Repeatability of Motion Health Screening Scores Acquired from a Three-Dimensional Markerless Motion Capture System
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
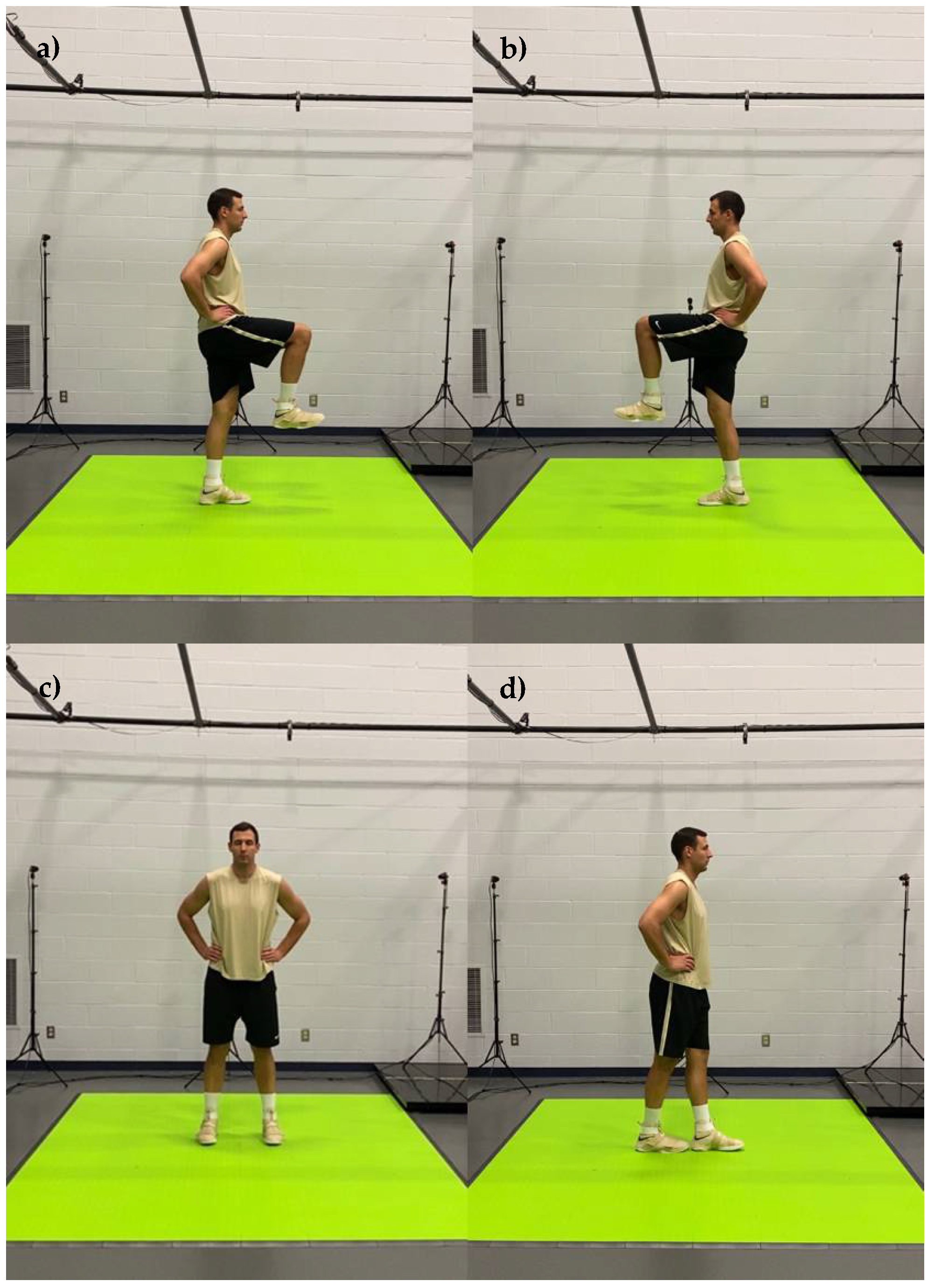
2.2. Procedures
2.3. Statistical Analysis
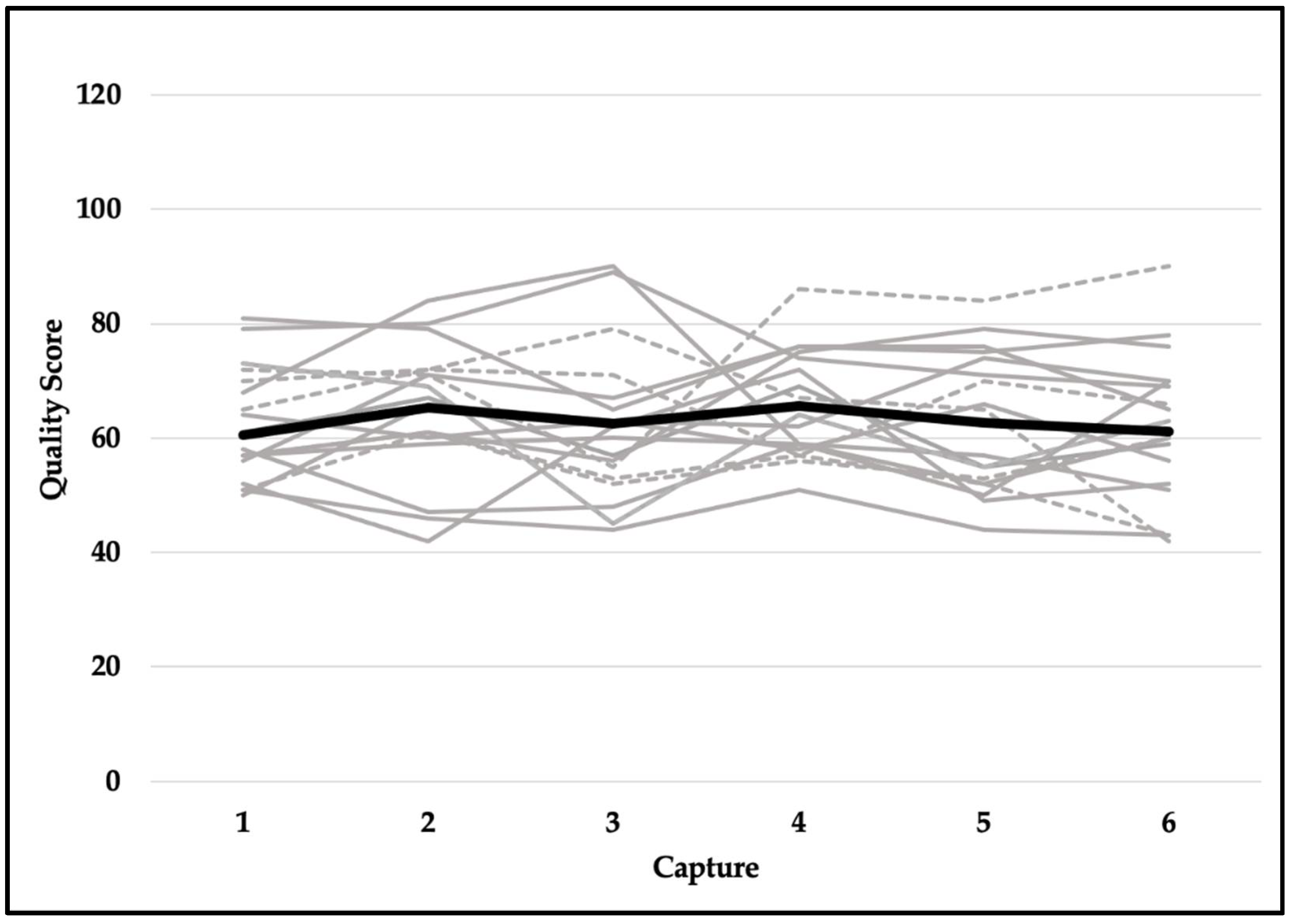
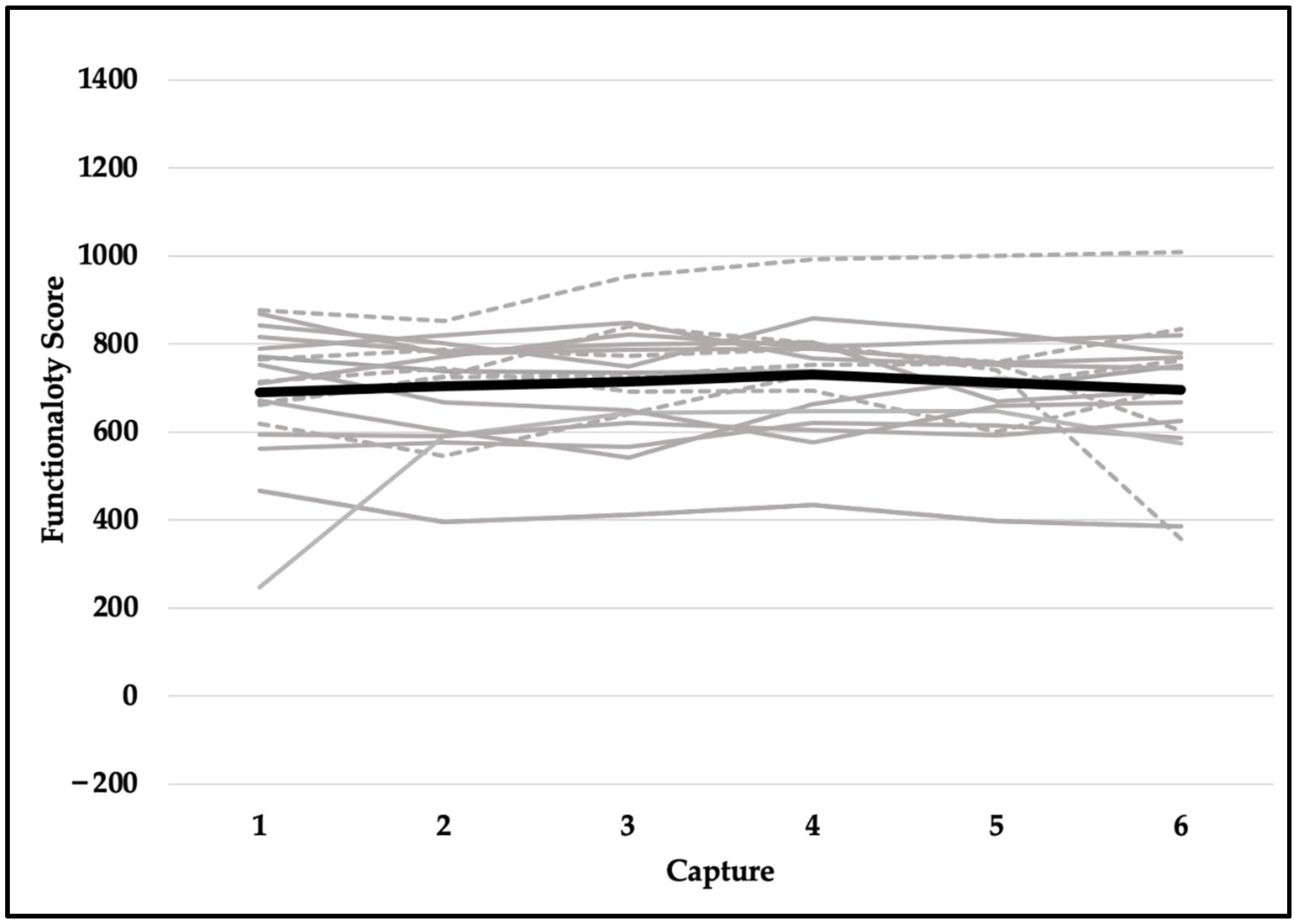
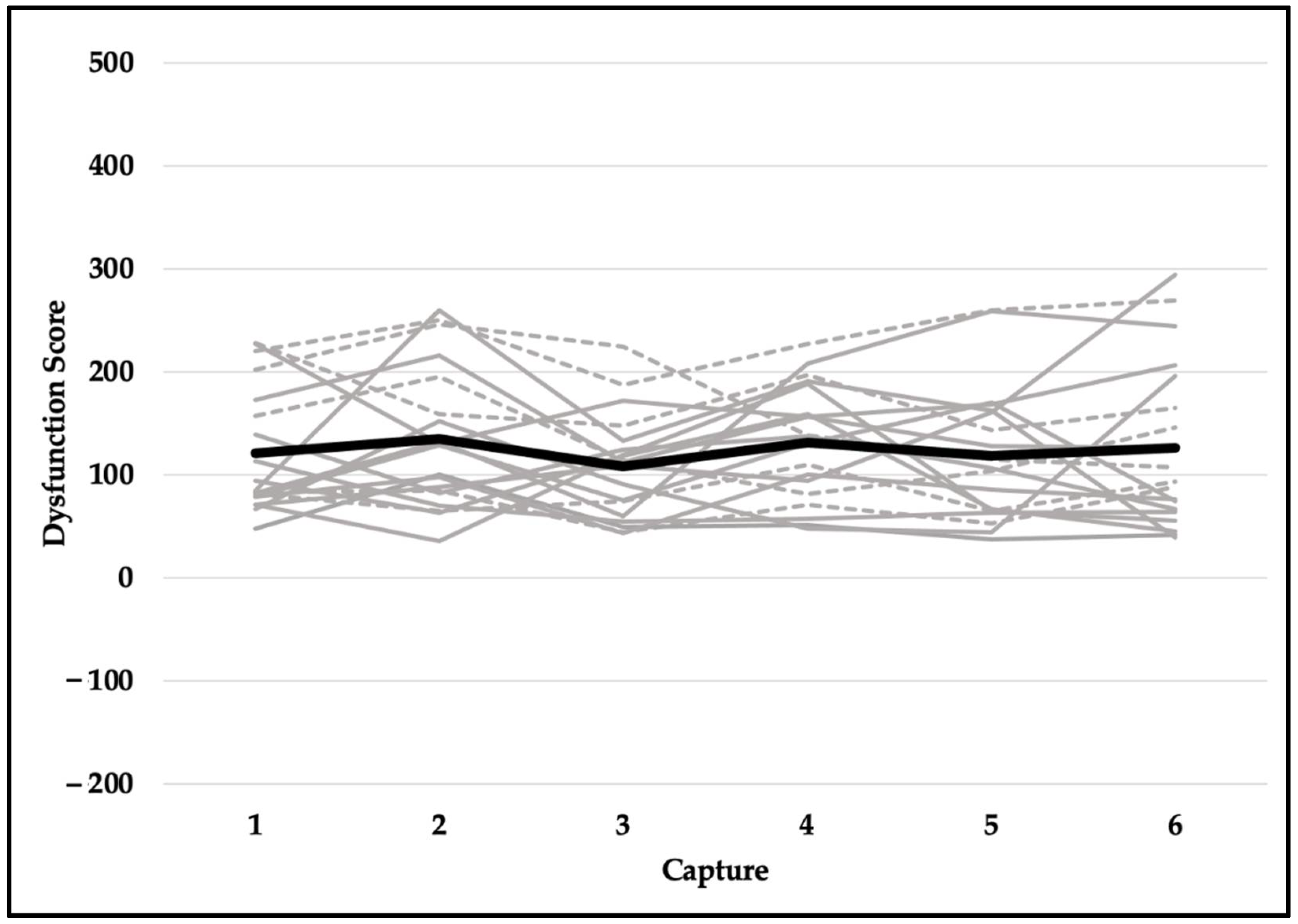
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bird, M.B.; Mi, Q.; Koltun, K.J.; Lovalekar, M.; Martin, B.J.; Fain, A.; Nindl, B.C. Unsupervised clustering techniques identify movement strategies in the countermovement jump associated with musculoskeletal injury risk during US marine corps officer candidates school. Front. Phys. 2022, 13, 787. [Google Scholar] [CrossRef] [PubMed]
- Daggett, M.C.; Witte, K.A.; Cabarkapa, D.; Cabarkapa, D.V.; Fry, A.C. Evidence-based data models for return-to-play criteria after anterior cruciate ligament reconstruction. Healthcare 2022, 10, 929. [Google Scholar] [CrossRef]
- Weinhandl, J.T.; Armstrong, B.S.; Kusik, T.P.; Barrows, R.T.; O’Connor, K.M. Validation of a single camera three-dimensional motion tracking system. J. Biomech. 2010, 43, 1437–1440. [Google Scholar] [CrossRef]
- Pfister, A.; West, A.M.; Bronner, S.; Noah, J.A. Comparative abilities of Microsoft Kinect and Vicon 3D motion capture for gait analysis. J. Med. Eng. Technol. 2014, 38, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Brink, Y.; Louw, Q.; Grimmer, K.; Schreve, K.; Van der Westhuizen, G.; Jordaan, E. Development of a cost effective three-dimensional posture analysis tool: Validity and reliability. BMC Musculoskelet. Disord. 2013, 14, 335. [Google Scholar] [CrossRef]
- Dutta, T. Evaluation of the Kinect™ sensor for 3-D kinematic measurement in the workplace. Appl. Ergon. 2012, 43, 645–649. [Google Scholar] [CrossRef]
- Harsted, S.; Holsgaard-Larsen, A.; Hestbæk, L.; Boyle, E.; Lauridsen, H.H. Concurrent validity of lower extremity kinematics and jump characteristics captured in pre-school children by a markerless 3D motion capture system. Chirop. Man. Ther. 2019, 27, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Clark, R.A.; Pua, Y.H.; Fortin, K.; Ritchie, C.; Webster, K.E.; Denehy, L.; Bryant, A.L. Validity of the Microsoft Kinect for assessment of postural control. Gait Posture 2012, 36, 372–377. [Google Scholar] [CrossRef]
- Corazza, S.; Muendermann, L.; Chaudhari, A.M.; Demattio, T.; Cobelli, C.; Andriacchi, T.P. A markerless motion capture system to study musculoskeletal biomechanics: Visual hull and simulated annealing approach. Ann. Biomed. Eng. 2006, 34, 1019–1029. [Google Scholar] [CrossRef]
- Monaghan, K.; Delahunt, E.; Caulfield, B. Increasing the number of gait trial recordings maximises intra-rater reliability of the CODA motion analysis system. Gait Posture 2007, 25, 303–315. [Google Scholar] [CrossRef] [PubMed]
- Ferber, R.; McClay Davis, I.; Williams III, D.S.; Laughton, C. A comparison of within-and between-day reliability of discrete 3D lower extremity variables in runners. J. Orthop. Res. 2002, 20, 1139–1145. [Google Scholar] [CrossRef]
- Windolf, M.; Gotzen, N.; Morlock, M. Systematic accuracy and precision analysis of video motion capturing systems—Exemplified on the Vicon-460 system. J. Biomech. 2008, 41, 2776–2780. [Google Scholar] [CrossRef] [PubMed]
- Bilesan, A.; Owlia, M.; Behzadipour, S.; Ogawa, S.; Tsujita, T.; Komizunai, S.; Konno, A. Marker-based motion tracking using Microsoft Kinect. IFAC-PapersOnLine 2018, 51, 399–404. [Google Scholar] [CrossRef]
- Cabarkapa, D.; Fry, A.C.; Mosier, E.M. Validity of 3-D markerless motion capture system for assessing basketball dunk kinetics—A case study. Sport J. 2020. Available online: https://thesportjournal.org/article/tag/basketball/ (accessed on 18 June 2022).
- Cabarkapa, D.; Whetstone, J.M.; Patterson, A.M.; Mosier, E.M.; Cabarkapa, D.V.; Fry, A.C. Relationship between health-related physical fitness parameters and functional movement screening scores acquired from a three-dimensional markerless motion capture system. Int. J. Environ. Res. Public Health 2022, 19, 4551. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Hando, B.R.; Scott, W.C.; Bryant, J.F.; Tchandja, J.N.; Scott, R.M.; Angadi, S.S. Association between markerless motion capture screenings and musculoskeletal injury risk for military trainees: A large cohort and reliability study. Orthop. J. Sports Med. 2021, 9, 23259671211041656. [Google Scholar] [CrossRef] [PubMed]
- Martinez, H.R.; Garcia-Sarreon, A.; Camara-Lemarroy, C.; Salazar, F.; Guerrero-González, M.L. Accuracy of markerless 3D motion capture evaluation to differentiate between on/off status in Parkinson’s disease after deep brain stimulation. Parkinson’s Dis. 2018, 2018, 5830364. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Specific Body Movement | Description of Movement |
|---|---|
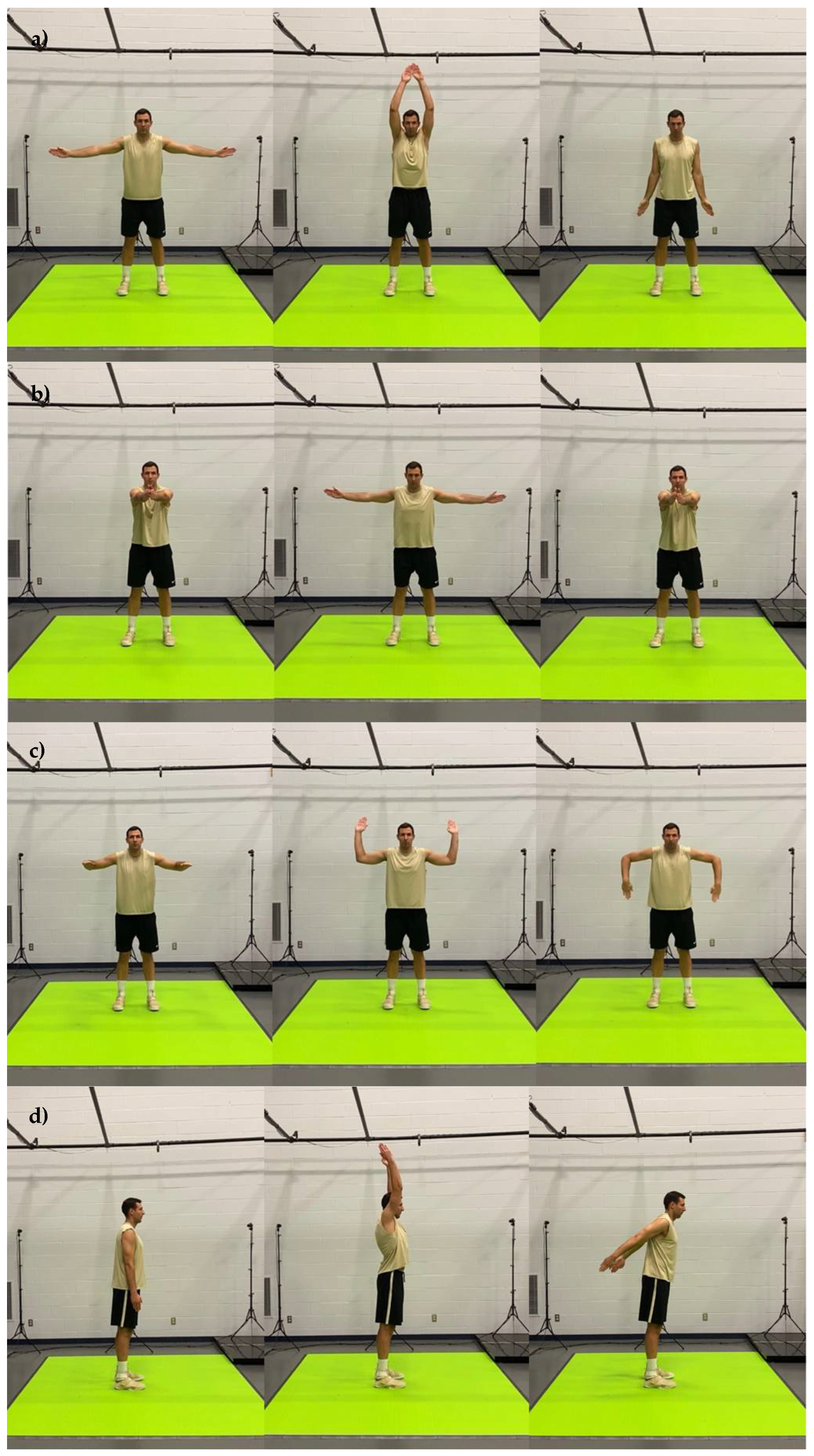
| Shoulder abduction and adduction | Start with arms out in a T-position, raise arms overhead and lower hands to sides. |
| Shoulder horizontal abduction | Start with arms straight-out in front of body, separating arms, reach back behind body and return to the starting position. |
| Shoulder internal and external rotation | Start with arms in a goalpost position, holding this position, rotate arms upward and back, followed by rotating arms forward and down. |
| Shoulder flexion and extension | Start with arms to side and with palms facing inward, raise arms upward as far as possible and then back as far as possible. |
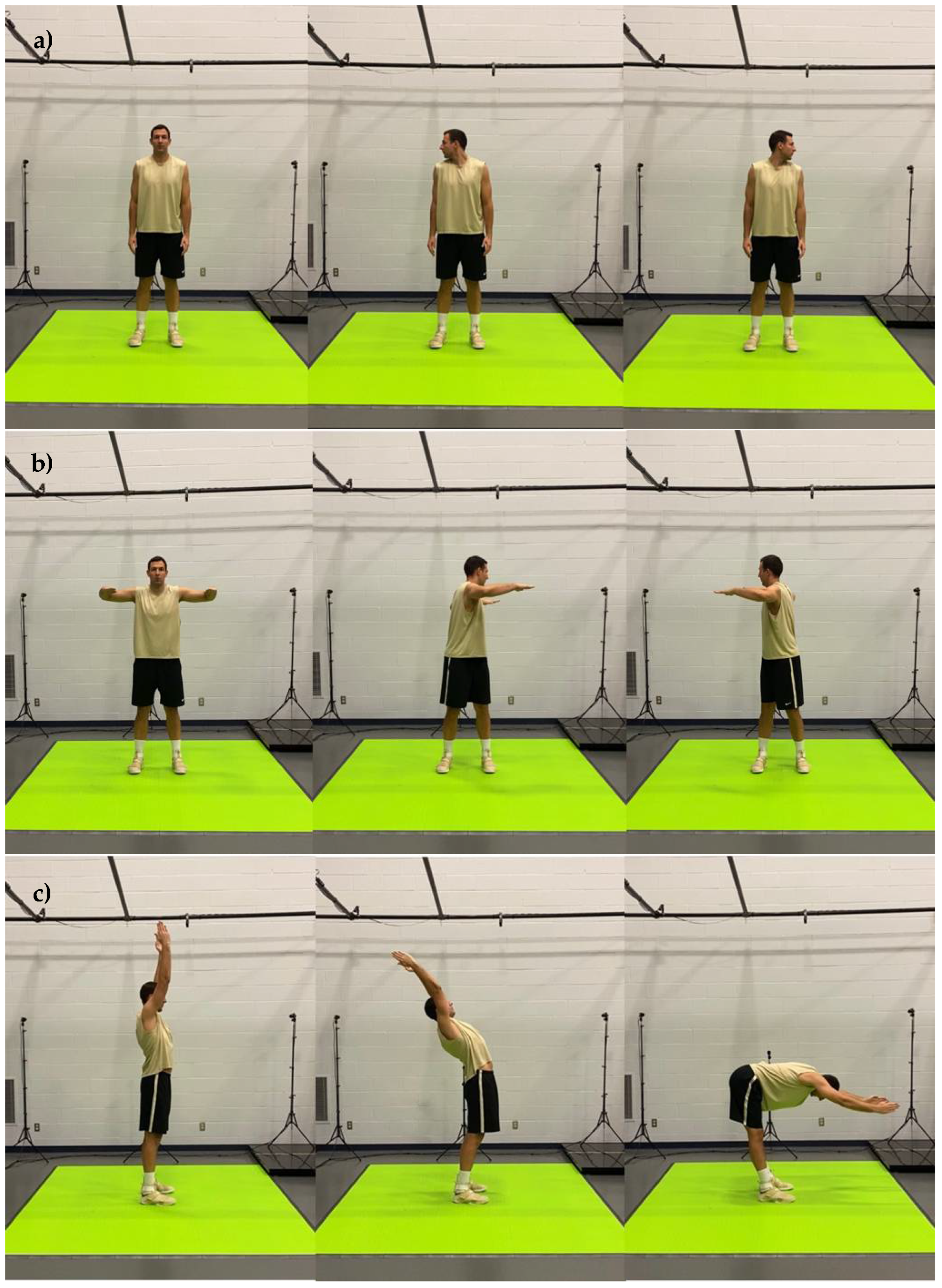
| Cervical rotation | Start with the head facing forward and rotate the head as far to the right as possible, then as far to the left as possible. |
| Trunk rotation | Start with arms upward and in a goalpost position, then rotate as far as possible to the left and then as far as possible to the right, keeping hips in a forward position. |
| Trunk extension and flexion | Start with arms overhead and lean back as far as possible, then return to start position and bend forward as far as possible (trying to touch toes), keeping legs as straight as possible. |
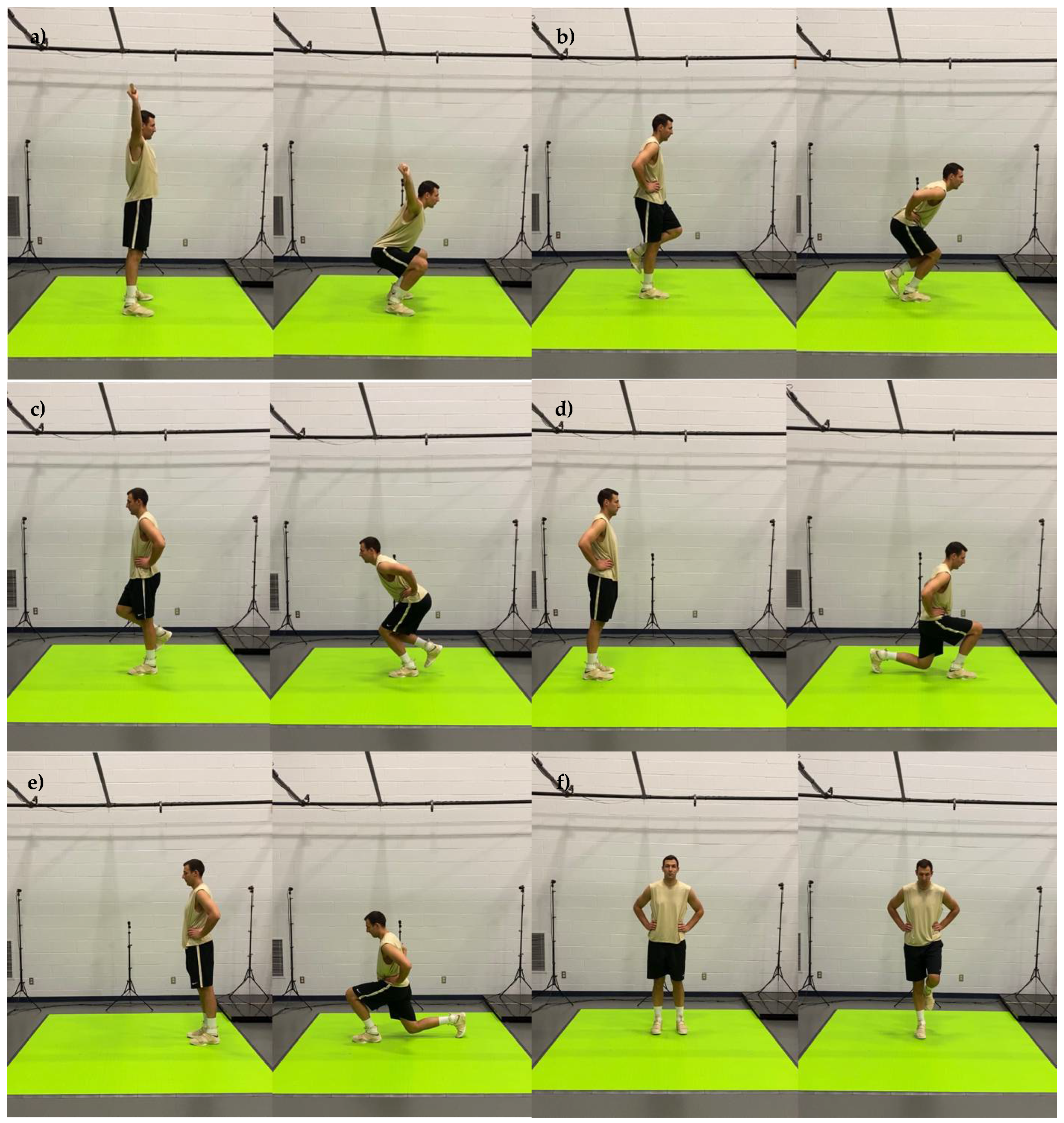
| Bilateral squat | Start with feet forward and shoulder distance apart, and while holding a light bar directly above head, lower body downward as far as possible. |
| Right leg squat | Start by raising left foot off the ground and while balancing on the right leg, lower body down as far as possible on the standing leg and return to the starting position. |
| Left leg squat | Start by raising right foot off the ground and while balancing on the left leg, lower body down as far as possible on the standing leg and return to the starting position. |
| Right leg lunge | Start with body and feet in a forward position, then take a big step forward with right foot only and lower body toward the ground. Return to the starting position. |
| Left leg lunge | Start with body and feet in a forward position, then take a big step forward with left foot only and lower body toward the ground. Return to the starting position. |
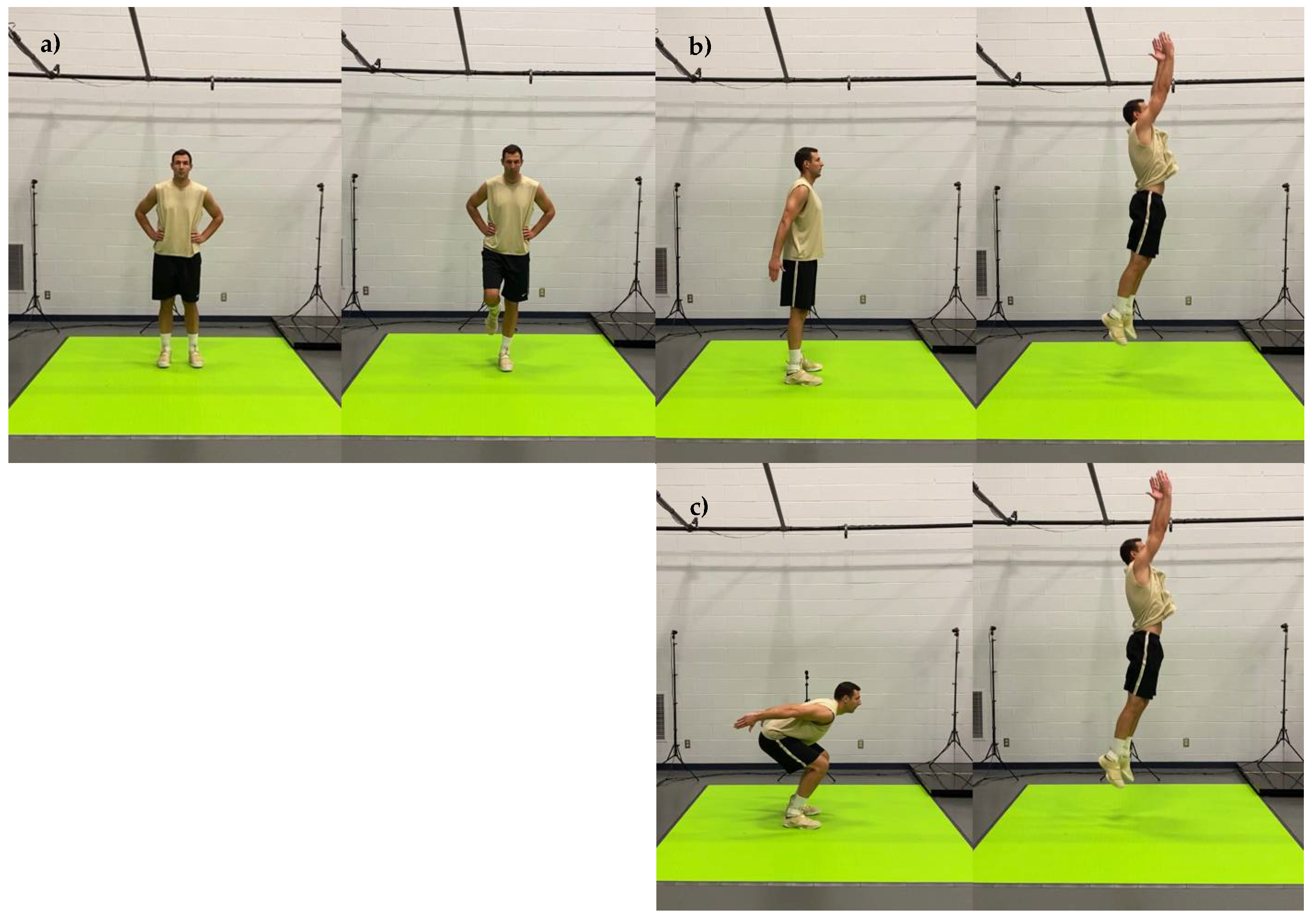
| Right leg balance | Start with the body and feet in a forward position, then raise the left slightly off the ground. Standing on the right leg, balance body for 30 s. Hopping on one leg is allowed as long as the left foot does not touch the ground. |
| Left leg balance | Start with body and feet in a forward position, then raise the right leg slightly off the ground. Standing on the left leg, balance body for 30 s. Hopping on one leg is allowed as long as the right foot does not touch the ground. |
| Bilateral standing vertical jump | Start with feet forward, legs straight and arms extended backwards as far as possible, then jump as high as possible off both legs. |
| Concentric jump | Start with feet forward, legs bent to a near 90-degree angle and arms extended backwards as far as possible, then jump as high as possible off both legs. |
| Right stork stance | Start with body and feet in a forward position, then raise the left leg upward to a near 90-degree angle. Close eyes and standing on the right leg, balance body for 20 s. Hopping on one leg is allowed as long as left foot does not touch the ground. |
| Left stork stance | Start with body and feet in a forward position, then raise the right leg upward to a near 90-degree angle. Close eyes and standing on the left leg, balance body for 20 s. Hopping on one leg is allowed as long as right foot does not touch the ground. |
| Standing double leg balance | Start with body and feet in a forward position. With feet together, close eyes and balance body for 20 s. |
| Tandem stance balance | Start with body in a forward position and place one foot directly in front of the other foot in a forward position. Close eyes and balance body for 20 s. |
| Dependent Variable | Capture 1 | Capture 2 | Capture 3 |
| Quality | 60.6 ± 12.1 | 65.4 ± 11.5 | 62.5 ± 13.0 |
| Readiness | 834.6 ± 198.8 | 821.1 ± 191.6 | 850.9 ± 186.7 |
| Explosiveness | 277.7 ± 73.7 | 252.7 ± 74.9 | 229.7 ± 126.3 |
| Functionality | 690.3 ± 151.3 | 702.9 ± 123.3 | 713.3 ± 126.9 |
| Dysfunction | 121.0 ± 60.9 | 134.5 ± 69.3 | 107.9 ± 50.6 |
| Dependent Variable | Capture 4 | Capture 5 | Capture 6 |
| Quality | 65.7 ± 9.2 | 62.7 ± 11.8 | 61.2 ± 12.9 |
| Readiness | 863.6 ± 232.3 | 859.5 ± 217.9 | 860.4 ± 249.1 |
| Explosiveness | 265.7 ± 101.6 | 266.4 ± 93.0 | 290.8 ± 126.2 |
| Functionality | 729.4 ± 121.5 | 711.8 ± 122.4 | 695.3 ± 155.5 |
| Dysfunction | 131.5 ± 55.8 | 118.7 ± 66.1 | 126.1 ± 80.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cabarkapa, D.; Cabarkapa, D.V.; Philipp, N.M.; Downey, G.G.; Fry, A.C. Repeatability of Motion Health Screening Scores Acquired from a Three-Dimensional Markerless Motion Capture System. J. Funct. Morphol. Kinesiol. 2022, 7, 65. https://doi.org/10.3390/jfmk7030065
Cabarkapa D, Cabarkapa DV, Philipp NM, Downey GG, Fry AC. Repeatability of Motion Health Screening Scores Acquired from a Three-Dimensional Markerless Motion Capture System. Journal of Functional Morphology and Kinesiology. 2022; 7(3):65. https://doi.org/10.3390/jfmk7030065
Chicago/Turabian StyleCabarkapa, Dimitrije, Damjana V. Cabarkapa, Nicolas M. Philipp, Gabriel G. Downey, and Andrew C. Fry. 2022. "Repeatability of Motion Health Screening Scores Acquired from a Three-Dimensional Markerless Motion Capture System" Journal of Functional Morphology and Kinesiology 7, no. 3: 65. https://doi.org/10.3390/jfmk7030065
APA StyleCabarkapa, D., Cabarkapa, D. V., Philipp, N. M., Downey, G. G., & Fry, A. C. (2022). Repeatability of Motion Health Screening Scores Acquired from a Three-Dimensional Markerless Motion Capture System. Journal of Functional Morphology and Kinesiology, 7(3), 65. https://doi.org/10.3390/jfmk7030065







