Functional Anatomy in Knee Osteoarthritis: Patellofemoral Joint vs. Tibiofemoral Joint
Abstract
:1. Introduction
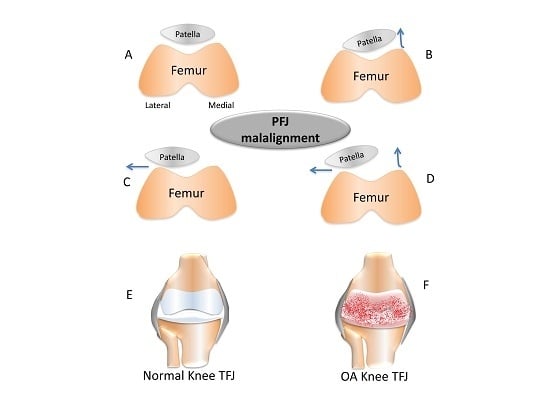
2. Short Overview of Patellofemoral Joint vs. Tibiofemoral Joint in the Osteoarthritis (OA) Process
3. Conclusions
Acknowledgments
Conflicts of Interest
References
- Castrogiovanni, P.; Musumeci, G. Which is the best physical treatment for osteoarthritis? J. Funct. Morphol. Kinesiol. 2016, 1, 54–68. [Google Scholar] [CrossRef]
- Warner, S.C.; Valdes, A.M. The genetics of osteoarthritis: A review. J. Funct. Morphol. Kinesiol. 2016, 1, 140–153. [Google Scholar] [CrossRef]
- Musumeci, G.; Szychlinska, M.A.; Mobasheri, A. Age-related degeneration of articular cartilage in the pathogenesis of osteoarthritis: Molecular markers of senescent chondrocytes. Histol. Histopathol. 2015, 30, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Mobasheri, A.; Matta, C.; Zákány, R.; Musumeci, G. Chondrosenescence: Definition, hallmarks and potential role in the pathogenesis of osteoarthritis. Maturitas 2015, 80, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Musumeci, G.; Loreto, C.; Carnazza, M.L.; Strehin, I.; Elisseeff, J. OA cartilage derived chondrocytes encapsulated in poly (ethylene glycol) diacrylate (PEGDA) for the evaluation of cartilage restoration and apoptosis in an in vitro model. Histol. Histopathol. 2011, 26, 1265–1278. [Google Scholar] [PubMed]
- Musumeci, G.; Castrogiovanni, P.; Leonardi, R.; Trovato, F.M.; Szychlinska, M.A.; di Giunta, A.; Loreto, C.; Castorina, S. Knee osteoarthritis. New perspectives for articular cartilage repair treatment through tissue engineering. A contemporary review. World J. Orthop. 2014, 5, 80–88. [Google Scholar] [CrossRef] [PubMed]
- Musumeci, G.; Loreto, C.; Imbesi, R.; Trovato, F.M.; di Giunta, A.; Lombardo, C.; Castorina, S.; Castrogiovanni, P. Advantages of exercise in rehabilitation, treatment and prevention of altered morphological features in knee osteoarthritis. A narrative review. Histol. Histopathol. 2014, 29, 707–719. [Google Scholar] [PubMed]
- Martel-Pelletier, J. Pathophysiology of osteoarthritis. Osteoarthr. Cartil. 2004, 12, 31–33. [Google Scholar] [CrossRef]
- Hinman, R.S.; Crossley, K.M. Patellofemoral joint osteoarthritis: An important subgroup of knee osteoarthritis. Rheumatology 2007, 46, 1057–1062. [Google Scholar] [CrossRef] [PubMed]
- Altman, R.; Asch, E.; Bloch, D.; Bole, G.; Borenstein, D.; Brandt, K.; Christy, W.; Cooke, T.D.; Greenwald, R.; Hochberg, M.; et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Arthritis Rheum. 1986, 29, 1039–1049. [Google Scholar] [CrossRef] [PubMed]
- Duncan, R.; Hay, E.; Saklatvala, J.; Croft, P. Prevalence of radiographic osteoarthritis: It all depends on your point of view. Rheumatology 2006, 45, 757–760. [Google Scholar] [CrossRef] [PubMed]
- McAlindon, T.E.; Snow, S.; Cooper, C.; Dieppe, P.A. Radiographic patterns of osteoarthritis of the knee joint in the community: The importance of the patellofemoral joint. Ann. Rheum. Dis. 1992, 51, 844–849. [Google Scholar] [CrossRef] [PubMed]
- Hunter, D.; March, L.; Sambrook, P. The association of cartilage volume with knee pain. Osteoarthr. Cartil. 2003, 11, 725–729. [Google Scholar] [CrossRef]
- Eckstein, F.; Lemberger, B.; Gratzke, C.; Hudelmaier, M.; Glaser, C.; Englmeier, K.H.; Reiser, M. In vivo cartilage deformation after different types of activity and its dependence on physical training status. Ann. Rheum. Dis. 2005, 64, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Sharif, M.; Granell, R.; Johansen, J.; Clarke, S.; Elson, C.; Kirwan, J.R. Serum cartilage oligomeric matrix protein and other biomarker profiles in tibiofemoral and patellofemoral osteoarthritis of the knee. Rheumatology 2006, 45, 522–526. [Google Scholar] [CrossRef] [PubMed]
- Cooper, C.; McAlindon, T.; Snow, S.; Vines, K.; Young, P.; Kirwan, J.; Dieppe, P. Mechanical and constitutional factors for symptomatic knee osteoarthritis: Differences between medial and patellofemoral joint disease. J. Rheumatol. 1994, 21, 307–313. [Google Scholar] [PubMed]
- Cicuttini, F.M.; Spector, T.; Baker, J. Risk factors for osteoarthritis in the tibiofemoral and patellofemoral joints of the knee. J. Rheumatol. 1997, 24, 1164–1167. [Google Scholar] [PubMed]
- Ledingham, J.; Regan, M.; Jones, A.; Doherty, M. Radiographic patterns and associations of osteoarthritis of the knee in patients referred to hospital. Ann. Rheum. Dis. 1993, 52, 520–526. [Google Scholar] [CrossRef] [PubMed]
- Kerrigan, D.; Lelas, J.; Goggins, J.; Merriman, G.; Kaplan, R.; Felson, D. Effectiveness of a lateral-wedge insole on knee varus torque in patients with knee osteoarthritis. Arch. Phys. Med. Rehabil. 2002, 83, 889–893. [Google Scholar] [CrossRef] [PubMed]
- Pollo, F.; Otis, J.; Backus, S.; Warren, R.; Wickiewicz, T. Reduction of medial compartment loads with valgus bracing of the osteoarthritic knee. Am. J. Sports Med. 2002, 30, 414–421. [Google Scholar] [PubMed]
- O’Reilly, S.C.; Jones, A.; Muir, K.R.; Doherty, M. Quadriceps weakness in knee osteoarthritis: The effect on pain and disability. Ann. Rheum. Dis. 1998, 57, 588–594. [Google Scholar] [CrossRef] [PubMed]
- Slemenda, C.; Heilman, D.; Brandt, K.; Katz, B.P.; Mazzuca, S.A.; Braunstein, E.M.; Byrd, D. Reduced quadriceps strength relative to body weight: A risk factor for knee osteoarthritis in women? Arthritis Rheum. 1998, 41, 1951–1959. [Google Scholar] [CrossRef]
- Thorstensson, C.; Petersson, I.; Jacobsson, L.; Boegard, T.; Roos, E. Reduced functional performance in the lower extremity predicted radiographic knee osteoarthritis five years later. Ann. Rheum. Dis. 2004, 63, 402–407. [Google Scholar] [CrossRef] [PubMed]
- Baker, K.; Xu, L.; Zhang, Y.; Nevitt, M.; Niu, J.; Aliabadi, P.; Yu, W.; Felson, D. Quadriceps weakness and its relationship to tibiofemoral and patellofemoral knee osteoarthritis in Chinese. The Beijing osteoarthritis study. Arthritis Rheum. 2004, 50, 1815–1821. [Google Scholar] [CrossRef] [PubMed]
- Tanamas, S.; Hanna, F.S.; Cicuttini, F.M.; Wluka, A.E.; Berry, P.; Urquhart, D.M. Does knee malalignment increase the risk of development and progression of kneeosteoarthritis? A systematic review. Arthritis Rheum. 2009, 61, 459–467. [Google Scholar] [CrossRef] [PubMed]
- Brouwer, G.M.; van Tol, A.W.; Bergink, A.P.; Belo, J.N.; Bernsen, R.M.; Reijman, M.; Pols, H.A.; Bierma-Zeinstra, S.M. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis Rheum. 2007, 56, 1204–1211. [Google Scholar] [CrossRef] [PubMed]
- Musumeci, G. Effects of exercise on physical limitations and fatigue in rheumatic diseases. World J. Orthop. 2015, 6, 762–769. [Google Scholar] [CrossRef] [PubMed]
- Castrogiovanni, P.; di Giunta, A.; Guglielmino, C.; Roggio, F.; Romeo, D.; Fidone, F.; Imbesi, R.; Loreto, C.; Castorina, S.; Musumeci, G. The effects of exercise and kinesio tape on physical limitations in patients with knee osteoarthritis. J. Funct. Morphol. Kinesiol. 2016, 1, 355–368. [Google Scholar] [CrossRef]
- Musumeci, G. Could cupping therapy be used to improve sports performance? J. Funct. Morphol. Kinesiol. 2016, 1, 373–377. [Google Scholar] [CrossRef]

© 2017 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Musumeci, G. Functional Anatomy in Knee Osteoarthritis: Patellofemoral Joint vs. Tibiofemoral Joint. J. Funct. Morphol. Kinesiol. 2017, 2, 8. https://doi.org/10.3390/jfmk2010008
Musumeci G. Functional Anatomy in Knee Osteoarthritis: Patellofemoral Joint vs. Tibiofemoral Joint. Journal of Functional Morphology and Kinesiology. 2017; 2(1):8. https://doi.org/10.3390/jfmk2010008
Chicago/Turabian StyleMusumeci, Giuseppe. 2017. "Functional Anatomy in Knee Osteoarthritis: Patellofemoral Joint vs. Tibiofemoral Joint" Journal of Functional Morphology and Kinesiology 2, no. 1: 8. https://doi.org/10.3390/jfmk2010008
APA StyleMusumeci, G. (2017). Functional Anatomy in Knee Osteoarthritis: Patellofemoral Joint vs. Tibiofemoral Joint. Journal of Functional Morphology and Kinesiology, 2(1), 8. https://doi.org/10.3390/jfmk2010008