Kinematic and Kinetic Gait Principal Component Domains in Older Adults With and Without Functional Disability: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Context
2.2. Sample Selection and Characterization
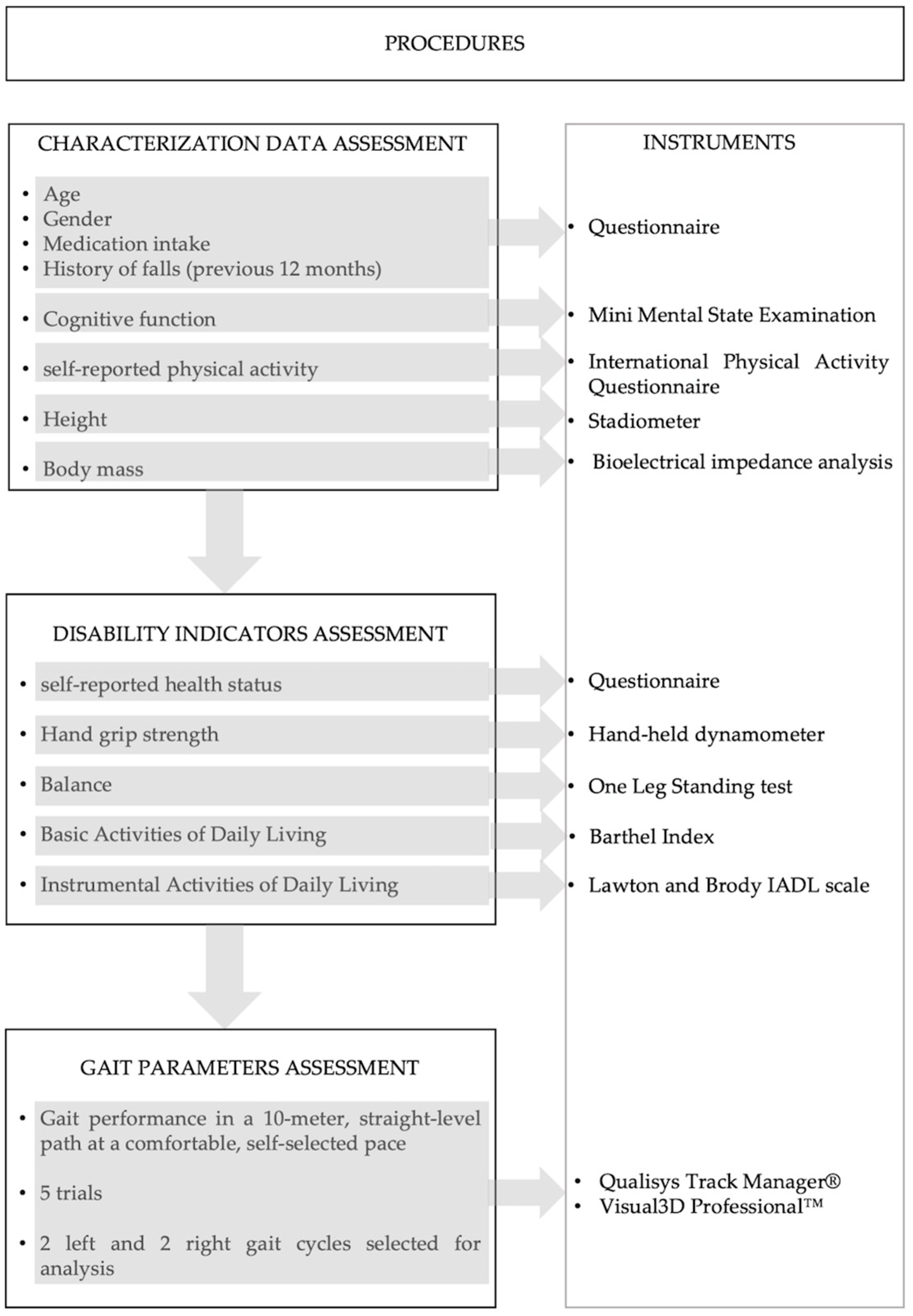
2.3. Procedures
2.4. Data Processing
2.5. Gait Parameters for PCA
| Type | Gait Outcome | Definition |
|---|---|---|
| Spatiotemporal parameters | Step length (meters) | Average distance, in meters, between the position of the right/left foot in the heel strike and the position of the left/right foot in the next heel strike [45]. |
| Step velocity (meters/second) | The calculation involves determining the length of each step divided by the corresponding step time for both the right and left sides [45]. | |
| Step time (seconds) | Average time, in seconds, between the right/left heel strike and the left/right heel strike [45]. | |
| Swing time (seconds) | Average time, in seconds, between the right/left toe-off and the right/left heel strike [45]. | |
| Stance time (seconds) | Average time, in seconds, between the right/left heel strike and the right/left toe-off [45]. | |
| Stride width (meters) | Distance between the proximal end position of the foot at ipsilateral heel strike to the proximal end position of the foot at the next ipsilateral heel strike [45]. | |
| Joint kinematics measures | Sagittal/frontal/transverse hip ROM (degrees) | Range of motion of hip, knee, and ankle angle, in sagittal/frontal/transverse plane, measured in degrees, obtained by subtracting the minimum from the maximum value along the gait cycle. |
| Sagittal/frontal/transverse knee ROM (degrees) | ||
| Sagittal/frontal/transverse ankle ROM (degrees) | ||
| Peak hip extension (degrees) | Maximum value, in degrees, of hip extension, flexion, and ankle plantar flexion along the gait cycle. | |
| Peak hip flexion (degrees) | ||
| Peak ankle plantar flexion (degrees) | ||
| Sagittal/frontal/transverse hip angle at HS (degrees) | Value, in degrees, of hip, knee, and ankle sagittal/frontal/transverse angles at the events of heel strike or toe-off. | |
| Sagittal/frontal/transverse hip angle at TO (degrees) | ||
| Sagittal/frontal/transverse knee angle at HS (degrees) | ||
| Sagittal/frontal/transverse knee angle at TO (degrees) | ||
| Sagittal/frontal/transverse ankle angle at HS (degrees) | ||
| Sagittal/frontal/transverse ankle angle at TO (degrees) | ||
| Variability measures | Step time variability (s) | The combined standard deviation of left and right steps was calculated by taking the square root of the mean variance of the left and right steps according to the formula: [46] |
| Stance time variability (s) | ||
| Swing time variability (s) | ||
| Step velocity variability (m/s) | ||
| Step length variability (m) | ||
| Asymmetry measures | Step time asymmetry (% gait cycle) | The comparison of the right side parameter to the left side parameter using the formula: [47] |
| Swing time asymmetry (% gait cycle) | ||
| Stance time asymmetry (% gait cycle | ||
| Step length asymmetry (% gait cycle) | ||
| Kinetic measures | Vertical GRF second peak (BW) | Second maximum value of vertical ground reaction force, measured in Newtons, normalized to participant mass measured in kilograms (Kg) multiplied by acceleration due to gravity (9.81 m/s2) [6,45]. |
| Anteroposterior GRF peak (BW) | Maximum value of antero-posterior ground reaction force, measured in Newtons, normalized to participant mass measured in kilograms (Kg) multiplied by acceleration due to gravity (9.81 m/s2) [48]. | |
| Ankle peak dorsiflexion moment (Nm/Kg) | Moment of force equivalent to the sum of all moments of force acting across the ankle joint, normalized to participant mass measured in kilograms (Kg) [33,45]. | |
| Sagittal peak ankle power generation (W/Kg) | The joint power was computed by multiplying the joint moments (Nm/kg) and joint angular velocities (rad/s), normalized to participant mass measured in kilograms (Kg) [45]. |
2.6. Data Analysis
2.7. Ethical Considerations
3. Results
3.1. Sample Characterization
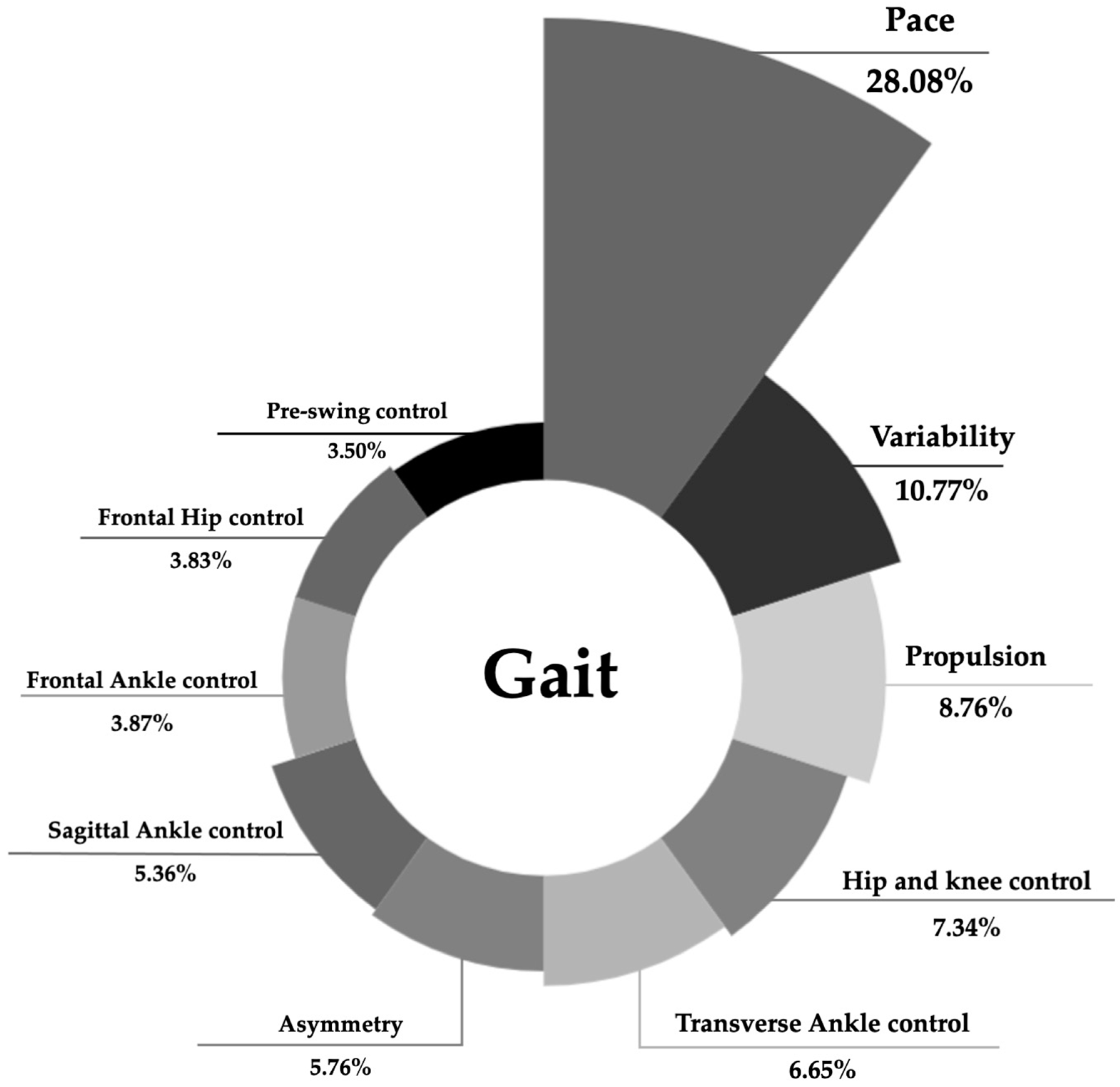
3.2. PCA Primary Models
3.3. Comprehensive Model of Gait of Older Adults and Differences Between Those with and Without Functional Disability
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ADL | Activities of Daily Living |
| GRF | Ground reaction force |
| HS | Heel strike |
| IADL | Instrumental Activities of Daily Living |
| IPAQ | International Physical Activity Questionnaire |
| KMO | Kaiser–Meyer–Olkin |
| MMSE | Mini-Mental State Examination |
| N | Newton |
| OLST | One-Leg Standing Test |
| PC | Principal components |
| PCA | Principal Component Analysis |
| PCM | Principal Component Model |
| ROM | Range of motion |
| SD | Standard deviation |
| SRH | Self-reported health |
| TO | Toe-off |
References
- Tieland, M.; Trouwborst, I.; Clark, B.C. Skeletal muscle performance and ageing. J. Cachexia Sarcopenia Muscle 2018, 9, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Jazwinski, S.M.; Kim, S. Examination of the Dimensions of Biological Age. Front. Genet. 2019, 10, 263. [Google Scholar] [CrossRef] [PubMed]
- Chung, E.; Lee, S.H.; Lee, H.J.; Kim, Y.H. Comparative study of young-old and old-old people using functional evaluation, gait characteristics, and cardiopulmonary metabolic energy consumption. BMC Geriatr. 2023, 23, 400. [Google Scholar] [CrossRef]
- Kowalski, E.; Catelli, D.S.; Lamontagne, M. Gait variability between younger and older adults: An equality of variance analysis. Gait Posture 2022, 95, 176–182. [Google Scholar] [CrossRef]
- Chiu, M.C.; Wu, H.C.; Chang, L.Y.; Wu, M.H. Center of pressure progression characteristics under the plantar region for elderly adults. Gait Posture 2013, 37, 408–412. [Google Scholar] [CrossRef]
- Boyer, K.A.; Johnson, R.T.; Banks, J.J.; Jewell, C.; Hafer, J.F. Systematic review and meta-analysis of gait mechanics in young and older adults. Exp. Gerontol. 2017, 95, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Pol, F.; Baharlouei, H.; Taheri, A.; Menz, H.B.; Forghany, S. Foot and ankle biomechanics during walking in older adults: A systematic review and meta-analysis of observational studies. Gait Posture 2021, 89, 14–24. [Google Scholar] [CrossRef]
- Figueiredo, J.; Santos, C.P.; Moreno, J.C. Automatic recognition of gait patterns in human motor disorders using machine learning: A review. Med. Eng. Phys. 2018, 53, 1–12. [Google Scholar] [CrossRef]
- Guzelbulut, C.; Suzuki, K.; Shimono, S. Singular value decomposition-based gait characterization. Heliyon 2022, 8, e12006. [Google Scholar] [CrossRef]
- Hagoort, I.; Vuillerme, N.; Hortobágyi, T.; Lamoth, C.J.C. Age and walking conditions differently affect domains of gait. Hum. Mov. Sci. 2023, 89, 103075. [Google Scholar] [CrossRef]
- Moreira, J.; Silva, B.; Faria, H.; Santos, R.; Sousa, A.S.P. Systematic Review on the Applicability of Principal Component Analysis for the Study of Movement in the Older Adult Population. Sensors 2023, 23, 205. [Google Scholar] [CrossRef] [PubMed]
- Lord, S.; Galna, B.; Verghese, J.; Coleman, S.; Burn, D.; Rochester, L. Independent domains of gait in older adults and associated motor and nonmotor attributes: Validation of a factor analysis approach. J. Gerontol. A Biol. Sci. Med. Sci. 2013, 68, 820–827. [Google Scholar] [CrossRef] [PubMed]
- Hollman, J.H.; McDade, E.M.; Petersen, R.C. Normative spatiotemporal gait parameters in older adults. Gait Posture 2011, 34, 111–118. [Google Scholar] [CrossRef]
- Verghese, J.; Robbins, M.; Holtzer, R.; Zimmerman, M.; Wang, C.; Xue, X.; Lipton, R.B. Gait dysfunction in mild cognitive impairment syndromes. J. Am. Geriatr. Soc. 2008, 56, 1244–1251. [Google Scholar] [CrossRef] [PubMed]
- Abdul Jabbar, K.; Seah, W.T.; Lau, L.K.; Pang, B.W.; Ng, D.H.; Tan, Q.L.; Chen, K.K.; Mallya Ullal, J.; Ng, T.P.; Wee, S.L. Fast gait spatiotemporal parameters in adults and association with muscle strength—The Yishun study. Gait Posture 2021, 85, 217–223. [Google Scholar] [CrossRef]
- Perera, S.; Patel, K.V.; Rosano, C.; Rubin, S.M.; Satterfield, S.; Harris, T.; Ensrud, K.; Orwoll, E.; Lee, C.G.; Chandler, J.M.; et al. Gait Speed Predicts Incident Disability: A Pooled Analysis. J. Gerontol. A Biol. Sci. Med. Sci. 2016, 71, 63–71. [Google Scholar] [CrossRef]
- Artaud, F.; Singh-Manoux, A.; Dugravot, A.; Tzourio, C.; Elbaz, A. Decline in Fast Gait Speed as a Predictor of Disability in Older Adults. J. Am. Geriatr. Soc. 2015, 63, 1129–1136. [Google Scholar] [CrossRef]
- Elm, E.v.; Altman, D.; Egger, M.; Pocock, S.; Gøtzsche, P.; Vandenbroucke, J. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. J. Clin. Epidemiol. 2008, 61, 806–808. [Google Scholar] [CrossRef]
- Moreira, J.S.; Melo, A.; Santos, R.; Sousa, A.S.P. Indicators and Instruments to Assess Components of Disability in Community-Dwelling Older Adults: A Systematic Review. Sensors 2022, 22, 8270. [Google Scholar] [CrossRef]
- Lee, E.A.; Brettler, J.W.; Kanter, M.H.; Steinberg, S.G.; Khang, P.; Distasio, C.C.; Martin, J.; Dreskin, M.; Thompson, N.H.; Cotter, T.M.; et al. Refining the Definition of Polypharmacy and Its Link to Disability in Older Adults: Conceptualizing Necessary Polypharmacy, Unnecessary Polypharmacy, and Polypharmacy of Unclear Benefit. Perm. J. 2020, 24, 212. [Google Scholar] [CrossRef]
- Folstein, M.; Folstein, S.; McHugh, P. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Morgado, J.; Rocha, C.; Maruta, C.; Guerreiro, M.; Martins, I. Novos valores normativos do Mini-Mental State Examination. Sinapse 2009, 2, 10–16. [Google Scholar]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Crimmins, E.M. Trends in the health of the elderly. Annu. Rev. Public Health 2004, 25, 79–98. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, F.; Barthel, D.W. Functional Evaluation: The Barthel Index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar]
- Araújo, F.; Ribeiro, J.; Oliveira, A.; Pinto, C. Validação do índice de Barthel numa amostra de idosos não institucionalizados. Rev. Port. Saúde de Pública 2007, 25, 59–66. [Google Scholar]
- Collin, C.; Wade, D.T.; Davies, S.; Horne, V. The Barthel ADL Index: A reliability study. Int. Disabil. Stud. 1988, 10, 61–63. [Google Scholar] [CrossRef]
- Lawton, M.P.; Brody, E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontol. 1969, 9, 179–186. [Google Scholar] [CrossRef]
- Araújo, F.; Ribeiro, J.P.; Oliveira, A.; Pinto, C.; Martins, T. Validação da escala de Lawton e Brody numa amostra de idosos não institucionalizados. In Actas do 7° Congresso Nacional de Psicologia da Saúde; ISPA: Lisbon, Portugal, 2008; pp. 217–220. [Google Scholar]
- Jansen, C.W.S.; Niebuhr, B.R.; Coussirat, D.J.; Hawthorne, D.; Moreno, L.; Phillip, M. Hand force of men and women over 65 years of age as measured by maximum pinch and grip force. J. Aging Phys. Act. 2008, 16, 24–41. [Google Scholar] [CrossRef]
- Furuna, T.; Nagasaki, H.; Nishizawa, S.; Sugiura, M.; Okuzumi, H.; Ito, H.; Kinugasa, T.; Hashizume, K.; Maruyama, H. Longitudinal change in the physical performance of older adults in the community. J. Jpn. Phys. Ther. Assoc. 1998, 1, 1–5. [Google Scholar] [CrossRef]
- Richards, J. The Comprehensive Textbook of Clinical Biomechanics, 2nd ed.; Elsevier: Amsterdam, The Netherlands; Churchill Livingstone: London, UK, 2018. [Google Scholar]
- Gordon, D.; Robertson, E.; Caldwell, G.E.; Hamill, J.; Kamen, G.; Whittlesey, S.N. Research Methods in Biomechanics, 2nd ed.; Human Kinetics: Champaign, IL, USA, 2014. [Google Scholar]
- Renner, K.E.; Peebles, A.T.; Socha, J.J.; Queen, R.M. The impact of sampling frequency on ground reaction force variables. J. Biomech. 2022, 135, 111034. [Google Scholar] [CrossRef]
- Leardini, A.; Sawacha, Z.; Paolini, G.; Ingrosso, S.; Nativo, R.; Benedetti, M. A new anatomically based protocol for gait analysis in children. Gait Posture 2007, 26, 560–571. [Google Scholar] [CrossRef] [PubMed]
- Leardini, A.; Biagi, F.; Merlo, A.; Belvedere, C.; Benedetti, M. Multi-segment trunk kinematics during locomotion and elementary exercises. Clin. Biomech. 2011, 26, 562–571. [Google Scholar] [CrossRef] [PubMed]
- Cappozzo, A.; Catani, F.; Croce, U.; Leardini, A. Position and orientation in space of bones during movement: Anatomical frame definition and determination. Clin. Biomech. 1995, 10, 171–178. [Google Scholar] [CrossRef] [PubMed]
- C-Motion. Marker Set Guidelines—Visual3D Wiki Documentation. Available online: https://www.c-motion.com/v3dwiki/index.php/Marker_Set_Guidelines (accessed on 1 January 2022).
- Petuskey, K.; Bagley, A.; Abdala, E.; James, M.A.; Rab, G. Upper extremity kinematics during functional activities: Three-dimensional studies in a normal pediatric population. Gait Posture 2007, 25, 573–579. [Google Scholar] [CrossRef]
- Tsuchida, W.; Kobayashi, Y.; Inoue, K.; Horie, M.; Yoshihara, K.; Ooie, T. Kinematic characteristics during gait in frail older women identified by principal component analysis. Sci. Rep. 2022, 12, 1676. [Google Scholar] [CrossRef]
- Svoboda, Z.; Bizovska, L.; Janura, M.; Kubonova, E.; Janurova, K.; Vuillerme, N. Variability of spatial temporal gait parameters and center of pressure displacements during gait in elderly fallers and nonfallers: A 6-month prospective study. PLoS ONE 2017, 12, e0171997. [Google Scholar] [CrossRef]
- Zeni, J.A., Jr.; Richards, J.G.; Higginson, J.S. Two simple methods for determining gait events during treadmill and overground walking using kinematic data. Gait Posture 2008, 27, 710–714. [Google Scholar] [CrossRef]
- Wu, G.; Siegler, S.; Allard, P.; Kirtley, C.; Leardini, A.; Rosenbaum, D.; Whittle, M.; D’Lima, D.D.; Cristofolini, L.; Witte, H.; et al. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—Part I: Ankle, hip, and spine. International Society of Biomechanics. J. Biomech. 2002, 35, 543–548. [Google Scholar] [CrossRef]
- Dicharry, J. Kinematics and kinetics of gait: From lab to clinic. Clin. Sports Med. 2010, 29, 347–364. [Google Scholar] [CrossRef]
- Has-Motion. List of Tutorials. Available online: https://wiki.has-motion.com/doku.php?id=visual3d:tutorials:list_of_tutorials (accessed on 9 September 2024).
- Galna, B.; Lord, S.; Rochester, L. Is gait variability reliable in older adults and Parkinson’s disease? Towards an optimal testing protocol. Gait Posture 2013, 37, 580–585. [Google Scholar] [CrossRef] [PubMed]
- Monaghan, A.S.; Huisinga, J.M.; Peterson, D.S. The application of principal component analysis to characterize gait and its association with falls in multiple sclerosis. Sci. Rep. 2021, 11, 12811. [Google Scholar] [CrossRef] [PubMed]
- Boyer, K.A.; Andriacchi, T.P.; Beaupre, G.S. The role of physical activity in changes in walking mechanics with age. Gait Posture 2012, 36, 149–153. [Google Scholar] [CrossRef]
- Pearson, K. LIII. On lines and planes of closest fit to systems of points in space. Lond. Edinb. Dublin Philos. Mag. J. Sci. 1901, 2, 559–572. [Google Scholar] [CrossRef]
- Hair, J.; Tatham, R.; Anderson, R.; Black, W. Multivariate Data Analysis, 5th ed.; Prentice-Hall: London, UK, 1998. [Google Scholar]
- Herssens, N.; Verbecque, E.; Hallemans, A.; Vereeck, L.; Rompaey, V.V.; Saeys, W. Do Spatiotemporal Parameters and Gait Variability Differ Across the Lifespan of Healthy Adults? A Systematic Review. Gait Posture 2018, 64, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Stenum, J.; Hsu, M.M.; Pantelyat, A.Y.; Roemmich, R.T. Clinical gait analysis using video-based pose estimation: Multiple perspectives, clinical populations, and measuring change. PLoS Digit. Health 2024, 3, e0000467. [Google Scholar] [CrossRef]
- de Campos, D.d.S.F.; Shokur, S.; de Lima-Pardini, A.C.; Runfeng, M.; Bouri, M.; Coelho, D.B. Kinematics predictors of spatiotemporal parameters during gait differ by age in healthy individuals. Gait Posture 2022, 96, 216–220. [Google Scholar] [CrossRef]
- Stergiou, N.; Decker, L.M. Human movement variability, nonlinear dynamics, and pathology: Is there a connection? Hum. Mov. Sci. 2011, 30, 869–888. [Google Scholar] [CrossRef]
- Hausdorff, J.M.; Rios, D.A.; Edelberg, H.K. Gait variability and fall risk in community-living older adults: A 1-year prospective study. Arch. Phys. Med. Rehabil. 2001, 82, 1050–1056. [Google Scholar] [CrossRef]
- Brach, J.S.; Wert, D.; VanSwearingen, J.M.; Newman, A.B.; Studenski, S.A. Use of stance time variability for predicting mobility disability in community-dwelling older persons: A prospective study. J. Geriatr. Phys. Ther. 2012, 35, 112–117. [Google Scholar] [CrossRef]
- Sloot, L.H.; Malheiros, S.; Truijen, S.; Saeys, W.; Mombaur, K.; Hallemans, A.; van Criekinge, T. Decline in gait propulsion in older adults over age decades. Gait Posture 2021, 90, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Franz, J.R. The Age-Associated Reduction in Propulsive Power Generation in Walking. Exerc. Sport. Sci. Rev. 2016, 44, 129–136. [Google Scholar] [CrossRef]
- Lanza, M.B.; Arbuco, B.; Ryan, A.S.; Shipper, A.G.; Gray, V.L.; Addison, O. Systematic Review of the Importance of Hip Muscle Strength, Activation, and Structure in Balance and Mobility Tasks. Arch. Phys. Med. Rehabil. 2022, 103, 1651–1662. [Google Scholar] [CrossRef]
- Gafner, S.C.; Bastiaenen, C.H.G.; Ferrari, S.; Gold, G.; Trombetti, A.; Terrier, P.; Hilfiker, R.; Allet, L. The Role of Hip Abductor Strength in Identifying Older Persons at Risk of Falls: A Diagnostic Accuracy Study. Clin. Interv. Aging 2020, 15, 645–654. [Google Scholar] [CrossRef]
- Coyle, P.C.; Knox, P.J.; Pohlig, R.T.; Pugliese, J.M.; Sions, J.M.; Hicks, G.E. Hip Range of Motion and Strength Predict 12-Month Physical Function Outcomes in Older Adults With Chronic Low Back Pain: The Delaware Spine Studies. ACR Open Rheumatol. 2021, 3, 850–859. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Xu, T.; Qi, S.; Cao, X.; Yeung, E.H.K.; Hu, Y. Non-age-related gait kinematics and kinetics in the elderly. BMC Musculoskelet. Disord. 2022, 23, 623. [Google Scholar] [CrossRef] [PubMed]
- Schloemer, S.; Thompson, J.; Silder, A.; Thelen, D.; Siston, R. Age-Related Differences in Gait Kinematics, Kinetics, and Muscle Function: A Principal Component Analysis. Ann. Biomed. Eng. 2017, 45, 695–710. [Google Scholar] [CrossRef]
- Cesari, M.; Kritchevsky, S.B.; Newman, A.B.; Simonsick, E.M.; Harris, T.B.; Penninx, B.W.; Brach, J.S.; Tylavsky, F.A.; Satterfield, S.; Bauer, D.C.; et al. Added value of physical performance measures in predicting adverse health-related events: Results from the Health, Aging And Body Composition Study. J. Am. Geriatr. Soc. 2009, 57, 251–259. [Google Scholar] [CrossRef]
- Abe, T.; Kitamura, A.; Taniguchi, Y.; Amano, H.; Seino, S.; Yokoyama, Y.; Nishi, M.; Narita, M.; Ikeuchi, T.; Fujiwara, Y.; et al. Pathway from gait speed to incidence of disability and mortality in older adults: A mediating role of physical activity. Maturitas 2019, 123, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Asai, T.; Oshima, K.; Fukumoto, Y.; Kubo, H.; Koyama, S.; Misu, S. Changes in step time variability, not changes in step length and width, are associated with lower-trunk sway during dual-task gait in older adults. Hum. Mov. Sci. 2019, 66, 157–163. [Google Scholar] [CrossRef]
- Rojas-Valverde, D.; Pino-Ortega, J.; Gómez-Carmona, C.D.; Rico-González, M. A Systematic Review of Methods and Criteria Standard Proposal for the Use of Principal Component Analysis in Team’s Sports Science. Int. J. Environ. Res. Public Health 2020, 17, 8712. [Google Scholar] [CrossRef] [PubMed]
- Hurt, C.P.; Grabiner, M.D. Age-related differences in the maintenance of frontal plane dynamic stability while stepping to targets. J. Biomech. 2015, 48, 592–597. [Google Scholar] [CrossRef] [PubMed]
- Novak, A.; Brouwer, B. Sagittal and Frontal Lower Limb Joint Moments During Stair Ascent and Descent in Young and Older Adults. Gait Posture 2011, 33, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Tillman, M.; Liu, J.M.; Hirsch, Z.M.; Molino, J.; Zaferiou, A.M. Healthy older adults generate transverse-plane momenta required for 90° turns while walking during the same phases of gait as used in straight-line gait. J. NeuroEng. Rehabil. 2024, 21, 145. [Google Scholar] [CrossRef] [PubMed]


| Marker Acronym | Description | |
|---|---|---|
| Anterior view | L/RALH | Left/right anterior head |
| L/RCAJ | Left/right acromion | |
| SJN | Deepest point of incisura jugularis | |
| SXS | Xiphoid process, the most caudal point of the sternum | |
| L/RA 1, 2, 3 | Left/right cluster arm 1, 2, 3 | |
| L/RFA 1, 2, 3 | Left/right cluster forearm 1, 2, 3 | |
| L/RRAD | Left/right radio-styloid process | |
| L/RULN | Left/right ulna-styloid process | |
| L/RIAS | Left/right anterior superior iliac spine | |
| L/RFTC | Most lateral prominence of the greater trochanter | |
| L/RTH 1, 2, 3, 4 | Left/right cluster thigh 1, 2, 3, 4 | |
| L/RFLE | Most lateral prominence of the lateral femoral epicondyle | |
| L/RFME | Most medial prominence of the medial femoral epicondyle | |
| L/RFAX | Proximal tip of the head of the fibula | |
| L/RTTC | Most anterior border of the tibial tuberosity | |
| L/RSK 1, 2, 3, 4 | Left/right cluster shank 1, 2, 3, 4 | |
| L/RFAL | Lateral prominence of the lateral malleolus | |
| L/RTAM | Most medial prominence of the medial malleolus | |
| L/RFM5 | Dorsal margin of the fifth metatarsal head | |
| L/RFM2 | Dorsal aspect of the second metatarsal head | |
| L/RFM1 | Dorsal margin of the first metatarsal head | |
| L/RDR | Left/right distal radius | |
| L/RDU | Left/right distal ulna | |
| Posterior View | L/RPH | Left/right posterior head |
| CV7 | Spinous process of the seventh cervical vertebra | |
| TV2 | Second thoracic vertebra | |
| TV7 | Midpoint between the inferior angles of the two scapulae | |
| LV1 | First lumbar vertebra | |
| LV3 | Third lumbar vertebra | |
| LV5 | Fifth lumbar vertebra | |
| L/RIPS | Left/right posterior superior iliac spine | |
| L/RFCC | Aspect of the achilles tendon insertion on the calcaneous | |
| L/RLELB | Left/right lateral epicondyle of humerous | |
| L/RMELB | Left/right medial epicondyle of humerous | |
| L/RMH | Left/right medial head of fifth metacarpal | |
| L/RLH | Left/right lateral head of fifth metacarpal |
| Demographic and Clinical Data | ND (n = 35) | D (n = 25) | p-Value (Test Value) | |
|---|---|---|---|---|
| Age (years) | 66.34 ± 5.60 | 68.60 ± 6.77 | 0.147(534) (a) | |
| Gender (n female; %) | 19; 54.29 | 19; 76 | 0.085(2.961) (b) | |
| BMI (kg/m2) | 25.22 ± 3.08 | 26.02 ± 2.66 | 0.298(−1.049) (c) | |
| History of the fall, previous 12 months (n fallers/%) | 11 (31.4) | 11 (44) | 0.469(0.525) (b) | |
| Polypharmacy (n polymedicated/%) | 2 (5.71) | 11 (44) | <0.001(12.595) (b) | |
| Cognitive function (MMSE score) | 28.94 ± 1.31 | 28.68 ± 1.49 | 0.495(394) (a) | |
| Self-reported physical activity (IPAQ MET-min/week) | 3186.46 ± 2964.91 | 3519.66 ± 2822.11 | 0.509 (393.5) (a) | |
| Disability indicators | ||||
| Self-reported health | poor | 8 (22.86) | 21 (84) | <0.001(21.832) (b) |
| good | 27 (77.14) | 4 (16) | ||
| Hand grip strength (kg) | 36.59 ± 39.86 | 25.07 ± 7.54 | 0.018(279.5) (a) | |
| One leg standing time (seconds) | 38.83 ± 20.93 | 18.19 ± 20.72 | <0.001(192.5) (a) | |
| ADL independence (Barthel index score) | 19.97 ± 0.17 | 19.76 ± 0.44 | 0.013(345) (a) | |
| IADL independence (Lawton and Brody score) | 23 ± 0.00 | 21.96 ± 2.67 | 0.002(332.5) (a) | |
| Principal Component | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Gait Parameters | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
| Pace | Step time | 0.882 | 0.284 | −0.224 | −0.052 | −0.172 | 0.039 | 0.112 | 0.048 | −0.095 | −0.022 |
| Stance time | 0.862 | 0.29 | −0.28 | −0.049 | −0.182 | 0.024 | 0.074 | 0.057 | −0.076 | 0.056 | |
| Swing time | 0.81 | 0.308 | −0.086 | −0.067 | −0.13 | 0.111 | 0.178 | 0.031 | −0.117 | −0.208 | |
| Step velocity | −0.698 | −0.291 | 0.487 | −0.083 | 0.147 | 0.125 | −0.208 | −0.06 | −0.033 | −0.122 | |
| Variability | Step time variability | 0.362 | 0.865 | −0.171 | 0.066 | −0.169 | 0.008 | 0.078 | 0.067 | −0.014 | 0.103 |
| Stance time variability | 0.357 | 0.853 | −0.169 | 0.076 | −0.229 | 0.01 | 0.091 | 0.072 | −0.015 | 0.063 | |
| Swing time variability | 0.39 | 0.793 | −0.184 | 0.007 | −0.069 | 0.037 | −0.019 | 0.006 | −0.012 | 0.127 | |
| Step velocity variability | −0.02 | 0.771 | −0.281 | −0.026 | 0.03 | −0.032 | 0.209 | 0.153 | 0.142 | −0.116 | |
| Propulsion | Sagittal peak ankle power | −0.179 | −0.247 | 0.829 | 0.044 | 0.162 | 0.011 | −0.053 | 0.05 | 0.003 | 0.075 |
| Vertical GRF second peak | −0.303 | −0.148 | 0.749 | 0.025 | −0.023 | −0.122 | −0.074 | −0.019 | −0.123 | −0.21 | |
| AP GRF peak | −0.402 | −0.29 | 0.714 | −0.031 | 0.214 | 0.007 | −0.066 | −0.015 | 0.065 | 0.04 | |
| Sagittal ankle ROM | 0.2 | −0.044 | 0.59 | 0.202 | 0.343 | 0.07 | −0.374 | 0.121 | 0.07 | 0.354 | |
| Hip and knee control | Transverse hip angle at TO | −0.056 | 0.086 | 0.068 | 0.903 | 0.154 | −0.008 | −0.103 | 0.108 | 0.064 | 0.018 |
| Transverse hip angle at HS | −0.104 | −0.017 | 0.164 | 0.845 | −0.015 | −0.117 | −0.085 | 0.031 | 0.171 | −0.019 | |
| Frontal knee angle at TO | 0.018 | 0.027 | −0.23 | 0.801 | −0.058 | 0.048 | −0.055 | −0.002 | −0.265 | 0.078 | |
| Sagittal knee ROM | −0.161 | −0.283 | 0.402 | −0.481 | 0.365 | −0.016 | −0.117 | −0.021 | −0.151 | 0.055 | |
| Transverse ankle control | Transverse ankle angle at TO | −0.173 | −0.136 | 0.187 | 0.011 | 0.871 | 0.073 | −0.048 | −0.158 | −0.074 | 0.015 |
| Transverse ankle angle at HS | −0.136 | −0.124 | 0.059 | −0.136 | 0.867 | −0.025 | 0.002 | −0.262 | −0.209 | −0.005 | |
| Transverse knee angle at TO | 0.231 | 0.112 | −0.131 | −0.477 | −0.676 | −0.004 | 0.071 | 0.025 | −0.149 | −0.136 | |
| Asymmetry | Swing time asymmetry | 0.092 | −0.135 | −0.016 | 0 | 0.126 | 0.878 | 0.262 | 0.028 | 0.012 | 0.029 |
| Step time asymmetry | −0.151 | 0 | −0.063 | −0.138 | 0.057 | 0.873 | −0.04 | −0.058 | −0.18 | 0.053 | |
| Stance time asymmetry | 0.069 | 0.39 | 0.064 | 0.127 | −0.255 | 0.704 | 0.183 | −0.029 | 0.039 | −0.02 | |
| Transverse hip ROM | 0.419 | −0.064 | 0.004 | −0.064 | 0.033 | 0.488 | −0.137 | 0.038 | −0.021 | −0.07 | |
| Sagittal ankle control | Ankle peak plantar flexion | 0.125 | 0.1 | −0.181 | −0.171 | −0.082 | 0.11 | 0.918 | 0.07 | −0.063 | 0.041 |
| Sagittal ankle angle at TO | 0.184 | 0.167 | −0.072 | −0.071 | −0.013 | 0.134 | 0.895 | 0.112 | −0.041 | 0.185 | |
| Frontal ankle control | Frontal ankle angle at HS | 0.011 | 0.058 | 0.112 | −0.013 | −0.142 | 0.003 | 0.006 | 0.951 | −0.102 | 0.034 |
| Frontal ankle angle at TO | 0.122 | 0.147 | −0.1 | 0.134 | −0.224 | −0.034 | 0.171 | 0.895 | 0.093 | −0.036 | |
| Frontal hip control | Frontal hip angle at TO | −0.028 | 0.117 | −0.064 | 0.118 | 0.014 | −0.037 | −0.043 | −0.054 | 0.892 | −0.157 |
| Frontal hip angle at HS | −0.193 | −0.071 | 0.007 | −0.117 | −0.252 | −0.131 | −0.07 | 0.039 | 0.792 | 0.241 | |
| Pre-swing control | Ankle peak dorsiflexion moment | −0.066 | −0.162 | 0.035 | −0.164 | −0.12 | 0.04 | −0.306 | −0.001 | 0.031 | −0.733 |
| Frontal hip ROM | −0.306 | −0.196 | 0.466 | −0.152 | −0.15 | 0.055 | −0.119 | −0.108 | −0.034 | 0.569 | |
| Hip peak extension | −0.228 | 0.168 | −0.284 | −0.455 | 0.079 | 0.146 | 0.051 | 0.153 | 0.236 | 0.47 | |
| p-value of PC scores comparison | 0.005 * | 0.725 | 0.297 | 0.816 | 0.702 | 0.770 | 0.946 | 0.534 | 0.004 * | 0.946 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moreira, J.; Cunha, B.; Félix, J.; Santos, R.; Sousa, A.S.P. Kinematic and Kinetic Gait Principal Component Domains in Older Adults With and Without Functional Disability: A Cross-Sectional Study. J. Funct. Morphol. Kinesiol. 2025, 10, 140. https://doi.org/10.3390/jfmk10020140
Moreira J, Cunha B, Félix J, Santos R, Sousa ASP. Kinematic and Kinetic Gait Principal Component Domains in Older Adults With and Without Functional Disability: A Cross-Sectional Study. Journal of Functional Morphology and Kinesiology. 2025; 10(2):140. https://doi.org/10.3390/jfmk10020140
Chicago/Turabian StyleMoreira, Juliana, Bruno Cunha, José Félix, Rubim Santos, and Andreia S. P. Sousa. 2025. "Kinematic and Kinetic Gait Principal Component Domains in Older Adults With and Without Functional Disability: A Cross-Sectional Study" Journal of Functional Morphology and Kinesiology 10, no. 2: 140. https://doi.org/10.3390/jfmk10020140
APA StyleMoreira, J., Cunha, B., Félix, J., Santos, R., & Sousa, A. S. P. (2025). Kinematic and Kinetic Gait Principal Component Domains in Older Adults With and Without Functional Disability: A Cross-Sectional Study. Journal of Functional Morphology and Kinesiology, 10(2), 140. https://doi.org/10.3390/jfmk10020140









