Abstract
During the COVID-19 pandemic, physical activity was significantly decreased in all age groups. The purpose of this study is to investigate children’s motor skills by administering an adapted physical activity program for the development of coordination skills. The sample consisted of 28 children aged 8 to 12 years, 20 neurotypical children and 8 with ASD-HF. Data collection employed various methods, including a personal information form, a leisure time exercise questionnaire, a semi-structured interview, and the Harre Dexterity Circuit for assessing physical activity improvements. The results of the two-way analysis of variance (two-way ANOVA) Tukey HSD test showed the differences between the specific groups, ASD-P vs. ASD-O (p < 0.001), ASD-O vs. AB-O (p < 0.001), ASD-O vs. AB-P (p < 0.001), ASD-O vs. AB-P (p = 0.136), ASD-P vs. AB-P (p < 0.0010, and AB-P vs. AB-O (p = 0.003). As result, both groups showed strong interest in practicing physical activity, and no statistical difference was found in doing so at home or in attendance, showing that physical activity practice is a tool for parent–child bonding and mutual enjoyment, emphasizing that the mixed approach yielded positive results in all participants.
1. Introduction
There is no doubt about the benefits of physical activity for psychophysical well-being [1] and the social involvement of children [2] who are either able-bodied or not. A characteristic of children with autism spectrum disorder is the difficulty in performing age-appropriate motor skills, affecting up to 83% of them [3]. Communication is the first means of relating to the world to ask and give something; in children with ASD-HF, this aspect presents some difficulties [4]. Children with high-functioning ASD (ASD-HF) have difficulty making friends and adapting to environmental changes [5], because they have an incomplete understanding of the communication process and have lower motor skills than their typically developed peers [6]. In recent years, scientific research has been concerned with determining whether motor impairment is a fundamental characteristic of ASD-HF [7] and whether the practice of structured physical activity programs fosters the process of social interaction and communication between the two categories [8]. The research aim is to provide specific workouts to develop game-based [9] exercise protocols that are suitable for all participants, helping them to increase their attention span and supporting them in learning new skills. From this, experimentation of the motor gesture is created, which involves the movement of our limbs and trunk, and the consequent sensations of effort, strength, and heaviness that derive from it [10]. The promotion of physical activity, healthy posture, sports, and active play modalities in preschool and school-age children in family, preschool, school, and local contexts is a necessary and indispensable intervention to promote bodily growth and physical health [11,12,13]. Despite the difficulties that children with ASD-HF may have with the proprioceptive [14] and vestibular systems, the position of the body in space and the statics and dynamics of balance are checked. Sport activities performed regularly not only improve muscle, bone, and cartilage health [15,16,17], also increase social and friendly contact, as being part of a team increases self-esteem and encourages competitive practice. During the COVID-19 emergency [18], people began to engage in less physical activity because of restrictions imposed to limit the spread of the virus, parents themselves also found it difficult to entertain their children, whose motor skills gradually reduced alongside increased sedentary behavior and poor nutrition [19]. On this basis, researchers considered conducting interventions remotely to allow able-bodied children with ASD-HF to practice sports even during the pandemic, as the risks of incurring health problems were considered important [20]. Most children with ASD-HF spend a lot of time partaking in sedentary activities such as using electronic devices. With the administration of remote physical activity, improvements have been seen not only in attention, communication, and social skills [21] but also in self-esteem, as individuals wanted to challenge themselves [22]. The use of technology promoted remote physical activity programs through the Zoom application [23]; the software was used as a communication broker during the COVID-19 pandemic, facilitating communication and supporting learning. The possibility of meeting online while practicing physical activity has made it possible to strengthen one’s character and learn to respect rules and face one’s emotions [24] and frustrations, but also to relate to others, through motor interventions [25]. If the exercises are effective, they generate fun and positive energy for the development of motor skills, whether or not subjects are children who have ASD-HF. Since this is important considering the health promotion of students [26], this study assumes significant importance for the educational community because it places the well-being of children at the center by offering an integrated set of educational, training, and recreational services. Not only does this approach directly benefit the children involved, but it also helps support their families by creating an emotionally and psychologically supportive space within the community through sports activities and learning new motor patterns. Through this study, a culture is promoted that values not only formal education but also the importance of experiential learning and children’s emotional well-being. In addition, the attention given to these children fosters the development of independence and skills, providing them with the tools they need to face future challenges and grow up in a healthy and balanced way. The main purpose of this study is to examine whether the administration of the same motor protocol is effective and applicable both in the presence and at distance [23], to test whether there is an increase in physical activity levels in both groups composed of the same number of participants and characteristics.
2. Materials and Methods
2.1. Participants
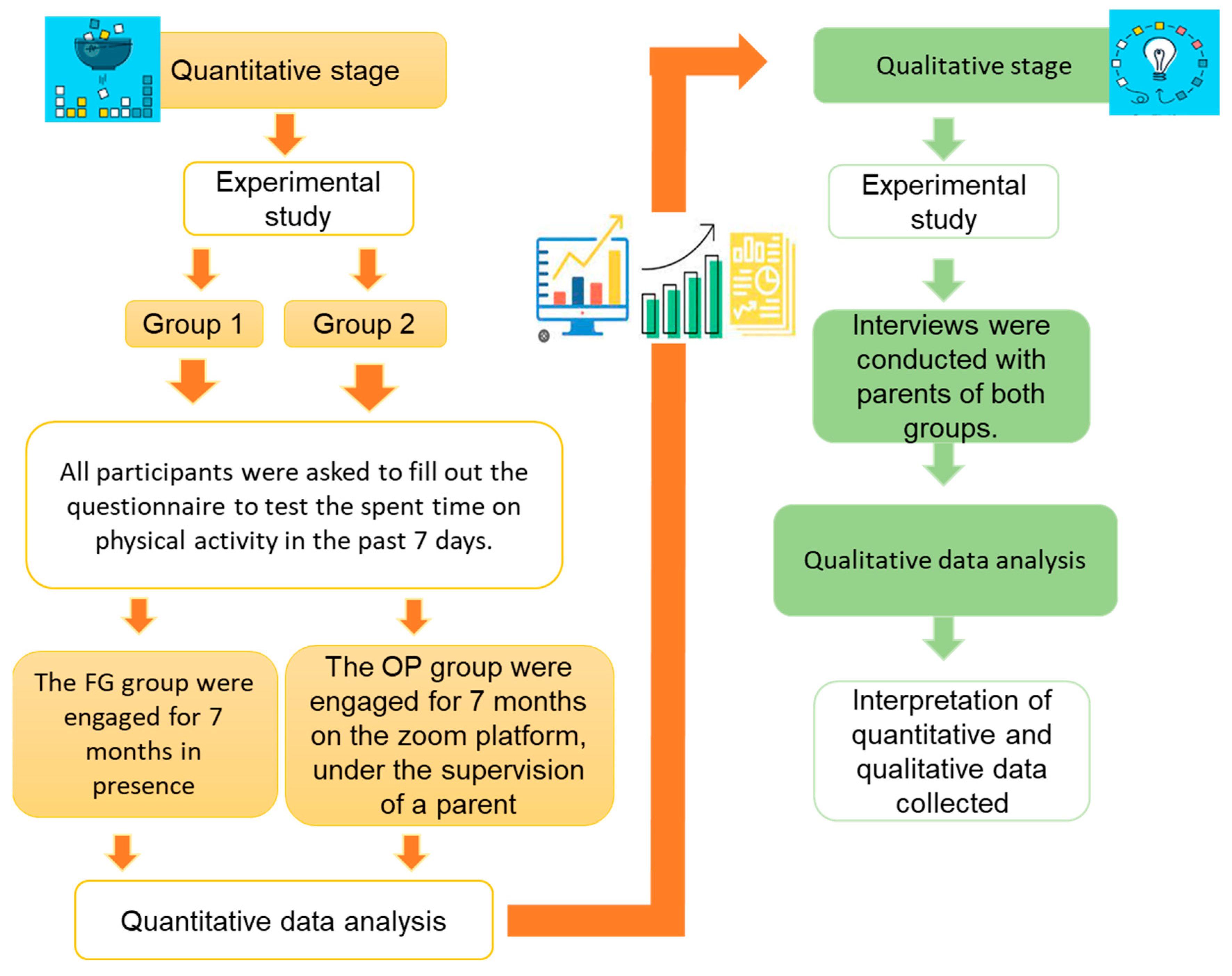
This study was conducted between June 2021 and May 2022, during which adapted physical activity (APA) programs were administered simultaneously online and face-to-face to a group of 28 children aged 8 to 12 years. The face-to-face group consisted of 10 able-bodied (AB-P) children and four ASD-HF children (ASD-P); the online group consisted of 10 able-bodied (AB-O) children and 4 children with ASD-HF (ASD-O). Children with ASD-HF were recruited on medical indication in collaboration with P.O. Gaspare Rodolico, U.O. Pediatric Clinic; movement and cooperation can be considered real therapy. Both groups received the same APA program: the FG group carried out their training at the Research Center on Motor Activities (CRAM) of the University of Catania; the OP group received their training through an online platform with parental supervision. The scientific committee of the Research Center on Motor Activities (CRAM) of the University of Catania approved data collection (Protocol No.: CRAM-011-2020, 16 March 2020), following the Declaration of Helsinki. The methodological design used in the study is that of a randomized controlled experiment, in which participants were randomly assigned to one of two groups (present or online) and received the same APA program, Figure 1. Parents of all participants provided signed informed consent, and the authors assured the parents that the data would be treated confidentially and used only for research purposes. This study used a mixed method based on both qualitative and quantitative tests; the quantitative aspect investigates the study that we wanted to carry out through the administration of the Harre dexterity circuit (HDC) physical test, while the qualitative aspect explores the results collected.
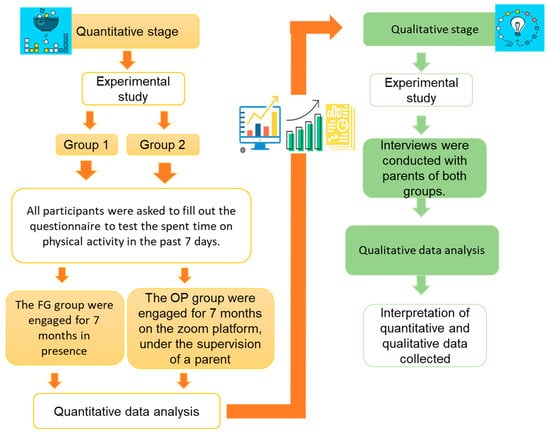
Figure 1.
Qualitative and quantitative strategies.
2.2. Data Analysis
The software R Project version 4.3.3 for Statistical Computing (Vienna, Austria) was used to conduct statistical analysis. The data collected were analyzed with the Shapiro–Wilk test to verify the normality distribution; Levene’s test to verify the homogeneity of the variance; and a two-way analysis of variance (two-way ANOVA) to determine whether any significant differences in the results were present between the two groups, the sub-groups, and each session. The groups were analyzed using the criteria chosen for this research [26]: accepting and voluntarily participating in the study, having a child with ASD-HF or one who is typically developing, and both parents and children who participate in the study should have no health problems; the individual was selected using this criterion. Cohen’s d was used to evaluate the effect size among the groups and the measurements.
2.3. Adapted Physical Activity Program
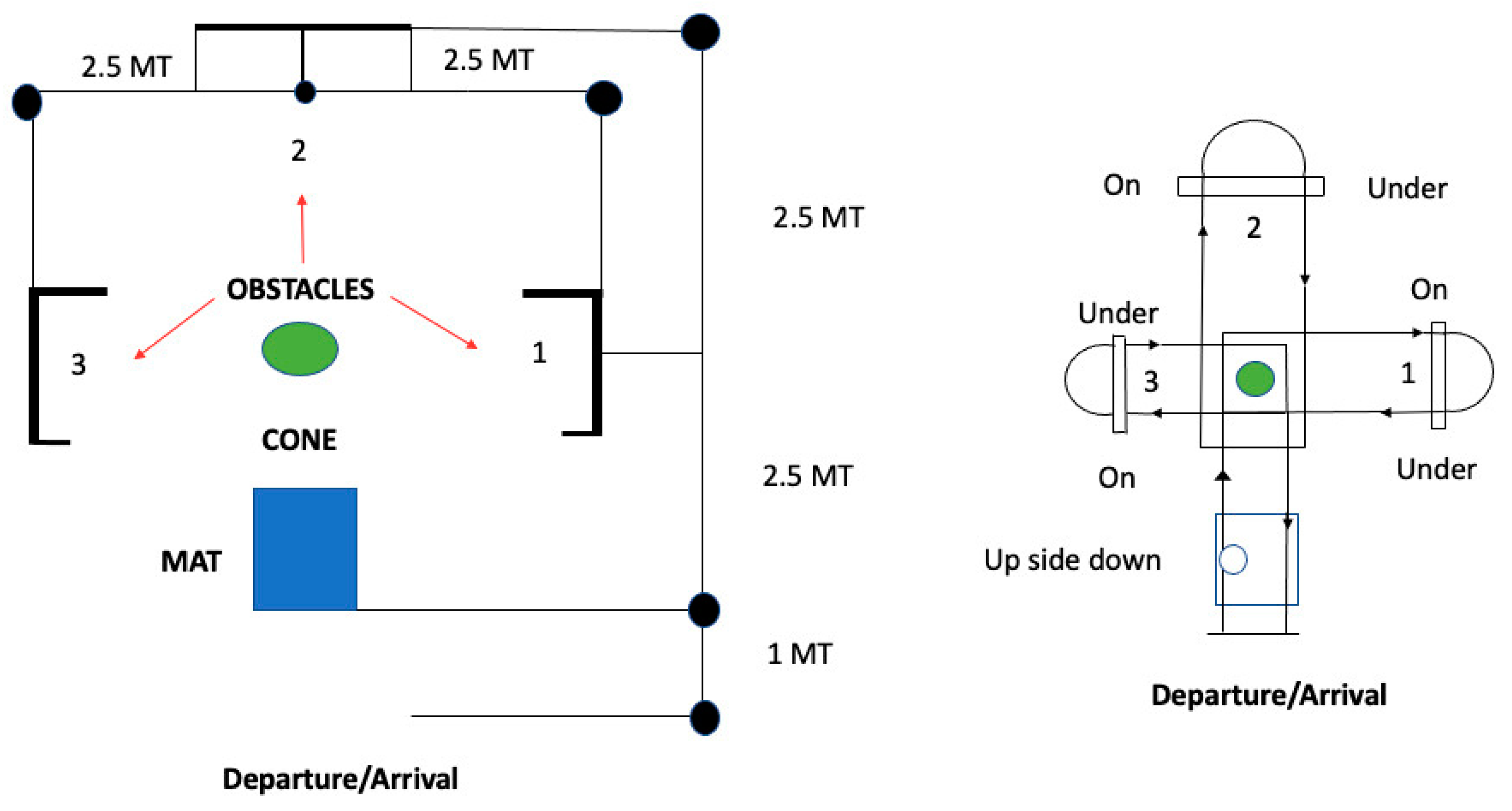
The Harre dexterity circuit (HDC) was used to assess improvements in motor skills following the APA protocol. It was employed to evaluate all general motor skills including balance, rhythm, speed, coordination, and proprioception as well as being a stimulus for socialization towards a path of global psychophysical well-being. Mats, a ball, three 50 cm hurdles, a centesimal stopwatch, and a decameter were used as tools. The Harre dexterity circuit is structured as follows: the subject positions themselves in front of the mat in an upright position, and performs a jump and an upside down; after having turned around, they run towards the center where the ball is and then go towards the first obstacle, pass it, and pass under it, and return to the ball, and the same procedure is repeated for the other two obstacles, up to the finish line (Figure 2). The ball must always be on the right and must not be touched, and the one shoulder stand is performed only at the beginning of the circuit. Participants completed the HDC every 15 days for a total of 14 evaluations. A trained evaluator administered the HDC and recorded the completion time. To ensure consistency across evaluations, a standardized protocol was used, including detailed instructions and a controlled testing environment.
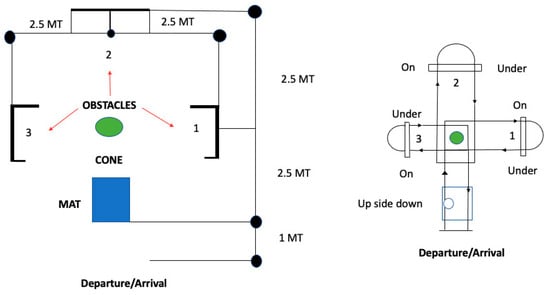
Figure 2.
Harre dexterity circuit.
In Figure 2, we can observe in graphic terms the order in which the circuit is carried out, indicated by numbers from 1 to 3. The leftmost image underlines the length of each straight line to be covered based on the motor gesture to be performed. A large space is required to carry out the course: 6 m long and 5 m wide. In the Figure 2 on the right, it is indicated when is necessary to overcome the obstacle by jumping or by passing underneath. A careful evaluation allows us to have an evolutionary picture of the individuals evaluated in the 7 months of study, through an evaluation scale which presents the following parameters: poor: >20 s; mediocre: 19/20 s; sufficient: 16/14 s; good: 13/11 s; and excellent 10/10. If the highest peak is reached, it will mean that there are no errors and you will execute the circuit correctly, with excellent command over completing the movement to a standing position and an excellent ability to initiate the motor gesture with an early or final jump both forwards and backwards.
2.4. Training Session
The 14 training sessions lasted 90 min each. The face-to-face group (both AB-P and ASD-P) carried out the training in a controlled environment under the supervision of a trainer. The inclusion criteria were age between 8 and 12 years old, an ability to follow simple instructions, and no reported health problems that would prevent participation in physical activity. The exclusion criteria were a history of major surgery in the past 6 months and musculoskeletal disorders that would limit participation. Furthermore, for the ASD-HF participants, we ensured that they had a formal diagnosis of ASD based on the DSM-5, an ability to understand and follow basic verbal and visual instructions related to the study’s physical activities, and sufficient motor skills and behavioral regulation to follow physical activities in a manner manageable by the instructors and with parental support for the online group. The online group (both AB-O and ASD-O) carried out their training sessions remotely through Zoom under the supervision of a trainer and the presence of the parents [27]. The online group was supervised by a parent because, as with school lessons, it is necessary not to leave a child alone in front of a computer, as well as to help them use the device. In addition, in the practice of motor activity, the presence of an adult is essential to avoid domestic accidents. This meeting occasion increased the parent–child relationship because it allowed the improvement of coping skills through play [28], problem-solving and parent–child and child–trainer communication [3]. The design of our APA program adhered to the guidelines and recommendations outlined by the American College of Sports Medicine (ACSM) [29] for individuals with disabilities, including autism spectrum disorder. Each session was programmed with precise steps: (A) 10–15 min of warm-up, (B) 10 min dedicated to reviewing, (C) a 50/60 min assessment of motor improvements, and (D) a 10 min cool-down and stretching. The 10–15 min warm-up consisted of upper and lower limb circles, neck, shoulder, and ankle movements, light jogging, fun games with objects that can also be found at home, and fitness activities [30]. The exercises chosen to improve technique and technical gestures were planks, back extensions, squats, side knee lifts, superman, bridges, chair dips, jumping jacks, burpees, chest openers, the leg-up-the-wall pose, and sit-ups. Aerobic activities such as dance (hip hop), Zumba, and step fitness were also included in the protocol. The last step was the cool-down, which consisted of balancing [31] and breathing activities. Each physical activity session was implemented synchronously through Zoom software version 5.6.6 and in attendance. Exercises were adapted as needed to accommodate the specific needs and abilities of participants with ASD-HF, ensuring safety and inclusivity. Qualified instructors were experienced in providing guidance and supervision for adapted physical activity in accordance with ACSM guidelines on safe, effective exercise programs. By following these principles, we aimed to ensure that our APA protocol was evidence-based, safe, and effective in promoting the physical fitness and well-being of children with and without ASD.
2.5. Measurements
The results of the administration of the APA program were collected with subject personal information forms, questionnaires for leisure time exercises, and semi-structured interviews. Measurements were made every 15 days for a total of 14 evaluations over 7 months of the proposed physical activity protocol carried out on the Zoom platform and face-to-face. The measurements concerning the Harre dexterity circuit were carried out with the use of a chronometer up to one-hundredth of a second. Computer consents and personal forms were used to obtain demographic information (gender, age, weight, height, education level, and other comorbidities) of ASD-HF and typically developing children. The test administered is the International Physical Activity Questionnaire (IPAQ) [32] which explores the time spent in physical activity in the last 7 days, considering recreational activities, work enjoyment, and exercise. Qualitative questions were administered to investigate the feeling of the participants concerning the physical activity protocol. The following questions were included in the interview form: (a) What was your overall impression of the physical activities offered either through Zoom or in person? (b) To what extent did you find the physical activities offered through Zoom or in person helpful about your child’s physical activity? (c) What is your opinion about the usefulness of the physical activities provided through Zoom or in person? This process was conducted through a multidisciplinary approach, involving experts in the fields of physical activity and qualitative research on autism spectrum disorder. Physical activity experts considered factors such as safety, activity adaptability, and physical health goals. Experts on autism addressed the behavioral patterns and specific challenges children face in the typical developmental domain and high-functioning autism. This multidisciplinary approach ensured that the questions were sensitive to the needs and experiences of the interviewed participants.
3. Results
Variation in Physical Activity Levels of Able-Bodied and ASD-HF Children
Among the measurements, the anthropometric data of the participants were also acquired at the Motor Activities Research Center (CRAM) of the University of Catania, where their height and weight were measured with a digital scale and a stadiometer; these two values allow us to calculate the BMI [28] (body mass index) of each subject. The average body weight of each participant was 38.32 kg for an average height of 141.07 cm with an average BMI of 20.36. Harre’s dexterity circuit measurements were made with an ANOVA to see if there were differences between the two groups (“Group 1 (FG)” ASD-O and ASD-P and “Group 2 (OP)” AB-O AND AB-P) by comparing the change in physical activity levels from the start of the protocol to the end (observe Table 1).

Table 1.
Descriptive analysis related to median, mean, and standard deviation.
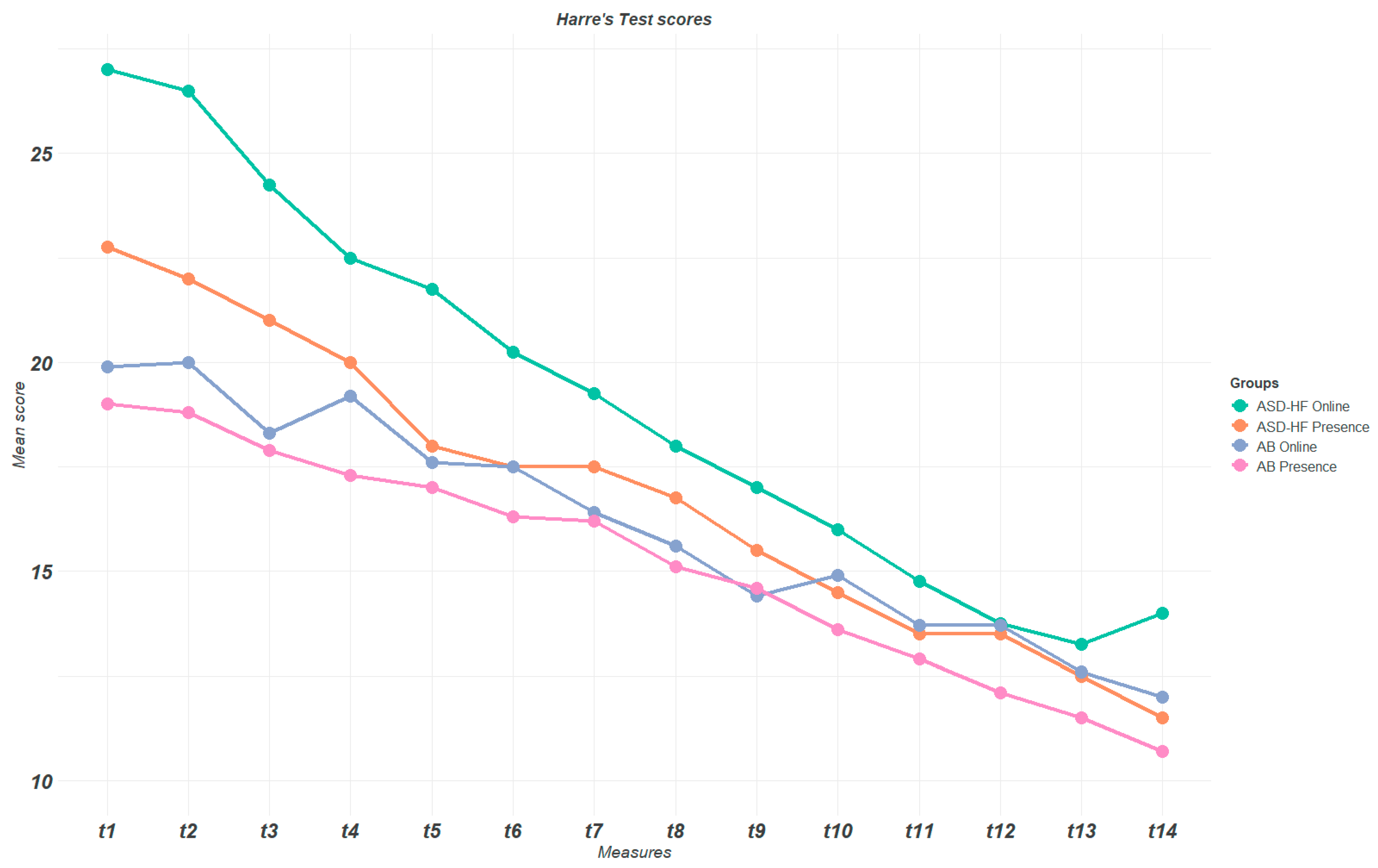
The descriptive analysis of the data related to the median, mean, and standard deviation (SD) is reported in Table 1. The results of the two-way ANOVA show a statistical difference between the groups (p < 0.001) and between each of the measures (p < 0.001), but there was no statistical difference between the combined variables of group and measures (p = 0.144). The Tukey HSD test highlighted the differences between the specific groups, ASD-P vs. ASD-O (p < 0.001), ASD-O vs. AB-O (p < 0.001), ASD-O vs. AB-P (p < 0.001), ASD-O vs. AB-P (p = 0.136), ASD-P vs. AB-P (p < 0.001), and AB-P vs. AB-O (p = 0.003). The following graph highlights the change that occurred during the seven months of study in the 14 sessions, in which the Harre dexterity circuit test on the development of coordination skills was administered, associated with a motor protocol. We observed a valuable effect size among the different conditions as reported in Table 2.

Table 2.
Effect size differences among the groups.
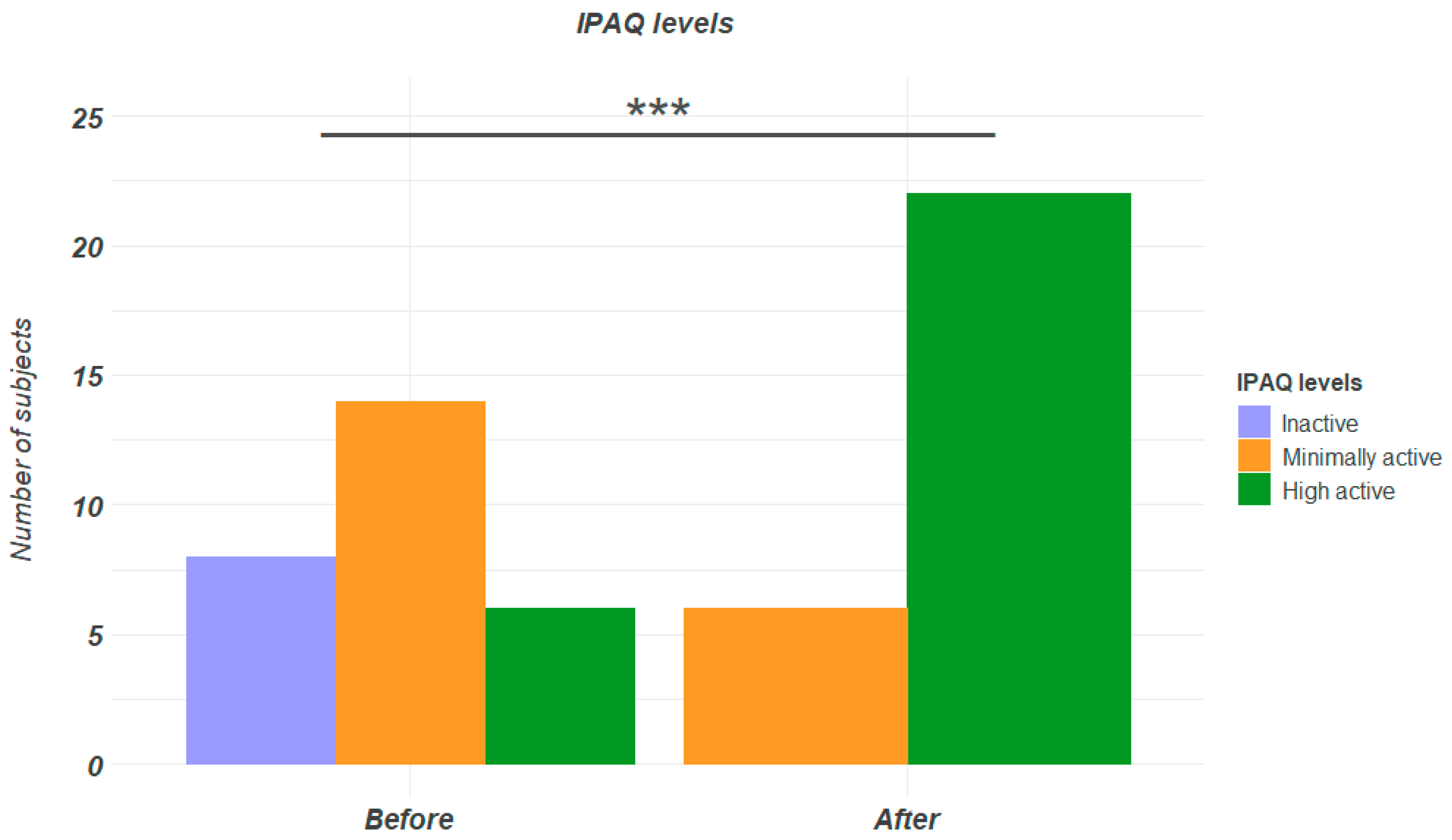
From the following results, Figure 3 it can be seen that the two groups differ from each other; in particular, the FG group obtained better results in the Harre circuit between one session and another, with significant changes. There was no change by type and session between the OP and FG groups, but there was a reduction in their HDC scores; the protocol had the same effect face-to-face as online. In the present study, in addition to completing the informed consent, participants were asked to answer a questionnaire on daily physical activity. The questionnaire was completed 3 days before starting the motor protocol both remotely and face-to-face; the same Google forms were completed at the end of 7 months to assess whether there was an increase in daily physical activity. From the analysis of the score obtained from the closed-response variables, there is a statistical difference between before and after the 7 months of physical activity administered to all groups with p = 0.0002, but there is no difference among the groups (p = 0.848) or both interactions (p = 0.993). Table 3 shows the levels of daily physical activity from which we started; in particular, at the beginning of the administration of the motor protocol, 8 participants were sedentary, 14 were minimally active, and 6 were physically active. Instead, at the end of the 7 months, sedentary lifestyle was reduced by 100%; 6 participants were minimally active, with a decrease of 57.14% compared to the beginning, and the remaining 22 were physically active with an increase of 266.66% of the initial value. If we consider the analyses that were made by administering the IPAQ, all subjects had a positive outcome [32] by increasing their practice of daily physical activity, Figure 4. The following graph shows the IPAQ levels as a function of the number of participants and the increase in physically active subjects.
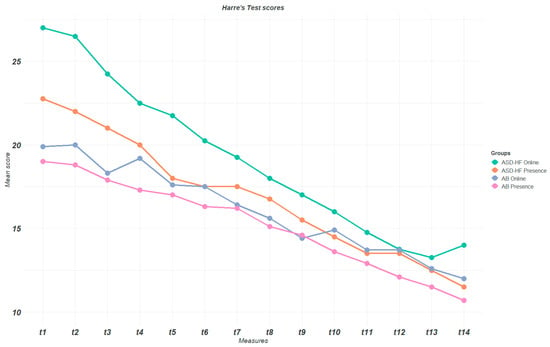
Figure 3.
Harre’s test line chart reporting the mean value of each group per measurement.

Table 3.
Descriptive analysis related to statistical differences before and after the administration of the motor protocol.
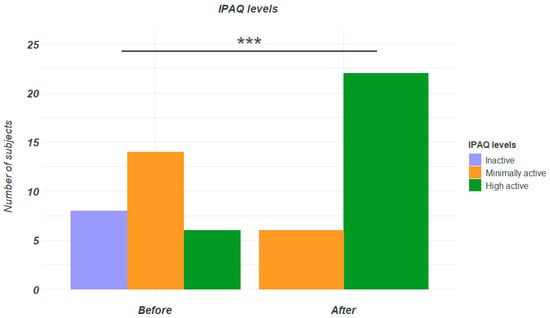
Figure 4.
IPAQ differences: before and after.
4. Discussion
The purpose of the following study was to examine the benefits of administering physical activity during the COVID-19 pandemic, comparing the same motor protocol administered on the Zoom Online Platform [15] with parental supervision too that carried out face-to-face in the year 2021/2022. This study involved 28 families (parent–child) for 7 months, lightening the tension of COVID-19 and avoiding an increase in sedentary lifestyles for those of developmental age and for the entire population [33]. This experience improved the relationship between parents and children, reconnecting through Bowlby’s attachment bond [34], who claims that the relationship with a reference figure, based on secure base theory [35], influences current and future relationships. Attachment research has shown that past and current experiences are important for the development of internal working models. Parents have been seen as a point of reference in daily life as a social modifier of stress [36], and playful experiences unite them with their children. Harre’s dexterity circuit had the purpose of stimulating the subjects to compare the various elements proposed, decoding their differences and similarities, identifying strategies to deal with each situation, but also developing different tools and methods to approach the “space”. With this study, it was understood that is possible to develop the same motor protocol both in face-to-face and online. Coaches must listen to the words and evaluate the behaviors of the children they train during the practice of physical activity [37], always offering them new stimuli and focusing on the child as a person, treating them individually and not as belonging to a single group [38]. The results of the IPAQ on leisure and exercise [32] recorded that there was no significant difference between the physical activity levels of typically developing children and those with ASD-HF performed on Zoom compared to face-to-face activities. Two main themes emerged, as parents’ findings on physical activities provided by Zoom and in person highlighted positive outcomes during the activities performed: (1) the effects of physical activities provided by Zoom and in person on the level of physical activity of children with ASD-HF and those of typical development and (2) the applicability of physical activities provided by Zoom and in person. Parents emphasized that at the start of the pandemic, their children were more sedentary, and then they became more physically active during the administration of the physical activities provided by Zoom and face-to-face. The greatest effect size we observed was between T1 ASD-O vs. AB-O (d = 2.11), followed by T1 ASD-O vs. ASD-P (d = 1.09) and T14 ASD-O vs. ASD-P (d = 1.18). For the AB groups, the effect size was lower than 0.50; namely, there were no valuable differences between online or face-to-face administration of the APA program. The results confirm that for the ASD group, the protocol reported meaningful effects on the examined population. This activity represented a valid strategy to safeguard the emotional well-being, family, and relational well-being of these subjects, who saw meetings as a channel for social relationships with their peers. In our sample, the execution of the motor protocol combined with the possibility of meeting each other, even if virtually, led to a growing desire in the children to improve themselves, with the incentive to overcome their limits; it is plausible to say that there were also experiences of positive motor reinforcement [39], filling some initial gaps. The participants with ASD-HF integrated perfectly with the group and they protected and supported each other, creating a community that aimed to improve all participants [40]. The decision to include both children with typical development and those with high-functioning autism (ASD-HF) was based on an interest in comparing children’s responses and needs related to physical activity practice and well-being. An inclusive approach involving children with and without autism spectrum disorder reflects the importance of considering the different perspectives and experiences within research and practice. This can help to promote a greater awareness and understanding of the needs of all children, regardless of their developmental type. Various studies have been conducted on sustainable physical activity interventions, particularly for children with ASD-HF who cannot access physical activity [41]. The results highlight that the activities conducted through the Zoom platform and face-to-face with the guidelines sent on WhatsApp were useful for the sample analyzed. Although the results have been promising, there are limits to sustainability; the parents had no previous training in physical activity practices, as they only had a supervisory role in the remote activities for ASD-HF and typically developing children [42]. The researchers did not immediately provide feedback to the parents on the improvement that occurred after the evaluation, and it emerged that remote activities generate disadvantages in communication [43], low motivation, and a reduction in interpersonal relationships among the participants [44].
Several trials were given so that the subject could memorize the path and perform the test in the shortest time possible. The data obtained for the activities carried out both in person and online were a mediator against sedentary lifestyles and emotional crises, both for the child and for the parent who saw their child engaged in a playful activity. In the study, targeted strategies were adopted to engage all participants in a meaningful way as they performed the exercises shown in Figure 5, using both verbal and nonverbal communication. It was ensured that no one was left behind, ensuring that both groups were equally represented. The questions formulated during the interview were simple, understandable, and relevant to all children involved, taking into account their specific individual differences. The authors took an ethical and sensitive approach, ensuring informed consent and respecting the needs and rights of all participants, regardless of their background. The research faced certain limitations, including a limited sample size and a lack of exploration into the perceived efficacy of parental mediation training. Subsequent investigations should expand their scope beyond the IPAQ questionnaire, incorporating parental assessments to gauge each participant’s physical activity levels. Moreover, future studies might delve into the emotional experiences of both participants and their parents. Engaging parents in the program alongside their children could provide an avenue for sharing emotions and celebrating achievements together.

Figure 5.
The exercises that compose the Harre Dexterity circuit are shown in sequence, performed by the participants under the supervision of a kinesiologist, who timed the execution and verified the correctness of the motor gestures. (1) The subject performs a forward roll on a mat. (2) The subject continues the forward roll with a roll and then gets up. (3) The subject moves towards the cone and then circles around it. (4) The subject crawls under the obstacle. (5) The subject performs the flight phase, jumping over the obstacle. (6) The subject concludes the flight phase by landing on the floor. The entire sequence is repeated except for the forward roll, which is performed only at the start. The subject will complete the circuit in a clockwise direction, performing the movements at all three obstacles.
5. Conclusions
By administering Harre’s circuit dexterity test (HCT) and a full motor protocol, the children increased their daily physical activity levels, increasing their learning from a motor point of view, but it was also a tool for aggregation, parent–child bonding, and fun. This study underlines that a mixed approach, both in person and online, found positive results in the practice of physical activity in both able-bodied participants and those with ASD-HF. The synergy between parents and trainers was important, which allowed the children to have a good growth path. Parents reported that they were happy to start this journey and that they had fun with their children. Furthermore, it would be essential to create training programs with a unified approach that collaborates with the children. The results obtained seem auspicious, and through its application on a large scale, the primary objective is to expand the sample and deepen this topic. Naturally, the weekly practice of this protocol shared between parents and children helped to increase the relationship between the two units on both a pedagogical and an emotional level.
Author Contributions
Conceptualization, M.Z., F.R. and G.M.; investigation, M.Z. and P.P.; methodology, M.Z., F.R., A.C. and G.M.; resources, M.Z. and G.M.; validation, M.Z., A.C. and G.M.; visualization, M.Z. and G.M.; writing—original draft, M.Z., A.C. and G.M.; writing—review and editing, M.Z., F.R., A.C. and G.M.; project administration, F.R. and P.P.; software, F.R.; supervision, F.R. and G.M. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by the University Research Project Grant (PIACERI Found—NATURE-OA—2020–2022), Department of Biomedical and Biotechnological Sciences (BIOME-TEC), University of Catania, Italy.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the scientific committee of the University of Catania (Protocol No.: CRAM-011-2020, 16 March 2020).
Informed Consent Statement
All subjects signed informed consent forms before participating in the study.
Data Availability Statement
The data are available upon request.
Conflicts of Interest
All authors declare that they have no conflicts of interest to declare, and no financial and personal relationships.
References
- Maugeri, G.; D’agata, V.; Magrì, B.; Roggio, F.; Castorina, A.; Ravalli, S.; Di Rosa, M.; Musumeci, G. Neuroprotective Effects of Physical Activity via the Adaptation of Astrocytes. Cells 2021, 10, 1542. [Google Scholar] [CrossRef] [PubMed]
- Morán, M.L.; Gómez, L.E.; Alcedo, M.; Pedrosa, I. Gender Differences in Social Inclusion of Youth with Autism and Intellectual Disability. J. Autism Dev. Disord. 2019, 49, 2980–2989. [Google Scholar] [CrossRef] [PubMed]
- Brignell, A.; Chenausky, K.V.; Song, H.; Zhu, J.; Suo, C.; Morgan, A.T. Communication interventions for autism spectrum disorder in minimally verbal children. Cochrane Database Syst. Rev. 2018, 11, Cd012324. [Google Scholar] [CrossRef] [PubMed]
- Lai, M.C.; Lombardo, M.V.; Baron-Cohen, S. Autism. Lancet 2014, 383, 896–910. [Google Scholar] [CrossRef]
- Pusponegoro, H.D.; Efar, P.; Soedjatmiko; Soebadi, A.; Firmansyah, A.; Chen, H.-J.; Hung, K.-L. Gross Motor Profile and Its Association with Socialization Skills in Children with Autism Spectrum Disorders. Pediatr. Neonatol. 2016, 57, 501–507. [Google Scholar] [CrossRef] [PubMed]
- Bhat, A.N. Is Motor Impairment in Autism Spectrum Disorder Distinct from Developmental Coordination Disorder? A Report from the SPARK Study. Phys. Ther. 2020, 100, 633–644. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.; Chen, S. The Effects of Structured Physical Activity Program on Social Interaction and Communication for Children with Autism. Biomed. Res. Int. 2018, 2018, 1825046. [Google Scholar] [CrossRef]
- Rinehart, N. Motor stereotypies in children with autism and other developmental disorders. Dev. Med. Child. Neurol. 2009, 51, 2–3. [Google Scholar] [CrossRef]
- Pesce, C.; Masci, I.; Marchetti, R.; Vazou, S.; Sääkslahti, A.; Tomporowski, P.D. Deliberate Play and Preparation Jointly Benefit Motor and Cognitive Development: Mediated and Moderated Effects. Front. Psychol. 2016, 7, 349. [Google Scholar] [CrossRef] [PubMed]
- Proske, U.; Gandevia, S.C. The proprioceptive senses: Their roles in signaling body shape, body position and movement, and muscle force. Physiol. Rev. 2012, 92, 1651–1697. [Google Scholar] [CrossRef]
- Hills, A.P.; Dengel, D.R.; Lubans, D.R. Supporting public health priorities: Recommendations for physical education and physical activity promotion in schools. Prog. Cardiovasc. Dis. 2015, 57, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Trovato, B.; Roggio, F.; Sortino, M.; Zanghì, M.; Petrigna, L.; Giuffrida, R.; Musumeci, G. Postural Evaluation in Young Healthy Adults through a Digital and Reproducible Method. J. Funct. Morphol. Kinesiol. 2022, 7, 98. [Google Scholar] [CrossRef] [PubMed]
- Marsigliante, S.; Gómez-López, M.; Muscella, A. Effects on Children’s Physical and Mental Well-Being of a Physical-Activity-Based School Intervention Program: A Randomized Study. Int. J. Environ. Res. Public Health 2023, 20, 1927. [Google Scholar] [CrossRef] [PubMed]
- Mesa-Fernández, M.; Pérez-Padilla, J.; Nunes, C.; Menéndez, S. Bienestar psicológico en las personas mayores no dependientes y su relación con la autoestima y la autoeficacia. Ciência Saúde Coletiva 2019, 24, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Trovato, B.; Petrigna, L.; Sortino, M.; Roggio, F.; Musumeci, G. The influence of different sports on cartilage adaptations: A systematic review. Heliyon 2023, 9, e14136. [Google Scholar] [CrossRef] [PubMed]
- Malm, C.; Jakobsson, J.; Isaksson, A. Physical Activity and Sports-Real Health Benefits: A Review with Insight into the Public Health of Sweden. Sports 2019, 7, 127. [Google Scholar] [CrossRef] [PubMed]
- Petrigna, L.; Roggio, F.; Trovato, B.; Zanghì, M.; Guglielmino, C.; Musumeci, G. How Physical Activity Affects Knee Cartilage and a Standard Intervention Procedure for an Exercise Program: A Systematic Review. Healthcare 2022, 10, 1821. [Google Scholar] [CrossRef] [PubMed]
- Musumeci, G. Effects of COVID-19 Syndemic on Sport Community. J. Funct. Morphol. Kinesiol. 2022, 7, 19. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.Y.; Tsai, C.L.; Hsieh, K.W. Physical activity correlates for children with autism spectrum disorders in middle school physical education. Res. Q. Exerc. Sport. 2011, 82, 491–498. [Google Scholar] [CrossRef]
- Rios Colorado, J.D.; Patricia Sánchez, D.; Ordoñez Mora, L.T. Herramientas de evaluación psicomotriz en el trastorno del espectro autista. Revisión exploratoria. Rev. Española Salud Pública 2022, 95, e202109127. [Google Scholar]
- Maugeri, G.; Castrogiovanni, P.; Battaglia, G.; Pippi, R.; D’Agata, V.; Palma, A.; Di Rosa, M.; Musumeci, G. The impact of physical activity on psychological health during COVID-19 pandemic in Italy. Heliyon 2020, 6, e04315. [Google Scholar] [CrossRef] [PubMed]
- Dudley, D.; Okely, A.; Pearson, P.; Cotton, W. A systematic review of the effectiveness of physical education and school sport interventions targeting physical activity, movement skills and enjoyment of physical activity. Eur. Phys. Educ. Rev. 2011, 17, 353–378. [Google Scholar] [CrossRef]
- Yarımkaya, E.; Esentürk, O.K.; İlhan, E.L.; Kurtipek, S.; Işım, A.T. Zoom-delivered Physical Activities Can Increase Perceived Physical Activity Level in Children with Autism Spectrum Disorder: A Pilot Study. J. Dev. Phys. Disabil. 2023, 35, 189–207. [Google Scholar] [CrossRef] [PubMed]
- Ai, X.; Yang, J.; Lin, Z.; Wan, X. Mental Health and the Role of Physical Activity During the COVID-19 Pandemic. Front. Psychol. 2021, 12, 759987. [Google Scholar] [CrossRef] [PubMed]
- Yu, C.C.W.; Wong, S.W.L.; Lo, F.S.F.; So, R.C.H.; Chan, D.F.Y. Study protocol: A randomized controlled trial study on the effect of a game-based exercise training program on promoting physical fitness and mental health in children with autism spectrum disorder. BMC Psychiatry 2018, 18, 56. [Google Scholar] [CrossRef] [PubMed]
- Trovato, F.M.; Roggio, F.; Szychlinska, M.A.; Borzì, F.; Musumeci, G. Clinical Kinesiology and Posturology Applied to a Group of Italian Students. A Morphological Observational Study. J. Funct. Morphol. Kinesiol. 2015, 1, 16–29. [Google Scholar] [CrossRef]
- Deb, S.S.; Retzer, A.; Roy, M.; Acharya, R.; Limbu, B.; Roy, A. The effectiveness of parent training for children with autism spectrum disorder: A systematic review and meta-analyses. BMC Psychiatry 2020, 20, 583. [Google Scholar] [CrossRef]
- Nijhof, S.L.; Vinkers, C.H.; van Geelen, S.M.; Duijff, S.N.; Achterberg, E.J.M.; van der Net, J.; Veltkamp, R.C.; Grootenhuis, M.A.; van de Putte, E.M.; Hillegers, M.H.J.; et al. Healthy play, better coping: The importance of play for the development of children in health and disease. Neurosci. Biobehav. Rev. 2018, 95, 421–429. [Google Scholar] [CrossRef]
- Liguori, G.; American College of Sports Medicine (ACSM). ACSM’s Guidelines for Exercise Testing and Prescription; Lippincott Williams, Wilkins: Philadelphia, PA, USA, 2020. [Google Scholar]
- Donnelly, J.E.; Hillman, C.H.; Castelli, D.; Etnier, J.L.; Lee, S.; Tomporowski, P.; Lambourne, K.; Szabo-Reed, A.N. Physical Activity, Fitness, Cognitive Function, and Academic Achievement in Children: A Systematic Review. Med. Sci. Sports Exerc. 2016, 48, 1197–1222. [Google Scholar] [CrossRef]
- Radesky, J.S. Young children’s online-offline balance. Acta Paediatr. 2021, 110, 748–749. [Google Scholar] [CrossRef]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef] [PubMed]
- Roggio, F.; Trovato, B.; Ravalli, S.; Di Rosa, M.; Maugeri, G.; Bianco, A.; Palma, A.; Musumeci, G. One Year of COVID-19 Pandemic in Italy: Effect of Sedentary Behavior on Physical Activity Levels and Musculoskeletal Pain among University Students. Int. J. Environ. Res. Public Health 2021, 18, 8680. [Google Scholar] [CrossRef] [PubMed]
- Partis, M. Bowlby’s attachment theory: Implications for health visiting. Br. J. Community Nurs. 2000, 5, 499–503. [Google Scholar] [CrossRef] [PubMed]
- Waters, E.; Crowell, J.; Elliott, M.; Corcoran, D.; Treboux, D. Bowlby’s secure base theory and the social/personality psychology of attachment styles: Work(s) in progress. Attach. Hum. Dev. 2002, 4, 230–242. [Google Scholar] [CrossRef] [PubMed]
- Packard, K.; Opendak, M.; Soper, C.D.; Sardar, H.; Sullivan, R.M. Infant Attachment and Social Modification of Stress Neurobiology. Front. Syst. Neurosci. 2021, 15, 718198. [Google Scholar] [CrossRef] [PubMed]
- Dollman, J.; Norton, K.; Norton, L. Evidence for secular trends in children’s physical activity behaviour. Br. J. Sports Med. 2005, 39, 892–897, discussion 2005, 897. [Google Scholar] [CrossRef] [PubMed]
- Nelson, S.; Agoston, M.; Kovar-Gough, I.; Cunningham, N. A Scoping Review and Proposed Framework for Coping in Youth with a History of Psychological Trauma and Chronic Pain. J. Pediatr. Psychol. 2022, 47, 469–482. [Google Scholar] [CrossRef] [PubMed]
- Dhawale, A.K.; Smith, M.A.; Ölveczky, B.P. The Role of Variability in Motor Learning. Annu. Rev. Neurosci. 2017, 40, 479–498. [Google Scholar] [CrossRef] [PubMed]
- Ngai, S.S.; Cheung, C.-K.; Ng, Y.-H.; Shang, L.; Tang, H.-Y.; Ngai, H.-L.; Wong, K.H.-C. Time Effects of Supportive Interaction and Facilitator Input Variety on Treatment Adherence of Young People with Chronic Health Conditions: A Dynamic Mechanism in Mutual Aid Groups. Int. J. Environ. Res. Public Health 2021, 18, 3061. [Google Scholar] [CrossRef] [PubMed]
- Yarımkaya, E.; Esentürk, O.K. Promoting physical activity for children with autism spectrum disorders during Coronavirus outbreak: Benefits, strategies, and examples. Int. J. Dev. Disabil. 2022, 68, 430–435. [Google Scholar] [CrossRef]
- Baranowski, T. Families and health actions. In Handbook of Health Behavior Research 1: Personal and Social Determinants; Plenum Press: New York, NY, USA, 1997. [Google Scholar]
- Cochran, J.D.; Campbell, S.M.; Baker, H.M.; Leeds, E.M. The role of student characteristics in predicting retention in online courses. Res. High. Educ. 2014, 55, 27–48. [Google Scholar] [CrossRef]
- Taylor, W.C.; Baranowski, T.; Young, D.R. Physical activity interventions in low-income, ethnic minority, and populations with disability. Am. J. Prev. Med. 1998, 15, 334–343. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).