Sleep Deprivation and Physiological Responses. A Case Report
Abstract
:1. Introduction
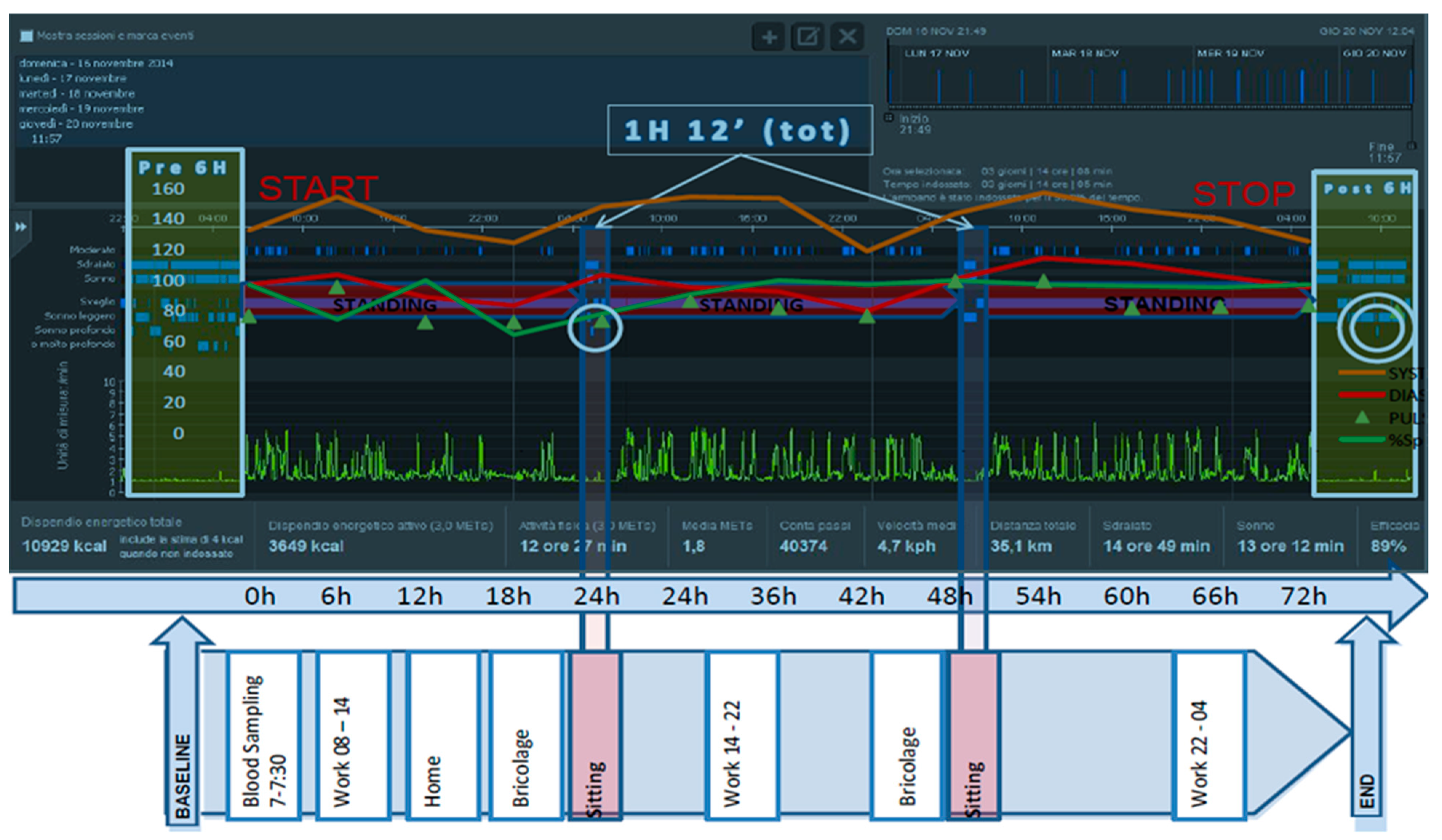
2. Materials and Methods
- An abbreviated 30-item version of the Profile of Mood States (POMS) was used for measuring mood [41]. Respondents must complete the POMS questionnaire by rating each item on a 5-point Likert scale, ranging from ‘Not at all’ to ‘Extremely’. Internal consistency is extremely high (r = 0.90). Items form six separate subscales: Tension-anxiety (T), depression–dejection (D), anger–hostility (A), vigor–activity (V), fatigue–inertia (F) and confusion–bewilderment (C). The subscale scores may be combined to form an overall measure of effect that is labeled as total mood disturbance (Global score).
- The Psychological Stress Measure (PSM) was used to measure a global index of the state of psychological stress [42]. The PSM is a 49-item self-report paper and pencil questionnaire. Internal consistency is approximately 0.95. The subject was asked to answer questions about his/her psychological stress condition using a 4-point scale (very much = 4, much = 3, little = 2, none = 1).
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Terzano, M.G.; Parrino, L.; Spaggiari, M.C. The cyclic alternating pattern sequences in the dynamic organization of sleep. Electroencephalogr. Clin. Neurophysiol. 1988, 69, 437–447. [Google Scholar] [CrossRef]
- Spiegel, K.; Leproult, R.; Van Cauter, E. Impact of sleep debt on physiological rhythms. Rev. Neurol. 2003, 159, 6S11-20. [Google Scholar] [PubMed]
- Berger, R.J.; Oswald, I. Effects of sleep deprivation on behaviour, subsequent sleep, and dreaming. J. Ment. Sci. 1962, 108, 457–465. [Google Scholar] [CrossRef]
- Webb, W.B.; Agnew, H.W. Stage 4 sleep: Influence of time course variables. Science 1971, 174, 1354–1356. [Google Scholar] [CrossRef]
- Williams, H.L.; Hammack, J.T.; Daly, R.L.; Dement, W.C.; Lubin, A. Responses to auditory stimulation, sleep loss and the EEG stages of sleep. Electroencephalogr. Clin. Neurophysiol. 1964, 16, 269–279. [Google Scholar] [CrossRef]
- Moses, J.M.; Johnson, L.C.; Naitoh, P.; Lubin, A. Sleep stage deprivation and total sleep loss: Effects on sleep behavior. Psychophysiology 1975, 12, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Nakazawa, Y.; Kotorii, M.; Oshima, M.; Kotorii, T.; Hasuzawa, H. Changes in sleep pattern after sleep deprivation. Folia Psychiatr. Neurol. Jap. 1978, 32, 85–93. [Google Scholar] [CrossRef]
- Reite, M.L.; Rhodes, J.M.; Kavan, E.; Adey, W.R. Normal sleep patterns in macaque monkey. Arch. Neurol. 1965, 12, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Crowley, T.J.; Kripke, D.F.; Haiberg, F.; Pegram, G.V.; Schildkraut, J.J. Circadian rhythms of Macaca mulatta: Sleep, EEG, body and eye movement, and temperature. Primates 1972, 13, 149–168. [Google Scholar] [CrossRef]
- Ursin, R. Differential effect of sleep deprivation on the two slow wave sleep stages in the cat. Acta Physiol. Scand. 1971, 83, 352–361. [Google Scholar] [CrossRef] [PubMed]
- Pappenheimer, J.R.; Koski, G.; Fencl, V.; Karnovsky, M.L.; Krueger, J. Extraction of sleep-promoting factor S from cerebrospinal fluid and from brains of sleep-deprived animals. J. Neurophysiol. 1975, 38, 1299–1311. [Google Scholar] [CrossRef]
- Takahashi, Y.; Ebihara, S.; Nakamura, Y.; Takahashi, K. Temporal distributions of delta wave sleep and REM sleep during recovery sleep after 12-h forced wakefulness in dogs; similarity to human sleep. Neurosci. Lett. 1978, 10, 329–334. [Google Scholar] [CrossRef]
- Borbly, A.A.; Tobler, I. The search for an endogenous “sleep-substance”. Trends Pharmacol. Sci. 1980, 1, 356–358. [Google Scholar] [CrossRef]
- Jennings, J.R.; Monk, T.H.; van der Molen, M.W. Sleep deprivation influences some but not all processes of supervisory attention. Psychol. Sci. 2003, 14, 473–479. [Google Scholar] [CrossRef] [PubMed]
- Vaara, J.P.; Oksanen, H.; Kyröläinen, H.; Virmavirta, M.; Koski, H.; Finni, T. 60-Hour Sleep Deprivation Affects Submaximal but Not Maximal Physical Performance. Front. Physiol. 2018, 9, 1437. [Google Scholar] [CrossRef]
- Bruce, J.M. Effect of sleep deprivation on tolerance of prolonged exercise. Eur. J. Appl. Physiol. Occup. Physiol. 1981, 47, 345–354. [Google Scholar] [CrossRef]
- Martin, B.J. Sleep deprivation and exercise. Exerc. Sport Sci. Rev. 1986, 14, 213–229. [Google Scholar] [PubMed]
- Martin, B.J.; Gaddis, G.M. Exercise after sleep deprivation. Med. Sci. Sports Exerc. 1981, 13, 220–223. [Google Scholar] [CrossRef] [Green Version]
- Reilly, T.; Deykin, T. Effects of partial sleep loss on subjective states, psychomotor and physical performance tests. J. Hum. Mov. Stud. 1983, 9, 157–170. [Google Scholar]
- Samuels, C. Sleep, recovery, and performance: The new frontier in high-performance athletics. Neurol. Clin. 2008, 26, 169–180. [Google Scholar] [CrossRef] [PubMed]
- VanHelder, T.; Radomski, M.W. Sleep deprivation and the effect on exercise performance. Sports Med. 1989, 7, 235–247. [Google Scholar] [CrossRef]
- Babkoff, H.; Genser, S.G.; Sing, H.C.; Thorne, D.R.; Hegge, F.W. The effects of progressive sleep loss on a lexical decision task: Response lapses and response accuracy. Behav. Res. Methods Instrum. Comput. 1985, 17, 614–622. [Google Scholar] [CrossRef] [Green Version]
- Fullagar, H.H.K.; Skorski, S.; Duffield, R.; Hammes, D.; Coutts, A.J.; Meyer, T. Sleep and Athletic Performance: The Effects of Sleep Loss on Exercise Performance, and Physiological and Cognitive Responses to Exercise. Sports Med. 2015, 45, 161. [Google Scholar] [CrossRef]
- Petralia, M.C.; Perciavalle, V.; Basile, M.S.; Alagona, G.; Monaca, A.; Buscemi, A.; Coco, M. The rise of lactic acid, from a pharmacist’s laboratory to entry into the central nervous system. Sport Sci. Health 2018, 14, 455–457. [Google Scholar] [CrossRef]
- Coco, M.; Platania, S.; Castellano, S.; Sagone, E.; Ramaci, T.; Petralia, M.C.; Agati, M.; Massimino, S.; Di Corrado, D.; Guarnera, M.; et al. Memory, personality and blood lactate during a judo competition. Sport Sci. Health 2018, 1–7. [Google Scholar] [CrossRef]
- Coco, M. The brain behaves as a muscle? Neurol. Sci. 2017, 38, 1865–1868. [Google Scholar] [CrossRef] [PubMed]
- Perciavalle, V.; Blandini, M.; Fecarotta, P.; Buscemi, A.; Di Corrado, D.; Bertolo, L.; Fichera, F.; Coco, M. The role of deep breathing on stress. Neurol. Sci. 2017, 38, 451–458. [Google Scholar] [CrossRef] [PubMed]
- Perciavalle, V.; Marchetta, N.S.; Giustiniani, S.; Borbone, C.; Perciavalle, V.; Petralia, M.C.; Buscemi, A.; Coco, M. Attentive processes, blood lactate and CrossFit®. Phys. Sportsmed. 2016, 44, 403–406. [Google Scholar] [CrossRef] [PubMed]
- Perciavalle, V.; Alagona, G.; De Maria, G.; Rapisarda, G.; Costanzo, E.; Perciavalle, V.; Coco, M. Somatosensory evoked potentials and blood lactate levels. Neurol. Sci. 2015, 36, 1597–1601. [Google Scholar] [CrossRef] [PubMed]
- Coco, M.; Alagona, G.; De Maria, G.; Rapisarda, G.; Costanzo, E.; Perciavalle, V.; Perciavalle, V. Relationship of high blood lactate levels with latency of visual-evoked potentials. Neurol. Sci. 2015, 36, 541–546. [Google Scholar] [CrossRef]
- Coco, M.; Fiore, A.S.; Perciavalle, V.; Maci, T.; Petralia, M.C.; Perciavalle, V. Stress exposure and postural control in young females. Mol. Med. Rep. 2015, 11, 2135–2140. [Google Scholar] [CrossRef]
- Coco, M.; Alagona, G.; Perciavalle, V.; Cavallari, P.; Caronni, A.; Perciavalle, V. Changes in cortical excitability and blood lactate after a fatiguing hand-grip exercise. Somatosens. Mot. Res. 2014, 31, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Perciavalle, V.; Di Corrado, D.; Scuto, C.; Perciavalle, V.; Coco, M. Attention and blood lactate levels in equestrians performing show jumping. Percept. Mot. Skills 2014, 118, 733–745. [Google Scholar] [CrossRef]
- Perciavalle, V.; Di Corrado, D.; Scuto, C.; Perciavalle, V.; Coco, M. Anthropometrics related to the performance of a sample of male swimmers. Percept. Mot. Skills 2014, 118, 940–950. [Google Scholar] [CrossRef] [PubMed]
- Coco, M.; Di Corrado, D.; Calogero, R.A.; Perciavalle, Va.; Maci, T.; Perciavalle, V. Attentional processes and blood lactate levels. Brain Res. 2009, 1302, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Pedrinolla, A.; Li Volti, G.; Galvano, F.; Schena, F.; Perciavalle, V.; Di Corrado, D. Bioenergetics and psychological profile of an ultra endurance walker. J. Sports Med. Phys. Fit. 2018, 58, 549–554. [Google Scholar] [CrossRef]
- Killgore, W.D.S.; Kahn-Greene, E.T.; Killgore, D.B.; Kamimori, G.H.; Balkin, T.J. Effects of acute caffeine withdrawal on Short Category Test performance in sleep-deprived individuals. Percept. Mot. Skills 2007, 105, 1265–1274. [Google Scholar] [CrossRef]
- Costantini, D. Oxidative stress ecology and the d-ROMs test: Facts, misfacts and an appraisal of a decade’s work. Behav. Ecol. Sociobiol. 2016, 70, 809–820. [Google Scholar] [CrossRef]
- Bhammar, D.M.; Sawyer, B.J.; Tucker, W.J.; Lee, J.M.; Gaesser, G.A. Validity of SenseWear® Armband v5.2 and v2.2 for estimating energy expenditure. J. Sports Sci. 2016, 34, 1830–1838. [Google Scholar] [CrossRef]
- Hernández-Padilla, J.M.; Granero-Molina, J.; Márquez-Hernández, V.V.; Suthers, F.; López-Entrambasaguas, O.M.; Fernández-Sola, C. Design and validation of a three-instrument toolkit for the assessment of competence in electrocardiogram rhythm recognition. Eur. J. Cardiovasc. Nurs. 2017, 16, 425–434. [Google Scholar] [CrossRef] [Green Version]
- McNair, D.M.; Lorr, M.; Droppleman, L.M. Profile of Mood States Manual; Educational and Industrial Testing Service: San Diego, CA, USA, 1992. [Google Scholar]
- Di Nuovo, S.; Rispoli, L. Misurare lo Stress; Franco Angeli: Milan, Italy, 2000. [Google Scholar]
- Dew, M.A.; Hoch, C.C.; Buysse, D.J.; Monk, T.H.; Begley, A.E.; Houck, P.R.; Hall, M.; Kupfer, D.J.; Reynolds, C.F., III. Healthy older adults’ sleep predicts all-cause mortality at 4 to 19 years of follow-up. Psychosom. Med. 2003, 65, 63–73. [Google Scholar] [CrossRef]
- Kripke, D.F.; Garfinkel, L.; Wingard, D.L.; Klauber, M.R.; Marler, M.R. Mortality associated with sleep duration and insomnia. Arch. Gen. Psychiatry 2002, 59, 131–136. [Google Scholar] [CrossRef]
- Mallon, L.; Broman, J.E.; Hetta, J. Sleep complaints predict coronary artery disease mortality in males: A 12-year follow-up study of a middle-aged Swedish population. J. Intern. Med. 2002, 251, 207–216. [Google Scholar] [CrossRef]
- Vgontzas, A.N.; Fernandez-Mendoza, J.; Liao, D.; Bixler, E.O. Insomnia with objective short sleep duration: The most biologically severe phenotype of the disorder. Sleep Med. Rev. 2013, 17, 241–254. [Google Scholar] [CrossRef]
- Irwin, M.I.; Olmstead, R.; Carroll, J.E. Sleep Disturbance, Sleep Duration, and Inflammation: A Systematic Review and Meta-Analysis of Cohort Studies and Experimental Sleep Deprivation. Biol. Psychiatry 2016, 80, 40–52. [Google Scholar] [CrossRef] [PubMed]
- Semplonius, T.; Willoughby, T. Long-term links between physical activity and sleep quality. Med. Sci. Sports Exerc. 2018, 13. [Google Scholar] [CrossRef]
- Coco, M.; Perciavalle, V.; Cavallari, P.; Perciavalle, V. Effects of an Exhaustive Exercise on Motor Skill Learning and on the Excitability of Primary Motor Cortex and Supplementary Motor Area. Medicine 2016, 95, e2978. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perciavalle, Va.; Maci, T.; Perciavalle, Vi.; Massimino, S.; Coco, M. Working memory and blood lactate levels. Neurol. Sci. 2015, 36, 2129–2136. [Google Scholar] [CrossRef] [PubMed]
- Coco, M.; Di Corrado, D.; Ramaci, T.; Di Nuovo, S.; Perciavalle, Vi.; Puglisi, A.; Cavallari, P.; Bellomo, M.; Buscemi, A. Role of lactic acid on cognitive functions. Phys. Sportsmed. 2019. [Google Scholar] [CrossRef] [PubMed]
- Kirschen, G.W.; Jones, J.J.; Hale, L. The Impact of Sleep Duration on Performance among Competitive Athletes: A Systematic Literature Review. Clin. J. Sport Med. 2018, 14. [Google Scholar] [CrossRef]
| PSM (Stress Measure) | Tension | Depression | Anger | Vigor | Fatigue | Confusion | |
|---|---|---|---|---|---|---|---|
| Basal | 66 | 41 | 51 | 43 | 53 | 39 | 37 |
| T0 | 68 | 44 | 46 | 40 | 41 | 39 | 41 |
| T1 (6 h) | 66 | 46 | 42 | 41 | 38 | 41 | 41 |
| T2 (12 h) | 69 | 43 | 43 | 41 | 36 | 41 | 43 |
| T3 (18 h) | 60 | 41 | 42 | 40 | 36 | 39 | 41 |
| T4 (24 h) | 68 | 41 | 43 | 45 | 28 | 39 | 50 |
| T5 (30 h) | 66 | 41 | 42 | 40 | 38 | 39 | 41 |
| T6 (36 h) | 67 | 41 | 43 | 40 | 38 | 39 | 37 |
| T7 (42 h) | 62 | 41 | 42 | 40 | 33 | 41 | 43 |
| T8 (48 h) | 70 | 39 | 42 | 40 | 29 | 41 | 43 |
| T9 (54 h) | 68 | 43 | 43 | 43 | 33 | 39 | 41 |
| T10 (60 h) | 63 | 43 | 45 | 40 | 48 | 41 | 37 |
| T11 (66 h) | 73 | 41 | 42 | 41 | 28 | 41 | 41 |
| T12 (72 h) | 63 | 41 | 43 | 40 | 28 | 41 | 41 |
| T0 | T12 | Normal Ranges | |
|---|---|---|---|
| Catecholamines | 115.5 | 137 | (90–720) |
| Cortisol | 13.7 | 15.7 | (3.7–19.4) |
| d-ROMs | 190 | 190 | (250–300) |
| BAP (test) | 2690 | 2690 | (>2200) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Coco, M.; Buscemi, A.; Guarnera, M.; La Paglia, R.; Perciavalle, V.; Di Corrado, D. Sleep Deprivation and Physiological Responses. A Case Report. J. Funct. Morphol. Kinesiol. 2019, 4, 17. https://doi.org/10.3390/jfmk4020017
Coco M, Buscemi A, Guarnera M, La Paglia R, Perciavalle V, Di Corrado D. Sleep Deprivation and Physiological Responses. A Case Report. Journal of Functional Morphology and Kinesiology. 2019; 4(2):17. https://doi.org/10.3390/jfmk4020017
Chicago/Turabian StyleCoco, Marinella, Andrea Buscemi, Maria Guarnera, Rosamaria La Paglia, Valentina Perciavalle, and Donatella Di Corrado. 2019. "Sleep Deprivation and Physiological Responses. A Case Report" Journal of Functional Morphology and Kinesiology 4, no. 2: 17. https://doi.org/10.3390/jfmk4020017
APA StyleCoco, M., Buscemi, A., Guarnera, M., La Paglia, R., Perciavalle, V., & Di Corrado, D. (2019). Sleep Deprivation and Physiological Responses. A Case Report. Journal of Functional Morphology and Kinesiology, 4(2), 17. https://doi.org/10.3390/jfmk4020017







