Measurement of Neutron Dose Equivalent within and Outside of a LINAC Treatment Vault Using a Neutron Survey Meter
Abstract
:1. Introduction
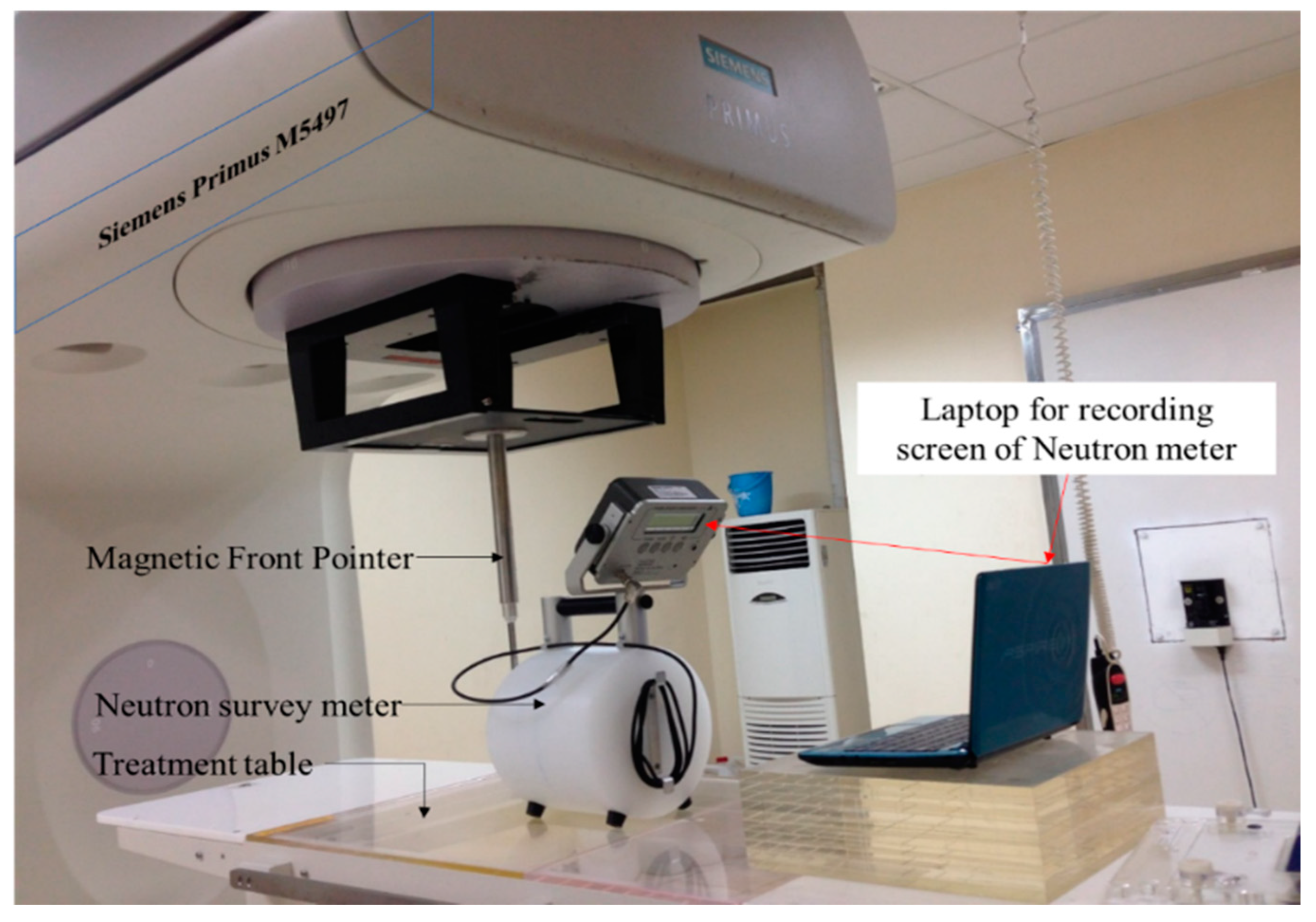
2. Materials and Methods
2.1. Dose Measurement
2.2. Detector
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Pucci, C.; Martinelli, C.; Ciofani, G. Innovative approaches for cancer treatment: Current perspectives and new challenges. Ecancermedicalscience 2019, 13, 961. [Google Scholar] [CrossRef] [PubMed]
- Baskar, R.; Lee, K.A.; Yeo, R.; Yeoh, K.-W. Cancer and Radiation Therapy: Current Advances and Future Directions. Int. J. Med. Sci. 2012, 9, 193–199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gianfaldoni, S.; Gianfaldoni, R.; Wollina, U.; Lotti, J.; Tchernev, G.; Lotti, T. An Overview on Radiotherapy: From Its History to Its Current Applications in Dermatology. Maced. J. Med. Sci. 2017, 5, 521–525. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anderson, I.; Andreani, C.; Carpenter, J.; Festa, G.; Gorini, G.; Loong, C.-K.; Senesi, R. Research opportunities with compact accelerator-driven neutron sources. Phys. Rep. 2016, 654, 1–58. [Google Scholar] [CrossRef] [Green Version]
- Eaton, B.R.; Macdonald, S.M.; Yock, T.I.; Tarbell, N.J. Secondary Malignancy Risk Following Proton Radiation Therapy. Front. Oncol. 2015, 5, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ng, J.; Shuryak, I. Minimizing second cancer risk following radiotherapy: Current perspectives. Cancer Manag. Res. 2015, 7, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Konig, L.; Haering, P.; Lang, C.; Splinter, M.; von Nettelbladt, B.; Weykamp, F.; Hoegen, P.; Lischalk, J.W.; Herfarth, K.; Debus, J.; et al. Secondary Malignancy Risk Following Proton vs. X-ray Treatment of Mediastinal Malignant Lymphoma: A Comparative Modelling Study of Thoracic Organ-Specific Cancer Risk. Front. Oncol. 2020, 10, 989. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, K.E.; Yock, T.I. Radiation Therapy for Pediatric Central Nervous System Tumors. J. Child Neurol. 2009, 24, 1387–1396. [Google Scholar] [CrossRef] [PubMed]
- Hall, E.J. Intensity-modulated radiation therapy, protons, and the risk of second cancers. Int. J. Radiat. Oncol. Biol. Phys. 2006, 65, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Ekendahl, D.; Bečková, V.; Zdychová, V.; Bulánek, B.; Prouza, Z.; Štefánik, M. Accidental neutron dosimetry with human hair. Radiat. Phys. Chem. 2014, 104, 80–83. [Google Scholar] [CrossRef]
- Farhood, B.; Ghorbani, M.; Goushbolagh, N.A.; Najafi, M.; Geraily, G. Different Methods of Measuring Neutron Dose/Fluence Generated During Radiation Therapy with Megavoltage Beams. Health Phys. 2020, 118, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Howell, R.M.; Kry, S.F.; Burgett, E.; Hertel, N.E.; Followill, D.S. Secondary neutron spectra from modern Varian, Siemens, and Elekta linacs with multileaf collimators. Med. Phys. 2009, 36, 4027–4038. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Followill, D.S.; Stovall, M.S.; Kry, S.F.; Ibbott, G.S. Neutron source strength measurements for Varian, Siemens, Elekta, and General Electric linear accelerators. J. Appl. Clin. Med. Phys. 2003, 4, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Naseri, A.; Mesbahi, A. A review on photoneutrons characteristics in radiation therapy with high-energy photon beams. Rep. Prac. Oncol. Radiother. 2010, 15, 138–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peña, J.; Franco, L.; Gómez, F.; Iglesias, A.; Pardo, J.; Pombar, M. Monte Carlo study of Siemens PRIMUS photoneutron production. Phys. Med. Biol. 2005, 50, 5921–5933. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.-P.; Liu, W.-C.; Lin, C.-C. Investigation of photoneutron dose equivalent from high-energy photons in radiotherapy. Appl. Radiat. Isot. 2007, 65, 599–604. [Google Scholar] [CrossRef] [PubMed]
- Schauer, D.; Linton, O.W. National Council on Radiation Protection and Measurements Report Shows Substantial Medical Exposure Increase. Radiology 2009, 253, 293–296. [Google Scholar] [CrossRef] [PubMed]
- Ma, A.; Awotwi-Pratt, J.; Alghamdi, A.; Alfuraih, A.; Spyrou, N.M. Monte Carlo study of photoneutron production in the Varian Clinac 2100C linac. J. Radioanal. Nucl. Chem. 2007, 276, 119–123. [Google Scholar] [CrossRef]
- Barquero, R.; Mendez, R.; Vega-Carrillo, H.R.; Iñiguez, M.P.; Edwards, T.M. Neutron spectra and dosimetric features around an 18 MV linac accelerator. Health Phys. 2005, 88, 48–58. [Google Scholar] [CrossRef] [PubMed]



| Source Surface Distance (SSD, cm) | Point Measurement (x,y,z) | Field Size (cm2) | Neutron Dose Equivalent Rate (mSv/h) |
|---|---|---|---|
| 100 | A (0, 0, 0) | 0 × 0 | 6.31 |
| 10 × 10 | 5.25 | ||
| 20 × 20 | 4.56 | ||
| 100 | A (0, 0, 0) | 10 × 10 | 5.25 |
| B (0, 50, 0) | 5.50 | ||
| C (0, 100, 0) | 5.20 |
| Field Size (cm2) | Point Measurement (x,y,z) | Neutron Dose Equivalent Rate (mSv/h) |
|---|---|---|
| 0 × 0 | D (170,200, 230) | 8.5 |
| E (−170, 200, 230) | 8.6 | |
| F (170, 0, 230) | 8.5 | |
| G (190,460, 230) | 0.0002 | |
| H (650, 460, 230) | 0.0001 | |
| I (850, 460, 230) | 0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tai, D.T.; Loan, T.T.H.; Sulieman, A.; Tamam, N.; Omer, H.; Bradley, D.A. Measurement of Neutron Dose Equivalent within and Outside of a LINAC Treatment Vault Using a Neutron Survey Meter. Quantum Beam Sci. 2021, 5, 33. https://doi.org/10.3390/qubs5040033
Tai DT, Loan TTH, Sulieman A, Tamam N, Omer H, Bradley DA. Measurement of Neutron Dose Equivalent within and Outside of a LINAC Treatment Vault Using a Neutron Survey Meter. Quantum Beam Science. 2021; 5(4):33. https://doi.org/10.3390/qubs5040033
Chicago/Turabian StyleTai, Duong Thanh, Truong Thi Hong Loan, Abdelmoneim Sulieman, Nissren Tamam, Hiba Omer, and David A. Bradley. 2021. "Measurement of Neutron Dose Equivalent within and Outside of a LINAC Treatment Vault Using a Neutron Survey Meter" Quantum Beam Science 5, no. 4: 33. https://doi.org/10.3390/qubs5040033
APA StyleTai, D. T., Loan, T. T. H., Sulieman, A., Tamam, N., Omer, H., & Bradley, D. A. (2021). Measurement of Neutron Dose Equivalent within and Outside of a LINAC Treatment Vault Using a Neutron Survey Meter. Quantum Beam Science, 5(4), 33. https://doi.org/10.3390/qubs5040033