Assessment of Common Risk Factors of Non-Communicable Diseases (NCDs) and Periodontal Disease in Indian Adults: An Analytical Cross-Sectional Study
Abstract
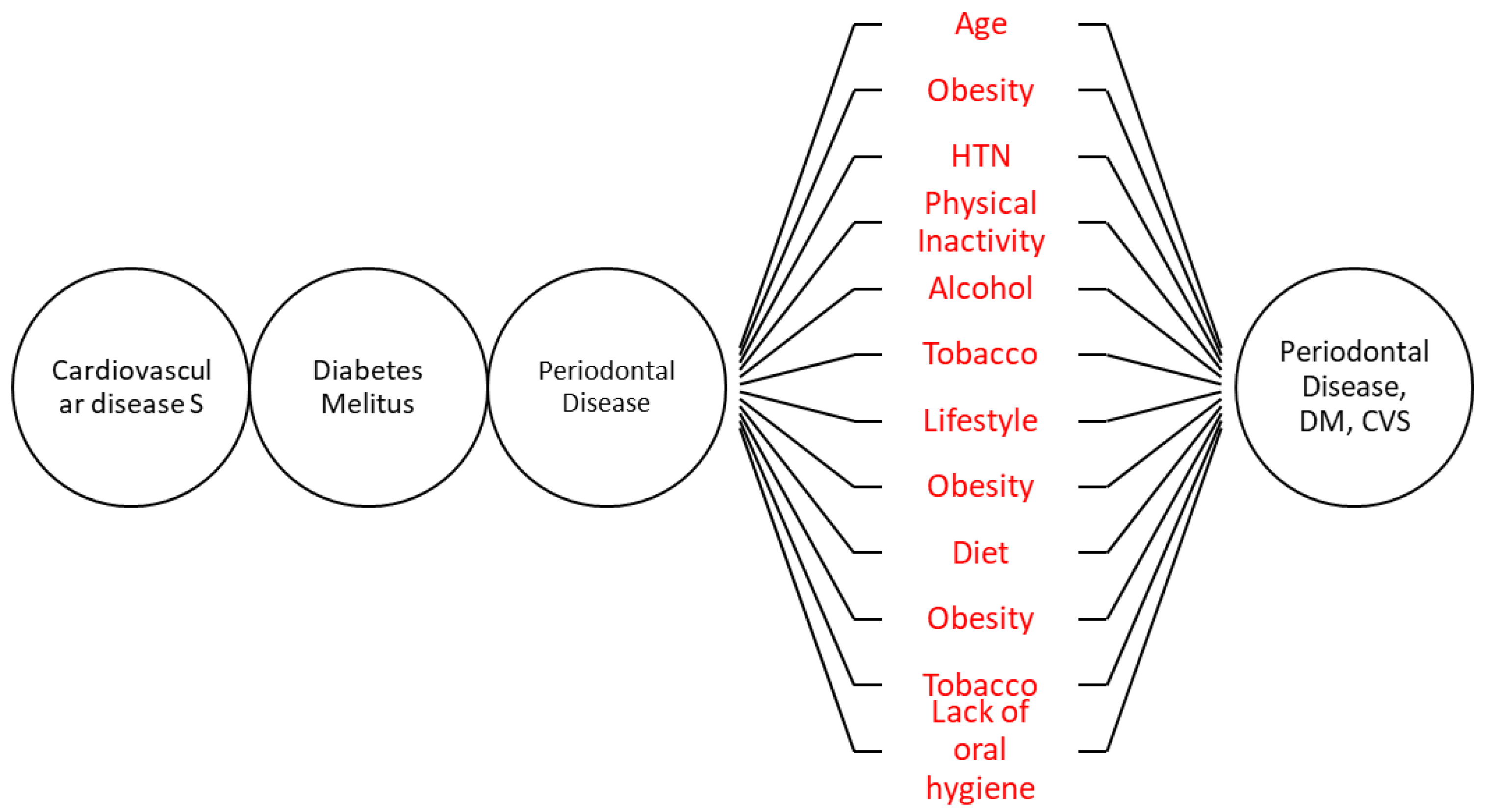
:1. Introduction
1.1. Research Question
1.2. Hypothesis
1.3. Objective
2. Experimental Design
2.1. Study Design
2.2. Study Setting
2.3. Participants
- I.
- Diabetes mellitus type 2 is diagnosed if a patient has any two of the following findings [24]:
- The presence of symptoms of diabetes such as increased thirst, increased urination and the random plasma glucose test shows a glucose level of 200 milligrams per deciliter (mg/dL).
- The fasting blood sugar level is equal to or greater than 126 mg/dL.
- A 2-h oral glucose tolerance test (OGTT) is ≥200 mg/dL.
- The hemoglobin A1c (HbA1c) is 6.5% or higher.
- II.
- Cardiovascular disease is defined as the name for the group of disorders of the heart and blood vessels [25], and includes:
- (a)
- (b)
- Coronary heart disease (heart attack)/myocardial infarction (MI) diagnosed by abnormalities detected in an electrocardiogram (ECG), echocardiogram, exercise stress test, a nuclear stress test, cardiac catheterization, an angiogram, a cardiac CT scan or CT coronary angiogram [27].
- (c)
- (d)
- III.
- Periodontal disease is defined as an inflammatory process affecting the supporting structures of the teeth resulting in pocket formation, recession or both and is diagnosed with a periodontal screening and recording (PSR) score of three in at least one sextant [33].
2.4. Participant Recruitment
- Patient will have at least one or more of the selected NCDs or periodontal disease as stated earlier.
- Patients should not have any comorbidities such as infectious diseases or other diseases other than non-communicable diseases taken into consideration.
- Subjects with no NCD or periodontal disease;
- Subjects not willing to participate in the study;
- Moribund patients.
2.5. Outcomes
- Dependent variables;
- Periodontal disease and non-communicable diseases (diabetes mellitus type 2, cardiovascular disease).
- ➢
- Age;
- ➢
- Gender;
- ➢
- Address;
- ➢
- Occupation;
- ➢
- Access to care;
- ➢
- Affordability of care;
- ➢
- Familial pattern;
- ➢
- Family size;
- ➢
- Insurance;
- ➢
- Socioeconomic status (modified Kuppuswamy criteria) [34];
- ➢
- Obesity–body mass index (BMI) is very commonly used to classify being overweight and obesity in adults. Body mass index (BMI) is measured as weight in kilograms/square of height in meters (Kg/m2) [35];
- ➢
- Tobacco usage: yes/no;
- ➢
- If yes: type/duration/frequency/quantity;
- ➢
- A physical activity measurement tool will be measured by the Physical Activity Assessment Tool devised by American Family Physician [36];
- ➢
- Alcohol consumption will be assessed by an alcohol consumption screening AUDIT questionnaire in adults introduced by WHO [37];
- ➢
- Food frequency questionnaire [38];
- ➢
- Stress can be assessed using the standard stress assessment questionnaire [39];
- ➢
- Oral hygiene;
- ➢
- Simplified Oral Hygiene Index [40];
- ➢
- Plaque index (Sillness and Loe) [41].
3. Procedure
3.1. Data Sources/Measurement
3.1.1. Tools Used
- (a)
- Data collection forms for the clinical and laboratory investigations data and recording of anthropometric data;
- (b)
- Validated structured questionnaire forms for enumerating the risk factors of each of the NCDs.
3.1.2. Data Collection
3.2. Bias
3.3. Sample Size
3.4. Statistical Methods
3.5. Data Monitoring
3.6. Ethical Considerations
3.7. Protocol Amendments
3.8. Consent to Participate in the Study
3.9. Confidentiality
4. Expected Results
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Noncommunicable Diseases. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 7 January 2022).
- The Top 10 Causes of Death. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 8 January 2022).
- Forouzanfar, M.H.; Afshin, A.; Alexander, L.T.; Biryukov, S.; Brauer, M.; Cercy, K.; Charlson, F.J.; Cohen, A.J.; Dandona, L.; Estep, K.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1659–1724. [Google Scholar] [CrossRef] [Green Version]
- WHO. Preventing Chronic Diseases: A Vital Investment. Available online: https://www.who.int/chp/chronic_disease_report/en/ (accessed on 7 June 2021).
- Thakur, J.S.; Prinja, S.; Garg, C.C.; Mendis, S.; Menabde, N. Social and Economic Implications of Noncommunicable diseases in India. Indian J. Community Med. 2011, 36, S13. [Google Scholar] [CrossRef] [PubMed]
- Chapple, I.L.C. Time to take periodontitis seriously. BMJ 2014, 348, g2645. [Google Scholar] [CrossRef] [PubMed]
- Janakiram, C.; Mehta, A.; Venkitachalam, R. Prevalence of periodontal disease among adults in India: A systematic review and meta-analysis. J. Oral. Biol. Craniofacial Res. 2020, 10, 800–806. [Google Scholar] [CrossRef] [PubMed]
- Chapple, I.L.C.; Van Der Weijden, F.; Doerfer, C.; Herrera, D.; Shapira, L.; Polak, D.; Madianos, P.; Louropoulou, A.; Machtei, E.; Donos, N.; et al. Primary prevention of periodontitis: Managing gingivitis. J. Clin. Periodontol. 2015, 42, S71–S76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Humphrey, L.L.; Fu, R.; Buckley, D.I.; Freeman, M.; Helfand, M. Periodontal disease and coronary heart disease incidence: A systematic review and meta-analysis. J. Gen. Intern. Med. 2008, 23, 2079–2086. [Google Scholar] [CrossRef] [Green Version]
- Janket, S.J.; Baird, A.E.; Chuang, S.K.; Jones, J.A. Meta-analysis of periodontal disease and risk of coronary heart disease and stroke. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2003, 95, 559–569. [Google Scholar] [CrossRef]
- Saremi, A.; Nelson, R.G.; Tulloch-Reid, M.; Hanson, R.L.; Sievers, M.L.; Taylor, G.W.; Shlossman, M.; Bennett, P.H.; Genco, R.; Knowler, W.C. Periodontal disease and mortality in type 2 diabetes. Diabetes Care 2005, 28, 27–32. [Google Scholar] [CrossRef] [Green Version]
- Ezzati, M.; Riboli, E. Can noncommunicable diseases be prevented? Lessons from studies of populations and individuals. Science 2012, 337, 1482–1487. [Google Scholar] [CrossRef] [Green Version]
- Listl, S.; Galloway, J.; Mossey, P.A.; Marcenes, W. Global economic impact of dental diseases. J. Dent. Res. 2015, 94, 1355–1361. [Google Scholar] [CrossRef]
- Sheiham, A.; Watt, R.G. The common risk factor approach: A rational basis for promoting oral health. Community Dent. Oral. Epidemiol. 2000, 28, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Fehily, A.M.; Phillips, K.M.; Yarnell, J.W.G. Diet, smoking, social class, and body mass index in the Caerphilly Heart Disease Study. Am. J. Clin. Nutr. 1984, 40, 827–833. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santhosh Kumar, C.; Somasundara, S. Common Risk Factor Approach: Finding Common Ground for Better Health Outcomes. Int. J. Contemp. Med. Res. 2017, 4, 1367–1370. [Google Scholar]
- Yuan, S.Y.; Freeman, R. Can social support in the guise of an oral health education intervention promote mother-infant bonding in Chinese immigrant mothers and their infants? Health Educ. J. 2011, 70, 57–66. [Google Scholar] [CrossRef]
- Kwan, S.Y.L.; Petersen, P.E.; Pine, C.M.; Borutta, A. Health-promoting schools: An opportunity for oral health promotion. Bull World Health Organ. 2005, 83, 677–685. [Google Scholar] [PubMed]
- WHO. The Liverpool Declaration: Promoting Oral Health in the 21st Century. 2010. Available online: https://www.who.int/oral_health/events/orh_liverpool_declaration_05.pdf?ua=1 (accessed on 7 January 2022).
- EMI. CED—European Dentists Call for Better Integration of Oral and General Health. Available online: https://europeanmovement.eu/news/ced-european-dentists-call-for-better-integration-of-oral-and-general-health/ (accessed on 7 June 2021).
- World Health Professions Alliance. WHPA Statement on Non-Communicable Diseases and Social Determinants for Health. Available online: https://www.whpa.org/news-resources/statements/whpa-statement-non-communicable-diseases-and-social-determinants-health (accessed on 7 June 2021).
- FDI. Oral Health and the United Nations Political Declaration on NCDs. Available online: https://www.fdiworlddental.org/resource/oral-health-and-united-nations-political-declaration-ncds (accessed on 7 June 2021).
- Benzian, H.; Guarnizo-Herreño, C.C.; Kearns, C.; Muriithi, M.W.; Watt, R.G. The WHO global strategy for oral health: An opportunity for bold action. Lancet 2021, 398, 192–194. [Google Scholar] [CrossRef]
- Kerner, A.W.; Brückel, J. Definition, Classification and Diagnosis of Diabetes Mellitus. Exp. Clin. Endocrinol. Diabetes 2014, 122, 384–386. [Google Scholar] [CrossRef] [Green Version]
- WHO. About Cardiovascular Diseases. Available online: https://www.who.int/cardiovascular_diseases/about_cvd/en/ (accessed on 7 June 2021).
- The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Available online: https://www.nhlbi.nih.gov/files/docs/guidelines/jnc7full.pdf (accessed on 7 January 2022).
- Coronary Artery Disease: Causes, Symptoms, Diagnosis & Treatments. Available online: https://my.clevelandclinic.org/health/diseases/16898-coronary-artery-disease (accessed on 7 June 2021).
- Hasan, T.F.; Rabinstein, A.A.; Middlebrooks, E.H.; Haranhalli, N.; Silliman, S.L.; Meschia, J.F.; Tawk, R.G. Diagnosis and Management of Acute Ischemic Stroke. Mayo Clin. Proc. 2018, 93, 523–538. [Google Scholar] [CrossRef] [Green Version]
- Stroke—Diagnosis and Treatment—Mayo Clinic. Available online: https://www.mayoclinic.org/diseases-conditions/stroke/diagnosis-treatment/drc-20350119 (accessed on 7 June 2021).
- National Institutes of Health Stroke Scale—Wikipedia. Available online: https://en.wikipedia.org/wiki/National_Institutes_of_Health_Stroke_Scale (accessed on 7 June 2021).
- Peripheral Artery Disease (PAD)—Diagnosis and Treatment—Mayo Clinic. Available online: https://www.mayoclinic.org/diseases-conditions/peripheral-artery-disease/diagnosis-treatment/drc-20350563 (accessed on 7 June 2021).
- Sontheimer, D.L. Peripheral Vascular Disease: Diagnosis and Treatment. Am. Fam. Physician 2006, 73, 1971–1976. [Google Scholar]
- Landry, R.G.; Jean, M. Periodontal Screening and Recording (PSR) Index: Precursors, utility and limitations in a clinical setting. Int. Dent. J. 2002, 52, 35–40. [Google Scholar] [CrossRef]
- Wani, R. Socioeconomic status scales-modified Kuppuswamy and Udai Pareekh’s scale updated for 2019. J. Fam. Med. Prim. Care 2019, 8, 1846. [Google Scholar] [CrossRef] [PubMed]
- CDC. About Adult BMI | Healthy Weight, Nutrition, and Physical Activity. Available online: https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html (accessed on 7 June 2021).
- Physical Activity Assessment Tool. Available online: https://www.aafp.org/afp/2008/0415/afp20080415p1129-f1.pdf (accessed on 7 June 2021).
- Calculator: Alcohol Consumption Screening AUDIT Questionnaire in Adults (Patient Education)—UpToDate. Available online: https://www.uptodate.com/contents/calculator-alcohol-consumption-screening-audit-questionnaire-in-adults-patient-education (accessed on 7 June 2021).
- Telles, S.; Bhardwaj, A.K.; Gupta, R.K.; Kumar, A.; Balkrishna, A. Development of a Food Frequency Questionnaire to Assess Dietary Intake for the Residents of the Northern Region of India. Indian J. Anc. Med. Yoga 2016, 9, 139–147. [Google Scholar] [CrossRef]
- Standard Process Instrument Standard Process Stress Assess. Available online: https://irp.cdn-website.com/b624d5fe/files/uploaded/Stress-Forms%20%281%29.pdf (accessed on 7 June 2021).
- Greene, J.C.; Vermillion, J.R. The Simplified Oral Hygiene Index. J. Am. Dent. Assoc. 1964, 68, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Löe, H. The Gingival Index, the Plaque Index and the Retention Index Systems. J. Periodontol. 1967, 38, 610–616. [Google Scholar] [CrossRef]
- Hefti, A.F.; Preshaw, P.M. Examiner alignment and assessment in clinical periodontal research. Periodontology 2000 2012, 59, 41–60. [Google Scholar] [CrossRef]


| Blood Pressure Classification | SBP | DBP |
|---|---|---|
| mmHg | mmHg | |
| Normal | <120 | <80 |
| Prehypertension | 120–139 | 80–89 |
| Stage 1 Hypertension | 140–159 | 90–99 |
| Stage 2 Hypertension | ≥160 | ≥100 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Puzhankara, L.; Janakiram, C. Assessment of Common Risk Factors of Non-Communicable Diseases (NCDs) and Periodontal Disease in Indian Adults: An Analytical Cross-Sectional Study. Methods Protoc. 2022, 5, 22. https://doi.org/10.3390/mps5020022
Puzhankara L, Janakiram C. Assessment of Common Risk Factors of Non-Communicable Diseases (NCDs) and Periodontal Disease in Indian Adults: An Analytical Cross-Sectional Study. Methods and Protocols. 2022; 5(2):22. https://doi.org/10.3390/mps5020022
Chicago/Turabian StylePuzhankara, Lakshmi, and Chandrashekar Janakiram. 2022. "Assessment of Common Risk Factors of Non-Communicable Diseases (NCDs) and Periodontal Disease in Indian Adults: An Analytical Cross-Sectional Study" Methods and Protocols 5, no. 2: 22. https://doi.org/10.3390/mps5020022
APA StylePuzhankara, L., & Janakiram, C. (2022). Assessment of Common Risk Factors of Non-Communicable Diseases (NCDs) and Periodontal Disease in Indian Adults: An Analytical Cross-Sectional Study. Methods and Protocols, 5(2), 22. https://doi.org/10.3390/mps5020022





