Pain Education in the Management of Patients with Chronic Low Back Pain: A Systematic Review
Abstract
:1. Introduction
1.1. Pathology and Intervention
1.2. Objective
2. Methods
2.1. Protocol
2.2. Inclusion and Exclusion Criteria
2.2.1. Types of Studies
2.2.2. Types of Participants
Inclusion Criteria
- Studies that admitted, as elements of comparison, the conventional low back pain physiotherapeutic protocols.
- Studies that presented additional intervention groups (in addition to the one identified as the experimental group and the control group).
Exclusion Criteria
- Back pain, post-operative lumbar pain and lumbar pain related to specific pathologies;
- Populations with individuals under the age of 18;
- Cardiovascular, psychiatric, rheumatic, neoplastic or inflammatory pathologies.
- Studies that comprised additional pharmacological, instrumental or other interventions, not attributable to physiotherapy techniques.
2.2.3. Types of Outcome
2.3. Bibliographic Research
3. Results
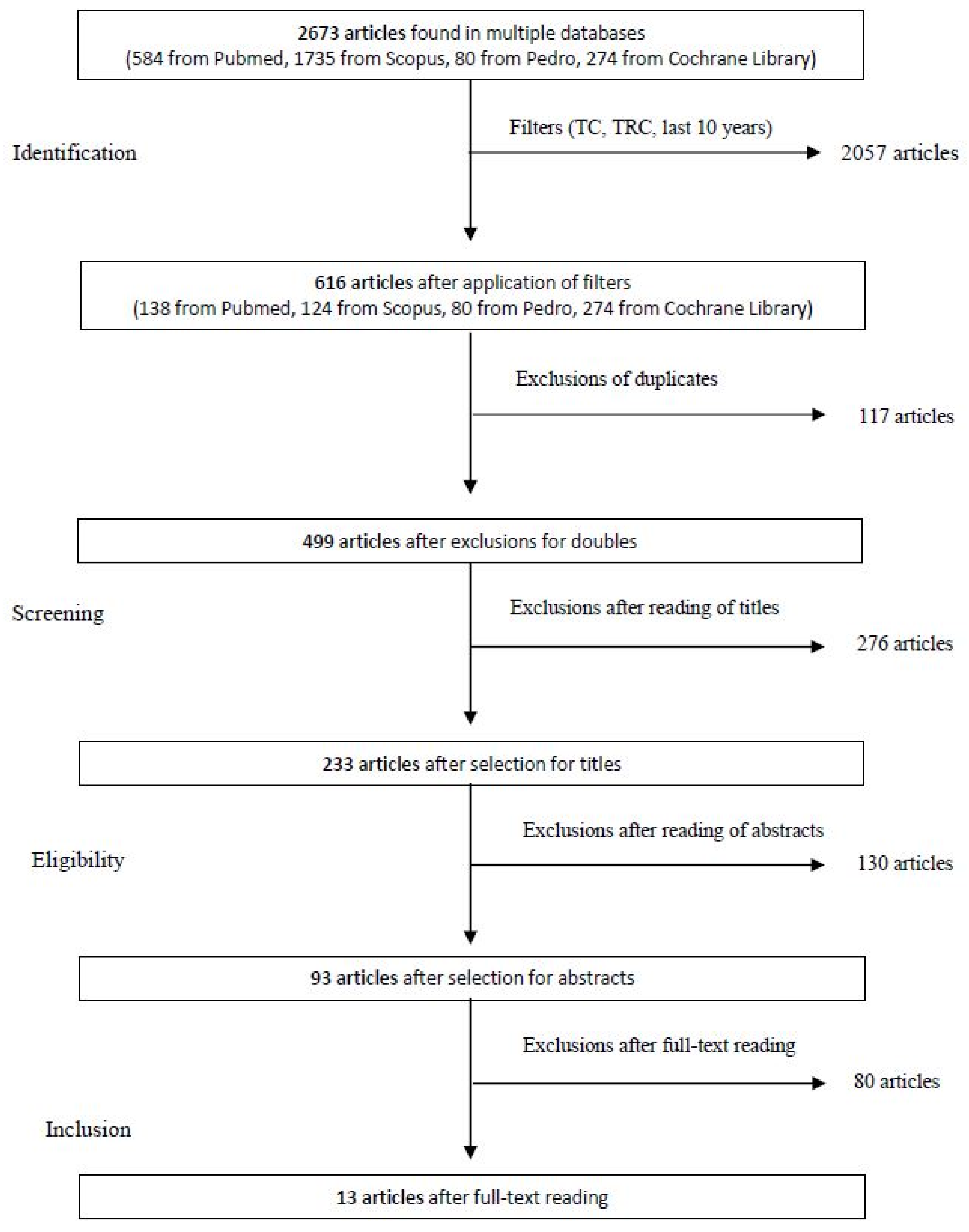
3.1. Selection of the Articles
3.2. Bias Risk Assessment in the Included Studies
3.3. Evaluation of External Validity or “Applicability”
3.4. Extractions and Characteristics of Datas
- General information: Author, year of publication, study design and level of evidence of the study;
- Participants: sample size, age of participants and duration of pain;
- Interventions/Controls: number of participants for each group (experimental and control), content, number of interventions;
- Outcome: type of outcome taken into consideration;
- Follow-up(s): baseline, post-treatment and re-evaluations;
- Results: summary of the results obtained, with mean difference (and standard deviation);
- Score on the PEDro scale.
4. Discussion
Limits of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grotle, M.; Vøllestad, N.K.; Veierød, M.B.; Brox, J.I. Fear-Avoidance Beliefs and Distress in Relation to Disability in Acute and Chronic Low Back Pain. Pain 2004, 112, 343–352. [Google Scholar] [CrossRef] [PubMed]
- Picavet, H.S.J. Pain Catastrophizing and Kinesiophobia: Predictors of Chronic Low Back Pain. Am. J. Epidemiol. 2002, 156, 1028–1034. [Google Scholar] [CrossRef] [PubMed]
- Linton, S.J. Models of Pain Perception. In Understanding Pain for Better Clinical Practice: A Psychological Perspective; Elsevier: Amsterdam, The Netherlands, 2005; pp. 9–18. [Google Scholar]
- Schaible, H.-G.; Richter, F. Pathophysiology of Pain. Langenbecks Arch. Surg. 2004, 389, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Adams, L.; Turk, D. Psychosocial Factors and Central Sensitivity Syndromes. Curr. Rheumatol. Rev. 2015, 11, 96–108. [Google Scholar] [CrossRef]
- Nijs, J.; Paul van Wilgen, C.; Van Oosterwijck, J.; van Ittersum, M.; Meeus, M. How to Explain Central Sensitization to Patients with ‘Unexplained’ Chronic Musculoskeletal Pain: Practice Guidelines. Man. Ther. 2011, 16, 413–418. [Google Scholar] [CrossRef]
- Louw, A.; Diener, I.; Butler, D.S.; Puentedura, E.J. The Effect of Neuroscience Education on Pain, Disability, Anxiety, and Stress in Chronic Musculoskeletal Pain. Arch. Phys. Med. Rehabil. 2011, 92, 2041–2056. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Stone, P.W. Popping the (PICO) Question in Research and Evidence-Based Practice. Appl. Nurs. Res. 2002, 15, 197–198. [Google Scholar] [CrossRef]
- de Morton, N.A. The PEDro Scale Is a Valid Measure of the Methodological Quality of Clinical Trials: A Demographic Study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef]
- Bodes Pardo, G.; Lluch Girbés, E.; Roussel, N.A.; Gallego Izquierdo, T.; Jiménez Penick, V.; Pecos Martín, D. Pain Neurophysiology Education and Therapeutic Exercise for Patients With Chronic Low Back Pain: A Single-Blind Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2018, 99, 338–347. [Google Scholar] [CrossRef]
- Cherkin, D.C.; Sherman, K.J.; Baloerson, B.H.; Cook, A.J.; Anderson, M.L.; Hawkes, R.J.; Hansen, K.E.; Turner, J.A. Effect of Mindfulness-Based Stress Reduction vs Cognitive Behavioral Therapy or Usual Care on Back Pain and Functional Limitations in Adults With Chronic Low Back Pain: A Randomized Clinical Trial. JAMA 2016, 315, 1240. [Google Scholar] [CrossRef]
- Díaz-Cerrillo, J.L.; Rondón-Ramos, A.; Pérez-González, R.; Clavero-Cano, S. Ensayo no aleatorizado de una intervención educativa basada en principios cognitivo-conductuales para pacientes con lumbalgia crónica inespecífica atendidos en fisioterapia de atención primaria. Aten. Primaria 2016, 48, 440–448. [Google Scholar] [CrossRef]
- Khodadad, B.; Letafatkar, A.; Hadadnezhad, M.; Shojaedin, S. Comparing the Effectiveness of Cognitive Functional Treatment and Lumbar Stabilization Treatment on Pain and Movement Control in Patients With Low Back Pain. Sports Health Multidiscip. Approach 2020, 12, 289–295. [Google Scholar] [CrossRef]
- Louw, A.; Farrell, K.; Landers, M.; Barclay, M.; Goodman, E.; Gillund, J.; McCaffrey, S.; Timmerman, L. The Effect of Manual Therapy and Neuroplasticity Education on Chronic Low Back Pain: A Randomized Clinical Trial. J. Man. Manip. Ther. 2017, 25, 227–234. [Google Scholar] [CrossRef]
- O’Keeffe, M.; O’Sullivan, P.; Purtill, H.; Bargary, N.; O’Sullivan, K. Cognitive Functional Therapy Compared with a Group-Based Exercise and Education Intervention for Chronic Low Back Pain: A Multicentre Randomised Controlled Trial (RCT). Br. J. Sports Med. 2020, 54, 782–789. [Google Scholar] [CrossRef]
- Petrozzi, M.J.; Leaver, A.; Ferreira, P.H.; Rubinstein, S.M.; Jones, M.K.; Mackey, M.G. Addition of MoodGYM to Physical Treatments for Chronic Low Back Pain: A Randomized Controlled Trial. Chiropr. Man. Ther. 2019, 27, 54. [Google Scholar] [CrossRef]
- Pincus, T.; Anwar, S.; McCracken, L.M.; McGregor, A.; Graham, L.; Collinson, M.; McBeth, J.; Watson, P.; Morley, S.; Henderson, J.; et al. Delivering an Optimised Behavioural Intervention (OBI) to People with Low Back Pain with High Psychological Risk; Results and Lessons Learnt from a Feasibility Randomised Controlled Trial of Contextual Cognitive Behavioural Therapy (CCBT) vs. Physiotherapy. BMC Musculoskelet. Disord. 2015, 16, 147. [Google Scholar] [CrossRef]
- Rabiei, P.; Sheikhi, B.; Letafatkar, A. Comparing Pain Neuroscience Education Followed by Motor Control Exercises With Group-Based Exercises for Chronic Low Back Pain: A Randomized Controlled Trial. Pain Pract. 2021, 21, 333–342. [Google Scholar] [CrossRef]
- Van Erp, R.M.A.; Huijnen, I.P.J.; Ambergen, A.W.; Verbunt, J.A.; Smeets, R.J.E.M. Biopsychosocial Primary Care versus Physiotherapy as Usual in Chronic Low Back Pain: Results of a Pilot-Randomised Controlled Trial. Eur. J. Physiother. 2021, 23, 3–10. [Google Scholar] [CrossRef]
- Semrau, J.; Hentschke, C.; Peters, S.; Pfeifer, K. Effects of Behavioural Exercise Therapy on the Effectiveness of Multidisciplinary Rehabilitation for Chronic Non-Specific Low Back Pain: A Randomised Controlled Trial. BMC Musculoskelet. Disord. 2021, 22, 500. [Google Scholar] [CrossRef]
- Vibe Fersum, K.; O’Sullivan, P.; Skouen, J.S.; Smith, A.; Kvåle, A. Efficacy of Classification-based Cognitive Functional Therapy in Patients with Non-specific Chronic Low Back Pain: A Randomized Controlled Trial. Eur. J. Pain 2013, 17, 916–928. [Google Scholar] [CrossRef]
- Wälti, P.; Kool, J.; Luomajoki, H. Short-Term Effect on Pain and Function of Neurophysiological Education and Sensorimotor Retraining Compared to Usual Physiotherapy in Patients with Chronic or Recurrent Non-Specific Low Back Pain, a Pilot Randomized Controlled Trial. BMC Musculoskelet. Disord. 2015, 16, 83. [Google Scholar] [CrossRef] [Green Version]
| Database | String Used | Note |
|---|---|---|
| Pubmed | (([pain education [MeSH Terms]) OR (cognitive behavior therapy [MeSH Terms])) AND (chronic low back pain [MeSH Terms])) AND (lumbar pain [MeSH Terms]) | - |
| Scopus | (TITLE-ABS-KEY (pain AND education) OR TITLE-ABS-KEY (cognitive AND behavior AND therapy) AND TITLE-ABS-KEY (chronic AND low AND back AND pain)) | - |
| Pedro | Abstract & title: pain education chronic low back pain; Method: clinical trial; Published since: 2011; Abstract & title: cognitive behavior therapy chronic low back pain; Method: clinical trial; Published since: 2011. | The results of the two researches were combined |
| Cochrane library | ((Title abstract keyword: pain education) AND (Title abstract keyword: chronic low back pain)) with Publication Year from 2011 to 2021, with Cochrane Library publication date from Sep 2011 to Sep 2021, in Trials; ((Title abstract keyword cognitive behavior therapy) AND (Title abstract keyword: chronic low back pain)) with Publication Year from 2011 to 2021, with Cochrane Library publication date from Sep 2011 to Sep 2021, in Trials. | The results of the two researches were combined |
| 1. Eligibility criteria were specified | no ❑ | yes ❑ | where: |
| 2. Subjects were randomly allocated to groups (in a crossover study, subjects were randomly allocated an order in which treatments were received) | no ❑ | yes ❑ | where: |
| 3. Allocation was concealed | no ❑ | yes ❑ | where: |
| 4. The groups were similar at baseline regarding the most important prognostic indicators | no ❑ | yes ❑ | where: |
| 5. There was blinding of all subjects | no ❑ | yes ❑ | where: |
| 6. There was blinding of all therapists who administered the therapy | no ❑ | yes ❑ | where: |
| 7. There was blinding of all assessors who measured at least one key outcome | no ❑ | yes ❑ | where: |
| 8. Measures of at least one key outcome were obtained from more than 85% of the subjects initially allocated to groups | no ❑ | yes ❑ | where: |
| 9. All subjects for whom outcome measures were available received the treatment or control condition as allocated or, where this was not the case, data for at least one key outcome was analysed by “intention to treat” | no ❑ | yes ❑ | where: |
| 10. The results of between-group statistical comparisons are reported for at least one key outcome | no ❑ | yes ❑ | where: |
| 11. The study provides both point measures and measures of variability for at least one key outcome | no ❑ | yes ❑ | where: |
| 1-Eligibility Criteria | 2-Randomization? | 3-Hidden Assignment? | 4-Homogeneity of the Groups? | 5-Blindness of the Subjects? | 6-Blindness of Therapists? | 7-Blindness of the Evaluators? | 8-Subject to Follow-Up? | 9-Intention to Treat? | 10-Statistical Comparison between Groups? | 11-Measurements of Magnitude and Variability? | PEDro Score | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GB Pardo et al. (2017) [12] | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✓ | ✗ | ✓ | ✓ | 6/10 |
| DC Cherkin et al. (2016) [12] * | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✓ | 5/10 |
| JL Díaz-Cerrillo et al. (2015) [13] * | ✓ | ✗ | ✗ | ✓ | ✗ | ✗ | ✓ | ✓ | ✗ | ✓ | ✓ | 5/10 |
| B. Khodadad et al. (2019) [14]* | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✗ | ✓ | ✓ | 4/10 |
| A. Louw et al. (2016) [15] | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✓ | ✗ | ✓ | ✓ | 6/10 |
| M. O’Keeffe et al., (2019) [16] | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✓ | ✓ | ✓ | 6/10 |
| MJ Petrozzi et al. (2019) [17] | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ | 7/10 |
| T. Pincus et al. (2015) [18] | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✗ | ✓ | 4/10 |
| P. Rabiei, B. Sheikhi, A. Letafatkar (2021) [19] | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ | ✓ | ✗ | ✓ | ✓ | 6/10 |
| RMA Van Erp et al. (2019) [20] | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✗ | ✓ | ✓ | ✓ | 7/10 |
| J. Semrau et al. (2021) [21] | ✗ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✗ | ✓ | ✓ | ✓ | 8/10 |
| KV Fersum et al. (2013) [22] | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✗ | ✗ | ✓ | ✓ | 5/10 |
| P. Wälti et al. (2015) [23] | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | 8/10 |
| Level of Evidence (LOE) | Study/I. | PEDro Score (Ps) |
|---|---|---|
| Level I | J. Semrau et al. (2021) [21] P. Wälti et al. (2015) [23] | Ps ≥ 8/10 |
| Level II | GB Pardo et al. (2017) [11] DC Cherkin et al. (2016) [12] JL Díaz-Cerrillo et al. (2015) [13] A. Louw et al. (2016) [15] M. O’Keeffe et al., (2019) [16] MJ Petrozzi et al. (2019) [17] P. Rabiei, B. Sheikhi, A. Letafatkar (2021) [19] RMA Van Erp et al. (2019) [20] KV Fersum et al. (2013) [22] | 5/10 ≤ Ps <8/10 |
| Level III | B. Khodadad et al. (2019) [14] T. Pincus et al. (2015) [15] | Ps = 4/10 |
| Level IV | - | |
| Level V | - |
| Author and Year of Publication | Study Design and Level of Evidence (LOE) | No. of Patients (n), Characteristics and Duration of Symptoms (DDS) | Groups, Intervention and Number of Treatments (NT) | Outcome | Evaluations and Follow-Up | Summary of the Results | PEDro SCORE |
|---|---|---|---|---|---|---|---|
| GB Pardo et al. (2017) [11] | TRC LOE: II | n = 56 Age (years): 20–75 DDS ≥ 6 months | Experimental group n = 28 Motor control exercises, stretching, aerobic exercises, PNE Control group n = 28 Motor control exercises, stretching, aerobic exercises NT: Two sessions of 30–50 min each month apart + home exercises during the follow-up | PAIN: NRS DISABILITY: RDQ | Baseline 1 month 3 months | PAIN: although an improvement was observed in both groups, a significant difference was noticed the experimental group at each follow-up point (NRS: −2.2; −2.93, −1.28; p < 0.001; d = 1.37) DISABILITY: the results obtained on the RDQ also show significant improvements in favor of the experimental group (RDQ: −2.7; −3.9, −1.4), p < 0.001; d = 1.15) | 6/10 |
| DC Cherkin et al. (2016) [12] | TRC LOE: II | n = 342 males = 117 females = 225 Age (years): 20–70 (average 49) DDS: 3 months–50 years (mean 7.3 years) | Experimental group n = 113 (CBT, pain education and its relationship with worries and emotional state, relapse prevention, maintenance of improvements, relaxation techniques, pain adaptation strategies) Control group n = 113 (Any physiotherapy treatment the participants wanted to carry out) NT: 2 h per week for 8 weeks | PAIN: BPB DISABILITY: mRDQ | Baseline 4 weeks 8 weeks 26 weeks 52 weeks | PAIN: in terms of BPB, the participants who improved most consistently were those of the experimental group (45%) versus those of the control group (27%). DISABILITY: significant improvements were observed at 26 weeks, on the mRDQ, in a percentage manner higher for the experimental group (58%) than for the control group (44%). | 5/10 |
| JL Díaz-Cerrillo et al. (2015) [13] | quasiTRC LOE: II | n = 128 Males = 51 Females = 77 Age (years): 18–65 DDS > 3 months | Experimental group n = 64 Functional education, cognitive-behavioral education: cognitive restructuring, goal reorientation and attention deviation Control group n = 64 Functional education, strengthening and stretching exercises of the spine, physical activity at home NT: 7 | PAIN: NRS-11 DISABILITY: RDQ | Baseline Post intervention | Improvements were noted in both groups regarding the two outcome measures at the end of treatment. In addition, significant differences were observed between the two groups in favor of the experimental group as regards the reduction of the disability index, but not as regards the pain scale. PAIN: (p = 0.280) DISABILITY: (p = 0.046) | 5/10 |
| B. Khodadad et al. (2019) [14] | PRETEST-POSTTEST INTERVENTION LOE: III | n = 52 Age (years): mean 44.3 ± 2.46 VAS: 3/10–8/10 DDS > 3 months | Experimental group n = 17 CFT, pain physiology education, exercise, relaxation techniques, identification of incorrect movements and postures, aerobic exercise, stretching Control group n = 18 Traditional physiotherapy NT: Experimental group = Three sessions per week for 8 weeks Control group = not specified | PAIN: VAS | Baseline Post-surgery (8 weeks) | PAIN: An average decrease of 40% on the VAS was observed in the experimental group. No significant changes were observed for the same variable in the control group. | 4/10 |
| A. Louw et al. (2016) [15] | TRC LOE: II | n = 62 Females = 35 Males = 27 Age (years) > 18 (average 60.1) Mean age: 60.1 DDS> 6 months (mean 9.26 years) | Experimental group n = 33 Manual therapy techniques, Mulligan mobilizations Pain education, explanation of the mechanisms of neuroplasticity Control group n = 29 Manual therapy techniques, Mulligan mobilizations, explanation of the biomechanics of the lumbar spine NT: One session of 15 min (10 min of manual treatment + 5 min of explanation) | PAIN: NRS | Baseline Post intervention | PAIN: Neither group (experimental nor control) showed significant improvements on the NRS after the respective treatment sessions (Interaction effect p = 0.325) Experimental group: 3.8 ± 2.1 pre-treatment; 3.0 ± 2.4 post treatment. Control group: 4.3 ± 2.4 pre-treatment; 4.0 ± 2.5 post treatment. | 6/10 |
| M. O‘Keeffe et al., (2019) [16] | TRC LOE: II | n = 206 ODI score > 14% Age (years): 18–75 DDS ≥ 6 months | Experimental group n = 106 CFT, giving meaning to pain, pain control exposure, lifestyle change Control group n = 100 Exercise, education and relaxation NT: Experimental group = variable, on average five treatments in 6–8 weeks Control group = Six sessions in 6–8 weeks | PAIN: NRS DISABILITY: ODI | Baseline 6 months 12 months | PAIN: No obvious differences between groups were observed in pain intensity either at 6 months (mean difference: 0.76, −0.02 to 1.54; p = 0.056) or at 12 months (mean difference: 0.65, −0.20 to 1.50; p = 0.134). DISABILITY: the experimental group showed a more evident reduction in disability than the control group at 6 months (mean difference: 8.65, from 3.66 to 13.64; p = 0.001) and at 12 months (mean difference: 7.02, from 2.24 to 11.80; p = 0.004). | 6/10 |
| MJ Petrozzi et al. (2019) [17] | TRC LOE: II | n = 108 Age (years) > 18 average 50.4 ± 13.6 DDS > 3 months | Experimental group n = 54 Physiotherapy (manual therapy, exercise, education) CBT (information on negative emotions, cognitive-behavioral therapy; behavioral approach strategies) via MoodGYM software Control group n = 54 Physiotherapy (manual therapy, exercise, education) NT: Experimental group = mean 7.7 (SD 2.4) Control group = mean 7.7 (SD 2.0) | PAIN: NRS DISABILITY: RDQ | Baseline 8 weeks 6 months 12 months | PAIN: A moderate reduction in pain symptoms is observed for both groups at the end of treatment (8 weeks), although it is not effectively maintained during follow-up. DISABILITY: Significant improvements were observed in both groups at the end of treatment (8 weeks, and then maintained at 6 and 12 months), but without major differences between the two groups (p = 0.70) at each follow-up point. | 7/10 |
| T. Pincus et al. (2015) [18] | TRC LOE: III | n = 89 Males = 35 Females = 54 Age (years): mean 44.6 (SD 16.01) DDS > 3 months | Experimental group n = 45 CBT Control group n = 44 Physiotherapy NT: Eight sessions of 1 h | PAIN: BPI, CPAQ DISABILITY: RDQ | Baseline 3 months 6 months | PAIN: The average results on the pain acceptance scales were higher for the experimental group than for the control group (increase of 7.9 versus 5.1). DISABILITY: A change in the disability index at 6 months was greater in the experimental group than in the control group. | 4/10 |
| P. Rabiei, B. Sheikhi, A. Letafatkar (2021) [19] | TRC LOE: II | n = 73 DDS > 3 months | Experimental group n = 37 Neurophysiological education of pain, motor control exercises Control group n = 38 Conventional exercise NT: 16 (Two weekly sessions for 8 weeks) | PAIN: VAS DISABILITY: RDQ | Baseline 8 weeks | Both groups showed significant improvements under the two outcome measures examined, with the experimental group showing more significant improvements than the control group. ACHE: (p = 0.041, ηp2 = 0.06) DISABILITY: (p = 0.021, ηp2 = 0.07) | 6/10 |
| RMA Van Erp et al. (2019) [20] | TRC LOE: II | n = 25 Males = 11 Females = 14 Age (years): 18–62 (mean 44 (SD 12.2) DDS ≥ 12 weeks | Experimental group n = 12 Information on pain mechanisms, behavior and beliefs, coping strategies, goal-setting and self-management strategies, elements of CBT Control group n = 13 Usual treatment for low back pain NT: on average 8 (range 3–12) | PAIN: NRS DISABILITY: QBPD | Baseline Post intervention 3 months | PAIN: There were no significant differences between the two intervention groups at both endpoints. DISABILITY: No significant differences were found between the two groups after the intervention (mean difference 0.10, 95% CI: −12.9 to 13.1) and at follow-up (mean difference −5.4, 95% CI −19.1 to 8.3). | 7/10 |
| J. Semrau et al. (2021) [21] | TRC LOE: I. | n = 351 Age (years): Experimental group mean = 51.24 (SD 7.4) Control group mean = 51 (SD 7.4) DDS> 3 months | Experimental group n = 176 Behavioral exercises according to the BPS approach, coping strategies in relation to movement and low back pain episodes, education, maintenance of physical activity during the follow-up Control group n = 175 Standard exercises, physical activity NT: Experimental group = 15 sessions Control group = 13 sessions | PAIN: NRS DISABILITY: HFAQ | Baseline Post intervention 6 months 12 months | PAIN: There were no significant differences between the two groups on the NRS, either at the end of treatment or at the subsequent follow-up points, although modest improvements were observed in both groups. DISABILITY: There were no significant differences, neither at the end of the treatment sessions, nor at the subsequent follow-up points, with both study groups showing improvements on the HFAQ. | 8/10 |
| KV Fersum et al. (2013) [22] | TRC LOE: II | n = 121 Age (years): 18–65 ODI > 14%, NRS > 2/10 DDS > 3 months | Experimental group n = 62 CFT, functional education, physical activity Control group n = 59 Exercise, joint mobilization, manual therapy, applied to the spine or pelvis NT: Experimental group = 106 h of CB-CFT Control group = at the discretion of the physiotherapist | PAIN: NRS DISABILITY: ODI | Baseline Post-surgery (3 months) 12 months | The experimental group showed more significant improvements in both pain and disability, post-surgery and following the insane up. PAIN: The experimental group improved on average by 3.2 points on the NRS, and the control group by 1.5 points. DISABILITY: At 12 months, the experimental group showed an average improvement of 13.7 percentage points on the ODI scale, while the control group showed an improvement of 5.5%. | 5/10 |
| P. Wälti et al. (2015) [23] | TRC LOE: I. | n = 28 Males = 13 Females = 15 Age (years): 18–60 average 41.5 (Ds 10.6) DDS ≥ 3 months | Experimental group n = 14 Pain neurophysiology education, motor sense training for the trunk, trunk control exercises, home training during follow-up Control group n = 14 Conventional physiotherapy, functional education, home training during follow-up NT: One or two sessions per week, for 8 weeks (maximum 16 sessions) | PAIN: NRS DISABILITY: RDQ | Baseline 12 weeks | PAIN: A reduction in pain intensity was recorded both in the experimental group 2.14 (1.0 to 3.5) and in the control group (0.69, −2.0 to 2.5), with a moderate difference in favor of the experimental group DISABILITY: The reduction in the disability index, found in both groups, does not reveal significant differences in favor of one or the other. (Experimental group: 6.71, 4.2–9.3 Control group: 4.69, 1.9–7.4) | 8/10 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferlito, R.; Blatti, C.; Lucenti, L.; Boscarino, U.; Sapienza, M.; Pavone, V.; Testa, G. Pain Education in the Management of Patients with Chronic Low Back Pain: A Systematic Review. J. Funct. Morphol. Kinesiol. 2022, 7, 74. https://doi.org/10.3390/jfmk7040074
Ferlito R, Blatti C, Lucenti L, Boscarino U, Sapienza M, Pavone V, Testa G. Pain Education in the Management of Patients with Chronic Low Back Pain: A Systematic Review. Journal of Functional Morphology and Kinesiology. 2022; 7(4):74. https://doi.org/10.3390/jfmk7040074
Chicago/Turabian StyleFerlito, Rosario, Chiara Blatti, Ludovico Lucenti, Umberto Boscarino, Marco Sapienza, Vito Pavone, and Gianluca Testa. 2022. "Pain Education in the Management of Patients with Chronic Low Back Pain: A Systematic Review" Journal of Functional Morphology and Kinesiology 7, no. 4: 74. https://doi.org/10.3390/jfmk7040074





