Kinematic Comparison between Medially Congruent and Posterior-Stabilized Third-Generation TKA Designs
Abstract
:1. Background
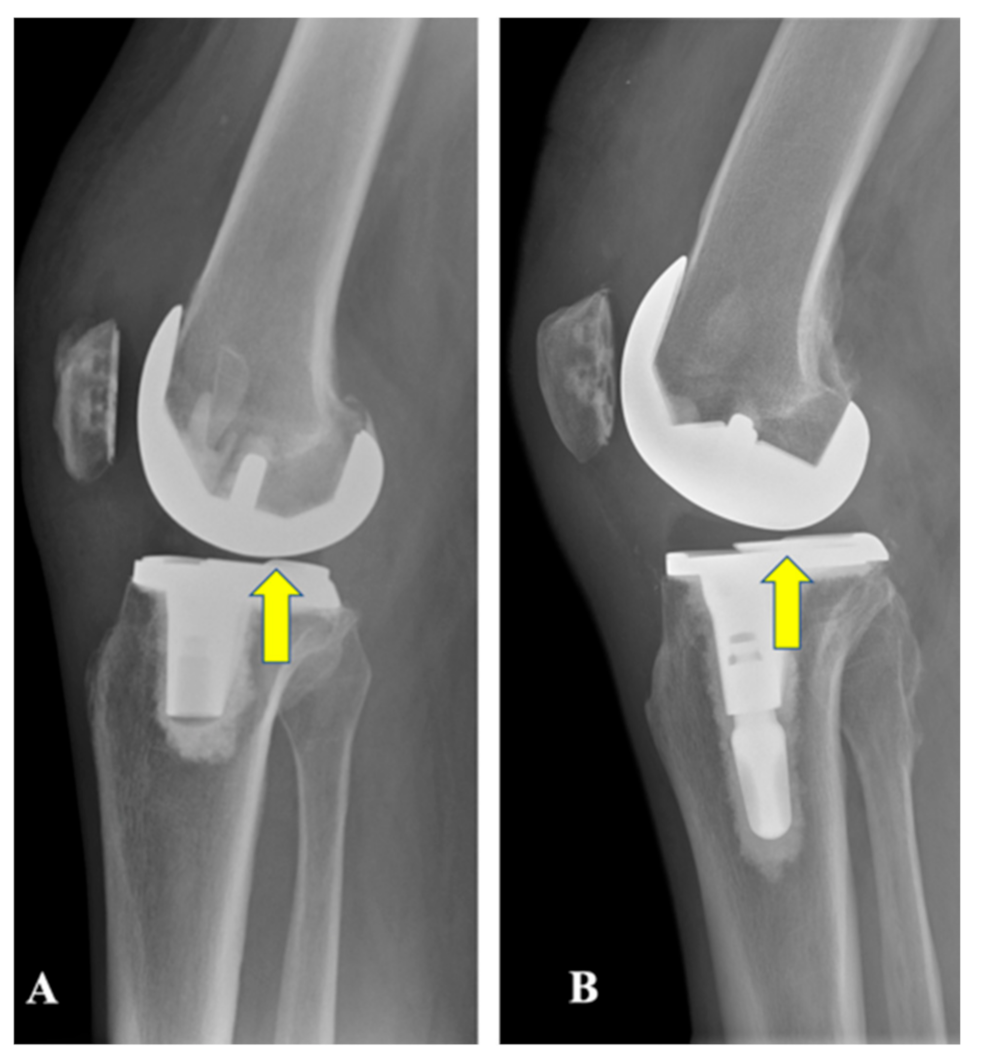
2. Materials and Methods
Gait Analysis
3. Results
3.1. Knee Flexion Angle at Heel-Strike (KFH)
3.2. Midstance Knee Flexion Angle
3.3. Knee Adduction Angle (KAA) and Knee Adduction Moment (KAM)
3.4. Peak Knee Flexion Moment (KFM)
3.5. Knee Rotational Moment (KRM)
3.6. TKA as a Whole Compared to the Healthy Control Group
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Ethics Declarations
References
- Choi, Y.-J.; Ra, H.J. Patient Satisfaction after Total Knee Arthroplasty. Knee Surg. Relat. Res. 2016, 28, 1–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gunaratne, R.; Pratt, D.N.; Banda, J.; Fick, D.P.; Khan, R.J.; Robertson, B.W. Patient Dissatisfaction Following Total Knee Arthroplasty: A Systematic Review of the Literature. J. Arthroplast. 2017, 32, 3854–3860. [Google Scholar] [CrossRef] [PubMed]
- Van Der Steen, M.C.; Janssen, R.P.A.; Reijman, M.; Tolk, J.J. Total Knee Arthroplasty: What to Expect? A Survey of the Members of the Dutch Knee Society on Long-Term Recovery after Total Knee Arthroplasty. J. Knee Surg. 2016, 30, 612–616. [Google Scholar] [CrossRef] [PubMed]
- Varadarajan, K.M.M.; Zumbrunn, T.; Rubash, H.E.; Malchau, H.; Li, G.; Muratoglu, O.K. Cruciate Retaining Implant With Biomimetic Articular Surface to Reproduce Activity Dependent Kinematics of the Normal Knee. J. Arthroplast. 2015, 30, 2149–2153.e2. [Google Scholar] [CrossRef] [PubMed]
- Noble, P.C.; Gordon, M.J.; Weiss, J.M.; Reddix, R.N.; Conditt, M.A.; Mathis, K.B. Does total knee replacement restore normal knee func-tion? Clin. Orthop. Relat. Res. 2005, 431, 157–165. [Google Scholar] [CrossRef]
- Song, S.J.; Detch, R.C.; Maloney, W.J.; Goodman, S.B.; Huddleston, J.I. Causes of Instability After Total Knee Arthroplasty. J. Arthroplast. 2014, 29, 360–364. [Google Scholar] [CrossRef]
- Wylde, V.; Artz, N.; Howells, N.; Blom, A.W. Kneeling ability after total knee replacement. EFORT Open Rev. 2019, 4, 460–467. [Google Scholar] [CrossRef]
- Stramazzo, L.; Bassi, N.; Ghirardelli, S.; Amoroso, T.; Osti, L.; Indelli, P.F. Posterior stability in posterior-stabilized vs medially congruent total knee replacement: A radiological comparison of two polyethylene designs in a single model. J. Orthop. Trauma Rehabil. 2020. [CrossRef]
- Ranawat, C.S. History of total knee replacement. J. South. Orthop. Assoc. 2002, 11, 218–226. [Google Scholar]
- Insall, J.N.; Clarke, H.D. Historic Development, Classification, and Characteristics of Knee Prostheses. In Insall & Scott Surgery of the Knee, 6th ed.; Elsevier: New York, NY, USA, 2017; ISBN 9780323400466. [Google Scholar]
- Indelli, P.F.; Risitano, S.; Hall, K.E.; Leonardi, E.; Migliore, E. Effect of polyethylene conformity on total knee arthroplasty early clinical outcomes. Knee Surg. Sports Traumatol. Arthrosc. 2018, 27, 1028–1034. [Google Scholar] [CrossRef]
- Harman, M.K.; Banks, S.A.; Kirschner, S.; Lützner, J. Prosthesis alignment affects axial rotation motion after total knee replacement: A prospective in vivo study combining computed tomography and fluoroscopic evaluations. BMC Musculoskelet. Disord. 2012, 13, 206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dennis, D.A.; Komistek, R.D.; Mahfouz, M.R.; Haas, B.D.; Stiehl, J.B. Multicenter Determination of In Vivo Kinematics after Total Knee Arthroplasty. Clin. Orthop. Relat. Res. 2003, 416, 37–57. [Google Scholar] [CrossRef] [Green Version]
- Cardinale, U.; Bragonzoni, L.; Bontempi, M.; Alesi, D.; Di Sarsina, T.R.; Presti, M.L.; Zaffagnini, S.; Muccioli, G.M.M.; Iacono, F. Knee kinematics after cruciate retaining highly congruent mobile bearing total knee arthroplasty: An in vivo dynamic RSA study. Knee 2020, 27, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Hatfield, G.L.; Hubley-Kozey, C.L.; Wilson, J.L.A.; Dunbar, M.J. The Effect of Total Knee Arthroplasty on Knee Joint Kinematics and Kinetics During Gait. J. Arthroplast. 2011, 26, 309–318. [Google Scholar] [CrossRef]
- Steinbrück, A.; Schröder, C.; Woiczinski, M.; Fottner, A.; Müller, P.E.; Jansson, V. Patellofemoral contact patterns before and after total knee arthroplasty: An in vitro measurement. Biomed. Eng. Online 2013, 12, 58. [Google Scholar] [CrossRef] [Green Version]
- Koo, S.; Andriacchi, T.P. The knee joint center of rotation is predominantly on the lateral side during normal walking. J. Biomech. 2008, 41, 1269–1273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamaguchi, S.; Gamada, K.; Sasho, T.; Kato, H.; Sonoda, M.; Banks, S.A. In vivo kinematics of anterior cruciate ligament deficient knees during pivoting and squat activities. Clin. Biomech. 2009, 24, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Mikashima, Y.; Harman, M.K.; Coburn, J.; Hodge, W.A.; Banks, S.A. In vivo kinematics of an acl- substituting total knee arthro-plasty during gait and stair activities. Orthop. Proc. 2010, 92, 889–896. [Google Scholar]
- Andriacchi, T.P.; Dyrby, C.O. Interactions between kinematics and loading during walking for the normal and ACL deficient knee. J. Biomech. 2005, 38, 293–298. [Google Scholar] [CrossRef]
- Risitano, S.; Indelli, P.F. Is “symmetric” gap balancing still the gold standard in primary total knee arthroplasty? Ann. Transl. Med. 2017, 5, 325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Risitano, S.; Karamian, B.; Indelli, P.F. Intraoperative load-sensing drives the level of constraint in primary total knee arthroplasty: Surgical technique and review of the literature. J. Clin. Orthop. Trauma 2017, 8, 265–269. [Google Scholar] [CrossRef]
- Indelli, P.F.; Morello, F.; Ghirardelli, S.; Fidanza, A.; Iannotti, F.; Ferrini, A. No clinical differences at the 2-year follow-up between single radius and J-curve medial pivot total knee arthroplasty in the treatment of neutral or varus knees. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 3949–3954. [Google Scholar] [CrossRef]
- Roos, E.M.; Toksvig-Larsen, S. Knee injury and Osteoarthritis Outcome Score (KOOS)—Validation and comparison to the WOMAC in total knee replacement. Health Qual. Life Outcomes 2003, 1, 17. [Google Scholar] [CrossRef] [Green Version]
- Thienpont, E.; Opsomer, G.; Koninckx, A.; Houssiau, F. Joint Awareness in Different Types of Knee Arthroplasty Evaluated With the Forgotten Joint Score. J. Arthroplast. 2014, 29, 48–51. [Google Scholar] [CrossRef] [PubMed]
- Andriacchi, T.P.; Alexander, E.J.; Toney, M.K.; Dyrby, C.; Sum, J. A Point Cluster Method for In Vivo Motion Analysis: Applied to a Study of Knee Kinematics. J. Biomech. Eng. 1998, 120, 743–749. [Google Scholar] [CrossRef] [PubMed]
- Chehab, E.; Andriacchi, T.; Favre, J. Speed, age, sex, and body mass index provide a rigorous basis for comparing the kinematic and kinetic profiles of the lower extremity during walking. J. Biomech. 2017, 58, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Favre, J.; Erhart-Hledik, J.; Andriacchi, T. Age-related differences in sagittal-plane knee function at heel-strike of walking are increased in osteoarthritic patients. Osteoarthr. Cartil. 2014, 22, 464–471. [Google Scholar] [CrossRef] [Green Version]
- Samy, D.A.; Wolfstadt, J.I.; Vaidee, I.; Backstein, D.J. A Retrospective Comparison of a Medial Pivot and Posterior-Stabilized Total Knee Arthroplasty With Respect to Patient-Reported and Radiographic Outcomes. J. Arthroplast. 2018, 33, 1379–1383. [Google Scholar] [CrossRef] [Green Version]
- Meneghini, R.M.; Deckard, E.R.; Ishmael, M.K.; Ziemba-Davis, M. A dual-pivot pattern simulating native knee kinematics opti-mizes functional outcomes after total knee arthroplasty. J. Arthroplast. 2017, 32, 3009–3015. [Google Scholar] [CrossRef] [Green Version]
- Banks, S.A.; Meneghini, R.M. Achieving More Natural Motion, Stability, and Function With a Dual-Pivot ACL-substituting Total Knee Arthroplasty Design. Tech. Orthop. 2018, 33, 48–51. [Google Scholar] [CrossRef]
- Lewek, M.; Rudolph, K.; Axe, M.; Snyder-Mackler, L. The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin. Biomech. 2002, 17, 56–63. [Google Scholar] [CrossRef]
- Mizner, R.L.; Snyder-Mackler, L. Altered loading during walking and sit-to-stand is affected by quadriceps weakness after total knee arthroplasty. J. Orthop. Res. 2005, 23, 1083–1090. [Google Scholar] [CrossRef]
- Andriacchi, T.P.; Galante, J.O.; Fermier, R.W. The influence of total knee-replacement design on walking and stair-climbing. J. Bone Jt. Surg. Am. 1982, 64, 1328–1335. [Google Scholar] [CrossRef] [Green Version]
- Banks, S.A.; Harman, M.K.; Bellemans, J.; Hodge, W.A. Making sense of knee arthroplasty kinematics: News you can use. JBJS 2003, 85, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Steinbrück, A.; Schröder, C.; Woiczinski, M.; Fottner, A.; Pinskerova, V.; Müller, P.E.; Jansson, V. Femorotibial kinematics and load patterns after total knee arthroplasty: An in vitro comparison of posterior-stabilized versus medial-stabilized design. Clin. Biomech. 2016, 33, 42–48. [Google Scholar] [CrossRef]
- Zhao, D.; Banks, S.A.; Mitchell, K.H.; D’Lima, D.D.; Colwell, C.W.; Fregly, B.J. Correlation between the knee adduction torque and medial contact force for a variety of gait patterns. J. Orthop. Res. 2007, 25, 789–797. [Google Scholar] [CrossRef] [PubMed]
- Schipplein, O.D.; Andriacchi, T.P. Interaction between active and passive knee stabilizers during level walking. J. Orthop. Res. 1991, 9, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Kozanek, M.; Hosseini, A.; Liu, F.; Van de Velde, S.K.; Gill, T.J.; Rubash, H.E.; Li, G. Tibiofemoral kinematics and condylar motion during the stance phase of gait. J. Biomech. 2009, 42, 1877–1884. [Google Scholar] [CrossRef] [Green Version]
- Hoshino, Y.; Tashman, S. Internal tibial rotation during in vivo, dynamic activity induces greater sliding of tibio-femoral joint contact on the medial compartment. Knee Surg. Sports Traumatol. Arthrosc. 2011, 20, 1268–1275. [Google Scholar] [CrossRef] [PubMed]
- Shimmin, A.; Martinez-Martos, S.; Owens, J.; Iorgulescu, A.D.; Banks, S. Fluoroscopic motion study confirming the stability of a medial pivot design total knee arthroplasty. Knee 2015, 22, 522–526. [Google Scholar] [CrossRef]
- Scott, G.; Imam, M.A.; Eifert, A.; Freeman, M.A.R.; Pinskerova, V.; Field, R.E.; Skinner, J.; Banks, S.A. Can a total knee arthroplasty be both rotationally unconstrained and anteroposteriorly stabilised? A pulsed fluoroscopic investigation. Bone Jt. Res. 2016, 5, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Uvehammer, J.; Karrholm, J.; Brandsson, S. In vivo kinematics of total knee arthroplasty. Concave versus-posterior stabilized tibial joint surface. J. Bone Jt. Surg. Br. 2000, 82, 499–505. [Google Scholar] [CrossRef]
- Mitchell, K.; Banks, S.; Rawlins, J.; Wood, S.; Hodge, W. Strength on intrinsically stable TKA during stair-climbing. Trans. ORS 2005, 1, 563. [Google Scholar]
- Mahoney, O.M.; McClung, C.D.; Dela Rosa, M.A.; Schmalzried, T.P. The effect of total knee arthroplasty design on extensor mech-anism function. J. Arthroplast. 2002, 17, 416–421. [Google Scholar] [CrossRef] [PubMed]




| TKA | Healthy Controls | p-Value | |
|---|---|---|---|
| Age (years) | 65.8 ± 8.8 | 59.4 ± 7.9 | N.S. |
| Sex | 10 males | 10 males | N.S. |
| BMI (kg/m2) | 31.5 ± 4.9 | 30.3 ± 4.6 | N.S. |
| KOOS pain (points) | 75.0 ± 23.1 | 98.9 ± 1.9 | <0.01 |
| KOOS symptoms (points) | 71.4 ± 21.9 | 97.1 ± 4.1 | <0.01 |
| KOOS ADL (points) | 81.2 ± 18.2 | 99.7 ± 0.9 | <0.01 |
| KOOS Sports (points) | 60.0 ± 31.8 | 99.0 ± 2.1 | <0.01 |
| KOOS QOL (points) | 63.1 ± 31.0 | 96.9 ± 5.3 | <0.01 |
| Forgotten Joint Score (points) | 50.2 ± 38.1 | N/A | N/A |
| KFH (°) | 5.0 ± 4.1 | 4.5 ± 3.6 | N.S. |
| Midstance KFA (°) | 16.1 ± 5.2 | 20.7 ± 5.5 | 0.07 (trend) |
| Tibial rotation at heel-strike (°) | 5.8 ± 5.4 | 11.2 ± 5.5 | 0.04 |
| Peak KAA during swing (°) | 0.2 ± 4.2 | −5.1 ± 5.7 | 0.04 |
| KAA excursion during swing (°) | 6.0 ± 2.3 | 9.4 ± 4.9 | 0.07 (trend) |
| KAM1 (%BW*Ht) | 2.16 ± 0.52 | 2.38 ± 0.67 | N.S. |
| Peak KFM (%BW*Ht) | 2.91 ± 1.41 | 3.27 ± 1.08 | N.S. |
| Peak KIRM (%BW*Ht) | 0.78 ± 0.17 | 0.77 ± 0.27 | N.S. |
| MC TKA | PS TKA | p-Value | |
|---|---|---|---|
| Age (years) | 63.8 ± 9.2 | 68.8 ± 4.0 | N.S. |
| Sex | 6 males | 4 males | N.S. |
| BMI (kg/m2) | 32.2 ± 6.1 | 30.5 ± 2.7 | N.S. |
| KOOS pain (points) | 75.9 ± 26.5 | 73.6 ± 20.8 | N.S. |
| KOOS symptoms (points) | 75.0 ± 23.6 | 66.1 ± 21.1 | N.S. |
| KOOS ADL (points) | 83.8 ± 20.7 | 77.2 ± 15.7 | N.S. |
| KOOS Sports (points) | 63.3 ± 31.4 | 55.0 ± 36.5 | N.S. |
| KOOS QOL (points) | 60.4 ± 35.3 | 67.2 ± 27.7 | N.S. |
| Forgotten Joint Score (points) | 52.1 ± 40.1 | 47.4 ± 40.6 | N.S. |
| KFH (°) | 3.1 ± 1.3 | 7.9 ± 5.3 | 0.06 |
| Midstance KFA (°) | 14.0 ± 4.3 | 19.2 ± 5.4 | 0.12 |
| KAA excursion during swing (°) | 4.7 ± 1.4 | 7.9 ± 2.2 | 0.03 |
| KAM1 (%BW*Ht) | 2.21 ± 0.64 | 2.09 ± 0.31 | N.S. |
| Peak KFM (%BW*Ht) | 2.34 ± 1.16 | 3.78 ± 1.42 | 0.12 |
| Peak KIRM (%BW*Ht) | 0.88 ± 0.14 | 0.64 ± 0.09 | 0.02 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghirardelli, S.; Asay, J.L.; Leonardi, E.A.; Amoroso, T.; Andriacchi, T.P.; Indelli, P.F. Kinematic Comparison between Medially Congruent and Posterior-Stabilized Third-Generation TKA Designs. J. Funct. Morphol. Kinesiol. 2021, 6, 27. https://doi.org/10.3390/jfmk6010027
Ghirardelli S, Asay JL, Leonardi EA, Amoroso T, Andriacchi TP, Indelli PF. Kinematic Comparison between Medially Congruent and Posterior-Stabilized Third-Generation TKA Designs. Journal of Functional Morphology and Kinesiology. 2021; 6(1):27. https://doi.org/10.3390/jfmk6010027
Chicago/Turabian StyleGhirardelli, Stefano, Jessica L. Asay, Erika A. Leonardi, Tommaso Amoroso, Thomas P. Andriacchi, and Pier Francesco Indelli. 2021. "Kinematic Comparison between Medially Congruent and Posterior-Stabilized Third-Generation TKA Designs" Journal of Functional Morphology and Kinesiology 6, no. 1: 27. https://doi.org/10.3390/jfmk6010027
APA StyleGhirardelli, S., Asay, J. L., Leonardi, E. A., Amoroso, T., Andriacchi, T. P., & Indelli, P. F. (2021). Kinematic Comparison between Medially Congruent and Posterior-Stabilized Third-Generation TKA Designs. Journal of Functional Morphology and Kinesiology, 6(1), 27. https://doi.org/10.3390/jfmk6010027







