A Protocol for the Acquisition of Comprehensive Proteomics Data from Single Cases Using Formalin-Fixed Paraffin Embedded Sections
Abstract
:1. Introduction
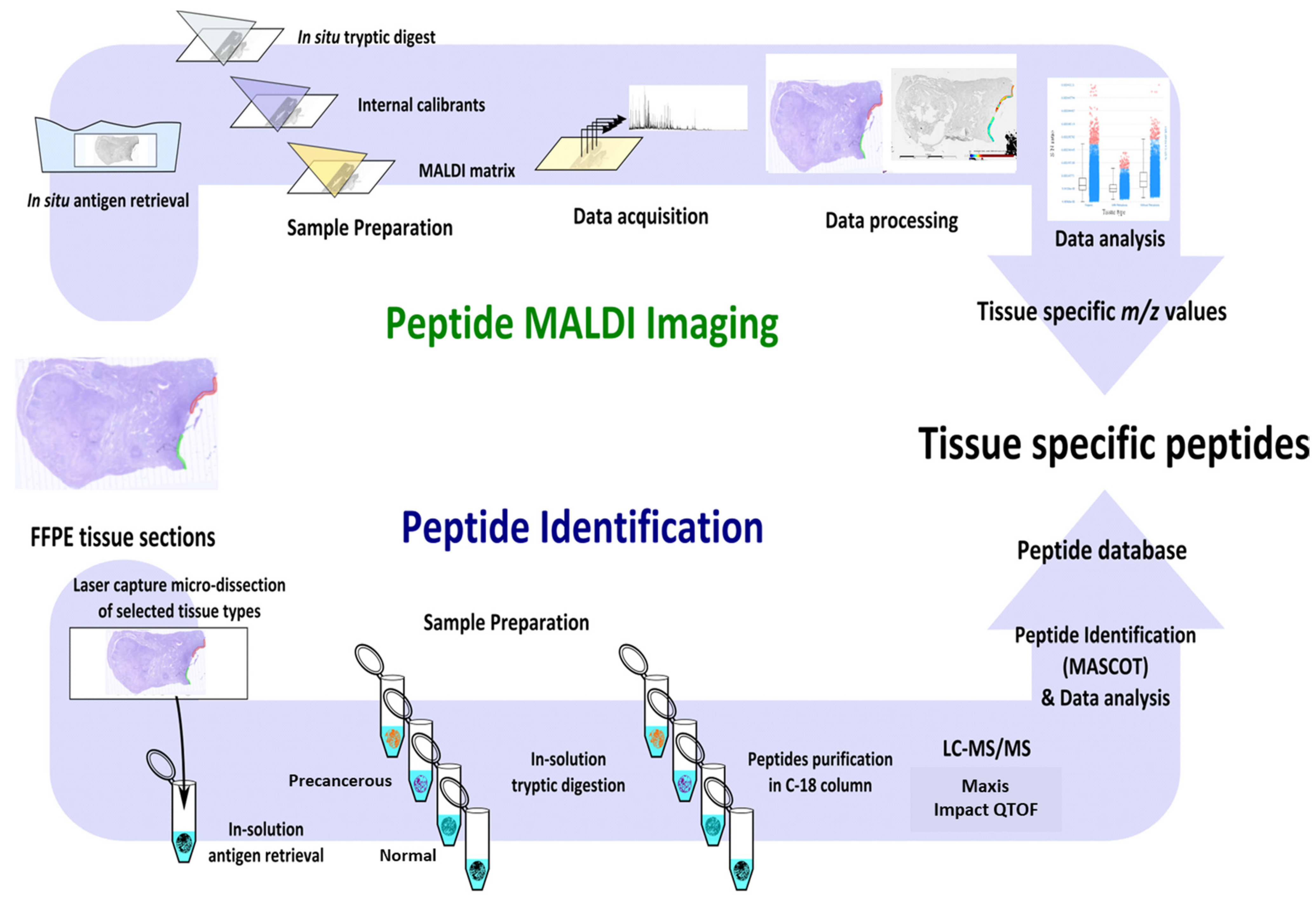
2. Experimental Design
2.1. Materials
- Acetonitrile, LC-MS/MS grade (1000302500, ACN, Merck, Darmstadt, Germany)
- A-cyano-4-hydroxycinnamic acid (201344, HCCA, Bruker Daltonics, Bremen, Germany)
- Ammonium bicarbonate (103025E, Merck, Feltham Middlesex, UK)
- Citric acid monohydrate (C0706, Sigma-Aldrich, Tokyo, Japan)
- Dithiothreitol (D9163, DTT, Sigma-Aldrich, Berlington, Massachusetts, USA)
- Eosin (HT110332, Sigma-Aldrich, Hamburg, Germany)
- ESI-L low concentration tuning mix (G1969-85000, Agilent, Santa Clara, California, USA)
- Ethanol AR grade (4.10230.2511, Merck, Bayswater, Victoria, Australia)
- Ethanol, LC-MS/MS grade (1117272500, Merck, Bayswater, Victoria, Australia)
- Formic acid, LC-MS/MS grade (21909098, FA, Sigma-Aldrich, Hamburg, Germany)
- Iodoacetamide (RPN6302OL/AG, IAA, GE Healthcare, Danderyd, Sweden)
- Isopropanol AR grade (8187661000, Merck, Darmstadt, Germany)
- Mayer’s hematoxylin (GH5232, Sigma-Aldrich, Hamburg, Germany)
- Methanol LC-MS/MS grade (1.06018.2500, Merck, Darmstadt Germany)
- Milli-Q® ultrahigh purity water (D11951, ≥18.2 MΩ, Barnstead International, Dubuque, IA, USA)
- Mounting medium (PER40000, Medite, Burgdorf, Germany)
- Neutral buffered formalin (HT501, Sigma-Aldrich, Hamburg, Germany)
- Sodium hydroxide (1.06498.0500, NaOH, Merck, Darmstadt Germany)
- Trifluoroacetic acid (1.08262.0100, TFA, Merck, Darmstadt Germany)
- Trypsin Gold (V5280, Promega, Maddison, Wisconsin, USA)
- Trypsin sequencing grade (V51111, Promega, Maddison, Wisconsin, USA)
- Xylene (XA003, Chem-Supply, Gillmann, South Australia, Australia)
- Urea (1084870500, Merck, Darmstadt, Germany)
2.2. Equipment
- Centrifuge 5810R (Eppendorf, Hamburg, Germany)
- CyberScan PC 300 pH Meter (Eutech Instruments, Singapore, Singapore)
- Data analysis software (e.g., MaxQuant 1.5.2.8)
- Dry block heater (Ratek, Boronia, Victoria, Australia)
- Flexcontrol v3.4, flexImaging v4.0 and flexanalysis v4.0 software (Bruker Daltonics, Bremen, Germany)
- Glass Coplin Jar (H441, ProSciTech, Kirwan, Queensland, Australia)
- High performance liquid chromatography (HPLC) vials (6820.0029, Dionex, Amsterdam, The Netherlands)
- ImagePrep (Bruker Daltonics, Bremen, Germany)
- Incubator at 37 °C (Boekel Scientific, Trevose, PA, USA)
- Indium-tin-oxide (ITO) slides (237001, Bruker Daltonics, Bremen, Germany)
- Leica EG 114OH embedder (Leica Biosystems, Mount Waverly, Victoria, Australia)
- Leica TP 1020 processor (Leica Biosystems, Mount Waverly, Victoria, Australia)
- Leica Zeiss Laser capture microdissection system (Leica Microsystems, Wetzlar, Germany)
- Mass spectrometer (e.g., Maxis Impact II QTOF (Bruker Daltonics, Bremen, Germany)
- Mass spectrometric data acquisition software [e.g., QTOF control (version 3.4) and hystar (version 3.2)]
- Microm HM 325 microtome (Zeiss, Niedersachsen, Germany)
- Microwave (LG 700 W MS19496, LG, Jinzhou, China)
- MTP slide adaptor II (Bruker Daltonics, Bremen, Germany)
- NanoDrop 2000 (Thermo-Fisher Scientific, Minneapolis, MN, USA)
- Nanozoomer (Hamamatsu, Hamamatsu City, China)
- nano-HPLC Ultimate 3000 RS system (Dionex, Amsterdam, The Netherlands)
- Polyethylene naphthalate (PEN) membrane slides (11505158, MicroDissect, Herborn, Germany)
- Thermomixer (Eppendorf, Hamburg, Germany)
- Tipp-Ex (water-based white out, Winc, Wingfield, South Australia, Australia).
- Scanner (CanoScan 5600 F, Canon, Phra Nakhon Si Ayutthaya, Thailand).
- SpeedVac concentrator (Savant SVC 100, Thermo Scientific, Minneapolis, MN, USA)
- SCiLS lab 2016b (Bruker Daltonics, Germany)
- Superfrost Plus microscopic slides (6.700 125, Thermo scientific, Minneapolis, Minnesota, Germany)
- Ultraflextreme MALDI TOF (Bruker Daltonics, Bremen, Germany)
- Ultra-low −80 °C freezer (SANYO, Tokyo, Japan)
- Vivacon ultrafiltration spin columns (VS0101, Sartorius Vivacon 500, 10,000 MWCO HY, Vivacon, Cologne, Germany).
- ZipTip C18 (ZTC18M096, Millipore, Burlington, MA, USA)
3. Procedure
3.1. Tissue Collection
- 1.
- In our study, tissues were collected after a total abdominal hysterectomy and bilateral salpingo-oophorectomy was performed on a patient with endometrial hyperplasia at the Royal Adelaide Hospital, Adelaide, Australia, with written informed consent from the patient. The study was approved by the ethics committee of the Royal Adelaide Hospital.
- 2.
- Process the tissue(s) using the standard procedure [19]. Briefly, fix the tissue(s) in 10% (v/v) neutral buffered formalin overnight at 4 °C, followed by washing with milli-Q® water and storing in 70% (v/v) ethanol before processing them with a Leica TP 1020 processor. Embed the tissue(s) in paraffin using a Leica EG 114OH embedder. In our study, tissues were processed and embedded by histology services at the University of Adelaide, Adelaide, Australia. Critical step: Formalin fixation time depends on the tissue size; on average, formalin penetrates tissue at a rate of ~1 mm/h [20].
- 3.
- Section the FFPE block(s) using Microm HM 325 microtome at 4 µm thickness and water bath mount at 38 °C onto PEN membrane slides for LC-MS/MS, ITO slides for MALDI MSI and superfrost slides for staining purposes.
- 4.
- Dry the slide(s) at 37 °C for 1 h, followed by overnight drying at room temperature.
- 5.
- For pathological identification, stain the tissue(s) using H&E or antibody using standard protocols [19]. Here, the identification of PLs (Figure 2) was performed by an experienced pathologist, Prof. Whitehead, using H&E and antibody-stained tissue(s) for P53 and M1B1 (data not shown). Areas of STIC, EIC, and adjacent healthy epithelium were annotated as shown in Supplementary Figure S1.
3.2. Laser Capture Microdissection and Protein Extraction for LC-MS/MS
- 6.
- Place the PEN membrane slide(s) on a heating block at 60 °C for 5 min, with the tissue facing up.
- 7.
- Remove paraffin by dipping the slide(s) in xylene for 90 sec followed by 2 min incubation in 100% ethanol (repeat twice) and 5 min incubation in Milli-Q® water (repeat twice), and then stain the slide(s) with hematoxylin for 20 sec or until the tissue appears purple. Critical step: Staining time depends upon the concentration/age of the solution and/or thickness of the tissue section.
- 8.
- Destain the slide in Milli-Q® water and then with 70% (v/v) ethanol for 1 min.
- 9.
- Let the slide dry at room temperature.
- 10.
- Load the stained slide and compatible LCM tubes into the Leica Zeiss LCM system. Critical step: To avoid tissue sticking to the side, 5 µL of 10 mM citric acid buffer is added to the cap of an LCM tube
- 11.
- Carefully cut out the regions of interest(s) (ROI) and ensure that each ROI has been collected into the cap of separate tubes. The tissue before and after LCM dissection of the tissue is shown in Supplementary Figure S1.
- 12.
- Briefly, centrifuge the tubes and make sure that the tissue region(s) are in the buffer and at the bottom of the tube. Pause step: tissue(s) can be stored for months at −80 °C
- 13.
- To retrieve the proteins, add 200 µL of 10 mM citric acid and boil the tubes for 100 min at 98 °C on a thermomixer.
- 14.
- Let the tubes cool at room temperature and centrifuge briefly.
- 15.
- Protein concentration can be estimated at this point using Bradford assay, EZQ assay, nanodrop, or tryptophan assay. We used NanoDrop 2000 at 280 nm.
3.3. Trypsin Digestion and Peptide Clean-Up for LC-MS/MS
- 16.
- Remove the supernatant and replace it with 200 μL of lysis buffer (8 M urea in 100 mM ammonium bicarbonate with a final concentration of DTT of 50 mM), followed by incubation at 20 °C for 1 h.
- 17.
- Put the Vivacon ultrafiltration spin columns’ filters into the provided 1.5 mL centrifuge tube and rinse the columns three times with 100 μL of 100 mM ammonium bicarbonate by centrifuging at 14,000× g for 10 min, followed three times with 100 µL of lysis buffer. Critical Step: Once the columns are equilibrated, try not to dry them out. This can be achieved by retaining a small amount of buffer on top of the column.
- 18.
- Replace the collection tube with a fresh 1.5 mL centrifuge tube. Load the tissue samples into the spin columns and centrifuge them at 14,000× g for 10 min at room temperature. Critical Step: To make sure the proper binding of proteins to the Vivacon ultrafiltration spin column membrane, this step can be repeated twice with the flow-through.
- 19.
- Discard the flow-through and subsequently alkylate the samples with 55 mM IAA in 100 mM ammonium bicarbonate, followed by incubation in the dark at room temperature for 30 min.
- 20.
- Centrifuge the filters as in step 17 above and wash the membrane twice with 100 μL of 100 mM ammonium bicarbonate, followed by one wash with 100 μL of 50 mM ammonium bicarbonate.
- 21.
- Digest the alkylated proteins at 37 °C overnight with sequencing grade trypsin at an enzyme-to-substrate ratio of 1:50 in 100 μL of 5 mM ammonium bicarbonate. Critical step: To minimize the evaporation and drying of the peptides, the bottom of the tubes can be filled with water and must be sealed using parafilm.
- 22.
- After overnight incubation, add 0.1% FA to stop the digestion.
- 23.
- Elute tryptic peptides off the filter by centrifuging the tubes at 14,000× g for 10 min.
- 24.
- Dry the samples by vacuum centrifugation without heating. Pause step: Dried samples can be stored for months at −80 °C.
- 25.
- Reconstitute the peptides in 2% (v/v) can, sonicate for 5 min, vortex, and centrifuge briefly.
- 26.
- Estimate the peptide concentration using a nanodrop at 205 nM wavelength.
- 27.
- Acidify the samples to a final concentration of 0.1% FA and place them in HPLC vials for peptide LC-MS/MS analysis (proceed to step 29). Alternatively, an optional extra clean-up step can be performed by using C18 Zip-tips. This will remove any residual salt that may be remaining.
- 28.
- C18 ZipTip preparation: Prepare the ZipTips as per the manufacturer’s protocol. Critical step: Use one tip per sample.
- Equilibrate the tips three times with 100% can followed by three times with 0.1% FA (v/v).
- Load the peptide samples ten times by pipetting the digest up and down.
- Wash the samples six times with 0.1% FA (v/v).
- Elute the bound peptides six times with 60% (v/v) can containing 0.1% (v/v) FA.
- Dry the eluted peptide mixture using a speedVac without heating.
- Resuspend the peptides in 2% (v/canACN, sonicate for 5 min, vortex, and centrifuge briefly. Pause step: Samples can be stored at −80 °C until required.
3.4. Nano-LC-MS/MS Analysis
- 29.
- Prepared peptide samples can now be loaded onto an HPLC system connected online to a mass spectrometry. Our laboratory uses an ultimate 3000 HPLC system (Dionex, Thermo-Fisher Scientific) connected online to a maxis impact II QTOF (Bruker Daltonics).
- 30.
- Inject ~1 µg of each sample and load for 8 min at a flow rate of 5 µL/min in 2% (v/canACN, 0.1% (v/v) FA onto a C18 trapping column. Critical step: Based on the flow rate and tubing size, the sample loading time and gradient should be optimized for the instrument in use.
- 31.
- Separate the peptides onto a C18 analytical column using 2% canv) ACN in 0.1% (v/v) FA (Buffer A) and 80% (v/v) ACN in 0.1% (v/v) FA (Buffer B) at a flow rate of 300 nL/min. The gradient used in our laboratory was 5% to 45% buffer B over 130 min, followed by a gradual increase in buffer B from 45% to 90% for 1 min and then held at 90% buffer B for 20 min, followed by re-equilibration of the column for 20 min at 5% buffer B, for a total run time of 180 min.
- 32.
- Depending on the selected ion source and the HPLC flow rate, the appropriate settings for the nebulizer and dry gas must be selected. In our laboratory, the column eluent from the LC was connected online to Bruker’s CaptiveSprayTM source optimized to a capillary voltage of 1300 V with capillary temperature of 150 °C, at a nebulizing pressure of 3 L/mins.
- 33.
- Data-dependent acquisition can be performed using Bruker’s Shotgun InstantExpertiseTM method. This is an advanced intelligent method to provide greater coverage and data analysis compatibility. Instead of the typical Top Intensity or Increasing m/z selection, this method uses a simplified acquisition model via an intelligent duty cycle optimizer. In this method,
- The depth of sampling is auto-optimized;
- The acquisition speed for each MS/MS event is auto-regulated;
- The acquisition exclusion is auto-optimized;
- The peak depth is optimized on the collision cell recovery using factory settings.
- 34.
- On the orthogonal TOF systems, the mass range for the MS and MS/MS mode is the same. For tryptic peptides, we recommend setting the mass range to 50 to 2200 m/z.
- 35.
- Exclude the singly charged precursor ions from acquisition, which prevents the selection of singly charged background ions, as well as polymer signals.
- 36.
- As determined by the m/z of the precursor ion, the collision energy ranges from 23 to 65%.
- 37.
- Set up a sample table in HyStar and select the appropriate LC and MS methods for the sample analysis.
3.5. LC-MS/MS Data Analysis
- 38.
- The standard Bruker QTOF settings can be used with a mass error tolerance of 40 ppm; more specific parameters are defined as explained below:
- Select the appropriate. fasta files, for, e.g., UniProt human-reviewed database;
- Select the digestion enzyme for Trypsin;
- Set the maximum number of missed cleavages to 1;
- Select fixed modification to carbamidomethyl of cysteines;
- Select the variable modification of oxidation of methionine;
- Set the protein false discovery rate (FDR) and peptide spectrum match FDRs to 1% using a target decoy approach;
- Set a minimum peptide length of seven amino acids;
- Set only unique and razor peptides when reporting protein identifications/
3.6. In Situ Tryptic Peptide MALDI MSI Analysis
- 39.
- Place the ITO slide onto a heating block at 60 °C for 1 h.
- 40.
- Wash the slide twice in 100% xylene for 5 min each.
- 41.
- Wash the slide twice in 100% ethanol for 2 min each.
- 42.
- Rinse the slide twice with 10 mM ammonium bicarbonate for 5 min each.
- 43.
- Place the slide in an empty cleaned Coplin jar and fill the remaining slots with blank super frost slides (to prevent the formation of big air bubbles during the antigen retrieval step).
- 44.
- Fill the Coplin jar with 10 mM citric acid monohydrate and microwave it at high power for 1.05 min or until the citric acid starts to boil.
- 45.
- Once the citric acid reached the boiling point, microwave the slide for 10 min at power 10.
- 46.
- Following microwave incubation, rapidly transfer the Coplin jar to a heating block set at 98 °C for 30 min.
- 47.
- Remove the slide from the Coplin jar and allow it to cool down at room temperature.
- 48.
- Rinse the slide twice with 10 mM ammonium bicarbonate.
- 49.
- Dry the slide at room temperature for ~10 min.
- 50.
- Apply teach marks on the 4 sides of the slide using Tipp-Ex (water-based white out).
- 51.
- Scan the slide at a 2400 dpi resolution (CanoScan 5600 F, Canon, Thailand).
- 52.
- Adjust the spray offset on the ImagePrep station (Bruker Daltonics), such that the spray lasts for at least 54 sec, and cover the whole slide slot. Set the Global Power Adjustment at 38% spray power with 0% modulation.
- 53.
- Dilute 40 µL of the trypsin gold aliquot with 160µL of 25 mM ammonium bicarbonate and load directly onto the spray generator of the ImagePrep.
- 54.
- Spray the trypsin using the trypsin deposition method as detailed in 6.2.1.
- 55.
- After trypsin deposition, incubate the slide at 37 °C for 2 h in a humidified chamber.
- 56.
- After 1.45 h, thaw, vortex, and quickly pulsecentrifuge an aliquot of internal calibrant and spray the internal calibrant using the same method as that of trypsin.
- 57.
- Fill the ImagePrep solution vial with the matrix and adjust the spray offset for the matrix deposition as detailed in6.2.1.
- 58.
- After matrix deposition, remove the slide from the Imageprep and clean both ends of the slides with 100% methanol.
- 59.
- Load the prepared slide into an MTP slide adapter II and acquire the data using the ultrafleXtreme MALDI TOF/TOF instrument.
- 60.
- Using the flexcontrol, create an autoXecute method with the following required settings:
- Select the optimized and calibrated flexControl method in the general tab.
- Turn the fuzzy control off and set the optimized laser power (we used 50% laser power).
- No background list should contain in the evaluation tab.
- Acquire 500 shots in 500 shot steps with dynamic termination and random walk-off.
- Choose an appropriate data processing method as in step 61.
- 61.
- Create a flexAnalysis method with the following defined settings: smoothing by Gaussian (2 cycles with the width of m/z 0.02), TopHat baseline subtraction, Monoisotopic SNAP peak algorithm, and the quadratic recalibration using the calibrations masses (1296.685, 1570.677, 2147.19,9 and 2932.588) with a mass tolerance of 500 ppm.
- 62.
- Open flexImaging and create a new sequence with a sample preparation type of uniformly distributed coating and 60 µm raster width for this workflow.
- 63.
- Teach the slide using the scanned slide and check the teaching by moving the sample carrier at various points on the slide.
- 64.
- Create the polygon measurement of the region(s) and save the flexImaging sequence.
- 65.
- Optimize the laser power by shooting the laser outside the tissue region and on the calibrants sprayed.
- 66.
- Calibrate the flexcontrol method from the calibration tab in the flexcontrol and save the method. Critical Note: Make sure monoisotopic peaks are resolved to baseline.
- 67.
- Start the data acquisition from the flexImaging checklist menu.
- 68.
- After data acquisition, remove the slide from the instrument and wash the matrix using 70% ethanol (AR grade) and H&E stain using the standard procedure; briefly,
- Rinse the slide with 70% ethanol (AR grade) for 5 min or until the matrix is removed;
- Dip into deionized water for 30 s;
- Immerse in hematoxylin solution (Mayer’s) for 50 s;
- Wash with tap water for 5 min;
- Immerse in eosin solution for 30 s;
- Rinse with 70% ethanol (AR grade) for 30 s;
- Rinse with 90% ethanol (AR grade) for 30 s;
- Rinse with 100% ethanol (AR grade) for 30 s;
- Rinse with 100% isopropanol (AR grade) for 30 s;
- Rinse twice with xylene for 1 min each;
- Apply the mounting medium onto the cover slide;
- Cover the tissue section with the coverslip and gently pressed it onto it;
- Let the slide dry overnight at room temperature under the fume hood.
- 69.
- Scan the slide at a 20× objective using a Nanozoomer and co-register the scanned slide using flexImaging edit drop-down menu “co-register image” and save the sequence.
- 70.
- Mark the region(s) of interest as per the pathologist’s annotation, in our case EIC and normal endometrium.
- 71.
- Load the raw data into SCiLS lab v2016b and process them there by selecting the instrument type “Time-of-flight”, Import raw, fallback to reduced spectra, and TopHat as the baseline subtraction method.
- 72.
- Open the imported dataset, set the denoising as weak, baseline removal as TopHat, and change the file properties from the file’s drop-down menu to 0.125 Da.
- 73.
- Using the Peak picked algorithm from the tools drop-down menu, create a list of peaks detected and manually go through each m/z value that is differentially regulated in the region(s) of interest (Figure 3).
4. Expected Results
5. Discussion
6. Reagent and Equipment Set-Up
6.1. Reagent Set Up
6.2. Equipment Set-Up
6.2.1. Nano-HPLC System
- -
- Deposit the trypsin using Bruker’s default method with minor modifications. Settings used:38% Spray Power with 0% Modulation, total number of 30 cycles with spraying time of 1.25 s, and 45 s of drying.
- -
- Deposit the matrix using Bruker’s default HCCA method with minor modifications. Settings used (Table 2):
6.2.2. Mass Spectrometer System
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Weke, K.; Kote, S.; Faktor, J.; Al Shboul, S.; Uwugiaren, N.; Brennan, P.M.; Goodlett, D.R.; Hupp, T.R.; Dapic, I. DIA-MS proteome analysis of formalin-fixed paraffin-embedded glioblastoma tissues. Anal. Chim. Acta 2022, 1204, 339695. [Google Scholar] [CrossRef]
- Gustafsson, O.J.; Arentz, G.; Hoffmann, P. Proteomic developments in the analysis of formalin-fixed tissue. Biochim. Biophys. Acta (BBA)-Proteins Proteom. 2014, 1854, 559–580. [Google Scholar] [CrossRef]
- Tolcher, M.C.; Swisher, E.M.; Medeiros, F.; Lima, J.F.; Hilderbrand, J.L.; Donovan, J.L.; Garcia, R.L.; Cliby, W.A.; Dowdy, S.C. Characterization of Precursor Lesions in the Endometrium and Fallopian Tube Epithelium of Early-Stage Uterine Serous Carcinoma. Int. J. Gynecol. Pathol. 2015, 34, 57–64. [Google Scholar] [CrossRef] [Green Version]
- Hui, P.; Kelly, M.P.; O’Malley, D.M.; Tavassoli, F.A.; Schwartz, P.E. Minimal uterine serous carcinoma: A clinicopathological study of 40 cases. Mod. Pathol. 2004, 18, 75–82. [Google Scholar] [CrossRef] [Green Version]
- Wheeler, D.T.; Bell, K.A.; Kurman, R.J.; Sherman, M.E. Minimal uterine serous carcinoma: Diagnosis and clinicopathologic correlation. Am. J. Surg. Pathol. 2000, 24, 797–806. [Google Scholar] [CrossRef]
- Gant, K.; Jambor, A.; Li, Z.; Rentchler, E.; Weisman, P.; Li, L.; Patankar, M.; Campagnola, P. Evaluation of Collagen Alterations in Early Precursor Lesions of High Grade Serous Ovarian Cancer by Second Harmonic Generation Microscopy and Mass Spectrometry. Cancers 2021, 13, 2794. [Google Scholar] [CrossRef]
- Zheng, W.; Xiang, L.; Fadare, O.; Kong, B. A Proposed Model for Endometrial Serous Carcinogenesis. Am. J. Surg. Pathol. 2011, 35, e1–e14. [Google Scholar] [CrossRef]
- Bowtell, D.D.L. The genesis and evolution of high-grade serous ovarian cancer. Nat. Cancer 2010, 10, 803–808. [Google Scholar] [CrossRef]
- George, S.H.L.; Shaw, P. BRCA and Early Events in the Development of Serous Ovarian Cancer. Front. Oncol. 2014, 4, 5. [Google Scholar] [CrossRef] [Green Version]
- Piek, J.; Van Diest, P.J.; Zweemer, R.P.; Jansen, J.W.; Poort-Keesom, R.J.J.; Menko, F.H.; Gille, J.; Jongsma, A.P.M.; Pals, G.; Kenemans, P. Dysplastic changes in prophylactically removed Fallopian tubes of women predisposed to developing ovarian cancer. J. Pathol. 2001, 195, 451–456. [Google Scholar] [CrossRef]
- Crum, C.P.; Drapkin, R.; Kindelberger, D.; Medeiros, F.; Miron, A.; Lee, Y. Lessons from BRCA: The Tubal Fimbria Emerges as an Origin for Pelvic Serous Cancer. Clin. Med. Res. 2007, 5, 35–44. [Google Scholar] [CrossRef] [Green Version]
- Crum, C.P.; Herfs, M.; Ning, G.; Bijron, J.G.; Howitt, B.E.; Jimenez, C.A.; Hanamornroongruang, S.; McKeon, F.D.; Xian, W. Through the glass darkly: Intraepithelial neoplasia, top-down differentiation, and the road to ovarian cancer. J. Pathol. 2013, 231, 402–412. [Google Scholar] [CrossRef] [Green Version]
- Akahane, T.; Masuda, K.; Hirasawa, A.; Kobayashi, Y.; Ueki, A.; Kawaida, M.; Misu, K.; Nakamura, K.; Nagai, S.; Chiyoda, T.; et al. TP53 variants in p53 signatures and the clonality of STICs in RRSO samples. J. Gynecol. Oncol. 2022, 33, e50. [Google Scholar] [CrossRef]
- Boerner, T.; Walch, H.S.; Nguyen, B.; Iasonos, A.; Zhou, Q.C.; Schultz, N.; Chui, M.H.; Grisham, R.N.; Tew, W.P.; O’Cearbhaill, R.E.; et al. Exploring the clinical significance of serous tubal intraepithelial carcinoma associated with advanced high-grade serous ovarian cancer: A Memorial Sloan Kettering Team Ovary Study. Gynecol. Oncol. 2020, 160, 696–703. [Google Scholar] [CrossRef]
- Xiang, L.; Rong, G.; Zhao, J.; Wang, Z.; Shi, F. Identification of candidate genes associated with tubal origin of high-grade serous ovarian cancer. Oncol. Lett. 2018, 15, 7769–7775. [Google Scholar] [CrossRef] [Green Version]
- Perets, R.; Wyant, G.A.; Muto, K.W.; Bijron, J.G.; Poole, B.B.; Chin, K.T.; Chen, J.Y.H.; Ohman, A.W.; Stepule, C.D.; Kwak, S.; et al. Transformation of the Fallopian Tube Secretory Epithelium Leads to High-Grade Serous Ovarian Cancer in Brca;Tp53;Pten Models. Cancer Cell 2013, 24, 751–765. [Google Scholar] [CrossRef] [Green Version]
- Zhai, Y.; Wu, R.; Kuick, R.; Sessine, M.S.; Schulman, S.; Green, M.; Fearon, E.R.; Cho, K.R. High-grade serous carcinomas arise in the mouse oviduct via defects linked to the human disease. J. Pathol. 2017, 243, 16–25. [Google Scholar] [CrossRef]
- Arentz, G.; Mittal, P.; Zhang, C.; Ho, Y.-Y.; Briggs, M.; Winderbaum, L.; Hoffmann, M.; Hoffmann, P. Applications of Mass Spectrometry Imaging to Cancer. Adv. Cancer Res. 2017, 134, 27–66. [Google Scholar] [CrossRef]
- Fischer, A.H.; Jacobson, K.A.; Rose, J.; Zeller, R. Hematoxylin and Eosin Staining of Tissue and Cell Sections. Cold Spring Harb. Protoc. 2008, 2008, pdb-prot4986. [Google Scholar] [CrossRef]
- Start, R.D.; Layton, C.M.; Cross, S.S.; Smith, J.H. Reassessment of the rate of fixative diffusion. J. Clin. Pathol. 1992, 45, 1120–1121. [Google Scholar] [CrossRef] [Green Version]
- Acland, M.; Arentz, G.; Mussared, M.; Whitehead, F.; Hoffmann, P.; Klingler-Hoffmann, M.; Oehler, M.K. Proteomic Analysis of Pre-Invasive Serous Lesions of the Endometrium and Fallopian Tube Reveals Their Metastatic Potential. Front. Oncol. 2020, 10, 523989. [Google Scholar] [CrossRef]
- Wiśniewski, J.R.; Zougman, A.; Nagaraj, N.; Mann, M. Universal sample preparation method for proteome analysis. Nat. Methods 2009, 6, 359–362. [Google Scholar] [CrossRef]
- Tyanova, S.; Temu, T.; Cox, J. The MaxQuant computational platform for mass spectrometry-based shotgun proteomics. Nat. Protoc. 2016, 11, 2301–2319. [Google Scholar] [CrossRef]
- Perez-Riverol, Y.; Csordas, A.; Bai, J.; Bernal-Llinares, M.; Hewapathirana, S.; Kundu, D.J.; Inuganti, A.; Griss, J.; Mayer, G.; Eisenacher, M.; et al. The PRIDE database and related tools and resources in 2019: Improving support for quantification data. Nucleic Acids Res. 2019, 47, D442–D450. [Google Scholar] [CrossRef]
- Gustafsson, O.J.; Eddes, J.S.; Meding, S.; McColl, S.R.; Oehler, M.K.; Hoffmann, P. Matrix-assisted laser desorption/ionization imaging protocol for in situ characterization of tryptic peptide identity and distribution in formalin-fixed tissue. Rapid Commun. Mass Spectrom. 2013, 27, 655–670. [Google Scholar] [CrossRef]
- Folkins, A.K.; Jarboe, E.A.; Saleemuddin, A.; Lee, Y.; Callahan, M.J.; Drapkin, R.; Garber, J.E.; Muto, M.G.; Tworoger, S.; Crum, C.P. A candidate precursor to pelvic serous cancer (p53 signature) and its prevalence in ovaries and fallopian tubes from women with BRCA mutations. Gynecol. Oncol. 2008, 109, 168–173. [Google Scholar] [CrossRef] [Green Version]
- Zheng, W.; Liang, S.X.; Yu, H.; Rutherford, T.; Chambers, S.K.; Schwartz, P.E. Endometrial Glandular Dysplasia: A Newly Defined Precursor Lesion of Uterine Papillary Serous Carcinoma. Part I: Morphologic Features. Int. J. Surg. Pathol. 2004, 12, 207–223. [Google Scholar] [CrossRef]
- Ricciardelli, C.; Lokman, N.; Cheruvu, S.; Tan, I.A.; Ween, M.; Pyragius, C.E.; Ruszkiewicz, A.; Hoffmann, P.; Oehler, M.K. Transketolase is upregulated in metastatic peritoneal implants and promotes ovarian cancer cell proliferation. Clin. Exp. Metastasis 2015, 32, 441–455. [Google Scholar] [CrossRef]
- Zhang, C.; Arentz, G.; Winderbaum, L.; Lokman, N.A.; Klingler-Hoffmann, M.; Mittal, P.; Carter, C.; Oehler, M.K.; Hoffmann, P. MALDI Mass Spectrometry Imaging Reveals Decreased CK5 Levels in Vulvar Squamous Cell Carcinomas Compared to the Precursor Lesion Differentiated Vulvar Intraepithelial Neoplasia. Int. J. Mol. Sci. 2016, 17, 1088. [Google Scholar] [CrossRef] [Green Version]
- Mittal, P.; Klingler-Hoffmann, M.; Arentz, G.; Winderbaum, L.; Kaur, G.; Anderson, L.; Scurry, C., Jr.; Leung, Y.; Stewart, C.J.; Carter, J.; et al. Annexin A2 and alpha actinin 4 expression correlates with metastatic potential of primary endometrial cancer. Biochim. Biophys. Acta (BBA) Proteins Proteom. 2017, 1865, 846–857. [Google Scholar] [CrossRef]
- Mittal, P.; Klingler-Hoffmann, M.; Arentz, G.; Winderbaum, L.; Lokman, N.; Zhang, C.; Anderson, L.; Scurry, J.; Leung, Y.; Stewart, C.J.; et al. Lymph node metastasis of primary endometrial cancers: Associated proteins revealed by MALDI imaging. Proteomics 2016, 16, 1793–1801. [Google Scholar] [CrossRef]
- Gustafsson, O.J.R.; Briggs, M.; Condina, M.R.; Winderbaum, L.; Pelzing, M.; McColl, S.R.; Everest-Dass, A.V.; Packer, N.H.; Hoffmann, P. MALDI imaging mass spectrometry of N-linked glycans on formalin-fixed paraffin-embedded murine kidney. Anal. Bioanal. Chem. 2014, 407, 2127–2139. [Google Scholar] [CrossRef] [Green Version]
- Briggs, M.T.; Kuliwaba, J.S.; Muratovic, D.; Everest-Dass, A.V.; Packer, N.H.; Findlay, D.M.; Hoffmann, P. MALDI mass spectrometry imaging of N -glycans on tibial cartilage and subchondral bone proteins in knee osteoarthritis. Proteomics 2016, 16, 1736–1741. [Google Scholar] [CrossRef]
- Everest-Dass, A.V.; Briggs, M.T.; Kaur, G.; Oehler, M.K.; Hoffmann, P.; Packer, N.H. N-glycan MALDI Imaging Mass Spectrometry on Formalin-Fixed Paraffin-Embedded Tissue Enables the Delineation of Ovarian Cancer Tissues. Mol. Cell Proteom. 2016, 15, 3003–3016. [Google Scholar] [CrossRef] [Green Version]
- Briggs, M.T.; Condina, M.R.; Ho, Y.Y.; Everest-Dass, A.V.; Mittal, P.; Kaur, G.; Oehler, M.K.; Packer, N.H.; Hoffmann, P. MALDI Mass Spectrometry Imaging of Early- and Late-Stage Serous Ovarian Cancer Tissue Reveals Stage-Specific N-Glycans. Proteomics 2019, 19, e1800482. [Google Scholar] [CrossRef] [Green Version]
- Briggs, M.T.; Ho, Y.Y.; Kaur, G.; Oehler, M.K.; Everest-Dass, A.V.; Packer, N.H.; Hoffmann, P. N-Glycan matrix-assisted laser desorption/ionization mass spectrometry imaging protocol for formalin-fixed paraffin-embedded tissues. Rapid Commun. Mass Spectrom. 2017, 31, 825–841. [Google Scholar] [CrossRef] [Green Version]
- Mezger, S.T.P.; Mingels, A.M.A.; Bekers, O.; Heeren, R.M.A.; Cillero-Pastor, B. Mass Spectrometry Spatial-Omics on a Single Conductive Slide. Anal. Chem. 2021, 93, 2527–2533. [Google Scholar] [CrossRef]
- Li, X.; Wang, W.; Chen, J. Recent progress in mass spectrometry proteomics for biomedical research. Sci. China Life Sci. 2017, 60, 1093–1113. [Google Scholar] [CrossRef]
- Gustafsson, J.O.; Eddes, J.S.; Meding, S.; Koudelka, T.; Oehler, M.K.; McColl, S.R.; Hoffmann, P. Internal calibrants allow high accuracy peptide matching between MALDI imaging MS and LC-MS/MS. J. Proteom. 2012, 75, 5093–5105. [Google Scholar] [CrossRef]


| Calibrants | Peptide Mass [M + H]+ | Final Concentration |
|---|---|---|
| Angiotensin I34-43 (C10-00002, BioRad, Hercules, CA, USA) | 1296.685 | 0.4 pmol/µL |
| [Glu1]-fibrinopeptide B (F3261, Sigma-Aldrich, St. Louis, MI, USA) | 1570.677 | 0.4 pmol/µL |
| Dynorphin A 1-17 (2032, Auspep, Tullamarine, Victoria, Australia) | 2147.199 | 2.0 pmol/µL |
| ACTH 1-24 (A0298, Sigma-Aldrich, St. Louis, MI, USA) | 2932.588 | 2.0 pmol/µL |
| TFA (10%) | 0.2% (v/v) | |
| Milli-Q® Water (≥18.2 MΩ) |
| Phase | Sensor | Nebulization | Incubation | Drying |
|---|---|---|---|---|
| 1 | 0.65 V within 8–20 cycles | 20% spray power ±35% modulation with fixed spray time of 2.5 s | 10 s | 90 s |
| 2 | 30 s drying | |||
| 3 | 0.1 V within 4–10 cycles | 20% spray power ± 35% modulation with 0.05 V sensor-controlled spray time | 30 s ± 30 s | Complete dry every cycle, safe dry 10 s |
| 4 | 0.1 V within 8–12 cycles | 20% spray power ± 35% modulation with 0.1 V sensor-controlled spray time | Grade 20 ± 40% complete dry every 2 cycle, safe dry 20 s | |
| 5 | 0.3 V within 12–30 cycles | 25% spray power ± 35% modulation with 0.2 V sensor-controlled spray time | Grade 30 ± 40% complete dry every 3 cycle, safe dry 30 s | |
| 6 | 0.6 ± 0.5 V within 20–64 cycles | 25% spray power ± 35% modulation with 0.3 V sensor-controlled spray time | Grade 40 ± 40% complete dry every 4 cycle, safe dry 40 s | |
| 7 | 0.6 ± 0.5 V within 20–64 cycles | 25% spray power ± 35% modulation with 0.3 V sensor-controlled spray time | Grade 40 ± 40%, complete dry every 4 cycle, safe dry 40 s | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Acland, M.; Mittal, P.; Arentz, G.; Whitehead, F.; Hoffmann, P.; Klingler-Hoffmann, M.; Oehler, M.K. A Protocol for the Acquisition of Comprehensive Proteomics Data from Single Cases Using Formalin-Fixed Paraffin Embedded Sections. Methods Protoc. 2022, 5, 57. https://doi.org/10.3390/mps5040057
Acland M, Mittal P, Arentz G, Whitehead F, Hoffmann P, Klingler-Hoffmann M, Oehler MK. A Protocol for the Acquisition of Comprehensive Proteomics Data from Single Cases Using Formalin-Fixed Paraffin Embedded Sections. Methods and Protocols. 2022; 5(4):57. https://doi.org/10.3390/mps5040057
Chicago/Turabian StyleAcland, Mitchell, Parul Mittal, Georgia Arentz, Fergus Whitehead, Peter Hoffmann, Manuela Klingler-Hoffmann, and Martin K. Oehler. 2022. "A Protocol for the Acquisition of Comprehensive Proteomics Data from Single Cases Using Formalin-Fixed Paraffin Embedded Sections" Methods and Protocols 5, no. 4: 57. https://doi.org/10.3390/mps5040057
APA StyleAcland, M., Mittal, P., Arentz, G., Whitehead, F., Hoffmann, P., Klingler-Hoffmann, M., & Oehler, M. K. (2022). A Protocol for the Acquisition of Comprehensive Proteomics Data from Single Cases Using Formalin-Fixed Paraffin Embedded Sections. Methods and Protocols, 5(4), 57. https://doi.org/10.3390/mps5040057






