The Importance of Correlation between CBCT Analysis of Bone Density and Primary Stability When Choosing the Design of Dental Implants—Ex Vivo Study
Abstract
1. Introduction
1.1. Osseointegration
- quantity and quality of bone tissue at the implant site,
- implant design, and
- surgical implantation technique [15].
1.2. Alveolar Bone
1.3. Application of CBCT
1.4. Implant Design
1.5. Primary Implant Stability
- Determine the correlation between the mean value of the bone density measured on the CBCT device and the primary stability of self-tapping and non-self-tapping dental implants determined by resonant frequency analysis on samples of pig ribs and a bovine femur;
- Compare the obtained values of primary stability on self-tapping and non-self-tapping implants installed on samples of pig ribs and bovine femur samples.
2. Materials and Methods
2.1. Experimental Animal Models
2.2. Implants Used in the Study
- self-tapping Bredent Narrow SKY (Bredent®, Weissenhorner Str. 2, 89250 Senden - Germany) dental implants, with the following dimensions: 3.5 × 10 mm, and
- non-self-tapping NobelReplace Conical Connection (Nobel Biocare, Nobel Biocare Services AG, P.O. Box, CH-8058 Zürich-Flughafen, Switzerland) with the following dimensions: 3.5 × 10 mm.
2.3. Individual Stent Fabrication
2.4. Radiographic Analysis of Bone Density
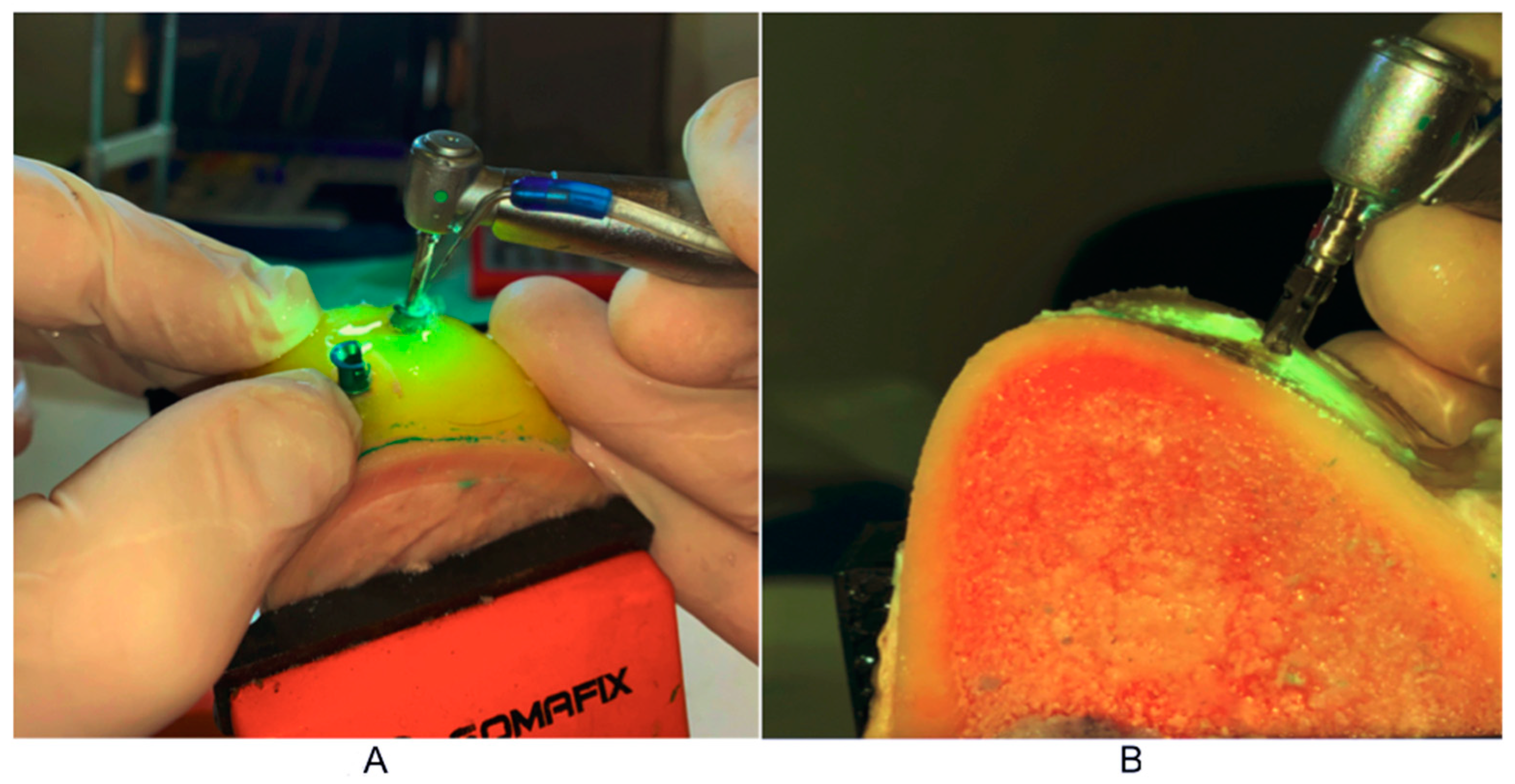
2.5. Procedure for Experimental Implant Placement
2.6. Primary Stability Measurement Procedure
2.7. Statistical Analysis
- Bone densities based on CBCT images in HU units;
- Primary stability of dental implants in ISQ units.
3. Results
4. Discussion
5. Conclusions
- By analyzing the density of the bone tissue in the CBCT images in the software of the device expressed in HU units, we cannot predict the degree of the primary stability of the non-self-tapping dental implants in bones of a lower quality D4, according to Misch, and Q4, according to Norton and Gamble;
- Self-tapping and non-self-tapping dental implants installed in D4- and Q4-quality bones do not show a significant statistical difference in the primary stability;
- By analyzing the density of the bone tissue in the CBCT images in the software of the device expressed in Hausfield units, we can predict the degree of the primary stability of the self-tapping dental implants in bones of the densities D1, D2 and Q1–Q3;
- By analyzing the density of the bone tissue in the CBCT images in the software of the device expressed in HU units, we can predict the degree of the primary stability of the non-self-tapping dental implants in bones of the densities D1, D2 and Q1–Q3.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barbato, P.R.; Nagano, H.C.M.; Zanchet, F.N.; Boing, A.F.; Peres, M.A. Tooth loss and associated socioeconomic, demographic, and dental-care factors in Brazilian adults: An analysis of the Brazilian Oral Health Survey, 2002–2003. Cad. Saude Publica 2007, 23, 1803–1814. [Google Scholar] [CrossRef] [PubMed]
- Moreira, C.H.C.; Zanatta, F.B.; Antoniazzi, R.P.; Meneguetti, P.C.; Rösing, C.K. Criteria adopted by dentists to indicate the extraction of periodontally involved teeth. J. Appl. Oral Sci. 2007, 15, 437–441. [Google Scholar] [CrossRef] [PubMed]
- Cahen, P.; Frank, R.; Turlot, J. A Survey of the Reasons for Dental Extractions in France. J. Dent. Res. 1985, 64, 1087–1093. [Google Scholar] [CrossRef] [PubMed]
- Ong, G.; Yeo, J.-F.; Bhole, S. A survey of reasons for extraction of permanent teeth in Singapore. Community Dent. Oral Epidemiol. 1996, 24, 124–127. [Google Scholar] [CrossRef]
- Nuvvula, S.; Chava, V.K.; Nuvvula, S. Primary culprit for tooth loss!! J. Indian Soc. Periodontol. 2016, 20, 222–224. [Google Scholar]
- Adell, R.; Lehholm, U.; Rockler, B.; Branemark, P.I. A I5-year study of osseointegrated implants in the treatment of the edentulous jaw. Int. J. Oral Surg. 1981, 10, 387–416. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Bone Quality and Quantity and Dental Implant Failure: A Systematic Review and Meta-analysis. Int. J. Prosthodont. 2017, 30, 219–237. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Dental implants inserted in male versus female patients: A systematic review and meta-analysis. J. Oral Rehabil. 2015, 42, 709–722. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Dental implants inserted in fresh extraction sockets versus healed sites: A systematic review and meta-analysis. J. Dent. 2015, 43, 16–41. [Google Scholar] [CrossRef]
- Vlahovic, Z.; Mikic, M. 3D Printing Guide Implant Placement:A Case Report. Balk. J. Dent. Med. 2017, 21, 65–68. [Google Scholar] [CrossRef][Green Version]
- Esposito, M.; Grusovin, M.G.; Polyzos, I.P.; Felice, P.; Worthington, H.V. Timing of implant placement after tooth extraction: Immediate, immediate-delayed or delayed implants? A Cochrane systematic review. Eur. J. Oral Implantol. 2010, 3, 189–205. [Google Scholar] [PubMed]
- Manivasagam, V.K.; Popat, K.C. Hydrothermally treated titanium surfaces for enhanced osteogenic differentiation of adipose derived stem cells. Mater. Sci. Eng. C 2021, 128, 112315. [Google Scholar] [CrossRef] [PubMed]
- Heinemann, F.; Hasan, I.; Bourauel, C.; Biffar, R.; Mundt, T. Bone stability around dental implants: Treatment related factors. Ann. Anat.-Anat. Anz. 2015, 199, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Sayed, M.E.; Mugri, M.H.; Almasri, M.A.; Al-Ahmari, M.M.; Bhandi, S.; Madapusi, T.B.; Varadarajan, S.; Raj, A.T.; Reda, R.; Testarelli, L.; et al. Role of Stem Cells in Augmenting Dental Implant Osseointegration: A Systematic Review. Coatings 2021, 11, 1035. [Google Scholar] [CrossRef]
- Al-Sabbagh, M.; Eldomiaty, W.; Khabbaz, Y. Can Osseointegration Be Achieved Without Primary Stability? Dent. Clin. North Am. 2019, 63, 461–473. [Google Scholar] [CrossRef]
- Punn, K.K.; Wong, F.H.W. Importance of measurement of bone density in the management of osteoporosis. Singap. Med. J. 1990, 31, 390–396. [Google Scholar]
- Krolo, I.; Zadravec, D. Dentalna radiologija. Zagreb Med. Nakl. 2016, 12, 197–212. [Google Scholar]
- Misch, C.E.; Kircos, L.T. Diagnostic imaging and techniques. In Contemporary Implant Dentistry, 2nd ed.; Misch, C.E., Ed.; Mosby: St. Louis, MO, USA, 1999; pp. 73–87. [Google Scholar]
- Norton, R.M.; Gamble, C. Bone classification: An objective scale of bone density using the computerized tomography scan. Clin. Oral Implant. Res. 2001, 12, 79–84. [Google Scholar] [CrossRef]
- Tsiklakis, K.; Donta, C.; Gavala, S.; Karayianni, K.; Kamenopoulou, V.; Hourdakis, C.J. Dose reduction in maxillofacial imaging using low dose Cone Beam CT. Eur. J. Radiol. 2005, 56, 413–417. [Google Scholar] [CrossRef]
- Alaqeely, R.; Babay, N.; AlQutub, M. Dental implant primary stability in different regions of the Jawbone: CBCT-based 3D finite element analysis. Saudi Dent. J. 2020, 32, 101–107. [Google Scholar] [CrossRef]
- Vyas, R.; Talluri, S.; Vaddamanu, S.K.; Apparaju, V.; Ahuja, S.; Kanji, M.A. Evaluating cortico-cancellous ratio using virtual implant planning and its relation with immediate and long-term stability of a dental implant—A CBCT-assisted prospective observational clinical study. Niger. J. Clin. Pract. 2019, 22, 982–987. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Choudhary, K.; Nagi, R.; Shukla, S.; Kaur, N.; Grover, D. New evolution of cone-beam computed tomography in dentistry: Combining digital technologies. Imaging Sci. Dent. 2019, 49, 179–190. [Google Scholar] [CrossRef] [PubMed]
- Tanimoto, H.; Arai, Y. The effect of voxel size on image reconstruction in cone-beam computed tomography. Oral Radiol. 2009, 25, 149–153. [Google Scholar] [CrossRef]
- Jacobs, R.; Salmon, B.; Codari, M.; Hassan, B.; Bornstein, M.M. Cone beam computed tomography in implant dentistry: Recommendations for clinical use. BMC Oral Health 2018, 18, 88. [Google Scholar] [CrossRef]
- Quereshy, F.A.; Savell, T.A.; Palomo, J.M. Applications of Cone Beam Computed Tomography in the Practice of Oral and Maxillofacial Surgery. J. Oral Maxillofac. Surg. 2008, 66, 791–796. [Google Scholar] [CrossRef]
- Bogaerde, L.V.; Pedretti, G.; Sennerby, L.; Meredith, N. Immediate/Early Function of Neoss Implants Placed in Maxillas and Posterior Mandibles: An 18-Month Prospective Case Series Study. Clin. Implant. Dent. Relat. Res. 2010, 12, e83–e94. [Google Scholar] [CrossRef]
- Sennerby, L.; Andersson, P.; Verrocchi, D.; Viinamaki, R. One-year outcomes of Neoss bimodal implants. A prospective clinical, radiographic, and RFA study. Clin. Implant. Dent. Relat. Res. 2012, 14, 313–320. [Google Scholar] [CrossRef]
- Tantanapornkul, W.; Okouchi, K.; Fujiwara, Y.; Yamashiro, M.; Maruoka, Y.; Ohbayashi, N.; Kurabayashi, T. A comparative study of conebeam computed tomography and conventional panoramic radiography in assessing the topographic correlation between the mandibular canal and impacted third molars. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 103, 253–259. [Google Scholar] [CrossRef]
- Osorio, F.; Perilla, M.; Doyle, D.J.; Palomo, J.M. Cone Beam Computed Tomography: An Innovative Tool for Airway Assessment. Anesth. Analg. 2008, 106, 1803–1807. [Google Scholar] [CrossRef]
- Fokas, G.; Vaughn, V.M.; Scarfe, W.C.; Bornstein, M.M. Accuracy of linear measurements on CBCT images related to presurgical implant treatment planning: A systematic review. Clin. Oral Implant. Res. 2018, 29, 393–415. [Google Scholar] [CrossRef]
- Mozzo, P.; Procacci, C.; Tacconi, A.; Martini, P.T.; Andreis, I.A.B. A new volumetric CT machine for dental imaging based on the cone-beam technique: Preliminary results. Eur. Radiol. 1998, 8, 1558–1564. [Google Scholar] [CrossRef] [PubMed]
- Gaviria, L.; Salcido, J.P.; Guda, T.; Ong, J.L. Current trends in dental implants. J. Korean Assoc. Oral Maxillofac. Surg. 2014, 40, 50–60. [Google Scholar] [CrossRef] [PubMed]
- de Andrade, C.L.; Carvalho, M.A.; Bordin, D.; da Silva, W.J.; Del Bel Cury, A.A.; Sotto-Maior, B.S. Biomechanical Behavior of the Dental Implant Macrodesign. Int. J. Oral Maxillofac. Implant. 2017, 32, 264–270. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.P.; Lu, S.H.; Zhu, J.X.; Hu, H.C.; Yue, Z.G.; Tang, Z.H. Influence of thread shapes of custo made root-analogue implants on stress distribution of peri-implant bone: A three-dimensional finite element analysis. Beijing Da Xue Xue Bao Yi Xue Ban 2019, 51, 1130–1137. [Google Scholar] [PubMed]
- Bavetta, G.; Bavetta, G.; Randazzo, V.; Cavataio, A.; Paderni, C.; Grassia, V.; Dipalma, G.; Isacco, C.G.; Scarano, A.; De Vito, D.; et al. A Retrospective Study on Insertion Torque and Implant Stability Quotient (ISQ) as Stability Parameters for Immediate Loading of Implants in Fresh Extraction Sockets. BioMed Res. Int. 2019, 2019, 9720419. [Google Scholar] [CrossRef]
- Meredith, N.; Alleyne, D.; Cawley, P. Quantitative determination of the stability of the implant–tissue interface using re-so-nance frequency analysis. Clin. Oral Implant. Res. 1996, 7, 261–267. [Google Scholar] [CrossRef]
- Noaman, A.T.; Bede, S.Y. The Effect of Bone Density Measured by Cone Beam Computed Tomography and Implant Dimensions on the Stability of Dental Implants. J. Craniofacial Surg. 2021. epub ahead of print. [Google Scholar] [CrossRef]
- Hakim, S.G.; Glanz, J.; Ofer, M.; Steller, D.; Sieg, P. Correlation of cone beam CT-derived bone density parameters with primary implant stability assessed by peak insertion torque and periotest in the maxilla. J. Cranio-Maxillofac. Surg. 2019, 47, 461–467. [Google Scholar] [CrossRef]
- Al-Jamal, M.F.J.; Al-Jumaily, H.A. Can the Bone Density Estimated by CBCT Predict the Primary Stability of Dental Implants? A New Measurement Protocol. J. Craniofacial Surg. 2021, 32, e171–e174. [Google Scholar] [CrossRef]
- Cummaudo, M. Histomorphometric analysis of osteocyte lacunae in human and pig: Exploring its potential forspecies discrimination. Int. J. Leg. Med. 2019, 133, 711–718. [Google Scholar] [CrossRef]
- González-Garcia, R.; Monje, F.; Moreno-Garcia, C. Predictability of the resonance frequency analysis in the survival of dental implants placed in the anterior non-atrophied edentulous mandible. Med. Oral Patol. Oral Cir. Bucal. 2011, 16, 664–669. [Google Scholar] [CrossRef] [PubMed]
- Petersson, A.; Sennerby, L. On standard calibration of ISQ transducer pegs. Integr. Diagn. Update 2016, 1, 1–3. [Google Scholar]
- Jaramillo, R.; Santos, R.; Lázaro, P.; Romero, M.; Rios-Santos, J.V.; Bullón, P.; Fernández-Palacín, A.; Herrero-Climent, M. Comparative analysis of 2 resonance frequency measurement devices: Osstell Mentor and Osstell ISQ. Implant. Dent. 2014, 23, 351–356. [Google Scholar] [CrossRef] [PubMed]
- Karabuda, Z.C.; Arιsan, V.; Abdel-Haq, J. Stability, marginal bone loss and survival of standard and modified sand-blasted, acid-etched implants in bilateral edentulous spaces: A prospective 15-month evaluation. Clin. Oral Implant. Res. 2011, 22, 840–849. [Google Scholar] [CrossRef]
- Kim, S.H.; Kim, S.J.; Lee, K.W.; Han, D.H. The effects of local factorson the survival rate of dental implants: A 19 year retrospective study. J. Korean Acad. Prosthodont. 2010, 48, 28–40. [Google Scholar] [CrossRef]
- Esposito, M.; Grusovin, M.G.; Coulthard, P.; Thomsen, P.; Worthington, H.V. A 5-year follow-up comparative analysis of the efficacy of various osseointegrated dental implant systems: A systematic review of randomized controlled clinical trials. Int. J. Oral Maxillofac. Implant. 2005, 20, 557–568. [Google Scholar]
- Renouard, F.; Nisand, D. Impact of implant length and diameter on survival rates. Clin. Oral Implant. Res. 2006, 17, 35–51. [Google Scholar] [CrossRef]
- Arsalanloo, Z.; Telchi, R.; Osgouie, K.G. Optimum Selection of the Dental Implants according to Length and Diameter Parameters by FE Method in the Anterior Position. Int. J. Biosci. Biochem. Bioinform. 2014, 4, 265–269. [Google Scholar] [CrossRef][Green Version]
- Busenlechner, D.; Fürhauser, R.; Haas, R.; Watzek, G.; Mailath, G.; Pommer, B. Long-term implant success at the academy for oral implantology: 8- year follow-up and risk factor analysis. J. Periodontal. Implant. Sci. 2014, 44, 102–108. [Google Scholar] [CrossRef]
- Yesildal, R.; Karabudak, F.; Bayındır, F.; Zamanlou, H.; Yıldırım, M.P.; Sağsöz, N.P.; Şen, S. Effect of implant diameter and length on stress distribution for titanium and zirconia implants by using finite element analysis (FEA). Open Access Libr. J. 2015, 2, 1–7. [Google Scholar] [CrossRef]
- Philip, J.M.; Abraham, H.M.; Jain, A.R.; Venkatakrishnan, C. The effect of implant and abutment diameter on peri-implant bone stress: A three-dimensional finite element analysis. J. Oral Res. Rev. 2016, 8, 49–52. [Google Scholar] [CrossRef]
- Omami, G.; Al Yafi, F. Should Cone Beam Computed Tomography Be Routinely Obtained in Implant Planning? Dent. Clin. N. Am. 2019, 63, 363–379. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, R.T. Acceptability of Cone Beam CT vs. Multi-Detector CT for 3D Anatomic Model Construction. J. Oral Maxillofac. Surg. 2006, 64, 37. [Google Scholar] [CrossRef]
- Arisan, V.; Karabuda, Z.C.; Avsever, H.; Özdemir, T. Conventional Multi-Slice Computed Tomography (CT) and Cone-Beam CT (CBCT) for Computer-Assisted Implant Placement. Part I: Relationship of Radiographic Gray Density and Implant Stability. Clin. Implant. Dent. Relat. Res. 2013, 15, 893–906. [Google Scholar] [CrossRef] [PubMed]
- Wada, M.; Tsuiki, Y.; Suganami, T.; Ikebe, K.; Sogo, M.; Okuno, I.; Maeda, Y. The correlation between the bone characters obtained by CBCT and primary stability of the implants. Int. J. Implant. Dent. 2015, 1, 1–7. [Google Scholar] [CrossRef]
- Molen, A.D. Considerations in the use of cone-beam computed tomography for buccal bone measurements. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 130–135. [Google Scholar] [CrossRef]
- Bilhan, H.; Bilmenoglu, C.; Urgun, A.C.; Ates, G.; Bural, C.; Cilingir, A.; Geckili, O. Comparison of the Primary Stability of Two Implant Designs in Two Different Bone Types: An In Vitro Study. Int. J. Oral Maxillofac. Implant. 2015, 30, 1036–1040. [Google Scholar] [CrossRef]
- Falco, A.; Berardini, M.; Trisi, P. Correlation Between Implant Geometry, Implant Surface, Insertion Torque, and Primary Stability: In Vitro Biomechanical Analysis. Int. J. Oral Maxillofac. Implant. 2018, 33, 824–830. [Google Scholar] [CrossRef]
- Cochran, D.; Stavropoulos, A.; Obrecht, M.; Pippenger, B.; Dard, M. A Comparison of Tapered and Nontapered Implants in the Minipig. Int. J. Oral Maxillofac. Implant. 2016, 31, 1341–1347. [Google Scholar] [CrossRef]
- Norton, M.R. The Influence of Low Insertion Torque on Primary Stability, Implant Survival, and Maintenance of Marginal Bone Levels: A Closed-Cohort Prospective Study. Int. J. Oral Maxillofac. Implant. 2017, 32, 849–857. [Google Scholar] [CrossRef]
- Schliephake, H.; Rödiger, M.; Phillips, K.; McGlumphy, E.A.; Chacon, G.E.; Larsen, P. Early loading of surface modified implants in the posterior mandible—5 year results of an open prospective non-controlled study. J. Clin. Periodontol. 2012, 39, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Abuhussein, H.; Pagni, G.; Rebaudi, A.; Wang, H.L. Effect of thread pattern upon implant osseointegration. Clin. Oral Impl. Res. 2010, 21, 129–136. [Google Scholar] [CrossRef] [PubMed]
- McCullough, J.J.; Klokkevold, P.R. The effect of implant macro-thread design on implant stability in the early post-operative period: A randomized, controlled pilot study. Clin. Oral Implant. Res. 2017, 28, 1218–1226. [Google Scholar] [CrossRef] [PubMed]
- Isoda, K.; Ayukawa, Y.; Tsukiyama, Y.; Sogo, M.; Matsushita, Y.; Koyano, K. Correlation between the bone density estimated by cone-beam computed tomography and the primary stability of dental implants. Clin. Oral Implant. Res. 2012, 23, 832–836. [Google Scholar] [CrossRef] [PubMed]
- Möhlhenrich, S.C.; Heussen, N.; Winterhalder, P.; Prescher, A.; Hölzle, F.; Modabber, A.; Wolf, M.; Kniha, K. Predicting primary stability of orthodontic mini-implants, according to position, screw-size, and bone quality, in the maxilla of aged patients: A cadaveric study. Eur. J. Oral Sci. 2019, 127, 462–471. [Google Scholar] [CrossRef] [PubMed]
- Marquezan, M.; Osório, A.; Sant’Anna, E.; Souza, M.M.; Maia, L. Does bone mineral density influence the primary stability of dental implants? A systematic review. Clin. Oral Implant. Res. 2012, 23, 767–774. [Google Scholar] [CrossRef]
- Fuster-Torres, M.A.; Peñarrocha-Diago, M.; Peñarrocha-Oltra, D. Correlations Between Bone Density Values from Cone Beam Computed Tomography, Maximum Insertion Torque, and Resonance Frequency Analysis at Implant Placement: A Pilot Study. Int. J. Oral Maxillofac. Implant. 2011, 26, 1051–1056. [Google Scholar]






| HU | n | sd | Med | Min | Max | |
|---|---|---|---|---|---|---|
| Bovine femur | 40 | 851.8 | 193.0 | 827.2 | 422.9 | 1236.9 |
| Pig rib | 40 | 255.7 | 66.1 | 254.1 | 99.7 | 388.6 |
| ISQ | n | sd | Med | Min | Max | |
|---|---|---|---|---|---|---|
| Self-tapping | 20 | 68.2 | 3.8 | 68.0 | 59.0 | 73.0 |
| Non-self-tapping | 20 | 67.0 | 4.5 | 68.5 | 54.0 | 72.0 |
| ISQ | n | sd | Med | Min | Max | |
|---|---|---|---|---|---|---|
| Self-tapping | 20 | 75.8 | 3.4 | 76.0 | 69.0 | 82.0 |
| Non-self-tapping | 20 | 74.2 | 3.9 | 75.0 | 66.0 | 80.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mikic, M.; Vlahovic, Z.; Stevanović, M.; Arsic, Z.; Mladenovic, R. The Importance of Correlation between CBCT Analysis of Bone Density and Primary Stability When Choosing the Design of Dental Implants—Ex Vivo Study. Tomography 2022, 8, 1293-1306. https://doi.org/10.3390/tomography8030107
Mikic M, Vlahovic Z, Stevanović M, Arsic Z, Mladenovic R. The Importance of Correlation between CBCT Analysis of Bone Density and Primary Stability When Choosing the Design of Dental Implants—Ex Vivo Study. Tomography. 2022; 8(3):1293-1306. https://doi.org/10.3390/tomography8030107
Chicago/Turabian StyleMikic, Mirko, Zoran Vlahovic, Momir Stevanović, Zoran Arsic, and Rasa Mladenovic. 2022. "The Importance of Correlation between CBCT Analysis of Bone Density and Primary Stability When Choosing the Design of Dental Implants—Ex Vivo Study" Tomography 8, no. 3: 1293-1306. https://doi.org/10.3390/tomography8030107
APA StyleMikic, M., Vlahovic, Z., Stevanović, M., Arsic, Z., & Mladenovic, R. (2022). The Importance of Correlation between CBCT Analysis of Bone Density and Primary Stability When Choosing the Design of Dental Implants—Ex Vivo Study. Tomography, 8(3), 1293-1306. https://doi.org/10.3390/tomography8030107







