Computed Tomography in the Diagnosis of Cerebral Venous Sinus Thrombosis. Radiol. Oncol. 2016, 50, 263–268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alsafi, A.; Lakhani, A.; Carlton Jones, L.; Lobotesis, K. Cerebral Venous Sinus Thrombosis, a Nonenhanced CT Diagnosis? Radiol. Res. Pract. 2015, 2015, 581437. [Google Scholar] [CrossRef]
- Tayyebi, S.; Akhavan, R.; Shams, M.; Salehi, M.; Farrokh, D.; Yousefi, F.; Abbasi, B. Diagnostic Value of Non-Contrast Brain Computed Tomography in the Evaluation of Acute Cerebral Venous Thrombosis. Sci. Rep. 2020, 10, 883. [Google Scholar] [CrossRef]
- Besachio, D.A.; Quigley, E.P.; Shah, L.M.; Salzman, K.L. Noncontrast Computed Tomographic Hounsfield Unit Evaluation of Cerebral Venous Thrombosis: A Quantitative Evaluation. Neuroradiology 2013, 55, 941–945. [Google Scholar] [CrossRef] [PubMed]
- Zaheer, S.; Iancu, D.; Seppala, N.; Patro, S.; Glikstein, R.; Thornhill, R.E.; Lum, C. Quantitative Non-Contrast Measurements Improve Diagnosing Dural Venous Sinus Thrombosis. Neuroradiology 2016, 58, 657–663. [Google Scholar] [CrossRef]
- Buyck, P.J.; Zuurbier, S.M.; Garcia-Esperon, C.; Barboza, M.A.; Costa, P.; Escudero, I.; Renard, D.; Lemmens, R.; Hinteregger, N.; Fazekas, F.; et al. Diagnostic Accuracy of Noncontrast CT Imaging Markers in Cerebral Venous Thrombosis. Neurology 2019, 92, E841–E851. [Google Scholar] [CrossRef]
- Xu, W.; Gao, L.; Li, T.; Ramdoyal, N.D.; Zhang, J.; Shao, A. The Performance of CT versus MRI in the Differential Diagnosis of Cerebral Venous Thrombosis. Thromb. Haemost. 2018, 118, 1067–1077. [Google Scholar] [CrossRef] [PubMed]
- Ghoneim, A.; Straiton, J.; Pollard, C.; Macdonald, K.; Jampana, R. Imaging of Cerebral Venous Thrombosis. Clin. Radiol. 2020, 75, 254–264. [Google Scholar] [CrossRef] [PubMed]


| Thrombosis | Mean | Standard Deviation | p | ||
|---|---|---|---|---|---|
| CVST patients vs. no CVST patients | mean HU% relative difference | no | 9.4 | 3 | |
| yes | 24.1 | 8.9 | <0.001 | ||
| max HU% relative difference | no | 7.8 | 2.6 | ||
| yes | 21.2 | 7.8 | <0.001 | ||
| CVST adult patients vs. no CVST adult patients | mean HU% relative difference | no | 8.6 | 3.4 | |
| yes | 21.5 | 9.1 | <0.001 | ||
| max HU% relative difference | no | 7.6 | 3.1 | ||
| yes | 19.9 | 8.2 | <0.001 | ||
| CVST pediatric patients vs. no CVST pediatric patients | mean HU% relative difference | no | 9.8 | 2.7 | |
| yes | 28.1 | 7.2 | <0.001 | ||
| max HU% relative difference | no | 8 | 2.3 | ||
| yes | 23.3 | 6.3 | <0.001 |
| Mean % Relative Differences | Max % Relative Differences | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cut-Off | Sensitivity | Specificity | PPV | NPV | Cut-Off | Sensitivity | Specificity | PPV | NPV | |
| all patients | 12.97 | 96% | 0.92 | 92% | 89% | 10.14 | 96% | 90% | 88% | 86% |
| adult group | 12.97 | 94% | 95% | 92% | 90% | 10.14 | 94% | 95% | 92% | 90% |
| pediatric group | 15.52 | 100% | 100% | 100% | 100% | 12.91 | 100% | 100% | 100% | 100% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romano, A.; Rossi-Espagnet, M.C.; Pasquini, L.; Di Napoli, A.; Dellepiane, F.; Butera, G.; Moltoni, G.; Gagliardo, O.; Bozzao, A. Cerebral Venous Thrombosis: A Challenging Diagnosis; A New Nonenhanced Computed Tomography Standardized Semi-Quantitative Method. Tomography 2022, 8, 1-9. https://doi.org/10.3390/tomography8010001
Romano A, Rossi-Espagnet MC, Pasquini L, Di Napoli A, Dellepiane F, Butera G, Moltoni G, Gagliardo O, Bozzao A. Cerebral Venous Thrombosis: A Challenging Diagnosis; A New Nonenhanced Computed Tomography Standardized Semi-Quantitative Method. Tomography. 2022; 8(1):1-9. https://doi.org/10.3390/tomography8010001
Chicago/Turabian StyleRomano, Andrea, Maria Camilla Rossi-Espagnet, Luca Pasquini, Alberto Di Napoli, Francesco Dellepiane, Giulia Butera, Giulia Moltoni, Olga Gagliardo, and Alessandro Bozzao. 2022. "Cerebral Venous Thrombosis: A Challenging Diagnosis; A New Nonenhanced Computed Tomography Standardized Semi-Quantitative Method" Tomography 8, no. 1: 1-9. https://doi.org/10.3390/tomography8010001
APA StyleRomano, A., Rossi-Espagnet, M. C., Pasquini, L., Di Napoli, A., Dellepiane, F., Butera, G., Moltoni, G., Gagliardo, O., & Bozzao, A. (2022). Cerebral Venous Thrombosis: A Challenging Diagnosis; A New Nonenhanced Computed Tomography Standardized Semi-Quantitative Method. Tomography, 8(1), 1-9. https://doi.org/10.3390/tomography8010001







