A Systematic Review of Cementation Techniques to Minimize Cement Excess in Cement-Retained Implant Restorations
Abstract
:1. Introduction
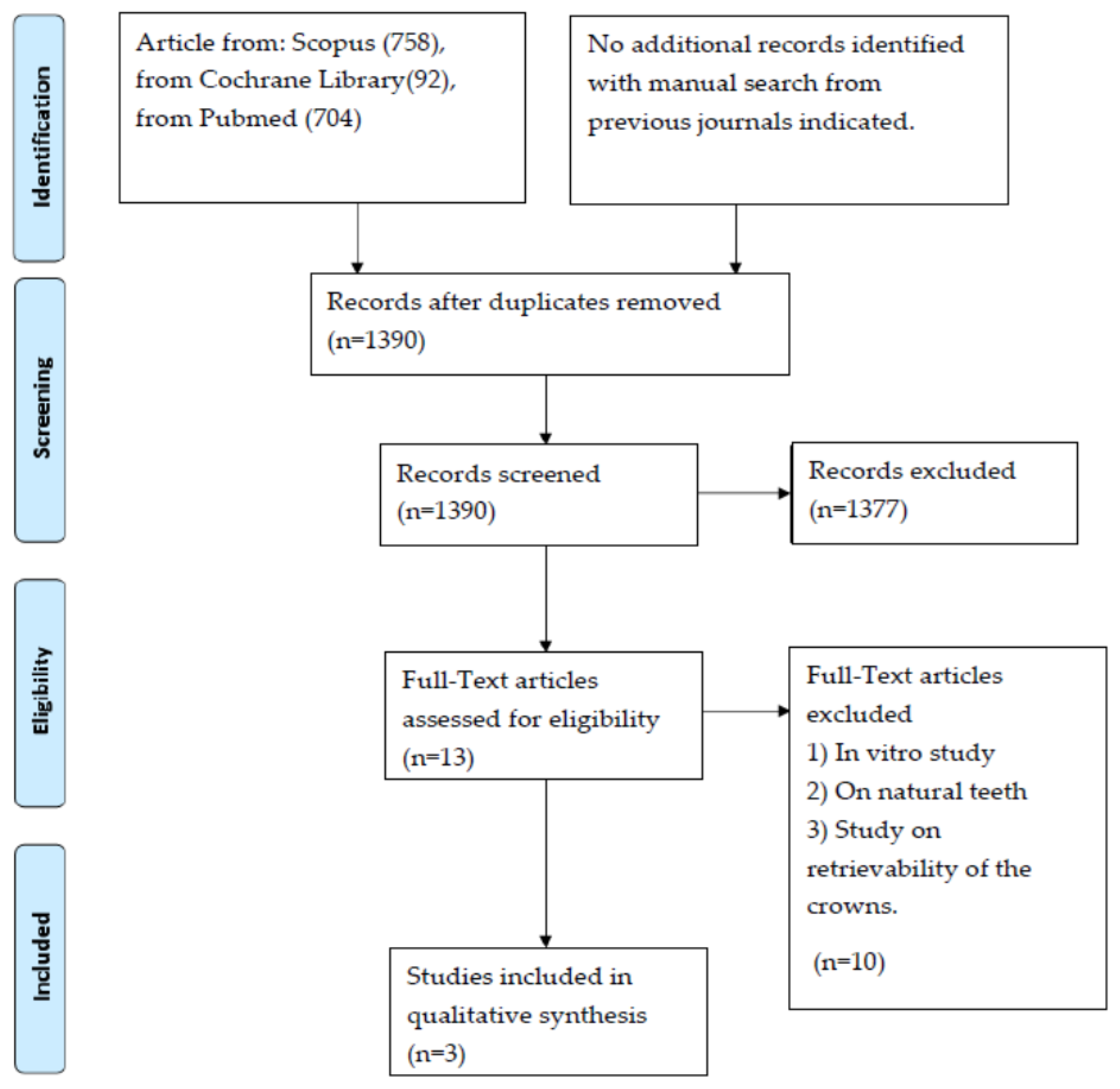
2. Materials and Methods
3. Results
4. Discussion
4.1. Cement Excess
4.2. Type of Cement Used
4.3. Cementation Technique
4.4. Prosthetic Finish Line
4.5. Cement Residues Visualization
5. Conclusions
- All the three studies evaluated in this review conclude that a small amount of cement residue is found in the gingival sulcus;
- The use of eugenol-free oxide cement made it possible to find no residues in the soft tissues but only in adhesion to the implant and prosthetic components;
- Pathologies caused by excess cement are low;
- Resinous cements should be considered, due to the free monomers present in them, toxic for the soft tissues;
- The provisional zinc-oxide cements, also eugenol-free, seem to represent the ideal choice to be brought into solution in oral fluids, as they are easily recognizable in intraoral radiography, are easily removed, and allow easier removal of prosthetic restorations, unlike definitive cements;
- The different grades of retentive forces provided by these cements do not seem to have a clinical effect on the decementation of the restorations.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Wittneben, J.G.; Joda, T.; Weber, H.P.; Brägger, U. Screw retained vs. cement retained implant-supported fixed dental prosthesis. Periodontology 2017, 73, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Wittneben, J.G.; Millen, C.; Brägger, U. Clinical Performance of Screw-Versus Cement-Retained Fixed Implant-Supported Reconstructions-A Systematic Review. Int. J. Oral Maxillofac. Implant. 2014, 29, 84–98. [Google Scholar] [CrossRef] [Green Version]
- Alraheam, I.A.; Ngoc, C.N.; Wiesen, C.A.; Dds, T.E.D. Five-year success rate of resin-bonded fixed partial dentures: A systematic review. J. Esthet. Restor. Dent. 2018, 31, 40–50. [Google Scholar] [CrossRef] [Green Version]
- Misch, C.E. Screw-retained versus cement-retained implant-supported prostheses. Pract. Periodont. Aesthet. Dent. 1995, 7, 15–18. [Google Scholar]
- Chee, W.W.; Duncan, J.; Afshar, M.; Moshaverinia, A. Evaluation of the amount of excess cement around the margins of cement-retained dental implant restorations: The effect of the cement application method. J. Prosthet. Dent. 2013, 109, 216–221. [Google Scholar] [CrossRef]
- Tribst, J.P.M.; Piva, A.M.D.O.D.; Penteado, M.M.; Borges, A.L.S.; Bottino, M.A. Influence of ceramic material, thickness of restoration and cement layer on stress distribution of occlusal veneers. Braz. Oral Res. 2018, 32, e118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tabata, L.F.; Assunção, W.G.; Barão, V.A.R.; de Sousa, E.A.C.; Gomes, É.A.; Delben, J.A. Implant platform switching: Biomechanical approach using two-dimensional finite element analysis. J. Craniofacial Surg. 2010, 21, 182–187. [Google Scholar] [CrossRef]
- Passaretti, A.; Petroni, G.; Miracolo, G.; Savoia, V.; Perpetuini, A.; Cicconetti, A. Metal free, full arch, fixed prosthesis for edentulous mandible rehabilitation on four implants. J. Prosthodont. Res. 2018, 62, 264–267. [Google Scholar] [CrossRef] [PubMed]
- Sinjari, B.; D’Addazio, G.; Traini, T.; Varvara, G.; Scarano, A.; Murmura, G.; Caputi, S. A 10-year retrospective comparative human study on screw-retained versus cemented dental implant abutments. J. Biol. Regul. Homeost. Agents 2019, 33, 787–797. [Google Scholar]
- Scarano, A.; Murmura, G.; Sinjiari, B.; Sollazzo, V.; Spinelli, G.; Carinci, F. Analysis and Structural Examination of Screw Loosening in Oral Implants. Int. J. Immunopathol. Pharmacol. 2011, 24 (Suppl. 2), 77–81. [Google Scholar] [CrossRef]
- Camatta, H.P.; Ferreira, R.M.; Ferrairo, B.M.; Strelhow, S.S.; Rubo, J.H.; Mori, A.A.; Ferruzzi, F. Mechanical Behavior and Fracture Loads of Screw-Retained and Cement-Retained Lithium Disilicate Implant-Supported Crowns. J. Prosthodont. 2020, 30, 690–697. [Google Scholar] [CrossRef]
- Apaza Alccayhuaman, K.A.; Soto-Peñaloza, D.; Nakajima, Y.; Papageorgiou, S.N.; Botticelli, D.; Lang, N.P. Biological and technical complications of tilted implants in comparison with straight implants supporting fixed dental prostheses. A systematic review and meta-analysis. Clin. Oral Implant. Res. 2018, 29, 295–308. [Google Scholar] [CrossRef]
- Pesce, P.; Canullo, L.; Grusovin, M.G.; De Bruyn, H.; Cosyn, J.; Pera, P. Systematic review of some prosthetic risk factors for periimplantitis. J. Prosthet. Dent. 2015, 114, 346–350. [Google Scholar] [CrossRef] [PubMed]
- Staubli, N.; Walter, C.; Schmidt, J.C.; Weiger, R.; Zitzmann, N.U. Excess cement and the risk of peri-implant disease—A systematic review. Clin. Oral Implant. Res. 2016, 28, 1278–1290. [Google Scholar] [CrossRef] [PubMed]
- Almehmadi, N.; Kutkut, A.; Al-Sabbagh, M. What is the Best Available Luting Agent for Implant Prosthesis? Dent. Clin. 2019, 63, 531–545. [Google Scholar] [CrossRef]
- Nematollahi, F.; Beyabanaki, E.; Alikhasi, M. Cement Selection for Cement-Retained Implant-Supported Prostheses: A Literature Review. J. Prosthodont. 2015, 25, 599–606. [Google Scholar] [CrossRef]
- Canullo, L.; Cocchetto, R.; Marinotti, F.; Penarrocha-Oltra, D.; Diago, M.P.; Loi, I. Clinical evaluation of an improved cementation technique for implant-supported restorations: A randomized controlled trial. Clin. Oral Implant. Res. 2015, 27, 1492–1499. [Google Scholar] [CrossRef] [PubMed]
- Linkevicius, T.; Puisys, A.; Vindasiute, E.; Linkeviciene, L.; Apse, P. Does residual cement around implant-supported restorations cause peri-implant disease? A retrospective case analysis. Clin. Oral Implant. Res. 2012, 24, 1179–1184. [Google Scholar] [CrossRef]
- Linkevicius, T.; Puisys, A.; Steigmann, M.; Vindasiute, E.; Linkeviciene, L. Influence of Vertical Soft Tissue Thickness on Crestal Bone Changes Around Implants with Platform Switching: A Comparative Clinical Study. Clin. Implant Dent. Relat. Res. 2014, 17, 1228–1236. [Google Scholar] [CrossRef]
- Vindasiute, E.; Puisys, A.; Maslova, N.; Linkeviciene, L.; Peciuliene, V.; Linkevicius, T. Clinical Factors Influencing Removal of the Cement Excess in Implant-Supported Restorations. Clin. Implant Dent. Relat. Res. 2013, 17, 771–778. [Google Scholar] [CrossRef] [PubMed]
- Linkevicius, T.; Vindasiute, E.; Puisys, A.; Peciuliene, V. The influence of margin location on the amount of undetected cement excess after delivery of cement-retained implant restorations. Clin. Oral Implant. Res. 2011, 22, 1379–1384. [Google Scholar] [CrossRef] [PubMed]
- Sancho-Puchades, M.; Crameri, D.; Özcan, M.; Sailer, I.; Jung, R.E.; Hämmerle, C.H.F.; Thoma, D.S. The influence of the emergence profile on the amount of undetected cement excess after delivery of cement-retained implant reconstructions. Clin. Oral Implant. Res. 2017, 28, 1515–1522. [Google Scholar] [CrossRef] [Green Version]
- Frisch, E.; Ratka-Kruger, P.; Weigl, P.; Woelber, J. Extraoral cementation technique to minimize cement-associated Peri-implant marginal bone loss: Can a thin layer of zinc oxide cement provide sufficient retention. Int. J. Prosthodont. 2016, 29, 360–362. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Behr, M.; Spitzer, A.; Preis, V.; Weng, D.; Gosau, M.; Rosentritt, M. The extent of luting agent remnants on titanium and zirconia abutment analogs after scaling. Int. J. Oral Maxillofac. Implant. 2014, 29, 1185–1192. [Google Scholar] [CrossRef] [Green Version]
- Frisch, E.; Ratka-Krüger, P.; Weigl, P.; Woelber, J. Minimizing excess cement in implant-supported fixed restorations using an extraoral replica technique: A prospective 1-year study. Int. J. Oral Maxillofac. Implant. 2015, 30, 1355–1361. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kıran, B.; Toman, M.; Buduneli, N.; Lappin, D.F.; Toksavul, S.; Nizam, N. Intraoral versus extraoral cementation of implant-supported single crowns: Clinical, biomarker, and microbiological comparisons. Clin. Implant Dent. Relat. Res. 2017, 20, 170–179. [Google Scholar] [CrossRef] [PubMed]
- Wadhwani, C.; Piñeyro, A.; Hess, T.; Zhang, H.; Chung, K.-H. Effect of implant abutment modification on the extrusion of excess cement at the crown-abutment margin for cement-retained implant restorations. Int. J. Oral Maxillofac. Implant. 2011, 26, 1241–1246. [Google Scholar]
- Schwarz, S.; Schröder, C.; Corcodel, N.; Hassel, A.J.; Rammelsberg, P. Retrospective Comparison of Semipermanent and Permanent Cementation of Implant-Supported Single Crowns and FDPs with Regard to the Incidence of Survival and Complications. Clin. Implant Dent. Relat. Res. 2011, 14 (Suppl. 1), e151–e158. [Google Scholar] [CrossRef] [PubMed]
- Schiessl, C.; Schaefer, L.; Winter, C.; Fuerst, J.; Rosentritt, M.; Zeman, F.; Behr, M. Factors determining the retentiveness of luting agents used with metal- and ceramic-based implant components. Clin. Oral Investig. 2012, 17, 1179–1190. [Google Scholar] [CrossRef]
- Korsch, M.; Walther, W.; Marten, S.M.; Obst, U. Microbial analysis of biofilms on cement surfaces: An investigation in cement-associated peri-implantitis. J. Appl. Biomater. Funct. Mater. 2014, 12, 70–80. [Google Scholar] [CrossRef]
- Raval, N.C.; Wadhwani, C.P.; Jain, S.; Darveau, R.P. The interaction of implant luting cements and oral bacteria linked to peri-implant disease: An in vitro analysis of planktonic and biofilm growth–a preliminary study. Clin. Implant Dent. Relat. Res. 2015, 17, 1029–1035. [Google Scholar] [CrossRef]
- Guarnieri, R.; Miccoli, G.; Reda, R.; Mazzoni, A.; Di Nardo, D.; Testarelli, L. Laser microgrooved vs. machined healing abutment disconnection/reconnection: A comparative clinical, radiographical and biochemical study with split-mouth design. Int. J. Implant Dent. 2021, 7, 19. [Google Scholar] [CrossRef] [PubMed]
- Guarnieri, R.; Di Nardo, D.; Di Giorgio, G.; Miccoli, G.; Testarelli, L. Evaluation of peri-implant tissues condition after 10–15 years of loading in treated chronic periodontitis patients attending a private practice setting: A retrospective study. Clin. Oral Implant. Res. 2021, 32, 422–436. [Google Scholar] [CrossRef] [PubMed]
- Guarnieri, R.; Miccoli, G.; Reda, R.; Mazzoni, A.; Di Nardo, D.; Testarelli, L. Sulcus fluid volume, IL-6, and Il-1b concentrations in periodontal and peri-implant tissues comparing machined and laser-microtextured collar/abutment surfaces during 12 weeks of healing: A split-mouth RCT. Clin. Oral Implant. Res. 2021, 33, 94–104. [Google Scholar] [CrossRef]
- Cocchetto, R.; Canullo, L. The “hybrid abutment”: A new design for implant cemented restorations in the esthetic zones. Int. J. Esthet. Dent. 2015, 10, 186–208. [Google Scholar] [PubMed]
- Scutellà, F.; Weinstein, T.; Lazzara, R.; Testori, T. Buccolingual implant position and vertical abutment finish line geometry: Two strictly related factors that may influence the implant esthetic outcome. Implant Dent. 2015, 24, 343–348. [Google Scholar] [CrossRef]
- Kurt, A.; Altintas, S.H.; Kiziltas, M.V.; Tekkeli, S.E.; Guler, E.M.; Kocyigit, A.; Usumez, A. Evaluation of residual monomer release and toxicity of self-adhesive resin cements. Dent. Mater. J. 2018, 37, 40–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Search Algorithm | Database | Results |
|---|---|---|
| ((((cementation) OR (cementing)) AND ((technique) OR (method))) AND ((cement) OR (luting agent))) AND (excess). | Scopus | 758 |
| ((((cementation) OR (cementing)) AND ((technique) OR (method))) AND ((cement) OR (luting agent))) AND (excess). | Cochrane Library | 92 |
| ((((cementation) OR (cementing)) AND ((technique) OR (method))) AND ((cement) OR (luting agent))) AND (excess). | Pubmed | 704 |
| Studies | Year | Sample Size | Sample Characteristics (and Follow-Up) | Implant Type | Implant Subgingival Location | Type of Prostheses | Type of Cementation | Type of Cement | Type of Cement Remotion | Cement Remnants Analysis |
|---|---|---|---|---|---|---|---|---|---|---|
| Kiran et al. | 2017 | 12 patients 24 implants | Bilateral-single tooth gap (extraction no later than 6 months before), presence of M-D teeth, -------- Follow up 6 months | Locking taper connection (this allows the crown to be extraorally cemented without drilling it to connect it to the implant) | 1 mm subgingival (abutment with shoulder preparation) | Metal ceramic crown | Extraoral (abutment with locking taper connection) - Intraoral | Zinc Polycarboxylate | Not Described | X-ray periapical radiograph long-cone paralleling technique |
| Canullo et al. | 2015 | 46 patients 90 implants | 2 adjacent implants posterior maxilla ----------- Follow up 3 months | Screwed Abutment 8–12° of convergence | 1.5 mm subgingival (abutment with shoulder or with feath er edge) | Metal ceramic crown (with occlusal opening closed with composite resin) | Extraoral Intraoral Thin layer of Vaseline around the external margin, cement positioned with micro brush, polyurethane resin replica | Eugenol free Zinc Oxide cement | Stainless steel explorer + ultrasonic plastic tip + superfloss (using magnifying loops) | Optical light microscope analysis of the occupied surface by cement remnants |
| Frisch et al. | 2015 | 68 patients 92 implants | Variable anatomical distribution, single crown Surgery performed in the same center. ---- Follow-up 12 months | Screwed abutment | 1.5 mm subgingival (abutment with shoulder preparation) | Metal ceramic crown | Extraoral Intraoral Resin replica of the internal crown side | Zinc oxide cement | Extraoral From Replica with synthetic pellets. Intraoral Dental probe only. | X-ray periapical radiographs Long-cone paralleling technique |
| Studies | Random Sequence Generation | Allocation Concealment | Blinding of Participants and Personnel | Blinding of Outcome Assessment | Incomplete Outcome Data | Selective Reporting |
|---|---|---|---|---|---|---|
| Kiran et al. 2017 | Low | Low | High | High | Low | Low |
| Canullo et al. 2015 | Low | Low | High | High | Low | Low |
| Frisch et al. 2015 | Unclear | High | High | High | Low | High |
| Study | Selection (***) | Comparability (**) | Outcome (**) | Total | |||
|---|---|---|---|---|---|---|---|
| Representativeness of exposed Cohort (*) | Selection of non exposed Cohort (*) | Ascertainment of exposure (*) | Assessment of outcome (*) | Adequacy of follow-up (*) | |||
| Kiran et al. 2017 | * | * | * | 3 | |||
| Canullo et al. 2015 | * | * | * | ** | * | 6 | |
| Frisch et al. 2015 | * | * | * | * | * | 5 | |
| Study | Type of the Study | Follow-Up |
|---|---|---|
| Kiran et al. 2017 | Prospective clinical study | 6 months |
| Canullo et al. 2015 | Randomized controlled prospective clinical study | 3 months |
| Frisch et al. 2015 | Prospective clinical study | 12 months |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reda, R.; Zanza, A.; Cicconetti, A.; Bhandi, S.; Guarnieri, R.; Testarelli, L.; Di Nardo, D. A Systematic Review of Cementation Techniques to Minimize Cement Excess in Cement-Retained Implant Restorations. Methods Protoc. 2022, 5, 9. https://doi.org/10.3390/mps5010009
Reda R, Zanza A, Cicconetti A, Bhandi S, Guarnieri R, Testarelli L, Di Nardo D. A Systematic Review of Cementation Techniques to Minimize Cement Excess in Cement-Retained Implant Restorations. Methods and Protocols. 2022; 5(1):9. https://doi.org/10.3390/mps5010009
Chicago/Turabian StyleReda, Rodolfo, Alessio Zanza, Andrea Cicconetti, Shilpa Bhandi, Renzo Guarnieri, Luca Testarelli, and Dario Di Nardo. 2022. "A Systematic Review of Cementation Techniques to Minimize Cement Excess in Cement-Retained Implant Restorations" Methods and Protocols 5, no. 1: 9. https://doi.org/10.3390/mps5010009
APA StyleReda, R., Zanza, A., Cicconetti, A., Bhandi, S., Guarnieri, R., Testarelli, L., & Di Nardo, D. (2022). A Systematic Review of Cementation Techniques to Minimize Cement Excess in Cement-Retained Implant Restorations. Methods and Protocols, 5(1), 9. https://doi.org/10.3390/mps5010009










