Oral Health and Fibromyalgia Syndrome: A Systemic Review
Abstract
:1. Introduction
1.1. Background
1.2. Objectives
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
- Study conducted on humans
- Studies containing information on fibromyalgia
- Studies containing information on oral health
- Studies older than 10 years
- Animal studies
- In vitro studies
- Studies on patients suffering from other pathologies (besides fibromyalgia and oral alterations)
- Studies not accessible (title or abstract)
2.3. Information Sources
2.4. Search
- Have Fibromyalgia Syndrome-affected patients an increased risk for oral health?
2.5. Study Selection
2.6. Data Collection Process
2.7. Data Items
2.8. Risk of Bias in Individual Studies
2.9. Summary Measures
- Authors and Year—author and year of the study (in order of year, from the most recent)
- Fibromyalgia—diagnosis confirmed or not
- Oral Health:
- ○
- Bone tissue—bone anomalies
- ○
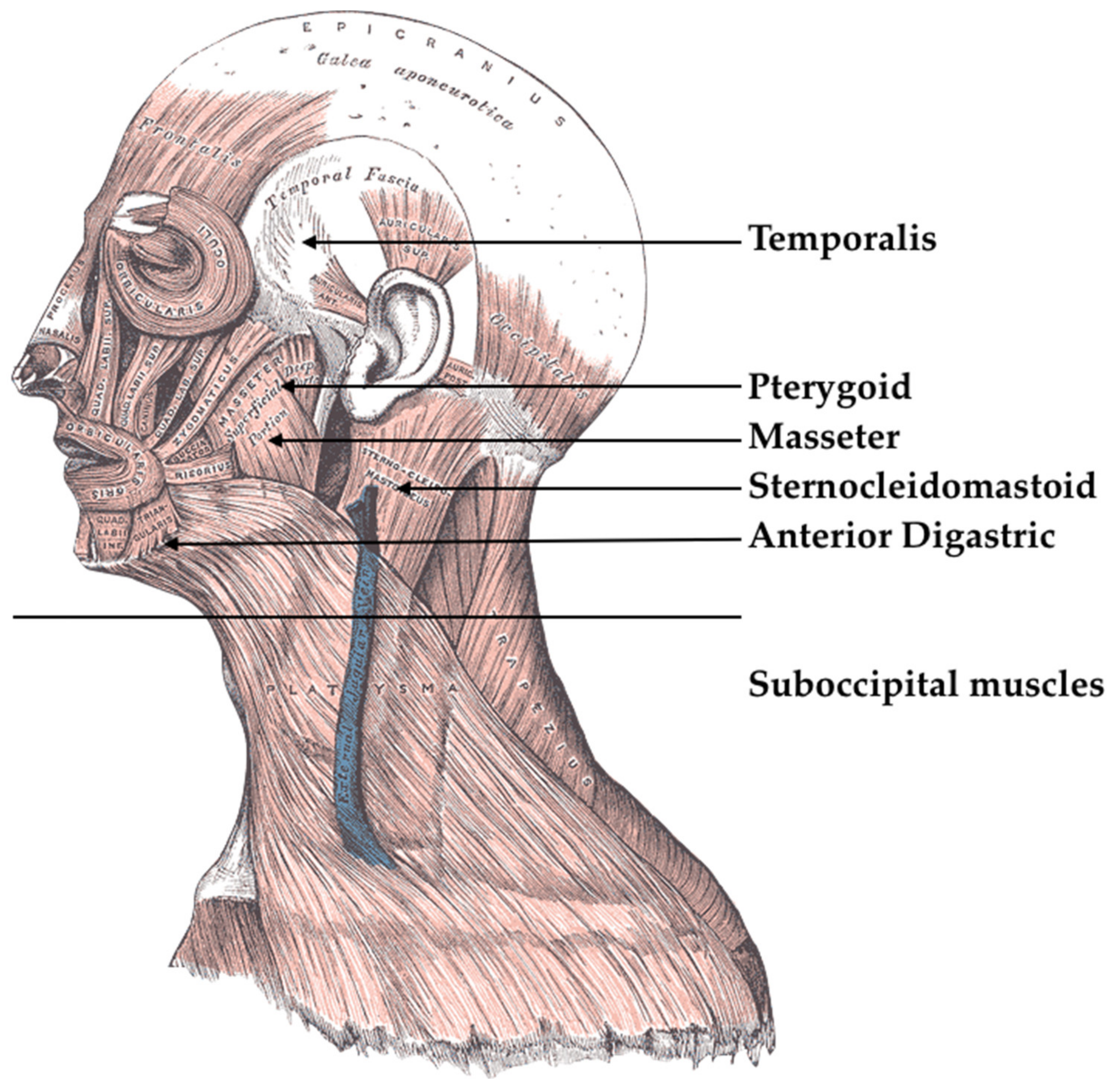
- Soft Tissue—anomalies on gums, mucous membranes, tongue, and muscles
- ○
- TMJ—temporomandibular joint anomalies
- Statistic—statistical data on the findings
- Sample and Methods—sample size and used methods or tests
2.10. Synthesis of Results
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of bias Within Studies
3.4. Results of Individual Studies and Synthesis of Results
4. Discussion
4.1. Summary of Evidence
4.2. Limitation
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sumpton, J.E.; Moulin, D.E. Fibromyalgia. Handb. Clin. Neurol. 2014, 119, 513–527. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, F.; Smythe, H.A.; Yunus, M.B.; Bennett, R.M.; Bombardier, C.; Goldenberg, D.L.; Tugwell, P.; Campbell, S.M.; Abeles, M.; Clark, P.; et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheumatol. 1990, 33, 160–172. [Google Scholar] [CrossRef] [PubMed]
- Fitzcharles, M.-A.; Perrot, S.; Häuser, W. Comorbid fibromyalgia: A qualitative review of prevalence and importance. Eur. J. Pain 2018, 22, 1565–1576. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hauser, W.; Ablin, J.; Fitzcharles, M.A.; Littlejohn, G.; Luciano, J.V.; Usui, C.; Walitt, B. Fibromyalgia. Nat. Rev. Dis. Primers 2015, 1, 15022. [Google Scholar] [CrossRef] [PubMed]
- Quintner, J.L.; Cohen, M.L. Fibromyalgia falls foul of a fallacy. Lancet 1999, 353, 1092–1094. [Google Scholar] [CrossRef]
- Henriksson, K.G.; Bengtsson, A.; Larsson, J.; Lindstrom, F.; Thornell, L.E. Muscle biopsy findings of possible diagnostic importance in primary fibromyalgia (fibrositis, myofascial syndrome). Lancet 1982, 2, 1395. [Google Scholar] [CrossRef]
- Cohen, M.L.; Quintner, J.L. Fibromyalgia syndrome, a problem of tautology. Lancet 1993, 342, 906–909. [Google Scholar] [CrossRef]
- Szychlinska, M.A.; Yamakado, K.; Castorina, A.; Ljubisavljevic, M. The “Journal of Functional Morphology and Kinesiology” Journal Club Series: Highlights on Recent Papers in Musculoskeletal Disorders. J. Funct. Morphol. Kinesiol. 2017, 2, 10. [Google Scholar] [CrossRef] [Green Version]
- Arnold, L.M.; Bennett, R.M.; Crofford, L.J.; Dean, L.E.; Clauw, D.J.; Goldenberg, D.L.; Fitzcharles, M.A.; Paiva, E.S.; Staud, R.; Sarzi-Puttini, P.; et al. AAPT Diagnostic Criteria for Fibromyalgia. J. Pain 2019, 20, 611–628. [Google Scholar] [CrossRef] [Green Version]
- Staud, R. Biology and therapy of fibromyalgia: Pain in fibromyalgia syndrome. Arthritis Res. Ther. 2006, 8, 208. [Google Scholar] [CrossRef] [Green Version]
- Yunus, M.B. Central sensitivity syndromes: A new paradigm and group nosology for fibromyalgia and overlapping conditions, and the related issue of disease versus illness. Semin. Arthritis Rheumatol. 2008, 37, 339–352. [Google Scholar] [CrossRef] [PubMed]
- Whiting, P.; Savovic, J.; Higgins, J.P.T.; Caldwell, D.M.; Reeves, B.C.; Shea, B.; Davies, P.; Kleijnen, J.; Churchill, R. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. Recenti Prog. Med. 2018, 109, 421–431. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Savovic, J.; Turner, R.M.; Mawdsley, D.; Jones, H.E.; Beynon, R.; Higgins, J.P.T.; Sterne, J.A.C. Association Between Risk-of-Bias Assessments and Results of Randomized Trials in Cochrane Reviews: The ROBES Meta-Epidemiologic Study. Am. J. Epidemiol. 2018, 187, 1113–1122. [Google Scholar] [CrossRef] [PubMed]
- Mansournia, M.A.; Higgins, J.P.; Sterne, J.A.; Hernan, M.A. Biases in Randomized Trials: A Conversation Between Trialists and Epidemiologists. Epidemiology 2017, 28, 54–59. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [Green Version]
- Velly, A.M.; Look, J.O.; Schiffman, E.; Lenton, P.A.; Kang, W.; Messner, R.P.; Holcroft, C.A.; Fricton, J.R. The effect of fibromyalgia and widespread pain on the clinically significant temporomandibular muscle and joint pain disorders--a prospective 18-month cohort study. J. Pain 2010, 11, 1155–1164. [Google Scholar] [CrossRef] [Green Version]
- Hoffmann, R.G.; Kotchen, J.M.; Kotchen, T.A.; Cowley, T.; Dasgupta, M.; Cowley, A.W., Jr. Temporomandibular disorders and associated clinical comorbidities. Clin. J. Pain 2011, 27, 268–274. [Google Scholar] [CrossRef] [Green Version]
- Karibe, H.; Goddard, G.; McNeill, C.; Shih, S.T. Comparison of patients with orofacial pain of different diagnostic categories. Cranio 2011, 29, 138–143. [Google Scholar] [CrossRef]
- Kindler, L.L.; Bennett, R.M.; Jones, K.D. Central sensitivity syndromes: Mounting pathophysiologic evidence to link fibromyalgia with other common chronic pain disorders. Pain Manag. Nurs. 2011, 12, 15–24. [Google Scholar] [CrossRef] [Green Version]
- Alonso-Blanco, C.; Fernandez-de-Las-Penas, C.; de-la-Llave-Rincon, A.I.; Zarco-Moreno, P.; Galan-Del-Rio, F.; Svensson, P. Characteristics of referred muscle pain to the head from active trigger points in women with myofascial temporomandibular pain and fibromyalgia syndrome. J. Headache Pain 2012, 13, 625–637. [Google Scholar] [CrossRef] [Green Version]
- Suma, S.; Veerendra Kumar, B. Temporomandibular disorders and functional somatic syndromes: Deliberations for the dentist. Indian J. Dent. Res. 2012, 23, 529–536. [Google Scholar] [CrossRef] [PubMed]
- De Rossi, S.S.; Stern, I.; Sollecito, T.P. Disorders of the masticatory muscles. Dent. Clin. N. Am. 2013, 57, 449–464. [Google Scholar] [CrossRef]
- De Siqueira, S.R.; Teixeira, M.J.; de Siqueira, J.T. Orofacial pain and sensory characteristics of chronic patients compared with controls. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 115, e37–e45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cassisi, G.; Sarzi-Puttini, P.; Casale, R.; Cazzola, M.; Boccassini, L.; Atzeni, F.; Stisi, S. Pain in fibromyalgia and related conditions. Reumatismo 2014, 66, 72–86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jin, H.; Patil, P.M.; Sharma, A. Topical review: The enigma of fibromyalgia. J. Oral Facial Pain Headache 2014, 28, 107–118. [Google Scholar] [CrossRef]
- Dahan, H.; Shir, Y.; Velly, A.; Allison, P. Specific and number of comorbidities are associated with increased levels of temporomandibular pain intensity and duration. J. Headache Pain 2015, 16, 528. [Google Scholar] [CrossRef] [Green Version]
- Eisenlohr-Moul, T.A.; Crofford, L.J.; Howard, T.W.; Yepes, J.F.; Carlson, C.R.; de Leeuw, R. Parasympathetic reactivity in fibromyalgia and temporomandibular disorder: Associations with sleep problems, symptom severity, and functional impairment. J. Pain 2015, 16, 247–257. [Google Scholar] [CrossRef] [Green Version]
- Furquim, B.D.; Flamengui, L.M.; Conti, P.C. TMD and chronic pain: A current view. Dent. Press J. Orthod. 2015, 20, 127–133. [Google Scholar] [CrossRef]
- Gui, M.S.; Pimentel, M.J.; Rizzatti-Barbosa, C.M. Temporomandibular disorders in fibromyalgia syndrome: A short-communication. Rev. Bras. Reumatol. 2015, 55, 189–194. [Google Scholar] [CrossRef] [Green Version]
- Cummiford, C.M.; Nascimento, T.D.; Foerster, B.R.; Clauw, D.J.; Zubieta, J.K.; Harris, R.E.; DaSilva, A.F. Changes in resting state functional connectivity after repetitive transcranial direct current stimulation applied to motor cortex in fibromyalgia patients. Arthritis Res. 2016, 18, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fujarra, F.J.; Kaziyama, H.H.; Siqueira, S.R.; Yeng, L.T.; Camparis, C.M.; Teixeira, M.J.; Siqueira, J.T. Temporomandibular disorders in fibromyalgia patients: Are there different pain onset? Arq NeuroPsiquiatr 2016, 74, 195–200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robinson, L.J.; Durham, J.; Newton, J.L. A systematic review of the comorbidity between Temporomandibular Disorders and Chronic Fatigue Syndrome. J. Oral Rehabil. 2016, 43, 306–316. [Google Scholar] [CrossRef] [PubMed]
- Losert-Bruggner, B.; Hulse, M.; Hulse, R. Fibromyalgia in patients with chronic CCD and CMD—A retrospective study of 555 patients. Cranio 2018, 36, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Isaia, B.; Ravarotto, M.; Finotti, P.; Nogara, M.; Piran, G.; Gamberini, J.; Biz, C.; Masiero, S.; Frizziero, A. Analysis of Dental Malocclusion and Neuromotor Control in Young Healthy Subjects through New Evaluation Tools. J. Funct. Morphol. Kinesiol. 2019, 4, 5. [Google Scholar] [CrossRef] [Green Version]
- Bruno, A.; Mico, U.; Lorusso, S.; Cogliandro, N.; Pandolfo, G.; Caminiti, M.; Zoccali, R.A.; Muscatello, M.R. Agomelatine in the treatment of fibromyalgia: A 12-week, open-label, uncontrolled preliminary study. J. Clin. Psychopharmacol. 2013, 33, 507–511. [Google Scholar] [CrossRef]
- Fiorillo, L.; Cervino, G.; Herford, A.S.; Lauritano, F.; D’Amico, C.; Lo Giudice, R.; Laino, L.; Troiano, G.; Crimi, S.; Cicciu, M. Interferon Crevicular Fluid Profile and Correlation with Periodontal Disease and Wound Healing: A Systemic Review of Recent Data. Int. J. Mol. Sci 2018, 19, 1908. [Google Scholar] [CrossRef] [Green Version]
- Isola, G.; Ramaglia, L.; Cordasco, G.; Lucchese, A.; Fiorillo, L.; Matarese, G. The effect of a functional appliance in the management of temporomandibular joint disorders in patients with juvenile idiopathic arthritis. Minerva Stomatol. 2017, 66, 1–8. [Google Scholar] [CrossRef]
- Lombardi, T.; Bernardello, F.; Berton, F.; Porrelli, D.; Rapani, A.; Camurri Piloni, A.; Fiorillo, L.; Di Lenarda, R.; Stacchi, C. Efficacy of Alveolar Ridge Preservation after Maxillary Molar Extraction in Reducing Crestal Bone Resorption and Sinus Pneumatization: A Multicenter Prospective Case-Control Study. Biomed. Res. Int. 2018, 2018, 9352130. [Google Scholar] [CrossRef] [Green Version]
- Fiorillo, L.; De Stefano, R.; Cervino, G.; Crimi, S.; Bianchi, A.; Campagna, P.; Herford, A.S.; Laino, L.; Cicciù, M. Oral and Psychological Alterations in Haemophiliac Patients. Biomedicines 2019, 7, 33. [Google Scholar] [CrossRef] [Green Version]
- Sambataro, S.; Cervino, G.; Fiorillo, L.; Cicciu, M. Upper First Premolar Positioning Evaluation for the Stability of the Dental Occlusion: Anatomical Considerations. J. Craniofac. Surg. 2018, 29, 1366–1369. [Google Scholar] [CrossRef]
- Wroe, A.L.; Bowers, H.M. Beliefs about sharing illness experiences: Development of a scale and relationship with symptoms of fibromyalgia. Br. J. Health Psychol. 2019. [Google Scholar] [CrossRef]
- Tesio, V.; Ghiggia, A.; Di Tella, M.; Castelli, L. Utility of the Diagnostic Criteria for Psychosomatic Research in assessing psychological disorders in fibromyalgia patients. J. Affect. Disord. 2019, 256, 219–220. [Google Scholar] [CrossRef]
- Onder, H.; Hamamci, M.; Alpua, M.; Ulusoy, E.K. Comorbid fibromyalgia in migraine patients: Clinical significance and impact on daily life. Neurol. Res. 2019, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Minerbi, A.; Gonzalez, E.; Brereton, N.J.B.; Anjarkouchian, A.; Dewar, K.; Fitzcharles, M.A.; Chevalier, S.; Shir, Y. Altered microbiome composition in individuals with fibromyalgia. Pain 2019. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jacobs, H.; Bockaert, M.; Bonte, J.; D’Haese, M.; Degrande, J.; Descamps, L.; Detaeye, U.; Goethals, W.; Janssens, J.; Matthys, K.; et al. The Impact of a Group-Based Multidisciplinary Rehabilitation Program on the Quality of Life in Patients With Fibromyalgia: Results From the QUALIFIBRO Study. J. Clin. Rheumatol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Stacchi, C.; Lombardi, T.; Cusimano, P.; Berton, F.; Lauritano, F.; Cervino, G.; Di Lenarda, R.; Cicciù, M. Bone Scrapers Versus Piezoelectric Surgery in the Lateral Antrostomy for Sinus Floor Elevation. J. Craniofac. Surg. 2017, 28, 1191–1196. [Google Scholar] [CrossRef] [PubMed]
- Cicciù, M.; Herford, A.S.; Cervino, G.; Troiano, G.; Lauritano, F.; Laino, L. Tissue fluorescence imaging (VELscope) for quick non-invasive diagnosis in oral pathology. J. Craniofac. Surg. 2017, 28, e112–e115. [Google Scholar] [CrossRef]
- Isola, G.; Cicciu, M.; Fiorillo, L.; Matarese, G. Association Between Odontoma and Impacted Teeth. J. Craniofac. Surg. 2017, 28, 755–758. [Google Scholar] [CrossRef]
- Lo Giudice, G.; Cutroneo, G.; Centofanti, A.; Artemisia, A.; Bramanti, E.; Militi, A.; Rizzo, G.; Favaloro, A.; Irrera, A.; Lo Giudice, R.; et al. Dentin morphology of root canal surface: A quantitative evaluation based on a scanning electronic microscopy study. BioMed Res. Int. 2015, 2015. [Google Scholar] [CrossRef] [Green Version]
- Herford, A.S.; Lu, M.; Akin, L.; Cicciù, M. Evaluation of a porcine matrix with and without platelet-derived growth factor for bone graft coverage in pigs. Int. J. Oral Maxillofac. Implants 2012, 27, 1351–1358. [Google Scholar]
- Maiorana, C.; Beretta, M.; Grossi, G.B.; Santoro, F.; Herford, A.S.; Nagursky, H.; Cicciù, M. Histomorphometric evaluation of anorganic bovine bone coverage to reduce autogenous grafts resorption: Preliminary results. Open Dent. J. 2011, 5, 71–78. [Google Scholar] [CrossRef] [Green Version]
- Cicciù, M.; Herford, A.S.; Stoffella, E.; Cervino, G.; Cicciù, D. Protein-signaled guided bone regeneration using titanium mesh and Rh-BMP2 in oral surgery: A case report involving left mandibular reconstruction after tumor resection. Open Dent. J. 2012, 6, 51–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giudice, G.; Cicciù, M.; Cervino, G.; Lizio, A.; Visco, A. Flowable resin and marginal gap on tooth third medial cavity involving enamel and radicular cementum: A SEM evaluation of two restoration techniques. Indian J. Dent. Res. 2012, 23, 763–769. [Google Scholar] [CrossRef] [PubMed]
- Cervino, G.; Fiorillo, L.; Herford, A.S.; Romeo, U.; Bianchi, A.; Crimi, S.; D’Amico, C.; De Stefano, R.; Troiano, G.; Santoro, R.; et al. Molecular Biomarkers Related to Oral Carcinoma: Clinical Trial Outcome Evaluation in a Literature Review. Dis. Markers 2019, 2019, 11. [Google Scholar] [CrossRef] [PubMed]
- Cervino, G.; Fiorillo, L.; Laino, L.; Herford, A.S.; Lauritano, F.; Giudice, G.L.; Fama, F.; Santoro, R.; Troiano, G.; Iannello, G.; et al. Oral Health Impact Profile in Celiac Patients: Analysis of Recent Findings in a Literature Review. Gastroenterol. Res. Pract. 2018, 2018, 7848735. [Google Scholar] [CrossRef]
- Giudice, G.; Lipari, F.; Lizio, A.; Cervino, G.; Cicciù, M. Tooth fragment reattachment technique on a pluri traumatized tooth. J. Conserv. Dent. 2012, 15, 80–83. [Google Scholar] [CrossRef] [Green Version]
- Crimi, S.; Fiorillo, L.; Bianchi, A.; D’Amico, C.; Amoroso, G.; Gorassini, F.; Mastroieni, R.; Marino, S.; Scoglio, C.; Catalano, F.; et al. Herpes Virus, Oral Clinical Signs and QoL: Systematic Review of Recent Data. Viruses 2019, 11, 463. [Google Scholar] [CrossRef] [Green Version]
- Cervino, G.; Terranova, A.; Briguglio, F.; De Stefano, R.; Famà, F.; D’Amico, C.; Amoroso, G.; Marino, S.; Gorassini, F.; Mastroieni, R.; et al. Diabetes: Oral health related quality of life and oral alterations. Biomed. Res. Int. 2019, 2019. [Google Scholar] [CrossRef] [Green Version]
- Troiano, G.; Laino, L.; Cicciu, M.; Cervino, G.; Fiorillo, L.; D’Amico, C.; Zhurakivska, K.; Lo Muzio, L. Comparison of Two Routes of Administration of Dexamethasone to Reduce the Postoperative Sequelae After Third Molar Surgery: A Systematic Review and Meta-Analysis. Open Dent. J. 2018, 12, 181–188. [Google Scholar] [CrossRef] [Green Version]
- Laino, L.; Cicciù, M.; Fiorillo, L.; Crimi, S.; Bianchi, A.; Amoroso, G.; Monte, I.P.; Herford, A.S.; Cervino, G. Surgical Risk on Patients with Coagulopathies: Guidelines on Hemophiliac Patients for Oro-Maxillofacial Surgery. Int. J. Environ. Res. Public Health 2019, 16, 1386. [Google Scholar] [CrossRef] [Green Version]
- Fiorillo, L. Chlorhexidine Gel Use in the Oral District: A Systematic Review. Gels 2019, 5, 31. [Google Scholar] [CrossRef] [Green Version]
- Stefano, R.D.; Bruno, A.; Muscatello, M.; Cedro, C.; Cervino, G.; Fiorillo, L. Fear and anxiety managing methods during dental treatments: Systematic review of recent data. Minerva Stomatol. 2019, in press. [Google Scholar] [CrossRef] [PubMed]
- De Stefano, R. Psychological Factors in Dental Patient Care: Odontophobia. Medicina 2019, 55, 678. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zoccali, R.; Muscatello, M.R.; Bruno, A.; Barilla, G.; Campolo, D.; Meduri, M.; Familiari, L.; Bonica, M.; Consolo, P.; Scaffidi, M. Anger and ego-defence mechanisms in non-psychiatric patients with irritable bowel syndrome. Dig. Liver Dis. 2006, 38, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Muscatello, M.R.; Bruno, A.; Scimeca, G.; Pandolfo, G.; Zoccali, R.A. Role of negative affects in pathophysiology and clinical expression of irritable bowel syndrome. World J. Gastroenterol. 2014, 20, 7570–7586. [Google Scholar] [CrossRef]
- Muscatello, M.R.; Bruno, A.; Pandolfo, G.; Mico, U.; Stilo, S.; Scaffidi, M.; Consolo, P.; Tortora, A.; Pallio, S.; Giacobbe, G.; et al. Depression, anxiety and anger in subtypes of irritable bowel syndrome patients. J. Clin. Psychol. Med. Settings 2010, 17, 64–70. [Google Scholar] [CrossRef]
- Muscatello, M.R.; Bruno, A.; Mento, C.; Pandolfo, G.; Zoccali, R.A. Personality traits and emotional patterns in irritable bowel syndrome. World J. Gastroenterol. 2016, 22, 6402–6415. [Google Scholar] [CrossRef]

| Dimension 1 Criteria |
|---|
| Dimension 1: Core Diagnostic Criteria |
| MSP defined as 6 or more pain sites from a total of 9 possible sites |
| Moderate to severe sleep problems OR fatigue |
| MSP plus fatigue or sleep problems must have been present for at least 3 months |
| Authors and Year | Fibromyalgia | Oral Health | Statistic | Sample and Methods | ||
|---|---|---|---|---|---|---|
| Bone Tissue | Soft Tissue | TMJ | ||||
| Velly et al., 2010 [16] | ✔ | ✔ | ✔ | Significant | 485 patients–Graded Chronic Pain Scale (GCPS). | |
| Hoffmann et al., 2011 [17] | ✔ | ✔ | p = 0.0001 | 1511 patients. | ||
| Karibe et al., 2011 [18] | ✔ | ✔ | p < 0.01 | 237 patients–Pain and Activity of Daily Living (ADL) | ||
| Kindler et al., 2011 [19] | ✔ | ✔ | Review | Review | ||
| Alonso-Bianco et al., 2012 [20] | ✔ | ✔ | ✔ | Significant | 20 patients–Active trigger points (TrPs) localization | |
| Suma et al., 2012 [21] | ✔ | ✔ | ✔ | Review | Review | |
| De Rossi et al., 2013 [22] | ✔ | ✔ | ✔ | Review | Review | |
| De Siqueira et al., 2013 [23] | ✔ | ✔ | ✔ | ✔ | Significant | 116 patients–pain evaluation, orofacial characteristics, oral health, sensivity to muscular palpation. |
| Cassisi et al., 2014 [24] | ✔ | ✔ | ✔ | Review | Review | |
| Jin et al., 2014 [25] | ✔ | ✔ | ✔ | Review | Review | |
| Dahan et al., 2015 [26] | ✔ | ✔ | ✔ | Significant | 224 patients–TMD comorbidities and which causes pain increase and duration | |
| Eisenlohr-Moul et al., 2015 [27] | ✔ | Significant | 43 patients–baseline assessment of respiratory sinus arrhythmia, parasympathetic assessment during a questionnaire period | |||
| Furquim et al., 2015 [28] | ✔ | Review | Review | |||
| Gui et al., 2015 [29] | ✔ | Review | Review | |||
| Cummiford et al., 2016 [30] | ✔ | Significant | 12 patients-Pain-Transcranial direct current stimulation (tDCS) use | |||
| Fujarra et al., 2016 [31] | ✔ | ✔ | ✔ | Significant | 53 patients–TMD diagnosis and Visual Analogue Scale (VAS) | |
| Robinson et al., 2016 [32] | ✔ | ✔ | ✔ | Review | Review | |
| Losert-Bruggner et al., 2018 [33] | ✔ | ✔ | ✔ | Significant | 555 patients–Pain index–bite splint therapy and neuromuscular relaxation measures | |
| Authors and Year | Risk of Bias | |||
|---|---|---|---|---|
| Low | Moderate | High | Unclear | |
| Velly et al., 2010 [16] | ✔ | |||
| Hoffmann et al., 2011 [17] | ✔ | |||
| Karibe et al., 2011 [18] | ✔ | |||
| Kindler et al., 2011 [19] | ✔ | |||
| Alonso-Bianco et al., 2012 [20] | ✔ | |||
| Suma et al., 2012 [21] | ✔ | |||
| De Rossi et al., 2013 [22] | ✔ | |||
| De Siqueira et al., 2013 [23] | ✔ | |||
| Cassisi et al., 2014 [24] | ✔ | |||
| Jin et al., 2014 [25] | ✔ | |||
| Dahan et al., 2015 [26] | ✔ | |||
| Eisenlohr-Moul et al., 2015 [27] | ✔ | |||
| Furquim et al., 2015 [28] | ✔ | |||
| Gui et al., 2015 [29] | ✔ | |||
| Cummiford et al., 2016 [30] | ✔ | |||
| Fujarra et al., 2016 [31] | ✔ | |||
| Robinson et al., 2016 [32] | ✔ | |||
| Losert-Bruggner et al., 2018 [33] | ✔ | |||
| Authors and Year | Results |
|---|---|
| Velly et al., 2010 [16] | According to the authors, the risk associated with baseline fibromyalgia was moderate. Centrally generated pain plays a role in TMJ disorders (TMJD) and muscle pain. |
| Hoffmann et al., 2011 [17] | According to the authors, TMJD-affected individuals were on average 41 years old and predominantly female (90%). Patients reported moderate-to-severe intensity of pain. In this case-control comparison study, a higher frequency of depression, fatigue and fibromyalgia is correlated to TMJD. Fibromyalgia was a comorbid condition |
| Karibe et al., 2011 [18] | Fibromyalgia patients and Neuropathy patients significantly reported greater pain intensity in the TMJ area. |
| Kindler et al., 2011 [19] | Central nervous system alteration could reflect TMJD |
| Alonso-Bianco et al., 2012 [20] | TrPs were identified by palpation, and patients referred to pain in these areas. The number of active TrPs was significantly higher in TMD patients than in FMS ones. Women with FMS referred to pain in these areas more than those with TMD. Significant differences within the center of gravity coordinates of TrPs were found in TMD and FMS. There are different TrPs localization between myofascial temporomandibular disorders (TMD) and fibromyalgia patients. |
| Suma et al., 2012 [21] | According to the authors, in fibromyalgia patients, TMD and pain remain a recurring problem and they need a correct diagnosis and management to resolve this problem. Often therapies are dictated by the cause as inflammation, trauma, aging or parafunctional habits. |
| De Rossi et al., 2013 [22] | According to the authors, many medicaments used for fibromyalgia could be used for TMJD. |
| De Siqueira et al., 2013 [23] | Sensorial anomalies were observed in neuropathic or somatic pain patients, as in fibromyalgia patients. According to the authors, the majority of patients had pain upon craniofacial muscle palpation. Persistent idiopathic facial pain and temporomandibular disorders were associated with a low threshold for pain perception. (p < 0.002) |
| Cassisi et al., 2014 [24] | Pain in fibromyalgia or TMJD is caused by CNS hypersensitivity. Pharmacological and non-pharmacological therapies have been suggested for the treatment of these conditions. |
| Jin et al., 2014 [25] | Masticatory muscle pain and TMJ pain could be associated with fibromyalgia, despite the internal derangements of the TMJ. |
| Dahan et al., 2015 [26] | There was a positive association between the number of comorbidities present and TMD pain duration (p < 0.01), also the presence of migraine was positively associated. TMD and fibromyalgia are associated with an increase of TMJ pain intensity and duration. |
| Eisenlohr-Moul et al., 2015 [27] | TMD and fibromyalgia showed a higher parasympathetic decline during a psychosocial assessment. |
| Furquim et al., 2015 [28] | TMD is managed by complex mechanisms by the autonomic nervous systems as is fibromyalgia. |
| Gui et al., 2015 [29] | TMD and fibromyalgia (FM) are not merely coexisting conditions, but they have a series of similar characteristics and predisposing triggering factors. |
| Cummiford et al., 2016 [30] | Transcranial direct current stimulation (tDCS) may produce analgesia by altering thalamic connectivity while there may be a placebo response. Stronger baseline functional connectivity between M1-VL (left primary motor cortex- ventral lateral) thalamus, S1-anterior insula (primary somatosensory cortices), and VL thalamus-PAG (periaqueductal) predicted greater analgesia after sham and real tDCS. Sham treatment (compared with baseline) reduced FC between the VPL (ventral posterolateral) thalamus, S1, and the amygdala. Real tDCS (compared with sham treatment) reduced FC between the VL thalamus, medial prefrontal, and supplementary motor cortices. Interestingly, decreased FC between the VL/VPL thalamus and posterior insula, M1, and S1 correlated with reductions in clinical pain after both sham and active treatments. |
| Fujarra et al., 2016 [31] | All patients showed TMD and muscle disorders, with limited opening and TMJ disc displacement. According to the authors, Myofascial pain could be associated with mouth opening limitation (p = 0.038); right disc displacement with reduction (p = 0.012) and jaw stiffness (p = 0.004) were predominant in the facial pain group. Myofascial pain without mouth opening limitation (p = 0.038) and numbness/burning were more common in the facial or generalized pain sample group. |
| Robinson et al., 2016 [32] | Chronic painful TMD is a central sensitivity syndrome related to the hypersensitivity of the CNS. Similar conditions are Chronic Fatigue Syndrome (CFS) and FM. |
| Losert-Bruggner et al., 2018 [33] | Patients with cranio-cervical disfunctions and craniomandibular disorders benefit from interdisciplinary treatment. Using myocentric bite splint therapy and therapy with oral orthosis in combination with neuromuscular relaxation measures, an improvement of physical symptoms was seen in 84% of CMD-FMS patients, and improvement of the symptoms in the jaw was achieved in 77% of cases. |
| Drug Category | Effect |
|---|---|
| Tricyclic antidepressants (TCAs) | Moderately helpful for pain, more side effects (xerostomia, fatigue) |
| Serotonin-selective reuptake inhibitors | Fewer side effects than TCAs, more effective for anxiety/depression than for pain |
| Muscle relaxants | Moderately helpful for local muscle pain, more side effects (xerostomia, sedation) |
| Serotonin-norepinephrine reuptake inhibitors | Moderately helpful for fibromyalgia-related pain, low-potency opioids, moderately helpful for fibromyalgia-related pain |
| NSAIDs | Helpful for acute inflammatory pain but not chronic muscle pain or fibromyalgia-related pain |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Stefano, R.; Bruno, A.; Muscatello, M.R.A.; Cedro, C.; Cicciù, A.; Rullo, R.; Gaeta, M.; Fiorillo, L. Oral Health and Fibromyalgia Syndrome: A Systemic Review. J. Funct. Morphol. Kinesiol. 2020, 5, 7. https://doi.org/10.3390/jfmk5010007
De Stefano R, Bruno A, Muscatello MRA, Cedro C, Cicciù A, Rullo R, Gaeta M, Fiorillo L. Oral Health and Fibromyalgia Syndrome: A Systemic Review. Journal of Functional Morphology and Kinesiology. 2020; 5(1):7. https://doi.org/10.3390/jfmk5010007
Chicago/Turabian StyleDe Stefano, Rosa, Antonio Bruno, Maria Rosaria Anna Muscatello, Clemente Cedro, Alessandra Cicciù, Rosario Rullo, Michele Gaeta, and Luca Fiorillo. 2020. "Oral Health and Fibromyalgia Syndrome: A Systemic Review" Journal of Functional Morphology and Kinesiology 5, no. 1: 7. https://doi.org/10.3390/jfmk5010007
APA StyleDe Stefano, R., Bruno, A., Muscatello, M. R. A., Cedro, C., Cicciù, A., Rullo, R., Gaeta, M., & Fiorillo, L. (2020). Oral Health and Fibromyalgia Syndrome: A Systemic Review. Journal of Functional Morphology and Kinesiology, 5(1), 7. https://doi.org/10.3390/jfmk5010007









