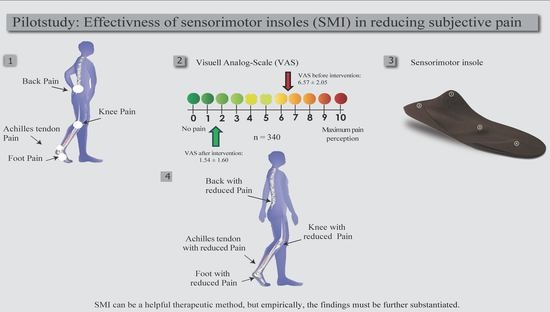
Assessing the Subjective Effectiveness of Sensorimotor Insoles (SMIs) in Reducing Pain: A Descriptive Multicenter Pilot Study
Abstract
:1. Introduction
- Muscle tonus reduction: Lengthening of muscle tendons produces tonus reduction of a muscle [13,19,22]. The application of a pressure point to the tendon lengthens and therefore stretches it. Through the Golgi tendon reflex, a tonus reduction in the inserting muscle occurs as a physiological response. In particular, the toe flexors and the plantar fascia respond to this mechanism.
- Muscle tonus increase: A pressure spot produces a directional force with a shortening effect of muscle tendons, which results in an increase of the muscle tonus [13,19,22]. Approaching the muscle tendon insertion to its origin neurobiologically triggers muscle spindles, and thus initiates sensitively increased muscle activity for an appropriate muscle tonus. The reduced tendon tonus is readjusted by the muscle to the required length. Type 2 afferents may also be responsible for a short-term increase in activity [17]. This mechanism is used for M. peroneus longus [17,18] and M. tibialis posterior to increase their muscle activity and support a foot supination or pronation depending on the overall foot kinematics.
- Indirect mechanical effects: Elements of the insoles can result in a rightening up of a structure. Calcaneus stabilization may have a beneficial effect in the case of excessive internal rotation of the leg by suppressing pronation motion of the subtalar joint [23]. The foot and leg axis and the center of pressure move away from a stimulating element that, as a result, can be used to influence internal or external foot rotation.
2. Materials and Methods
2.1. Patients and Insoles
2.2. Methods
3. Results
4. Discussion
4.1. Future Studies and Strengths of This Study
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Choo, Y.J.; Park, C.H.; Chang, M.C. Rearfoot disorders and conservative treatment: A narrative review. Ann. Palliat. Med. 2020, 9, 3546–3552. [Google Scholar] [CrossRef] [PubMed]
- Besse, J.-L. Metatarsalgia. Orthop. Traumatol. Surg. Res. 2017, 103, S29–S39. [Google Scholar] [CrossRef] [PubMed]
- Almeida, J.S.; Vanderlei, F.M.; Pastre, E.C.; Martins, R.A.; Padovani, C.R.; Filho, G.C. Comparison of Two Types of Insoles on Musculoskeletal Symptoms and Plantar Pressure Distribution in a Work Environment: A Randomized Clinical Trial. Clin. Med. Res. 2016, 14, 67–74. [Google Scholar] [CrossRef]
- Domínguez-Morales, M.J.; Luna-Perejón, F.; Miró-Amarante, L.; Hernández-Velázquez, M.; Sevillano-Ramos, J.L. Smart footwear insole for recognition of foot pronation and supination using neural networks. Appl. Sci. 2019, 9, 3970. [Google Scholar] [CrossRef]
- Chuter, V.; Spink, M.; Searle, A.; Ho, A. The effectiveness of shoe insoles for the prevention and treatment of low back pain: A systematic review and meta-analysis of randomised controlled trials. BMC Musculoskelet. Disord. 2014, 15, 140. [Google Scholar] [CrossRef]
- Rodrigues, P.T.; Ferreira, A.F.; Pereira, R.M.; Bonfá, E.; Borba, E.F.; Fuller, R. Effectiveness of medial-wedge insole treatment for valgus knee osteoarthritis. Arthritis Care Res. Off. J. Am. Coll. Rheumatol. 2008, 59, 603–608. [Google Scholar] [CrossRef]
- Bichsel, D.; Liechti, F.D.; Schlapbach, J.M.; Wertli, M.M. Cross-sectional analysis of recommendations for the treatment of hip and knee osteoarthritis in clinical guidelines. Arch. Phys. Med. Rehabil. 2021, 103, 559–569. [Google Scholar] [CrossRef]
- Gelis, A.; Coudeyre, E.; Hudry, C.; Pelissier, J.; Revel, M.; Rannou, F. Is there an evidence-based efficacy for the use of foot orthotics in knee and hip osteoarthritis? Elaboration of French clinical practice guidelines. Jt. Bone Spine 2008, 75, 714–720. [Google Scholar] [CrossRef]
- Magnusson, M.; Enbom, H.; Johansson, R.; Wiklund, J. Significance of pressor input from the human feet in lateral postural control: The effect of hypothermia on galvanically induced body-sway. Acta Oto-Laryngol. 1990, 110, 321–327. [Google Scholar] [CrossRef]
- Nurse, M.A.; Nigg, B.M. The effect of changes in foot sensation on plantar pressure and muscle activity. Clin. Biomech. 2001, 16, 719–727. [Google Scholar] [CrossRef]
- Russo, L.; Di Capua, R.; Arnone, B.; Borrelli, M.; Coppola, R.; Esposito, F.; Padulo, J. Shoes and Insoles: The Influence on Motor Tasks Related to Walking Gait Variability and Stability. Int. J. Environ. Res. Public Health 2020, 17, 4569. [Google Scholar] [CrossRef] [PubMed]
- Strzalkowski, N.D.J.; Peters, R.M.; Inglis, J.T.; Bent, L.R. Cutaneous afferent innervation of the human foot sole: What can we learn from single-unit recordings? J. Neurophysiol. 2018, 120, 1233–1246. [Google Scholar] [CrossRef] [PubMed]
- Greitemann, B.; Franzen, M.; Stinus, H.; Walther, M.; Dierolf, W.; Schievink, F.; Perick, H.; Stief, T.; Stumpf, J. DGOOC-Beratungsausschuss Orthopädieschuhtechnik. Orthop. Unf.-Mitt. Nachr. 2016, 5, 283–286. [Google Scholar] [CrossRef]
- Jahrling, L.; Rockenfeller, B. Sensomotorische Einlagenversorgung: Aktio gleich Reaktio. Orthop. Sonderh. Sensomotorik 2006, 2006, 50–55. [Google Scholar]
- Müller-Gliemann, C.; Drerup, B.; Osada, N.; Wetz, H. Der Einfluss neurologischer Einlagen nach Bourdiol auf die Rumpfhaltung. Der. Orthop. 2006, 35, 1131–1136. [Google Scholar] [CrossRef]
- Hatton, A.L.; Rome, K.; Dixon, J.; Martin, D.J.; McKeon, P.O. Footwear interventions: A review of their sensorimotor and mechanical effects on balance performance and gait in older adults. J. Am. Podiatr. Med. Assoc. 2013, 103, 516–533. [Google Scholar] [CrossRef]
- Ludwig, O.; Quadlieg, R.; Koch, M. Einfluss einer sensomotorischen Einlage auf die Aktivität des M. peroneus longus in der Standphase. Ger. J. Sport. Med. Dtsch. Z. Fur Sportmed. 2013, 64, 77–82. [Google Scholar] [CrossRef]
- Ludwig, O.; Kelm, J.; Fröhlich, M. The influence of insoles with a peroneal pressure point on the electromyographic activity of tibialis anterior and peroneus longus during gait. J. Foot Ankle Res. 2016, 9, 33. [Google Scholar] [CrossRef]
- Bernius, P. Sensomotorische Einlagenversorgung–was ist daran neu, was ist alt bekannt? Fuß Sprunggelenk 2010, 8, 16–27. [Google Scholar] [CrossRef]
- Klein, T.; Lastovicka, O.; Janura, M.; Svoboda, Z.; Chapman, G.J.; Richards, J. The immediate effects of sensorimotor foot orthoses on foot kinematics in healthy adults. Gait Posture 2021, 84, 93–101. [Google Scholar] [CrossRef]
- Hafkemeyer, U.; Poppenborg, D.; Drerup, B.; Möller, M.; Wetz, H. Improvements of gait in paraplegic patients using proprioceptive insoles. Gait Posture 2002, 16, 157–158. [Google Scholar]
- Ranker, A. Sensomotorische Schuheinlagen–Wirkprinzipien und Evidenz. Manuelletherapie 2020, 24, 168–172. [Google Scholar] [CrossRef]
- Mabuchi, A.; Kitoh, H.; Inoue, M.; Hayashi, M.; Ishiguro, N.; Suzuki, N. The biomechanical effect of the sensomotor insole on a pediatric intoeing gait. Int. Sch. Res. Not. 2012, 2012, 396718. [Google Scholar] [CrossRef] [PubMed]
- Hatton, A.L.; Dixon, J.; Rome, K.; Newton, J.L.; Martin, D.J. Altering gait by way of stimulation of the plantar surface of the foot: The immediate effect of wearing textured insoles in older fallers. J. Foot Ankle Res. 2012, 5, 11. [Google Scholar] [CrossRef]
- McKeon, P.O.; Ingersoll, C.D.; Kerrigan, D.C.; Saliba, E.; Bennett, B.C.; Hertel, J. Balance training improves function and postural control in those with chronic ankle instability. Med. Sci. Sport. Exerc. 2008, 40, 1810–1819. [Google Scholar] [CrossRef]
- Schmitt, A.P.-L.; Liebau, K.-H.; Hamm, A.; Hacke, C.; Mittelmeier, W.; Schulze, C. Comparison of the Influence of Supportive and Sensorimotor Insoles in the Muscle Activity of Tibialis anterior and Peroneus longus in Combat Boots. Foot 2022, 52, 101910. [Google Scholar] [CrossRef]
- Klauser, H. Der Gebrauch sensomotorischer Aktiveinlagen in der modernen Fußchirurgie. Orthop. Med. Tech. 2007, 4, 8–11. [Google Scholar]
- Dankerl, P.; Keller, A.K.; Häberle, L.; Stumptner, T.; Pfaff, G.; Uder, M.; Forst, R. Effects on posture by different neuromuscular afferent stimulations and proprioceptive insoles: Rasterstereographic evaluation. Prosthet. Orthot. Int. 2016, 40, 369–376. [Google Scholar] [CrossRef]
- Ferreira, L.A.B.; Galli, M.; Lazzari, R.D.; Dumont, A.J.L.; Cimolin, V.; Oliveira, C.S. Stabilometric analysis of the effect of postural insoles on static balance in patients with hemiparesis: A randomized, controlled, clinical trial. J. Bodyw. Mov. Ther. 2017, 21, 290–296. [Google Scholar] [CrossRef]
- Wegener, C.; Wegener, K.; Smith, R.; Schott, K.-H.; Burns, J. Biomechanical effects of sensorimotor orthoses in adults with Charcot–Marie–Tooth disease. Prosthet. Orthot. Int. 2016, 40, 436–446. [Google Scholar] [CrossRef]
- Bijur, P.E.; Silver, W.; Gallagher, E.J. Reliability of the visual analog scale for measurement of acute pain. Acad. Emerg. Med. 2001, 8, 1153–1157. [Google Scholar] [CrossRef] [PubMed]
- Waskom, M.L. Seaborn: Statistical data visualization. J. Open Source Softw. 2021, 6, 3021. [Google Scholar] [CrossRef]
- Ferreira, L.A.B.; Cimolin, V.; Neto, H.P.; Grecco, L.A.C.; Lazzari, R.D.; Dumont, A.J.L.; Galli, M.; Oliveira, C.S. Effect of postural insoles on gait pattern in individuals with hemiparesis: A randomized controlled clinical trial. J. Bodyw. Mov. Ther. 2018, 22, 792–797. [Google Scholar] [CrossRef]
- de Oliveira, H.A.V.; Natour, J.; Vassalli, M.; Rosenfeld, A.; Jennings, F.; Jones, A. Effectiveness of customized insoles in patients with Morton’s neuroma: A randomized, controlled, double-blind clinical trial. Clin. Rehabil. 2019, 33, 1898–1907. [Google Scholar] [CrossRef] [PubMed]
- Skou, S.T.; Hojgaard, L.; Simonsen, O.H. Customized foot insoles have a positive effect on pain, function, and quality of life in patients with medial knee osteoarthritis. J. Am. Podiatr. Med. Assoc. 2013, 103, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Levine, D.; Richards, J.; Whittle, M.W. Gait Analysis, 5th ed.; Elsevier Health Sience: Amsterdam, The Netherlands; Churchill Livingstone: London, UK, 2012. [Google Scholar]
- Perry, J.; Burnfield, J.M. Gait Analysis: Normal and Pathological Function, 2nd ed.; SLACK Incorporated: Thorofare, NJ, USA, 2010. [Google Scholar]
- Ohlendorf, D.; Natrup, J.; Niklas, A.; Kopp, S. Veränderung der Körperhaltung durch haltungsverbessernde, sensomotorische, Einlegesohlen. Man. Med. 2008, 46, 93–98. [Google Scholar] [CrossRef]
- Valenti, F. Use of in-soles to enchance postural con-trol. Proc. Socrat. Lect. 2022, 7, 17–21. [Google Scholar]
- Lipsitz, L.A.; Lough, M.; Niemi, J.; Travison, T.; Howlett, H.; Manor, B. A shoe insole delivering subsensory vibratory noise improves balance and gait in healthy elderly people. Arch. Phys. Med. Rehabil. 2015, 96, 432–439. [Google Scholar] [CrossRef]
- Strzalkowski, N.D.; Mildren, R.L.; Bent, L.R. Thresholds of cutaneous afferents related to perceptual threshold across the human foot sole. J. Neurophysiol. 2015, 114, 2144–2151. [Google Scholar] [CrossRef]
- Almeida, J.S.; Carvalho Filho, G.; Pastre, C.M.; Padovani, C.R.; Martins, R.A. Comparison of plantar pressure and musculoskeletal symptoms with the use of custom and prefabricated insoles in the work environment. Braz. J. Phys. Ther. 2009, 13, 542–548. [Google Scholar] [CrossRef]
- Duval, K.; Lam, T.; Sanderson, D. The mechanical relationship between the rearfoot, pelvis and low-back. Gait Posture 2010, 32, 637–640. [Google Scholar] [CrossRef] [PubMed]
- Awatef, M.L.; Ali, F.Z.; Shimaa, T.; Magda, G.S. Effect of Lumbar Hyperlordosis Correction on Craniovertebral Angle in Low Back Pain Patients. Med. J. Cairo Univ. 2020, 88, 2051–2057. [Google Scholar] [CrossRef]
- Cavanagh, P.R.; Rodgers, M.M. The arch index: A useful measure from footprints. J. Biomech. 1987, 20, 547–551. [Google Scholar] [CrossRef]
- Miller, J.E.; Nigg, B.M.; Liu, W.; Stefanyshyn, D.J.; Nurse, M.A. Influence of foot, leg and shoe characteristics on subjective comfort. Foot Ankle Int. 2000, 21, 759–767. [Google Scholar] [CrossRef] [PubMed]
- Mohr, M.; Meyer, C.; Nigg, S.; Nigg, B.M. The relationship between footwear comfort and variability of running kinematics. Footwear Sci. 2017, 9, 45–47. [Google Scholar] [CrossRef]


| Age Groups (Years) | |||||
|---|---|---|---|---|---|
| <20 | 20–29 | 30–39 | 40–49 | >49 | |
| Total (n = 340) | 80 | 32 | 45 | 44 | 139 |
| Male (n = 143) | 39 | 10 | 25 | 19 | 50 |
| Female (n = 197) | 41 | 22 | 20 | 25 | 89 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Becker, S.; Simon, S.; Mühlen, J.; Dindorf, C.; Fröhlich, M. Assessing the Subjective Effectiveness of Sensorimotor Insoles (SMIs) in Reducing Pain: A Descriptive Multicenter Pilot Study. J. Funct. Morphol. Kinesiol. 2023, 8, 66. https://doi.org/10.3390/jfmk8020066
Becker S, Simon S, Mühlen J, Dindorf C, Fröhlich M. Assessing the Subjective Effectiveness of Sensorimotor Insoles (SMIs) in Reducing Pain: A Descriptive Multicenter Pilot Study. Journal of Functional Morphology and Kinesiology. 2023; 8(2):66. https://doi.org/10.3390/jfmk8020066
Chicago/Turabian StyleBecker, Stephan, Steven Simon, Jan Mühlen, Carlo Dindorf, and Michael Fröhlich. 2023. "Assessing the Subjective Effectiveness of Sensorimotor Insoles (SMIs) in Reducing Pain: A Descriptive Multicenter Pilot Study" Journal of Functional Morphology and Kinesiology 8, no. 2: 66. https://doi.org/10.3390/jfmk8020066