Effectiveness of Physical Therapy in Orthognathic Surgery Patients: A Systematic Review of Randomized Controlled Trials
Abstract
:1. Introduction
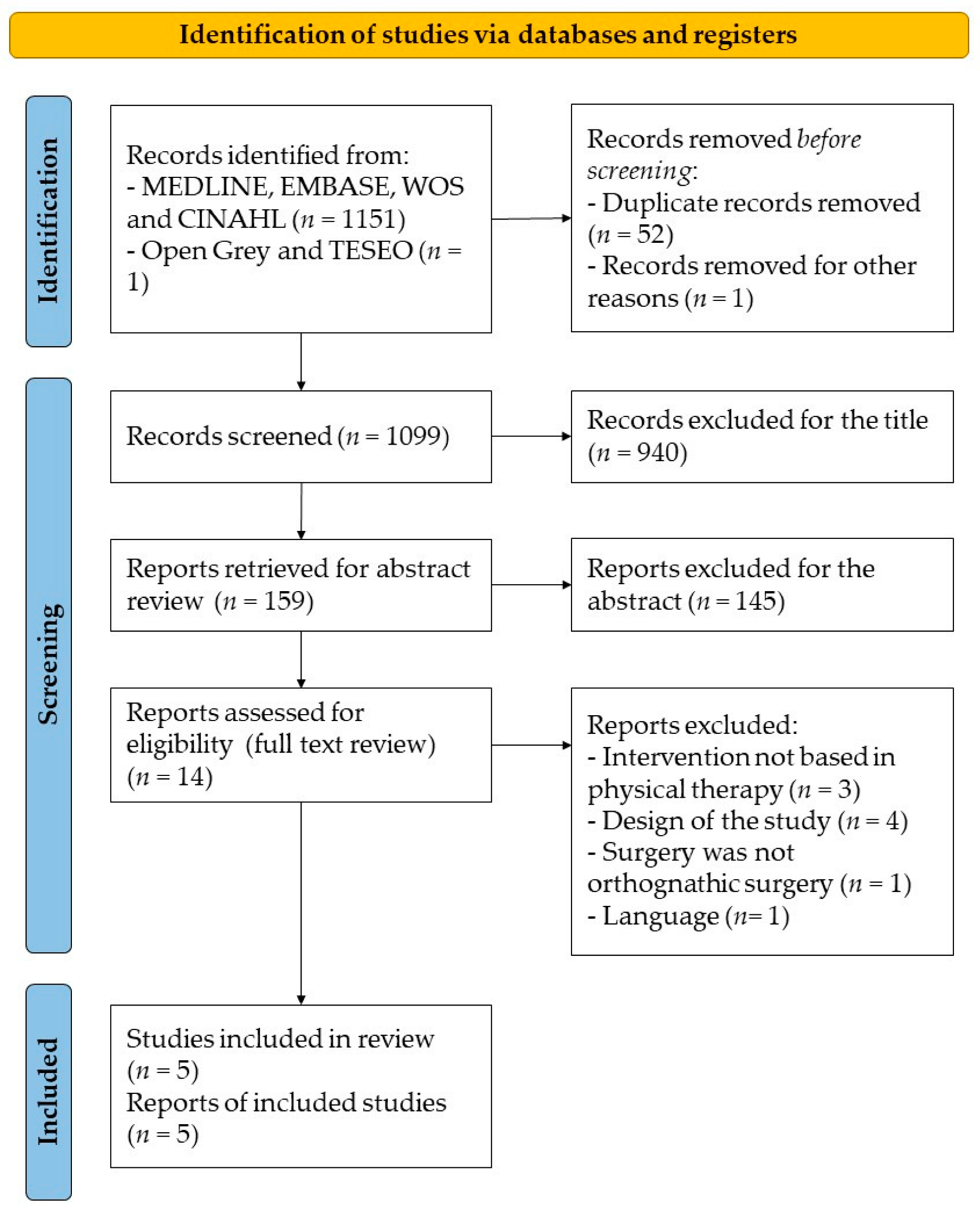
2. Materials and Methods
2.1. Inclusion Criteria
2.2. Search Strategy
2.3. Selection Criteria and Data Extraction
2.4. Methodological Quality Assessment
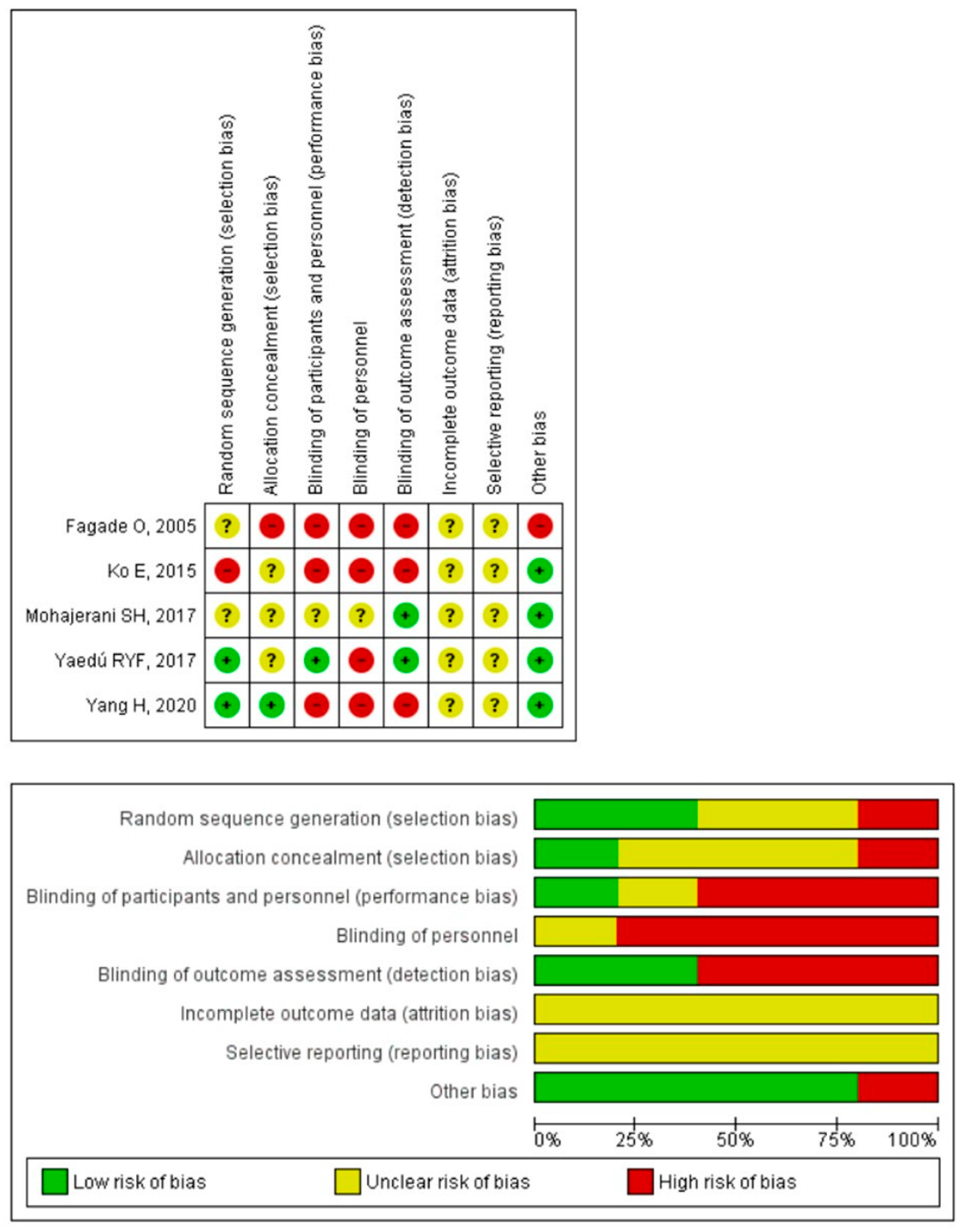
2.5. Risk of Bias Assessment
2.6. Qualitative Analysis
- (1)
- Strong evidence: represents results from multiple RCTs with acceptable methodological quality.
- (2)
- Moderate evidence: represents results from multiple RCTs with low methodological quality, controlled clinical trials or high-quality RCTs.
- (3)
- Limited evidence: represents results from an RCT or low-quality controlled clinical trial.
- (4)
- Conflicting evidence: represents conflicting results from an RCT or controlled clinical trials.
- (5)
- No evidence: there are no RCTs or controlled clinical trials.
3. Results
3.1. Characteristics of the Included Studies
3.1.1. Size and Characteristics of the Sample
3.1.2. Physiotherapy Interventions
3.1.3. Variables of the Clinical Trials
- Neurosensory impairment: evaluated using five tests that assessed the patient’s ability to discriminate external sensory stimuli, using a visual analog scale (VAS) with five levels (one point, total absence of sensation; two points, almost no sensation; three points, reduced sensation; four points, almost normal sensation; five points: completely normal sensation). The five neurosensory tests were divided into three levels depending on their difficulty. The easiest level consisted of discriminating two points using a caliber and directional discrimination of the stimuli applied with a brush. The intermediate level consisted of recognizing the size of the Semmes–Weinstein monofilaments employed. The most difficult level consisted of thermal discrimination performed with ethyl chloride spray and discriminating nociceptive stimuli with a needle compared with a cotton swab [22].
- Pain: measured using the VAS, a 10 cm scale where one end represents the absence of pain and the other represents unbearable pain [23].
- Mouth strength: The measurement was performed using a GM10 occlusal force meter (Nagano Keiki Co.) [17].
- Facial edema: measured with a flexible plastic tape measure employing a procedure based on four separate lines: (1) mandibular angle–external corner of the eye; (2) mandibular angle–internal corner of the eye; (3) mandibular angle–mental protuberance; and (4) mental protuberance–external corner of the eye [23].
3.1.4. Assessment of the Trials’ Methodological Quality
3.2. Risk of Bias
3.3. Qualitative Analysis
3.3.1. Range of Motion
3.3.2. Neurosensory Impairment
3.3.3. Myoelectric Activity of the Masticatory Muscles
3.3.4. Pain
3.3.5. Bite Strength
3.3.6. Facial Edema
4. Discussion
4.1. Range of Motion
4.2. Neurosensory Impairment
4.3. Myoelectric Activity of the Masticatory Muscles
4.4. Pain and Facial Edema
4.5. Clinical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Naran, S.; Steinbacher, D.M.; Taylor, J.A. Current concepts in orthognathic surgery. Plast. Reconstr. Surg. 2018, 141, 925e–936e. [Google Scholar] [CrossRef] [PubMed]
- Sato, F.R.L.; Mannarino, F.S.; Asprino, L.; de Moraes, M. Prevalence and treatment of dentofacial deformities on a multiethnic population: A retrospective study. Oral. Maxillofac. Surg. 2014, 18, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Buchanan, E.P.; Hyman, C.H. LeFort i osteotomy. Semin. Plast. Surg. 2013, 27, 149–154. [Google Scholar]
- Alhammadi, M.S.; Halboub, E.; Fayed, M.S.; Labib, A.; El-Saaidi, C. Global distribution of malocclusion traits: A systematic review. Dent. Press J. Orthod. 2018, 23, 40.e1. [Google Scholar] [CrossRef] [PubMed]
- Ortu, E.; Pietropaoli, D.; Cova, S.; Marci, M.C.; Monaco, A. Efficacy of elastodontic devices in overjet and overbite reduction assessed by computer-aid evaluation. BMC Oral Health 2021, 21, 269. [Google Scholar] [CrossRef] [PubMed]
- Asiri, S.N.; Tadlock, L.P.; Buschang, P.H. The prevalence of clinically meaningful malocclusion among US adults. Orthod. Craniofac. Res. 2019, 22, 321–328. [Google Scholar] [CrossRef]
- Lalloo, R.; Lucchesi, L.R.; Bisignano, C.; Castle, C.D.; Dingels, Z.V.; Fox, J.T.; Hamilton, E.B.; Liu, Z.; Roberts, N.L.S.; Sylte, D.O.; et al. Epidemiology of facial fractures: Incidence, prevalence and years lived with disability estimates from the Global Burden of Disease 2017 study. Inj. Prev. 2020, 26, i27–i35. [Google Scholar] [CrossRef] [Green Version]
- Al-Hiyali, A.; Ayoub, A.; Ju, X.; Almuzian, M.; Al-Anezi, T. The Impact of Orthognathic Surgery on Facial Expressions. J. Oral Maxillofac. Surg. 2015, 73, 2380–2390. [Google Scholar] [CrossRef]
- Agbaje, J.; Luyten, J.; Politis, C. Pain complaints in patients undergoing orthognathic surgery. Pain Res. Manag. 2018, 2018, 4235025. [Google Scholar] [CrossRef]
- Joachim, M.V.; Brosh, Y.; Rivera, C.M.; Troulis, M.J.; AbdelRaziq, M.; Abu El-Naaj, I. Surgical Complications of Orthognathic Surgery. Appl. Sci. 2023, 13, 478. [Google Scholar] [CrossRef]
- Phillips, C.; Essick, G.; Zuniga, J.; Tucker, M.; Blakey, G. Qualitative Descriptors Used by Patients Following Orthognathic Surgery to Portray Altered Sensation. J. Oral Maxillofac. Surg. 2006, 64, 1751–1760. [Google Scholar] [CrossRef] [PubMed]
- Bravo, M.; Kohan, J.B.; Monasterio, M.U. Effectiveness of glucocorticoids in orthognathic surgery: An overview of systematic reviews. Br. J. Oral Maxillofac. Surg. 2022, 60, e231–e245. [Google Scholar] [CrossRef] [PubMed]
- Rana, M.; Gellrich, N.C.; Ghassemi, A.; Gerressen, M.; Riediger, D.; Modabber, A. Three-dimensional evaluation of postoperative swelling after third molar surgery using 2 different cooling therapy methods: A randomized observer-blind prospective study. J. Oral Maxillofac. Surg. 2011, 69, 2092–2098. [Google Scholar] [CrossRef] [PubMed]
- Szolnoky, G.; Szendi-Horváth, K.; Seres, L.; Boda, K.; Kemény, L. Manual lymph drainage efficiently reduces postoperative facial swelling and discomfort after removal of impacted third molars. Lymphology 2007, 40, 138–142. [Google Scholar] [PubMed]
- Alan, H.; Yolcu, Ü.; Koparal, M.; Özgür, C.; Öztürk, S.A.; Malkoç, S. Evaluation of the effects of the low-level laser therapy on swelling, pain, and trismus after removal of impacted lower third molar. Head Face Med. 2016, 12, 25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fagade, O.O.; Oginni, F.O.; Obilade, T.O. Comparative study of the therapeutic effect of a systemic analgesic and transcutaneous electrical nerve stimulation (TENS) on post-IMF trismus and pain in Nigerian patients. Niger. Postgrad. Med. J. 2005, 12, 97–101. [Google Scholar]
- Yang, H.; Kwon, I.; Almansoori, A.; Son, Y.; Kim, B.; Kim, S.-M.; Lee, J.-H. Effects of chewing exerciser on the recovery of masticatory function recovery after orthognathic surgery: A single-center randomized clinical trial, a preliminary study. Medicina 2020, 56, 483. [Google Scholar] [CrossRef] [PubMed]
- PRISMA-P Group; Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [Green Version]
- de Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef] [Green Version]
- Furlan, A.D.; Chou, R.; Harbin, S.; Pardo, J.P. The 22nd Anniversary of the Cochrane Back and Neck Group. Spine 2020, 45, E1249–E1255. [Google Scholar] [CrossRef] [PubMed]
- Ko, E.W.C.; Teng, T.T.Y.; Huang, C.S.; Chen, Y.R. The effect of early physiotherapy on the recovery of mandibular function after orthognathic surgery for class III correction. Part II: Electromyographic activity of masticatory muscles. J. Cranio-Maxillofac. Surg. 2015, 43, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Mohajerani, S.H.; Tabeie, F.; Bemanali, M.; Tabrizi, R. Effect of Low-Level Laser and Light-Emitting Diode on Inferior Alveolar Nerve Recovery after Sagittal Split Osteotomy of the Mandible: A Randomized Clinical Trial Study. J. Craniofacial Surg. 2017, 28, e408–e411. [Google Scholar] [CrossRef] [PubMed]
- Yaedú, R.Y.F.; Mello, M.D.A.B.; Tucunduva, R.A.; da Silveira, J.S.Z.; Takahashi, M.P.M.S.; Valente, A.C.B. Postoperative Orthognathic Surgery Edema Assessment With and Without Manual Lymphatic Drainage. J. Craniofac. Surg. 2017, 28, 1816–1820. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Tulder, M.; Furlan, A.; Bombardier, C.; Bouter, L. Updated Method Guidelines for Systematic Reviews in the Cochrane Collaboration Back Review Group. Spine 2003, 28, 1290–1299. [Google Scholar] [CrossRef] [Green Version]
- Yilmaz, M.; Tarakci, D.; Tarakci, E. Comparison of high-intensity laser therapy and combination of ultrasound treatment and transcutaneous nerve stimulation on cervical pain associated with cervical disc herniation: A randomized trial. Complement. Ther. Med. 2020, 49, 102295. [Google Scholar] [CrossRef]
- Rakel, B.A.; Zimmerman, B.M.; Geasland, K.; Embree, J.; Clark, C.R.; Noiseux, N.O.; Callaghan, J.J.; Herr, K.; Walsh, D.; Sluka, K.A. Transcutaneous electrical nerve stimulation for the control of pain during rehabilitation after total knee arthroplasty: A randomized, blinded, placebo-controlled trial. Pain 2014, 155, 2599–2611. [Google Scholar] [CrossRef] [Green Version]
- Ryan, F.S.; Moles, D.R.; Shute, J.T.; Clarke, A.; Cunningham, S.J. Social anxiety in orthognathic patients. Int. J. Oral Maxillofac. Surg. 2016, 45, 19–25. [Google Scholar] [CrossRef]
- Cho, H.; Lynham, A.J.; Hsu, E. Postoperative interventions to reduce inflammatory complications after third molar surgery: Review of the current evidence. Aust. Dent. J. 2017, 62, 412–419. [Google Scholar] [CrossRef] [Green Version]
- Scott, B.; Butterworth, C.; Lowe, D.; Rogers, S.N. Factors associated with restricted mouth opening and its relationship to health-related quality of life in patients attending a Maxillofacial Oncology clinic. Oral Oncol. 2008, 44, 430–438. [Google Scholar] [CrossRef]
- de Meurechy, N.K.G.; Loos, P.J.; Mommaerts, M.Y. Postoperative Physiotherapy After Open Temporomandibular Joint Surgery: A 3-Step Program. J. Oral Maxillofac. Surg. 2019, 77, 932–950. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, E.; Lobbezoo, F.; Fueki, K.; Naeije, M. Effects of delayed-onset muscle soreness on masticatory function. Eur. J. Oral Sci. 2012, 120, 526–530. [Google Scholar] [CrossRef] [PubMed]
- Gasperini, G.; de Siqueira, I.C.R.; Costa, L.R. Lower-level laser therapy improves neurosensory disorders resulting from bilateral mandibular sagittal split osteotomy: A randomized crossover clinical trial. J. Cranio-Maxillofac. Surg. 2014, 42, e130–e133. [Google Scholar] [CrossRef] [PubMed]
- Hakimiha, N.; Dehghan, M.M.; Manaheji, H.; Zaringhalam, J.; Farzad-Mohajeri, S.; Fekrazad, R.; Moslemi, N. Recovery of inferior alveolar nerve by photobiomodulation therapy using two laser wavelengths: A behavioral and immunological study in rat. J. Photochem. Photobiol. B 2020, 204, 111785. [Google Scholar] [CrossRef]
- Abboud, W.A.; Yarom, N.; Yahalom, R.; Joachim, M.; Reiter, S.; Koren, O.; Elishoov, H. Comparison of two physiotherapy programmes for rehabilitation after temporomandibular joint arthroscopy. Int. J. Oral Maxillofac. Surg. 2018, 47, 755–761. [Google Scholar] [CrossRef]
- van de Velde, F.E.G.; Ortega-Castrillon, A.; Thierens, L.A.M.; Claes, P.; de Pauw, G.A.M. The effect of manual lymphatic drainage on patient recovery after orthognathic surgery-A qualitative and 3-dimensional facial analysis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2020, 130, 478–485. [Google Scholar] [CrossRef]
- Mancini, F.; Beaumont, A.L.; Hu, L.; Haggard, P.; Iannetti, G.D.D. Touch inhibits subcortical and cortical nociceptive responses. Pain 2015, 156, 1936–1944. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jang, H.J.; Kim, M.H. Effects of Active Mandibular Exercise for Mouth Opening Limitation Patients after Maxillomandibular Fixation Release: A Non-Randomized Controlled Trial. J. Korean Acad. Nurs. 2018, 48, 26–37. [Google Scholar] [CrossRef]
| PEDro Scale Items | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fagade et al., 2005 [16] | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
| Ko et al., 2015 [21] | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 3 |
| Mohajerani et al., 2017 [22] | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 7 |
| Yang et al., 2020 [17] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 5 |
| Yaedú et al., 2017 [23] | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 6 |
| Demographic Data | IG | CG | Key Outcomes | Assessment | Conclusions | |
|---|---|---|---|---|---|---|
| Fagade et al., 2005 [16] PEDro: 5 | G1 (n = 10), M: 6, F: 4, 34.5 ± 10.37 years on average G2 (n = 10), M: 4, F: 6, 36.2 ± 14.27 years on average | G1: TENS G2: paracetamol | There was no control group | MMO | A caliper was used to measure interincisal distance | G1: SSI in MMO Paracetamol: SSI in MMO G1 vs. G2: without statistically significant differences. |
| Ko et al., 2015 [21] PEDro: 3 | IG (n = 31), M: 9, F: 22, 24 ± 3.6 years on average CG (n = 32), M: 8, F: 24, 25.3 ± 4.8 years on average | Diet and PT program | Diet | Myoelectric activity of masticatory muscles | Surface EMG (Zebris EMG 4, Zebris gmbH, Isny im Allgäu, Germany) and software for analyzing myoelectric signal (WinJaw 10.5 Zebris GmbH, Isny im Allgäu, Germany) | IG vs. CG: SSI in favor of IG in myoelectrical activity recovery of masticatory muscles |
| Mohajerani et al., 2017 [22] PEDro: 7 | IG (n = 10), M: 5, F: 5, 24.1 ± 4.6 years on average CG (n = 10), M: 3, F: 7, 22.8 ± 3.6 years on average | LIL + LED | LED | Neurosensory Recovery | It was assessed by using a clinical neurosensory test including brush stroke allodynia, 2-point discrimination, contact detection, pinprick nociception and thermal discrimination. In addition, neurosensory recovery was subjectively measured using a VAS scale | IG: SSI in VAS score, brush stroke allodynia and 2-point discrimination IG vs. CG: SSI in favor of IG in neurosensory recovery of subjects. SSI in favor of IG in VAS score, brush stroke allodynia in 6-month follow up and in 2-point discrimination in the 2-month follow up. |
| Yang et al., 2020 [17] PEDro: 5 | IG (n = 12), M: 7, F:5, 22.3 ± 4.3 years on average CG (n = 10), M: 5, F:5, 21.9 ± 2.9 years on average | Standard PT + therapeutic exercise program. | Standard PT | Bite force, MMO, myoelectric activity | Bite force assessed with a specific device (Occlusal force-meter GM10, Nagano keiki Co., Ltd., Tokyo, Japan) MMO assessed with a ruler (interincisal distance) Myoelectric activity assessed with an electromyograph (BioEMG II Bioresearch Assoc., Milwaukee, WI, USA) | IG: SSI in bite force and MMO CG: SSI in bite force and MMO IG vs. CG: no differences |
| Yaedú et al., 2017 [23] PEDro: 6 | IG (n = 15), M: 12, F: 3, 25.67 ± 6.41 years on average CG (n = 15), M: 12, F: 3, 24.87 ± 3.18 years on average | Manual lymphatic drainage, cryotherapy, medication | Placebo lymphatic drainage, cryotherapy, medication | Edema and patient perception of edema and pain intensity | Edema was assessed with tape and photographs. Patient perception of edema and pain intensity were assessed with a VAS | IG: SSI in edema regression IG vs. CG: no differences |
| RCT | Intervention | Description |
|---|---|---|
| Fagade et al., 2005 [16] | TENS | TENS (100 µs width pulse, 50 Hz frequency) was applied using circular electrodes of 3 cm. The positive electrode was placed in masseter muscle and the negative in zygomatic bone. TENS intensity was adjusted based on the tolerance level of each patient, but without visible muscle contraction. The intervention lasted 30 min. Paracetamol was administrated to the control group. |
| Ko et al., 2015 [21] | Therapeutic Exercise | Therapeutic exercise intervention started on the 8th postsurgical day. During the first three weeks, intervention protocol included active mobility exercises (jaw opening 6 times of 30 s; lateralization 10 times of 5 s; protrusion 10 times of 5 s). After each session, patients were allowed to self-massage masticatory muscles. From the 5th post-surgical week, isometric contraction exercises were included (3 times of 10 s). Control group did not receive exercise intervention. |
| Mohajerani et al., 2017 [22] | LIL + LED | LIL of 810 nm, energy intensity of 5 J/cm2 LED of 632 nm, energy intensity of 2 J/cm2 The intervention was applied in four different locations (mandibular foramen, mandibular body, lips and chin) for 90 s each. The intervention was applied during the 1st, 2nd, 3rd, 7th, 14th, 28th days after the surgery. The control group received only LED. |
| Yang et al., 2020 [17] | Therapeutic Exercise | Therapeutic exercise intervention started on the third postsurgical week. Patients were instructed to use their first and second finger to self-assess opening jaw movement and to do active lateralization movements during 5 to 10 min. In addition, isometric contraction exercises were included using a specific device (NoSick, Hi-Feel World Co., Ltd., Seoul, Korea). Patients were instructed to bite the device 200 times, 3 times a day, with best occlusion possible. Control group did do not the isometric contraction exercises |
| Yaedú et al., 2017 [23] | MLD | MLD was applied over 5 consecutive days, always in the morning, starting on the second postsurgical day. The MLD technique was carried out in a relaxed environment, with the patient laying in supine position, head raised 30° and the physiotherapist conducted the Leduc method with a slight pressure (30–40 mmHg). Control group received placebo MLD, which consisted of superficial lymphatic drainage. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Navarro-Fernández, G.; Gil-Martínez, A.; Diaz-Saez, M.C.; Elizagaray-Garcia, I.; Pili-Mayayo, P.Q.; Ocampo-Vargas, J.E.; Beltran-Alacreu, H. Effectiveness of Physical Therapy in Orthognathic Surgery Patients: A Systematic Review of Randomized Controlled Trials. J. Funct. Morphol. Kinesiol. 2023, 8, 17. https://doi.org/10.3390/jfmk8010017
Navarro-Fernández G, Gil-Martínez A, Diaz-Saez MC, Elizagaray-Garcia I, Pili-Mayayo PQ, Ocampo-Vargas JE, Beltran-Alacreu H. Effectiveness of Physical Therapy in Orthognathic Surgery Patients: A Systematic Review of Randomized Controlled Trials. Journal of Functional Morphology and Kinesiology. 2023; 8(1):17. https://doi.org/10.3390/jfmk8010017
Chicago/Turabian StyleNavarro-Fernández, Gonzalo, Alfonso Gil-Martínez, Marta Carlota Diaz-Saez, Ignacio Elizagaray-Garcia, Paloma Qinling Pili-Mayayo, Julian Esteban Ocampo-Vargas, and Hector Beltran-Alacreu. 2023. "Effectiveness of Physical Therapy in Orthognathic Surgery Patients: A Systematic Review of Randomized Controlled Trials" Journal of Functional Morphology and Kinesiology 8, no. 1: 17. https://doi.org/10.3390/jfmk8010017
APA StyleNavarro-Fernández, G., Gil-Martínez, A., Diaz-Saez, M. C., Elizagaray-Garcia, I., Pili-Mayayo, P. Q., Ocampo-Vargas, J. E., & Beltran-Alacreu, H. (2023). Effectiveness of Physical Therapy in Orthognathic Surgery Patients: A Systematic Review of Randomized Controlled Trials. Journal of Functional Morphology and Kinesiology, 8(1), 17. https://doi.org/10.3390/jfmk8010017