An Atypical Presentation of Sympathetic Ophthalmia in an Intact Globe Following Mechanical Fall: A Case Report and Literature Review
Abstract
:1. Introduction
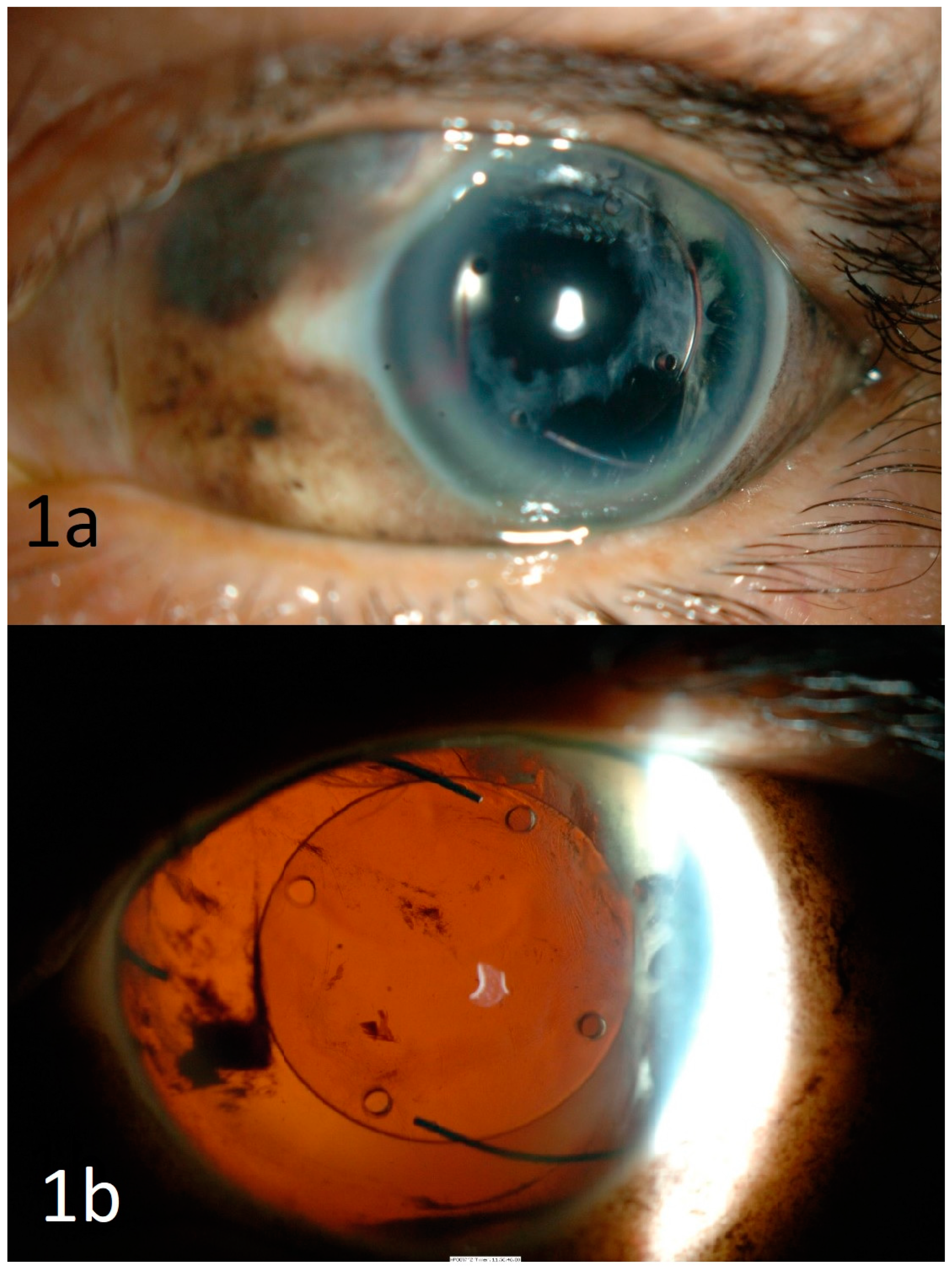
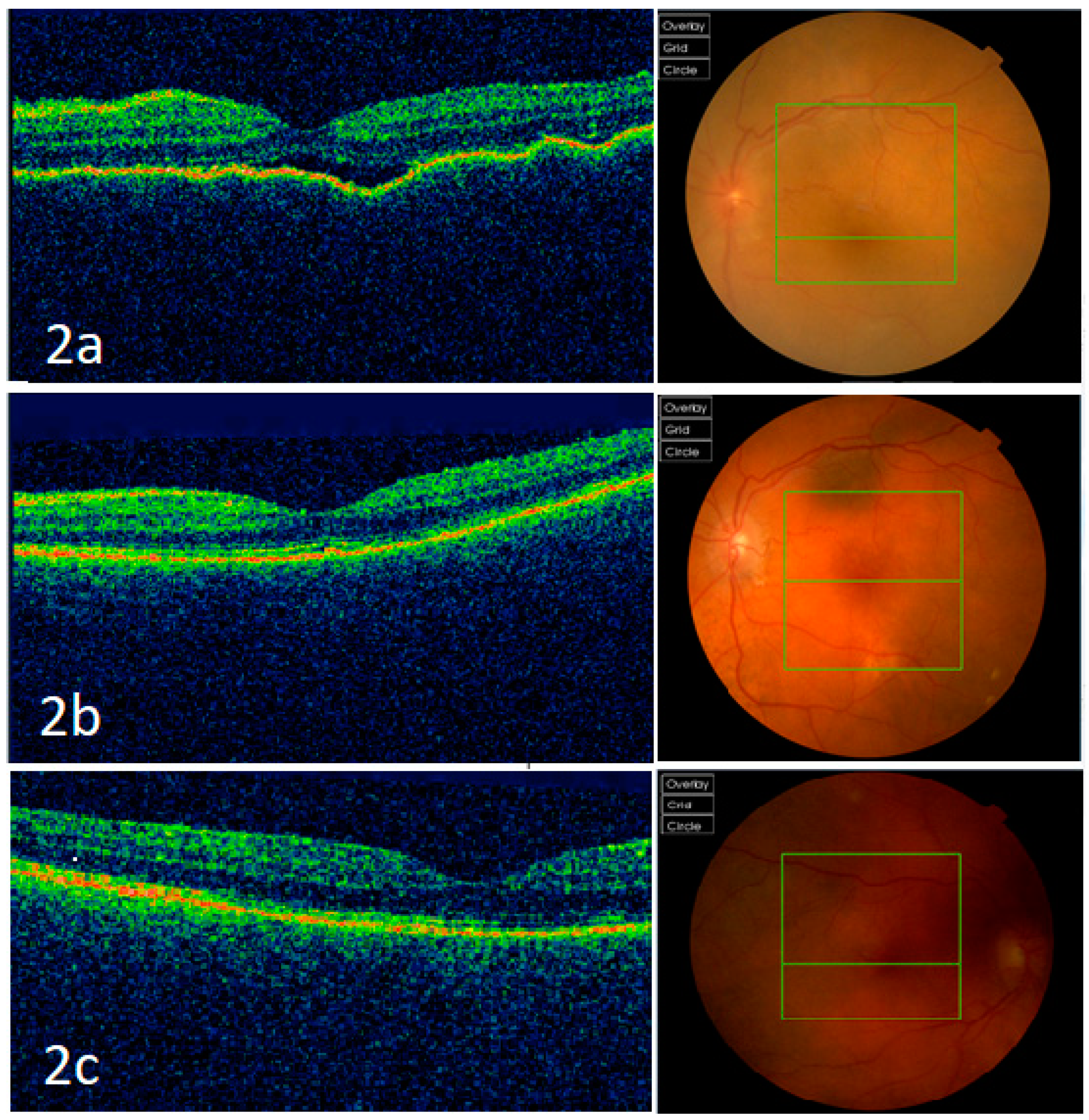
2. Case Report
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kilmartin, D.J. Prospective surveillance of sympathetic ophthalmia in the UK and Republic of Ireland. Br. J. Ophthalmol. 2000, 84, 259–263. [Google Scholar] [CrossRef] [Green Version]
- Shen, J.; Fang, W.; Jin, X.-H.; Yao, Y.-F.; Li, Y.-M. Sympathetic ophthalmia caused by a severe ocular chemical burn: A case report and literature review. Int. J. Clin. Exp. Med. 2015, 8, 2974–2978. [Google Scholar]
- Ahmad, N.; Soong, T.K.; Salvi, S.; Rudle, P.A.; Rennie, I.G. Sympathetic ophthalmia after ruthenium plaque brachytherapy. Br. J. Ophthalmol. 2007, 91, 399–400. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buller, A.J.; Doris, J.P.; Bonshek, R.; Brahma, A.K.; Jones, N.P. Sympathetic ophthalmia following severe fungal keratitis. Eye 2006, 20, 1306–1307. [Google Scholar] [CrossRef] [Green Version]
- Guerriero, S.; Montepara, A.; Ciracì, L.; Monno, R.; Cinquepalmi, V.; Vetrugno, M. A Case of Sympathetic Ophthalmia After a Severe Acanthamoeba Keratitis. Eye Contact Lens Sci. Clin. Pract. 2011, 37, 374–376. [Google Scholar] [CrossRef]
- Abu El-Asrar, A.; Al-Obeidan, S. Sympathetic Ophthalmia after Complicated Cataract Surgery and Intraocular Lens Implantation. Eur. J. Ophthalmol. 2001, 11, 193–196. [Google Scholar] [CrossRef]
- Subudhi, P.; Kanungo, S.; Subudhi, B.N.R. AN ATYPICAL CASE OF SYMPATHETIC OPHTHALMIA AFTER LIMBAL CORNEAL LACERATION. Retin. Cases Brief. Rep. 2017, 11, 141–144. [Google Scholar] [CrossRef] [Green Version]
- Tripathy, K.; Mittal, K.; Chawla, R. Sympathetic ophthalmia following a conjunctival flap procedure for corneal perforation. BMJ Case Rep. 2016, 2016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garcia-Arumi, J.; Gil, M.M.; Palau, M.M.; García, A.S. Sympathetic ophthalmia after surgical resection of iridociliary melanoma. A case report. Graefe’s Arch. Clin. Exp. Ophthalmol. 2006, 244, 1353–1356. [Google Scholar] [CrossRef] [PubMed]
- Jonas, J.; Back, W.; Sauder, G.; Jünemann, U.; Harder, B.; Spandau, U. Sympathetic Ophthalmia in VATER Association Combined with Persisting Hyperplastic Primary Vitreous after Cyclodestructive Procedure. Eur. J. Ophthalmol. 2006, 16, 171–172. [Google Scholar] [CrossRef] [PubMed]
- Lubin, J.R.; Albert, D.M.; Weinstein, M. Sixty-five years of sympathetic ophthalmia. A clinicopathologic review of 105 cases (1913–1978). Ophthalmology 1980, 87, 109–121. [Google Scholar] [CrossRef]
- Castiblanco, C.P.; Adelman, R.A. Sympathetic ophthalmia. Graefe’s Arch. Clin. Exp. Ophthalmol. 2009, 247, 289–302. [Google Scholar] [CrossRef] [PubMed]
- Chu, X.K.; Chan, C.-C. Sympathetic ophthalmia: To the twenty-first century and beyond. J. Ophthalmic Inflamm. Infect. 2013, 3, 49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, A.M.; Shepler, A.M.; Chu, C.T.; Nischal, K.K. Sympathetic ophthalmia presenting 5 days after penetrating injury. Am. J. Ophthalmol. Case Rep. 2020, 19, 100816. [Google Scholar] [CrossRef] [PubMed]
- Zheng, C.; Wu, A.Y. Enucleation versus Evisceration in Ocular Trauma: A Retrospective Review and Study of Current Literature. Orbit 2013, 32, 356–361. [Google Scholar] [CrossRef]
- Bakri, S.J.; Peters, G.B. CASE REPORT Sympathetic Ophthalmia after a Hyphema due to Nonpenetrating Trauma. Ocul. Immunol. Inflamm. 2005, 13, 85–86. [Google Scholar] [CrossRef]
- Khatri, A.; Timalsena, S.; Khatri, B.K.; Kharel, M.; Gautam, S.; Gurung, J.; Kafle, S. A rare entity: Sympathetic ophthalmia presumably after blunt trauma to the phthisical eye and optical coherence tomography angiography metrics to monitor response to treatment. Clin. Case Rep. 2019, 8, 149–154. [Google Scholar] [CrossRef] [Green Version]
- Bechrakis, N.E.; Müller-Stolzenburg, N.W.; Helbig, H.; Foerster, M.H. Sympathetic Ophthalmia Following Laser Cyclocoagulation. Arch. Ophthalmol. 1994, 112, 80–84. [Google Scholar] [CrossRef]
- Im, J.C.; Kang, Y.K.; Park, T.I.; Shin, J.P.; Kim, H.K. Sympathetic Ophthalmia after Ocular Wasp Sting. Korean J. Ophthalmol. 2015, 29, 435–436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, C.-C.; Roberge, F.G.; Whitcup, S.M.; Nussenblatt, R.B. 32 Cases of Sympathetic Ophthalmia. Arch. Ophthalmol. 1995, 113, 597–600. [Google Scholar] [CrossRef]
- Savar, A.; Andreoli, M.T.; Kloek, C.E.; Andreoli, C.M. Enucleation for Open Globe Injury. Am. J. Ophthalmol. 2009, 147, 595–600.e1. [Google Scholar] [CrossRef] [PubMed]
- Bastion, M.-L.C.; Mohamad, M.H. Missed perforation presenting as sympathetic ophthalmia in an adolescent Malay girl. BMJ Case Rep. 2012, 2012. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chean, C.S.; Lim, C.S.; Kumar, P.; Kapoor, B. An Atypical Presentation of Sympathetic Ophthalmia in an Intact Globe Following Mechanical Fall: A Case Report and Literature Review. Vision 2021, 5, 11. https://doi.org/10.3390/vision5010011
Chean CS, Lim CS, Kumar P, Kapoor B. An Atypical Presentation of Sympathetic Ophthalmia in an Intact Globe Following Mechanical Fall: A Case Report and Literature Review. Vision. 2021; 5(1):11. https://doi.org/10.3390/vision5010011
Chicago/Turabian StyleChean, Chung Shen, Christina S. Lim, Periyasamy Kumar, and Bharat Kapoor. 2021. "An Atypical Presentation of Sympathetic Ophthalmia in an Intact Globe Following Mechanical Fall: A Case Report and Literature Review" Vision 5, no. 1: 11. https://doi.org/10.3390/vision5010011
APA StyleChean, C. S., Lim, C. S., Kumar, P., & Kapoor, B. (2021). An Atypical Presentation of Sympathetic Ophthalmia in an Intact Globe Following Mechanical Fall: A Case Report and Literature Review. Vision, 5(1), 11. https://doi.org/10.3390/vision5010011




