Electromyographic Analysis of the Lumbar Extensor Muscles during Dynamic Exercise on a Home Exercise Device
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Sample Size Calculation
2.4. Procedures
2.4.1. Participant Selection and Screening
2.4.2. Assessment of Isometric Lumbar Extension Strength
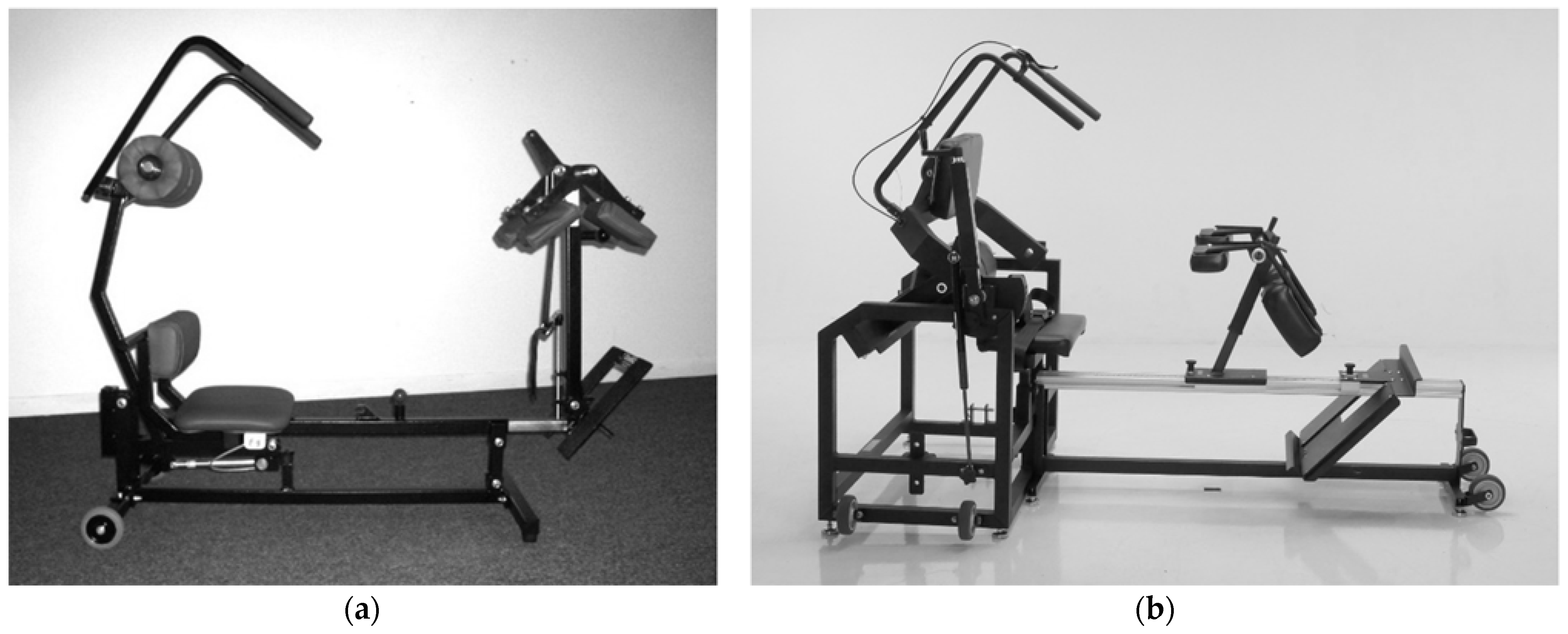
2.4.3. Assessment of Dynamic Lumbar Extension Exercise
2.4.4. Instrumentation and EMG Processing
2.5. Outcome Measures
2.6. Data Analysis
3. Results
4. Discussion
4.1. Limitations
4.2. Pragmatic Applications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. Underwood, M. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef]
- Foster, N.E.; Anema, J.R.; Cherkin, D.; Chou, R.; Cohen, S.P.; Gross, D.P.; Ferreira, P.H.; Fritz, J.M.; Koes, B.W.; Peul, W.; et al. Prevention and treatment of low back pain: Evidence, challenges, and promising directions. Lancet 2018, 391, 2368–2383. [Google Scholar] [CrossRef]
- Mayer, J.M.; Mooney, V.; Dagenais, S. Evidence-informed management of chronic low back pain with lumbar extensor strengthening exercises. Spine J. 2008, 8, 96–113. [Google Scholar] [CrossRef] [PubMed]
- Graves, J.E.; Webb, D.C.; Pollock, M.L.; Leggett, S.H.; Carpenter, D.M.; Foster, D.N.; Cirulli, J. Pelvic stabilization during resistance training: Its effect on the development of lumbar extension strength. Arch. Phys. Med. Rehabil. 1994, 75, 210–215. [Google Scholar] [CrossRef]
- Pollock, M.L.; Leggett, S.H.; Graves, J.E.; Jones, A.; Fulton, M.; Cirulli, J. Effect of resistance training on lumbar extension strength. Am. J. Sports Med. 1989, 17, 624–629. [Google Scholar] [CrossRef]
- Udermann, B.E.; Graves, J.E.; Donelson, R.; Iriso, J.; Boucher, J. Effect of pelvic restraint on hamstring, gluteal, and lumbar muscle emg activation. Arch. Phys. Med. Rehabil. 1999, 80, 1176–1179. [Google Scholar] [CrossRef]
- San Juan, J.G.; Yaggie, J.A.; Levy, S.S.; Mooney, V.; Udermann, B.E.; Mayer, J.M. Effects of pelvic stabilization on lumbar muscle activity during dynamic exercise. J. Strength Cond. Res. 2005, 19, 903–907. [Google Scholar] [CrossRef][Green Version]
- Leggett, S.; Mooney, V.; Matheson, L.; Nelson, B.; Dreisinger, T.; Van Zytveld, J.; Vie, L. Restorative exercise for clinical low back pain: A prospective two-center study with 1-year follow-up. Spine 1999, 24, 889–898. [Google Scholar] [CrossRef]
- Mooney, V.; Gulick, J.; Perlman, M.; Levy, D.; Pozos, R.; Leggett, S.; Resnick, D. Relationships between myoelectric activity, strength, and MRI of the lumbar extensor muscles in back pain patients and normal subjects. J. Spinal Disord. 1997, 10, 348–356. [Google Scholar] [CrossRef]
- Risch, S.; Norvell, N.; Pollock, M.; Risch, E.; Langer, H.; Fulton, M.; Graves, J.E.; Leggett, S. Lumbar strengthening in chronic low back pain patients: Physiological and psychosocial benefits. Spine 1993, 18, 232–238. [Google Scholar] [CrossRef]
- Corso, M.; Cancelliere, C.; Mior, S.; Salmi, L.R.; Cedraschi, C.; Nordin, M.; Taylor-Vaisey, A.; Côté, P. Are non-pharmacological interventions delivered through synchronous telehealth as effective and safe as in-person interventions for the management of patients with non-acute musculoskeletal conditions? A systematic rapid review. Arch. Phys. Med. Rehabil. 2022, 103, 145–154.e11. [Google Scholar] [CrossRef] [PubMed]
- Raiszadeh, K.; Tapicer, J.; Taitano, L.; Wu, J.; Shahidi, B. In-clinic versus web-based multidisciplinary exercise-based rehabilitation for treatment of low back pain: Prospective clinical trial in an integrated practice unit model. J. Med. Internet Res. 2021, 23, e22548. [Google Scholar] [CrossRef] [PubMed]
- Grundstein, M.J.; Fisher, C.; Titmuss, M.; Cioppa-Mosca, J. The role of virtual physical therapy in a post-pandemic world: Pearls, pitfalls, challenges, and adaptations. Phys. Ther. 2021, 101, pzab145. [Google Scholar] [CrossRef] [PubMed]
- Shephard, R.J. PAR-Q, Canadian home fitness test, and exercise screening alternatives. Sports Med. 1988, 5, 1985–1995. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Mayer, J.M.; Graves, J.E.; Robertson, V.L.; Pierra, E.A.; Verna, J.L.; Ploutz-Snyder, L.L. Electromyographic activity of the lumbar extensor muscles: Effect of angle and hand position during Roman chair exercise. Arch. Phys. Med. Rehabil. 1999, 80, 751–755. [Google Scholar] [CrossRef]
- Mayer, J.M.; Verna, J.L.; Manini, T.; Mooney, V.; Graves, J.E. Electromyographic activity of the trunk extensor muscles: Effect of varying hip position and lumbar posture during Roman chair exercise. Arch. Phys. Med. Rehabil. 2002, 83, 1543–1546. [Google Scholar] [CrossRef] [PubMed]
- Graves, J.E.; Pollock, M.L.; Carpenter, D.M.; Leggett, S.H.; Jones, A.; MacMillan, M.; Fulton, M. Quantitative assessment of full range-of-motion isometric lumbar extension strength. Spine 1990, 15, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Konrad, P. The ABC of EMG. A Practical Introduction to Kinesiological Electromyography; Noraxon USA Inc.: Scottsdale, AZ, USA, 2005; pp. 1–60. [Google Scholar]
- Noraxon USA Inc. MyoSystem 1400. Operation & Technical Manual; Noraxon USA, Inc.: Scottsdale, AZ, USA, 2010; pp. 1–29. [Google Scholar]
- MedX Corp. Lumbar Extension Machine Instructional Manual; MedX Corp.: Altamonte Springs, FL, USA, 2004; pp. 1–67. [Google Scholar]
- Clark, B.C.; Manini, T.M.; Ploutz-Snyder, L.L. Derecruitment of the lumbar musculature with fatiguing trunk extension exercise. Spine 2003, 28, 282–287. [Google Scholar] [CrossRef]
- Mayer, J.M.; Graves, J.E.; Clark, B.C.; Formikell, M.; Ploutz-Snyder, L.L. The use of magnetic resonance imaging to evaluate lumbar muscle activity during trunk extension exercise at varying intensities. Spine 2005, 30, 2556–2563. [Google Scholar] [CrossRef] [PubMed]
- Shirado, O.; Ito, T.; Kaneda, K.; Strax, T.E. Flexion-relaxation phenomenon in the back muscles. a comparative study between healthy subjects and patients with chronic low back pain. Am. J. Phys. Med. Rehabil. 1995, 74, 139–144. [Google Scholar] [PubMed]
- American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription, 11th ed.; Wolters Kluwer Health: Philadelphia, PA, USA, 2021. [Google Scholar]
- Verna, J.L.; Mayer, J.M.; Mooney, V.; Pierra, E.A.; Robertson, V.L.; Graves, J.E. Back extension endurance and strength: The effect of variable-angle roman chair exercise training. Spine 2002, 27, 1772–1777. [Google Scholar] [CrossRef]
- Fritz, J.M.; Lane, E.; Minick, K.I.; Bardsley, T.; Brennan, G.; Hunter, S.J.; McGee, T.; Rassu, F.S.; Wegener, S.T.; Skolasky, R.L. Perceptions of telehealth physical therapy among patients with chronic low back pain. Telemed. Rep. 2021, 2, 258–263. [Google Scholar] [CrossRef]
- Official Disability Guidelines (ODG). Medical Treatment Guidelines: Lumbar Extension Exercise Equipment for Low Back Conditions; and MedX Lumbar Extension Machine for Low Back Conditions; MCG Health: Austin, TX, USA, 2021; Available online: https://www.mcg.com/odg/ (accessed on 23 December 2021).
- George, S.Z.; Fritz, J.M.; Silfies, S.P.; Schneider, M.J.; Beneciuk, J.M.; Lentz, T.A.; Gilliam, J.R.; Hendren, S.; Norman, K.S. Interventions for the management of acute and chronic low back pain: Revision 2021. J. Orthop. Sports. Phys. Ther. 2021, 51, CPG1–CPG60. [Google Scholar] [CrossRef] [PubMed]


| Variable | Total (n = 10) | Female (n = 5) | Male (n = 5) | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| Age (year) | 33.0 | 8.4 | 29.0 | 9.5 | 37.0 | 5.5 |
| Body Height (cm) | 174.0 | 6.9 | 170.7 | 8.1 | 177.3 | 3.3 |
| Body Weight (kg) | 76.2 | 18.4 | 62.3 | 9.8 | 90.2 | 13.4 |
| Peak IM torque (N-m) | 392.0 | 190.5 | 254.2 | 95.3 | 529.9 | 157.8 |
| Exercise Load | ||||||
|---|---|---|---|---|---|---|
| 1.00 BW | 1.25 BW | 1.50 BW | ||||
| Mean | SD | Mean | SD | Mean | SD | |
| Full Repetition | 34.9 | 16.0 | 42.1 | 11.8 | 47.1 | 9.8 |
| Concentric Phase: | ||||||
| Full Concentric Phase | 41.2 | 17.9 | 50.5 | 16.2 | 52.8 | 10.3 |
| Flexion Position | 33.0 | 16.1 | 36.6 | 16.6 | 37.7 | 11.3 |
| Mid Position | 40.1 | 19.9 | 50.0 | 16.3 | 50.8 | 8.7 |
| Extension Position | 50.4 | 21.9 | 65.0 | 20.7 | 69.9 | 16.0 |
| Eccentric Phase: | ||||||
| Full Eccentric Phase | 28.7 | 16.0 | 33.6 | 12.7 | 41.4 | 13.8 |
| Flexion Position | 23.3 | 14.9 | 27.4 | 12.7 | 31.2 | 13.0 |
| Mid Position | 27.3 | 16.8 | 30.4 | 13.4 | 38.5 | 12.3 |
| Extension Position | 35.3 | 18.5 | 42.9 | 14.4 | 54.7 | 27.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mayer, J.M.; Udermann, B.E.; Verna, J.L. Electromyographic Analysis of the Lumbar Extensor Muscles during Dynamic Exercise on a Home Exercise Device. J. Funct. Morphol. Kinesiol. 2022, 7, 26. https://doi.org/10.3390/jfmk7010026
Mayer JM, Udermann BE, Verna JL. Electromyographic Analysis of the Lumbar Extensor Muscles during Dynamic Exercise on a Home Exercise Device. Journal of Functional Morphology and Kinesiology. 2022; 7(1):26. https://doi.org/10.3390/jfmk7010026
Chicago/Turabian StyleMayer, John M., Brian E. Udermann, and Joe L. Verna. 2022. "Electromyographic Analysis of the Lumbar Extensor Muscles during Dynamic Exercise on a Home Exercise Device" Journal of Functional Morphology and Kinesiology 7, no. 1: 26. https://doi.org/10.3390/jfmk7010026
APA StyleMayer, J. M., Udermann, B. E., & Verna, J. L. (2022). Electromyographic Analysis of the Lumbar Extensor Muscles during Dynamic Exercise on a Home Exercise Device. Journal of Functional Morphology and Kinesiology, 7(1), 26. https://doi.org/10.3390/jfmk7010026






