Vitamin D Status and Incidence of SARS-CoV-2 Reinfections in the Borriana COVID-19 Cohort: A Population-Based Prospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
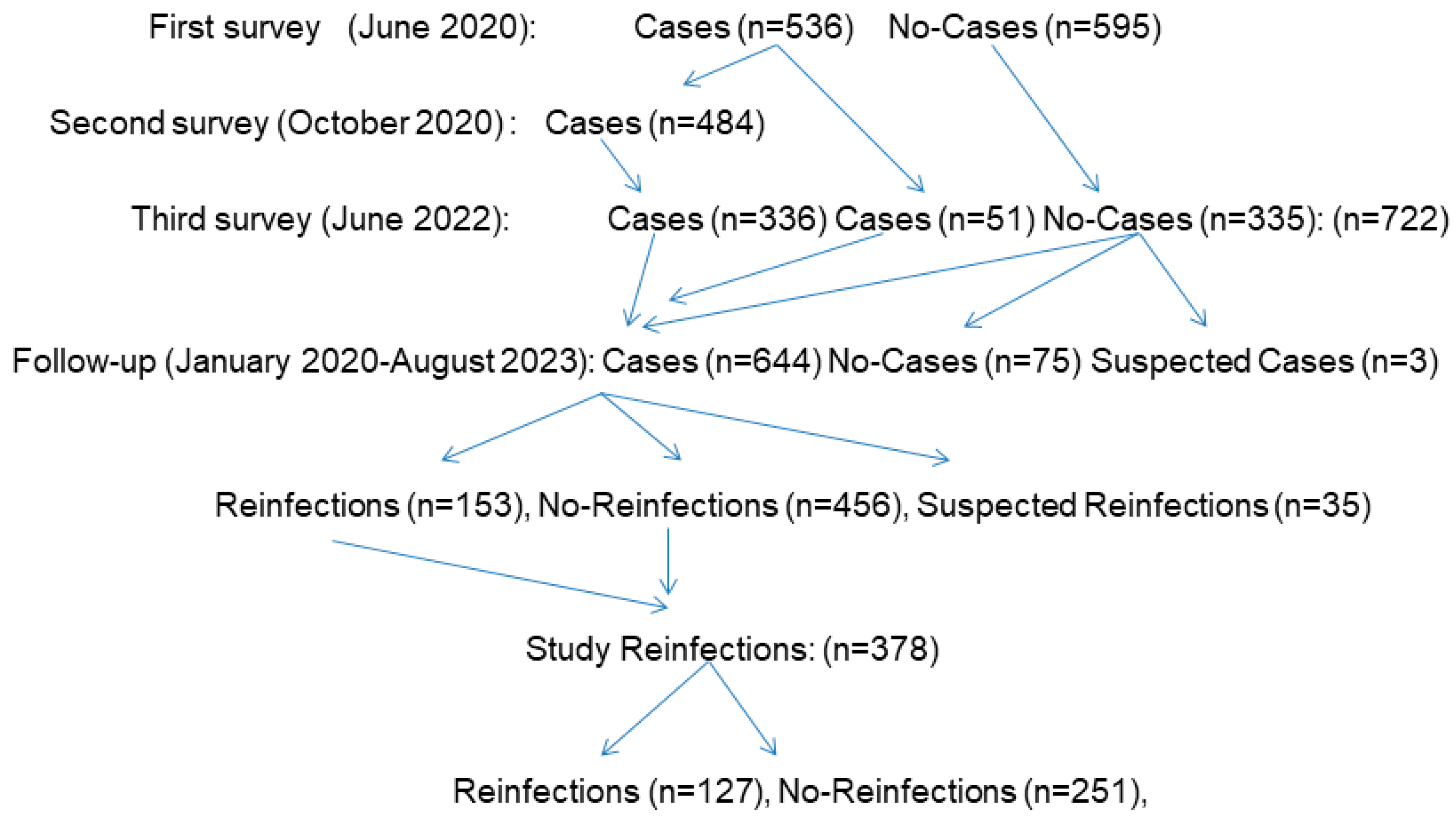
2.1. Description
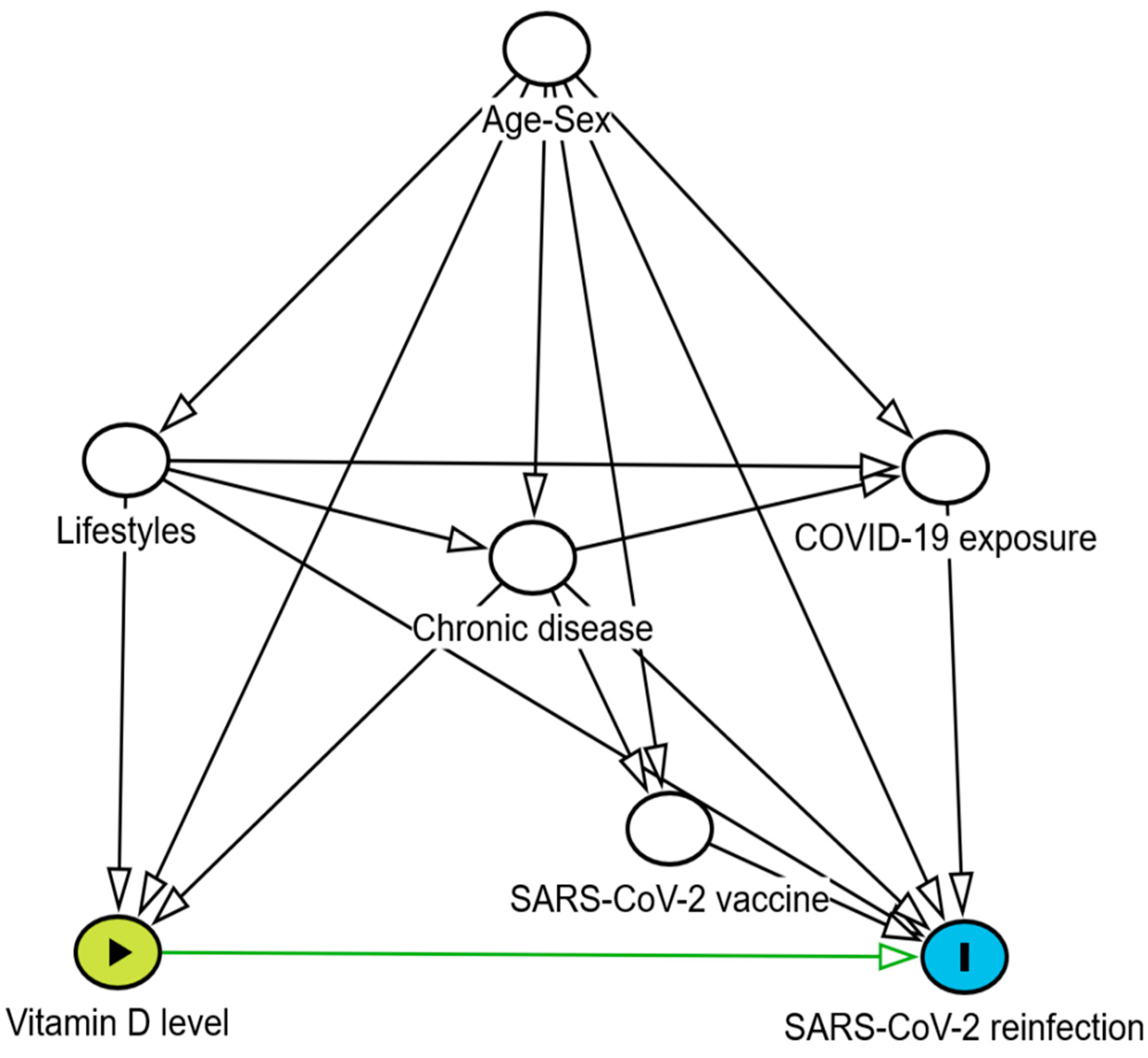
2.2. Statistical Methods
2.3. Sensitivity Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Grant, W.B.; Lahore, H.; McDonnell, S.L.; Baggerly, C.A.; French, C.B.; Aliano, J.L.; Bhattoa, H.P. Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients 2020, 12, 988. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Singh, C.M.; Ranjan, A.; Kumar, S.; Singh, D.K. Evidences suggesting a possible role of Vitamin D in COVID 19: The missing link. Indian J. Pharmacol. 2021, 53, 394–402. [Google Scholar] [CrossRef] [PubMed]
- Manson, J.E.; Bassuk, S.S. Commentary. Eliminating vitamin D deficiency during the COVID-19 pandemic: A call to action. Metabolism 2020, 112, 154322. [Google Scholar]
- Martineau, A.R.; Jolliffe, D.A.; Hooper, R.L.; Greenberg, L.; Aloia, J.F.; Bergman, P.; Dubnov-Raz, G.; Esposito, S.; Ganmaa, D.; Ginde, A.A.; et al. Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data. BMJ 2017, 356, i6583. [Google Scholar] [CrossRef]
- Aibana, O.; Huang, C.C.; Aboud, S.; Arnedo-Pena, A.; Becerra, M.C.; Bellido-Blasco, J.B.; Bhosale, R.; Calderon, R.; Chiang, S.; Contreras, C.; et al. Vitamin D status and risk of incident tuberculosis disease: A nested case-control study, systematic review, and individual-participant data meta-analysis. PLoS Med. 2019, 16, e1002907. [Google Scholar]
- Mercola, J.; Grant, W.B.; Wagner, C.L. Evidence regarding vitamin D and risk of COVID-19 and its severity. Nutrients 2020, 31, 3361. [Google Scholar] [CrossRef]
- Kaya, M.O.; Pamukçu, E.; Yakar, B. The role of vitamin D deficiency on COVID-19: A systematic review and meta-analysis of observational studies. Epidemiol. Health 2021, 43, e2021074. [Google Scholar]
- Akbar, M.R.; Wibowo, A.; Pranata, R.; Setiabudiawan, B. Low serum 25-hydroxyvitamin D (Vitamin D) level is associated with susceptibility to COVID-19, severity, and mortality: A systematic review and meta-analysis. Front. Nutr. 2021, 8, 660420. [Google Scholar] [CrossRef]
- Teshome, A.; Adane, A.; Girma, B.; Mekonnen, Z.A. The impact of vitamin D level on COVID-19 infection: Systematic review and meta-analysis. Front. Public Health 2021, 9, 624559. [Google Scholar]
- Hosseini, B.; El Abd, A.; Ducharme, F.M. Effects of vitamin D supplementation on COVID-19 related outcomes: A systematic review and meta-analysis. Nutrients 2022, 14, 2134. [Google Scholar] [CrossRef]
- Jamilian, A.; Ghalichi, F.; Hamedi Kalajahi, F.; Radkhah, N.; Jourabchi, N.; Musazadeh, V.; Amini-Salehi, E.; Zarezadeh, M.; Ostadrahimi, A. The role of vitamin D in outcomes of critical care in COVID-19 patients: Evidence from an umbrella meta-analysis of interventional and observational studies. Public Health Nutr. 2024, 27, e127. [Google Scholar] [CrossRef] [PubMed]
- Sartini, M.; Del Puente, F.; Oliva, M.; Carbone, A.; Bobbio, N.; Schinca, E.; Giribone, L.; Cristina, M.L. Preventive vitamin D supplementation and risk for COVID-19 infection: A systematic review and meta-analysis. Nutrients 2024, 16, 679. [Google Scholar] [CrossRef] [PubMed]
- Albergamo, A.; Apprato, G.; Silvagno, F. The role of vitamin D in supporting health in the COVID-19 Era. Int. J. Mol. Sci. 2022, 23, 3621. [Google Scholar] [CrossRef]
- Laporte, J.R. Crònica d’una Societat Intoxicada, 3rd ed.; Ediciones Península: Barcelona, Spain, 2024; pp. 384–387. [Google Scholar]
- Sinopoli, A.; Sciurti, A.; Isonne, C.; Santoro, M.M.; Baccolini, V. The efficacy of multivitamin, vitamin A, vitamin B, vitamin C, and vitamin D supplements in the prevention and management of COVID-19 and Long-COVID: An updated systematic review and meta-analysis of randomized clinical trials. Nutrients 2024, 16, 1345. [Google Scholar] [CrossRef]
- Bilezikian, J.P.; Binkley, N.; De Luca, H.F.; Fassio, A.; Formenti, A.M.; El-Hajj Fuleihan, G.; Heijboer, A.C.; Giustina, A. Consensus and controversial aspects of vitamin D and COVID-19. J. Clin. Endocrinol. Metab. 2023, 108, 1034–1042. [Google Scholar] [CrossRef]
- Jenkinson, C.; Desai, R.; McLeod, M.D.; Wolf Mueller, J.; Hewison, M.; Handelsman, D.J. Circulating conjugated and unconjugated vitamin D metabolite measurements by liquid chromatography mass spectrometry. J. Clin. Endocrinol. Metab. 2022, 107, 435–449. [Google Scholar] [CrossRef] [PubMed]
- Abdollahzadeh, R.; Shushizadeh, M.H.; Barazandehrokh, M.; Choopani, S.; Azarnezhad, A.; Paknahad, S.; Pirhoushiaran, M.; Makani, S.Z.; Yeganeh, R.Z.; Al-Kateb, A.; et al. Association of vitamin D receptor gene polymorphisms and clinical/severe outcomes of COVID-19 patients. Infect. Genet. Evol. 2021, 96, 105098. [Google Scholar] [CrossRef] [PubMed]
- Hamed, E.R.; Abdelhady, S.A.; Al-Touny, S.A.; Kishk, R.M.; Mohamed, M.H.; Rageh, F.; Othman, A.A.A.; Abdelfatah, W.; Azab, H. Correlation between rs7041 and rs4588 polymorphisms in vitamin D binding protein gene and COVID-19-related severity and mortality. BMC Med. Genom. 2024, 17, 284. [Google Scholar] [CrossRef]
- AlGhamdi, S.A.; Ghosh Dastidar, R.; Rybiński, M.; Alsufiani, H.M.; Khoja, S.O.; Enaibsi, N.N.; Saif, S.F.; Carlberg, C. Evaluation of the vitamin D response index in a Saudi cohort. Saudi Pharm. J. 2024, 32, 102137. [Google Scholar] [CrossRef]
- Smolders, J.; van den Ouweland, J.; Geven, C.; Pickkers, P.; Kox, M. Letter to the Editor: Vitamin D deficiency in COVID-19: Mixing up cause and consequence. Metabolism 2021, 115, 154434. [Google Scholar] [CrossRef]
- COVID-19 Forecasting Team. Past SARS-CoV-2 infection protection against re-infection: A systematic review and meta-analysis. Lancet 2023, 401, 833–842. [Google Scholar] [CrossRef] [PubMed]
- Deng, J.; Ma, Y.; Liu, Q.; Du, M.; Liu, M.; Liu, J. Severity and outcomes of SARS-CoV-2 reinfection compared with primary infection: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2023, 20, 3335. [Google Scholar] [CrossRef]
- Hu, W.H.; Cai, H.L.; Yan, H.C.; Wang, H.; Sun, H.M.; Wei, Y.Y.; Hao, Y.T. Protective effectiveness of previous infection against subsequent SARS-Cov-2 infection: Systematic review and meta-analysis. Front. Public Health 2024, 12, 1353415. [Google Scholar]
- Bøås, H.; Storm, M.L.; Tapia, G.; Kristoffersen, A.B.; Løvlie, A.L.; Størdal, K.; Lyngstad, T.M.; Bragstad, K.; Hungnes, O.; Veneti, L. Frequency and risk of SARS-CoV-2 reinfections in Norway: A nation-wide study, February 2020 to January 2022. BMC Public Health 2024, 24, 181. [Google Scholar]
- Gómez-Gonzales, W.; Chihuantito-Abal, L.A.; Gamarra-Bustillos, C.; Morón-Valenzuela, J.; Zavaleta-Oliver, J.; Gomez-Livias, M.; Vargas-Pancorbo, L.; Auqui-Canchari, M.E.; Mejía-Zambrano, H. Risk factors contributing to reinfection by SARS-CoV-2: A systematic review. Adv. Respir. Med. 2023, 91, 560–570. [Google Scholar] [CrossRef] [PubMed]
- Ismail, N.F.; Rahman, A.E.; Kulkarni, D.; Zhu, F.; Wang, X.; Del Carmen Morales, G.; Srivastava, A.; Allen, K.E.; Spinardi, J.; Kyaw, M.H.; et al. Incidence and outcome of SARS-CoV-2 reinfection in the pre-Omicron era: A global systematic review and meta-analysis. J. Glob. Health 2023, 13, 06051. [Google Scholar]
- Domènech-Montoliu, S.; Pac-Sa, M.R.; Vidal-Utrillas, P.; Latorre-Poveda, M.; Del Rio-González, A.; Ferrando-Rubert, S.; Ferrer-Abad, G.; Sánchez-Urbano, M.; Aparisi-Esteve, L.; Badenes-Marques, G.; et al. Mass gathering events and COVID-19 transmission in Borriana (Spain): A retrospective cohort study. PLoS ONE 2021, 16, e0256747. [Google Scholar]
- Domènech-Montoliu, S.; Puig-Barberà, J.; Pac-Sa, M.R.; Vidal-Utrillas, P.; Latorre-Poveda, M.; Del Rio-González, A.; Ferrando-Rubert, S.; Ferrer-Abad, G.; Sánchez-Urbano, M.; Aparisi-Esteve, L.; et al. Persistence of anti-SARS-CoV-2 antibodies six months after infection in an outbreak with five hundred COVID-19 cases in Borriana (Spain): A prospective cohort study. COVID 2021, 1, 71–82. [Google Scholar] [CrossRef]
- Domènech-Montoliu, S.; Puig-Barberà, J.; Guerra-Murcia, O.; Pac-Sa, M.R.; Orrico-Sanchéz, A.; Gómez-Lanas, L.; Sala-Trull, D.; Domènech-León, C.; Del Rio-González, A.; Sánchez-Urbano, M.; et al. ABO blood groups and incidence of COVID-19 in the mass gathering events in borriana (Spain), March 2020: A retrospective cohort study. Epidemiologia 2023, 4, 63–73. [Google Scholar] [CrossRef]
- Domènech-Montoliu, S.; Puig-Barberà, J.; Pac-Sa, M.R.; Orrico-Sanchéz, A.; Gómez-Lanas, L.; Sala-Trull, D.; Domènech-León, C.; Del Rio-González, A.; Sánchez-Urbano, M.; Satorres-Martinez, P.; et al. Cellular immunity of SARS-CoV-2 in the Borriana COVID-19 Cohort: A nested case-control study. Epidemiologia 2024, 5, 167–186. [Google Scholar] [CrossRef]
- Asif, M.; Groboske, S.E.; Leung, E.K.Y.; Yeo, K.J.; van Wijk, X.M.R. Evaluation of a new generation automated assay for 25-Hydroxy vitamin D based on competitive protein binding. J. Appl. Lab. Med. 2019, 4, 247–253. [Google Scholar] [PubMed]
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Reinfection with SARS-CoV-2: Implementation of a Surveillance Case Definition Within the EU/EEA. 2021. Available online: https://www.ecdc.europa.eu/en/publications-data/reinfection-sars-cov-2-implementation-surveillance-case-definition-within-eueea (accessed on 26 June 2024).
- Narasimhan, M.; Mahimainathan, L.; Araj, E.; Clark, A.E.; Markantonis, J.; Green, A.; Xu, J.; SoRelle, J.A.; Alexis, C.; Fankhauser, K.; et al. Clinical evaluation of the Abbott Alinity SARS-CoV-2 sike-specific quantitative IgG and IgM assays among infected, recovered, and vaccinated groups. J. Clin. Microbiol. 2021, 59, e0038821. [Google Scholar] [CrossRef]
- Egger, M.; Bundschuh, C.; Wiesinger, K.; Gabriel, C.; Clodi, M.; Mueller, T.; Dieplinger, B. Comparison of the Elecsys® Anti-SARS-CoV-2 immunoassay with the EDI™ enzyme linked immunosorbent assays for the detection of SARS-CoV-2 antibodies in human plasma. Clin. Chim. Acta 2020, 509, 18–21. [Google Scholar] [CrossRef]
- Textor, J.; van der Zander, B.; Gilthorpe, M.S.; Liskiewicz, M.; Ellison, G.T. Robust causal inference using directed acyclic graphs: The R package ‘dagitty’. Int. J. Epidemiol. 2016, 45, 1887–1894. [Google Scholar] [PubMed]
- Robins, J.M.; Hernán, M.A.; Brumback, B. Marginal structural models and causal inference in epidemiology. Epidemiology 2000, 11, 550–560. [Google Scholar]
- Oskarsson, V.; Eliasson, M.; Salomaa, V.; Reinikainen, J.; Männistö, S.; Palmieri, L.; Donfrancesco, C.; Sans, S.; Costanzo, S.; de Gaetano, G.; et al. Influence of geographical latitude on vitamin D status: Cross-sectional results from the BiomarCaRE consortium. Br. J. Nutr. 2022, 128, 2208–2218. [Google Scholar]
- Fernández-Vicente, M.; Miján-de-la-Torre, A.; Vella-Ramírez, J.C.; Martí-Bonmatí, E.; Benito-Ibáñez, V.V.; Martínez-de-Arriba, R. Influencing variables on total and free 25(OH)D levels in healthy population. Rev. Clínica Española 2022, 222, 313–320. [Google Scholar]
- Cui, A.; Zhang, T.; Xiao, P.; Fan, Z.; Wang, H.; Zhuang, Y. Global and regional prevalence of vitamin D deficiency in population-based studies from 2000 to 2022: A pooled analysis of 7.9 million participants. Front. Nutr. 2023, 10, 1070808. [Google Scholar] [CrossRef]
- Rivelli, A.; Fitzpatrick, V.; Blair, C.; Copeland, K.; Richards, J. Incidence of COVID-19 reinfection among Midwestern healthcare employees. PLoS ONE 2022, 17, e0262164. [Google Scholar]
- Yu, W.; Guo, Y.; Hu, T.; Liu, Y.; Fan, Q.; Guo, L.; Zheng, B.; Kong, Y.; Zhu, H.; Yu, J.; et al. Incidence and severity of SARS-CoV-2 reinfection, a multicenter cohort study in Shanghai, China. J. Med. Virol. 2023, 95, e28997. [Google Scholar] [CrossRef]
- Mokhayeri, Y.; Taherpour, N.; Shahbazi, F.; Ghorbani, S.S.; Fallah, S.; Etemad, K.; Izadi, N.; Mehri, A.; Farhadi-Babadi, K.; Rahimi, E.; et al. Estimation of outpatient SARS-CoV-2 reinfection and recurrence rates and associated factors among COVID-19 hospitalized patients over one-year old: A multicenter retrospective cohort study. BMC Infect. Dis. 2024, 24, 999. [Google Scholar] [CrossRef] [PubMed]
- Medić, S.; Anastassopoulou, C.; Lozanov-Crvenković, Z.; Vuković, V.; Dragnić, N.; Petrović, V.; Ristić, M.; Pustahija, T.; Gojković, Z.; Tsakris, A.; et al. Risk and severity of SARS-CoV-2 reinfections during 2020–2022 in Vojvodina, Serbia: A population-level observational study. Lancet Reg. Health–Eur. 2022, 20, 100453. [Google Scholar] [CrossRef] [PubMed]
- Zheng, H.; Wu, S.; Chen, W.; Cai, S.; Zhan, M.; Chen, C.; Lin, J.; Xie, Z.; Ou, J.; Ye, W. Meta-analysis of hybrid immunity to mitigate the risk of Omicron variant reinfection. Front. Public Health 2024, 12, 1457266. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.; Stoesser, N.; Matthews, P.C.; Khera, T.; Gethings, O.; Diamond, I.; Studley, R.; Taylor, N.; Peto, T.E.A.; Walker, A.S.; et al. Risk of SARS-CoV-2 reinfection during multiple Omicron variant waves in the UK general population. Nat. Commun. 2024, 15, 1008. [Google Scholar] [CrossRef]
- Hodcroft, E.; CoVariants. Overview of Variants in Countries. Covariants.org. Available online: https://covariants.org/per-country?country=Spain (accessed on 1 January 2025).
- Chen, J.; Lu, F.; Shen, B.; Xu, H.; Chen, Y.; Hu, Q.; Xu, A.; Tung, T.H.; Hong, D. Associations between pre-infection serum vitamin D concentrations and Omicron COVID-19 incidence, severity and reoccurrence in elderly individuals. Public Health Nutr. 2024, 27, e197. [Google Scholar] [CrossRef]
- Abu Fanne, R.; Moed, M.; Kedem, A.; Lidawi, G.; Maraga, E.; Mohsen, F.; Roguin, A.; Meisel, S.R. SARS-CoV-2 infection-blocking immunity post natural infection: The role of vitamin D. Vaccines 2023, 11, 475. [Google Scholar] [CrossRef]
- Oristrell, J.; Oliva, J.C.; Casado, E.; Subirana, I.; Domínguez, D.; Toloba, A.; Balado, A.; Grau, M. Vitamin D supplementation and COVID-19 risk: A population-based, cohort study. J. Endocrinol. Investig. 2022, 45, 167–179. [Google Scholar] [CrossRef]
- Basińska-Lewandowska, M.; Lewandowski, K.; Horzelski, W.; Lewiński, A.; Skowrońska-Jóźwiak, E. Frequency of COVID-19 infection as a function of vitamin D levels. Nutrients 2023, 15, 1581. [Google Scholar] [CrossRef]
- Meltzer, D.O.; Best, T.J.; Zhang, H.; Vokes, T.; Arora, V.; Solway, J. Association of vitamin D status and other clinical characteristics with COVID-19 test results. JAMA Netw. Open 2020, 3, e2019722. [Google Scholar] [CrossRef]
- Merzon, E.; Tworowski, D.; Gorohovski, A.; Vinker, S.; Golan Cohen, A.; Green, I.; Frenkel-Morgenstern, M. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: An Israeli population-based study. FEBS J. 2020, 287, 3693–3702. [Google Scholar]
- Israel, A.; Cicurel, A.; Feldhamer, I.; Stern, F.; Dror, Y.; Giveon, S.M.; Gillis, D.; Strich, D.; Lavie, G. Vitamin D deficiency is associated with higher risks for SARS-CoV-2 infection and COVID-19 severity: A retrospective case-control study. Intern. Emerg. Med. 2022, 17, 1053–1063. [Google Scholar] [PubMed]
- Kaufman, H.W.; Niles, J.K.; Kroll, M.H.; Bi, C.; Holick, M.F. SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels. PLoS ONE 2020, 15, e0239252. [Google Scholar]
- Zeidan, N.M.S.; Lateef, H.M.A.E.; Selim, D.M.; Razek, S.A.; Abd-Elrehim, G.A.B.; Nashat, M.; ElGyar, N.; Waked, N.M.; Soliman, A.A.; Elhewala, A.A.; et al. Vitamin D deficiency and vitamin D receptor FokI polymorphism as risk factors for COVID-19. Pediatr. Res. 2023, 93, 1383–1390. [Google Scholar] [PubMed]
- Seal, K.H.; Bertenthal, D.; Carey, E.; Grunfeld, C.; Bikle, D.D.; Lu, C.M. Association of vitamin D status and COVID-19-related hospitalization and mortality. J. Gen. Intern. Med. 2022, 37, 853–861. [Google Scholar] [CrossRef] [PubMed]
- Dror, A.A.; Morozov, N.; Daoud, A.; Namir, Y.; Yakir, O.; Shachar, Y.; Lifshitz, M.; Segal, E.; Fisher, L.; Mizrachi, M.; et al. Pre-infection 25-hydroxyvitamin D3 levels and association with severity of COVID-19 illness. PLoS ONE 2022, 17, e0263069. [Google Scholar]
- Ling, S.F.; Broad, E.; Murphy, R.; Pappachan, J.M.; Pardesi-Newton, S.; Kong, M.F.; Jude, E.B. High-dose cholecalciferol booster therapy is associated with a reduced risk of mortality in patients with COVID-19: A cross-sectional multi-centre observational study. Nutrients 2020, 12, 3799. [Google Scholar]
- Singh, A.; Rastogi, A.; Puri, G.D.; Ganesh, V.; Naik, N.B.; Kajal, K.; Kahlon, S.; Soni, S.L.; Kaloria, N.; Saini, K.; et al. Therapeutic high-dose vitamin D for vitamin D-deficient severe COVID-19 disease: Randomized, double-blind, placebo-controlled study (SHADE-S). J. Public Health 2024, 46, 256–266. [Google Scholar] [CrossRef]
- Ma, W.; Nguyen, L.H.; Yue, Y.; Ding, M.; Drew, D.A.; Wang, K.; Merino, J.; Rich-Edwards, J.W.; Sun, Q.; Camargo, C.A.; et al. Associations between predicted vitamin D status, vitamin D intake, and risk of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and coronavirus disease 2019 (COVID-19) severity. Am. J. Clin. Nutr. 2022, 115, 1123–1133. [Google Scholar]
- Li, Y.; Tong, C.H.; Bare, L.A.; Devlin, J.J. Assessment of the association of vitamin D level with SARS-CoV-2 seropositivity among working-age adults. JAMA Netw. Open 2021, 4, e2111634. [Google Scholar]
- Liu, Y.; Clare, S.; D’Erasmo, G.; Heilbronner, A.; Dash, A.; Krez, A.; Zaworski, C.; Haseltine, K.; Serota, A.; Miller, A.; et al. Vitamin D and SARS-CoV-2 infection: SERVE Study (SARS-CoV-2 exposure and the role of vitamin D among hospital employees). J. Nutr. 2023, 153, 1420–1426. [Google Scholar]
- Ferrari, D.; Locatelli, M. No significant association between vitamin D and COVID-19: A retrospective study from a northern Italian hospital. Int. J. Vitam. Nutr. Res. 2021, 91, 200–203. [Google Scholar] [CrossRef]
- Crandell, I.; Rockwell, M.; Whitehead, P.; Carter, K.F.; Hanlon, A. Examination of the moderating effect of race on the relationship between vitamin D status and COVID-19 test positivity using propensity score methods. J. Am. Nutr. Assoc. 2022, 41, 646–657. [Google Scholar] [CrossRef] [PubMed]
- Ganmaa, D.; Chinbayar, T.; Khudaykov, P.; Nasantogtoh, E.; Ariunbuyan, S.; Enkhtsetseg, T.; Sarangua, G.; Chan, A.; Tserendagva, D. Latent TB infection, vitamin D status and COVID-19 severity in Mongolian patients. Nutrients 2023, 15, 3979. [Google Scholar] [CrossRef] [PubMed]
- da Rocha, A.P.; Atallah, A.N.; Aldrighi, J.M.; Pires, A.L.R.; Dos Santos Puga, M.E.; Pinto, A.C.P.N. Insufficient evidence for vitamin D use in COVID-19: A rapid systematic review. Int. J. Clin. Pract. 2021, 75, e14649. [Google Scholar] [CrossRef]
- Butler-Laporte, G.; Nakanishi, T.; Mooser, V.; Morrison, D.R.; Abdullah, T.; Adeleye, O.; Mamlouk, N.; Kimchi, N.; Afrasiabi, Z.; Rezk, N.; et al. Vitamin D and COVID-19 susceptibility and severity in the COVID-19 host genetics initiative: A Mendelian randomization study. PLoS Med. 2021, 18, e1003605. [Google Scholar] [CrossRef] [PubMed]
- Villasis-Keever, M.A.; López-Alarcón, M.G.; Miranda-Novales, G.; Zurita-Cruz, J.N.; Barrada-Vázquez, A.S.; González-Ibarra, J.; Martínez-Reyes, M.; Grajales-Muñiz, C.; Santacruz-Tinoco, C.E.; Martínez-Miguel, B.; et al. Efficacy and safety of vitamin D supplementation to prevent COVID-19 in frontline healthcare workers. A randomized clinical trial. Arch. Med. Res. 2022, 53, 423–430. [Google Scholar]
- Jolliffe, D.A.; Holt, H.; Greenig, M.; Talaei, M.; Perdek, N.; Pfeffer, P.; Vivaldi, G.; Maltby, S.; Symons, J.; Barlow, N.L.; et al. Effect of a test-and-treat approach to vitamin D supplementation on risk of all cause acute respiratory tract infection and covid-19: Phase 3 randomised controlled trial (CORONAVIT). BMJ 2022, 378, e071230. [Google Scholar]
- Brunvoll, S.H.; Nygaard, A.B.; Ellingjord-Dale, M.; Holland, P.; Istre, M.S.; Kalleberg, K.T.; Søraas, C.L.; Holven, K.B.; Ulven, S.M.; Hjartåker, A.; et al. Prevention of covid-19 and other acute respiratory infections with cod liver oil supplementation, a low dose vitamin D supplement: Quadruple blinded, randomised placebo controlled trial. BMJ 2022, 378, e071245. [Google Scholar] [CrossRef]
- Karonova, T.L.; Chernikova, A.T.; Golovatyuk, K.A.; Bykova, E.S.; Grant, W.B.; Kalinina, O.V.; Grineva, E.N.; Shlyakhto, E.V. Vitamin D intake may reduce SARS-CoV-2 infection morbidity in health care workers. Nutrients 2022, 14, 505. [Google Scholar] [CrossRef]
- Grant, W.B.; Boucher, B.J.; Bhattoa, H.P.; Lahore, H. Why vitamin D clinical trials should be based on 25-hydroxyvitamin D concentrations. J. Steroid Biochem. Mol. Biol. 2018, 177, 266–269. [Google Scholar] [CrossRef]
- Pilz, S.; Trummer, C.; Theiler-Schwetz, V.; Grübler, M.R.; Verheyen, N.D.; Odler, B.; Karras, S.N.; Zittermann, A.; März, W. Critical appraisal of large vitamin D randomized controlled trials. Nutrients 2022, 14, 303. [Google Scholar] [CrossRef] [PubMed]
- Sobczak, M.; Pawliczak, R. Effect of Vitamin D3 supplementation on severe COVID-19: A meta-analysis of randomized clinical trials. Nutrients 2024, 16, 1402. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, S.; Griffin, G.; Hewison, M.; Hopkin, J.; Kenny, R.A.; Laird, E.; Quinton, R.; Thickett, D.; Rhodes, J.M. Vitamin D and COVID-19 revisited. J. Intern. Med. 2022, 292, 604–626. [Google Scholar] [CrossRef] [PubMed]
- Martineau, A.R. Vitamin D in the prevention or treatment of COVID-19. Proc. Nutr. Soc. 2023, 82, 200–207. [Google Scholar] [CrossRef]
- Autier, P.; Doi, G.; Mullie, P.; Vankrunkelsven, P.; D’Ecclesiis, O.; Gandini, S. Vitamin D, acute respiratory infections, and Covid-19: The curse of small-size randomised trials. A critical review with meta-analysis of randomised trials. PLoS ONE 2025, 20, e0303316. [Google Scholar] [CrossRef]
- Bishop, E.L.; Ismailova, A.; Dimeloe, S.; Hewison, M.; White, J.H. Vitamin D and immune regulation: Antibacterial, antiviral, anti-Inflammatory. J. Bone Miner. Res. Plus 2020, 5, e10405. [Google Scholar] [CrossRef]
- Ao, T.; Kikuta, J.; Ishii, M. The effects of vitamin D on immune system and inflammatory diseases. Biomolecules 2021, 11, 1624. [Google Scholar] [CrossRef]
- Ismailova, A.; White, J.H. Vitamin D, infections and immunity. Rev. Endocr. Metab. Disord. 2022, 23, 265–277. [Google Scholar] [CrossRef]
- Peng, M.Y.; Liu, W.C.; Zheng, J.Q.; Lu, C.L.; Hou, Y.C.; Zheng, C.M.; Song, J.Y.; Lu, K.C.; Chao, Y.C. Immunological aspects of SARS-CoV-2 infection and the putative beneficial role of vitamin-D. Int. J. Mol. Sci. 2021, 22, 5251. [Google Scholar] [CrossRef]
- Holick, M.F. The one-hundred-year anniversary of the discovery of the sunshine vitamin D3: Historical, personal experience and evidence-based perspectives. Nutrients 2023, 15, 593. [Google Scholar] [CrossRef] [PubMed]
- Arora, J.; Patel, D.R.; Nicol, M.J.; Field, C.J.; Restori, K.H.; Wang, J.; Froelich, N.E.; Katkere, B.; Terwilliger, J.A.; Weaver, V.; et al. Vitamin D and the ability to produce 1,25(OH)2D are critical for protection from viral infection of the lungs. Nutrients 2022, 14, 3061. [Google Scholar] [CrossRef]
- Campolina-Silva, G.; Andrade, A.C.D.S.P.; Couto, M.; Bittencourt-Silva, P.G.; Queiroz-Junior, C.M.; Lacerda, L.S.B.; Chaves, I.M.; de Oliveira, L.C.; Marim, F.M.; Oliveira, C.A.; et al. Dietary vitamin D mitigates coronavirus-induced lung inflammation and damage in mice. Viruses 2023, 15, 2434. [Google Scholar] [CrossRef] [PubMed]
- Jafarpoor, A.; Jazayeri, S.M.; Bokharaei-Salim, F.; Ataei-Pirkooh, A.; Ghaziasadi, A.; Soltani, S.; Sadeghi, A.; Marvi, S.S.; Poortahmasebi, V.; Khorrami, S.M.S.; et al. VDR gene polymorphisms are associated with the increased susceptibility to COVID-19 among iranian population: A case-control study. Int. J. Immunogenet. 2022, 49, 243–253. [Google Scholar]
- Domènech-Montoliu, S.; Puig-Barberà, J.; Pac-Sa, M.R.; Vidal-Utrillas, P.; Latorre-Poveda, M.; Del Rio-González, A.; Ferrando-Rubert, S.; Ferrer-Abad, G.; Sánchez-Urbano, M.; Aparisi-Esteve, L.; et al. Complications post-COVID-19 and risk factors among patients after six months of a SARS-CoV-2 infection: A population-based prospective cohort study. Epidemiologia 2022, 3, 49–67. [Google Scholar] [CrossRef] [PubMed]
- Domènech-Montoliu, S.; Puig-Barberà, J.; Badenes-Marques, G.; Gil-Fortuño, M.; Orrico-Sánchez, A.; Pac-Sa, M.R.; Perez-Olaso, O.; Sala-Trull, D.; Sánchez-Urbano, M.; Arnedo-Pena, A. Long COVID prevalence and the impact of the third SARS-CoV-2 vaccine dose: A cross-sectional analysis from the third follow-up of the Borriana Cohort, Valencia, Spain (2020–2022). Vaccines 2023, 11, 1590. [Google Scholar]
- Altieri, B.; Cavalier, E.; Bhattoa, H.P.; Pérez-López, F.R.; López-Baena, M.T.; Pérez-Roncero, G.R.; Chedraui, P.; Annweiler, C.; Della Casa, S.; Zelzer, S.; et al. Vitamin D testing: Advantages and limits of the current assays. Eur. J. Clin. Nutr. 2020, 74, 231–247. [Google Scholar]
- Binick, S.; Matthews, S.W.; Kamp, K.J.; Heitkemper, M. Vitamin D measurement: Clinical practice and research implications. J. Nurse Pract. 2023, 19, 104481. [Google Scholar]
- Geno, K.A.; Tolan, N.V.; Singh, R.J.; Nerenz, R.D. Improved recognition of 25-hydroxyvitamin D2 by 2 automated immunoassays. J. Appl. Lab. Med. 2020, 5, 1287–1295. [Google Scholar]
- Monson, R. Occupational Epidemiology; CRC Press: Boca Raton, FL, USA, 1982; pp. 94–95. [Google Scholar]
- DiNicolantonio, J.J.; O’Keefe, J.H. Magnesium and vitamin D deficiency as a potential cause of immune dysfunction, cytokine storm and disseminated intravascular coagulation in Covid-19 patients. Mo. Med. 2021, 118, 68–73. [Google Scholar]
- Guerrero-Romero, F.; Micke, O.; Simental-Mendía, L.E.; Rodríguez-Morán, M.; Vormann, J.; Iotti, S.; Banjanin, N.; Rosanoff, A.; Baniasadi, S.; Pourdowlat, G. Importance of magnesium status in COVID-19. Biology 2023, 12, 735. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, S.J.; Moradi, B.; Marhemati, M.; Firouzian, A.A.; Ildarabadi, E.; Abedi, A.; Firooz, M. Comparing serum levels of vitamin D and Zinc in novel coronavirus-infected patients and healthy individuals in Northeastern Iran, 2020. Infect. Dis. Clin. Pract. 2021, 29, e390–e394. [Google Scholar]
- Rizwan, M.; Cheng, K.; Gang, Y.; Hou, Y.; Wang, C. Immunomodulatory effects of vitamin D and zinc on viral infection. Biol. Trace Elem. Res. 2025, 203, 1–17. [Google Scholar] [PubMed]
| Variables | Reinfections n = 127 N (%) | No-Reinfections n = 251 N (%) | p-Value |
|---|---|---|---|
| Age (years) + SD 1 | 37.9 ± 17.0 | 39.2 ± 16.4 | 0.53 |
| Age 1–24 years | 34 (26.8) | 57 (22.7) | 0.70 |
| 25–44 years | 43 (33.9) | 90 (35.9) | |
| 45 years and over | 50 (39.7) | 104 (41.4) | |
| Sex Female | 82(64.6) | 159(63.3) | 0.91 |
| Male | 45(35.4) | 92 (36.7) | |
| Chronic disease 2 Yes | 48 (38.4) | 95 (38.2) | 1.00 |
| Chronic disease No | 77 (61.6) | 154(61.8) | |
| Cardiovascular disease Yes | 14 (11.3) | 37 (14.9) | 0.42 |
| No | 110 (88.7) | 212 (85.1) | |
| Arterial hypertension Yes | 12 (9.8) | 24 (9.6) | 1.00 |
| No | 111 (90.2) | 225 (90.4) | |
| Diabetes mellitus Yes | 3 (2.4) | 6 (2.4) | 1.00 |
| No | 121 (97.6) | 243 (97.6) | |
| Hypothyroidism Yes | 7 (5.7) | 12 (4.8) | 0.80 |
| No | 117 (94.3) | 237(95.2) | |
| Ashma Yes | 3 (2.4) | 14 (5.6) | 0.20 |
| No | 121 (97.6) | 235 (94.4) | |
| Allergic rhinitis Yes | 9 (7.3) | 10 (4.0) | 0.21 |
| No | 115 (92.7) | 239 (96.0) | |
| Obesity 3 BMI 4 ≥ 30 | 24 (18.9) | 51 (20.7) | 0.79 |
| BMI < 30 | 103 (81.1) | 195(79.3) | |
| Alcohol consumption 5 Yes | 28 (22.8) | 50 (20.7) | 0.59 |
| Alcohol consumption No | 95 (77.2) | 196 (79.3) | |
| Never smoked 6 | 70 (42.6) | 155 (63.3) | 0.31 |
| Current smoker and ex-smoker | 52 (57.4) | 90 (36.7) | |
| Doses SARS-CoV-2 vaccine | 0.10 | ||
| 0 | 6 (4.7) | 5 (2.0) | |
| 1 | 11 (8.7) | 11 (4.4) | |
| 2 | 40 (31.5) | 70 (27.9) | |
| 3–4 | 70 (55.1) | 165 (65.7) | |
| Family COVID-19 case Yes | 83(65.4) | 151 (60.2) | 0.37 |
| Family COVID-19 case No | 44 (34.5) | 100 (39.8) | |
| High exposure COVID-19 case 7 Yes | 70 (55.6) | 199 (60.3) | 0.44 |
| High exposure COVID-19 case No | 56 (44.4) | 98 (39.7) |
| Vitamin D | Reinfections | No-Reinfections | Total | |
|---|---|---|---|---|
| Three levels | N = 127 (%) | N = 251 (%) | N (%) | p-value |
| 0–19 ng/mL | 11 (8.7) | 17 (6.8) | 28 (39.2) | 0.10 |
| 20–29 ng/mL | 69 (54.3) | 112 (44.6) | 181 (38.1) | |
| ≥30 ng/mL | 47 (37.0) | 122 (48.6) | 169 (27.8) | |
| Two levels | ||||
| 0–29 ng/mL | 80 (63.0) | 129 (51.4) | 209 | 0.04 |
| ≥30 ng/mL | 47 (37.0) | 122 (48.6) | 169 | |
| Vitamin D ng/mL + SD 1 | 29.0 ± 8.3 | 30.4 ±8.9 | 0.17 |
| Vitamin D Levels | SARS-CoV-2 Reinfections | Person-Days | Incidence Rate 1000 Person-Days | 95% CI |
|---|---|---|---|---|
| <20 ng/mL | 11 | 22,074 | 0.50 | 0.28–0.90 |
| 20–29 ng/mL | 69 | 138,627 | 0.50 | 0.39–0.63 |
| ≥30 ng/mL | 47 | 126,578 | 0.37 | 0.28–0.49 |
| <30 ng/mL | 80 | 160,701 | 0.50 | 0.40–0.62 |
| ≥30 ng/mL | 47 | 126,578 | 0.37 | 0.28–0.49 |
| Total | 127 | 287,348 | 0.44 | 0.37–0.53 |
| Vitamin D | Crude Hazard Ratios | Adjusted Hazard Ratios 1 | ||
|---|---|---|---|---|
| Levels | HR (95% CI) | p-value | HR (95% CI) | p-value |
| <20 ng/mL | 1.25(0.65–2.42) | 0.50 | 1.79 (0.89–3.59) | 0.10 |
| 20–29 ng/mL | 1.26 (0.87–1.83) | 0.22 | 1.59 (1.06–2.38) | 0.02 |
| ≥30 ng/mL | 1.00 | 1.00 | ||
| Trend | 1.17 (0.89–1.55) | 0.26 | 1.42 (1.06–1.92) | 0.02 |
| <30 ng/mL | 1.26 (0.88–1.82) | 0.21 | 1.61 (1.09–2.39) | 0.02 |
| ≥30 ng/mL | 1.00 | 1.00 | ||
| Vitamin D Levels | Crude Incidence Rate | 95% CI | Adjusted 1 Incidence Rate | 95% CI |
|---|---|---|---|---|
| <20 ng/mL | 0.39 | 0.21–0.57 | 0.32 | 0.17–0.49 |
| 20–29 ng/mL | 0.38 | 0.31–0.45 | 0.40 | 0.33–0.47 |
| ≥30 ng/mL | 0.28 | 0.21–0.35 | 0.25 | 0.18–0.31 |
| Trend | Z = 2.09 | p-value = 0.04 | Z = 2.54 | p-value = 0.01 |
| <30 ng/mL | 0.38 | 0.31–0.45 | 0.40 | 0.33–0.47 |
| ≥30 ng/mL | 0.28 | 0.21–0.35 | 0.25 | 0.18–0.32 |
| Vitamin D | Crude Relative Risk | Adjusted Relative Risk 1 | ||
|---|---|---|---|---|
| Levels (ng/mL) | RR (95% CI) | p-value | RR (95% CI) | p-value |
| <20 ng/mL | 1.41 (0.84–2.38) | 0.19 | 1.29 (0.74–2.22) | 0.37 |
| 20–29 ng/mL | 1.37 (1.01–1.87) | 0.04 | 1.57 (1.15–2.16) | 0.01 |
| ≥30 ng/mL | 1.00 | 1.00 | ||
| <30 ng/mL | 1.38 (1.02–1.85) | 0.04 | 1.57 (1.15–2.15) | 0.01 |
| ≥30 ng/mL | 1.00 | 1.00 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Domènech-Montoliu, S.; López-Diago, L.; Aleixandre-Gorriz, I.; Pérez-Olaso, Ó.; Sala-Trull, D.; Rio-González, A.D.; Pac-Sa, M.R.; Sánchez-Urbano, M.; Satorres-Martinez, P.; Casanova-Suarez, J.; et al. Vitamin D Status and Incidence of SARS-CoV-2 Reinfections in the Borriana COVID-19 Cohort: A Population-Based Prospective Cohort Study. Trop. Med. Infect. Dis. 2025, 10, 98. https://doi.org/10.3390/tropicalmed10040098
Domènech-Montoliu S, López-Diago L, Aleixandre-Gorriz I, Pérez-Olaso Ó, Sala-Trull D, Rio-González AD, Pac-Sa MR, Sánchez-Urbano M, Satorres-Martinez P, Casanova-Suarez J, et al. Vitamin D Status and Incidence of SARS-CoV-2 Reinfections in the Borriana COVID-19 Cohort: A Population-Based Prospective Cohort Study. Tropical Medicine and Infectious Disease. 2025; 10(4):98. https://doi.org/10.3390/tropicalmed10040098
Chicago/Turabian StyleDomènech-Montoliu, Salvador, Laura López-Diago, Isabel Aleixandre-Gorriz, Óscar Pérez-Olaso, Diego Sala-Trull, Alba Del Rio-González, Maria Rosario Pac-Sa, Manuel Sánchez-Urbano, Paloma Satorres-Martinez, Juan Casanova-Suarez, and et al. 2025. "Vitamin D Status and Incidence of SARS-CoV-2 Reinfections in the Borriana COVID-19 Cohort: A Population-Based Prospective Cohort Study" Tropical Medicine and Infectious Disease 10, no. 4: 98. https://doi.org/10.3390/tropicalmed10040098
APA StyleDomènech-Montoliu, S., López-Diago, L., Aleixandre-Gorriz, I., Pérez-Olaso, Ó., Sala-Trull, D., Rio-González, A. D., Pac-Sa, M. R., Sánchez-Urbano, M., Satorres-Martinez, P., Casanova-Suarez, J., Notari-Rodriguez, C., Ruiz-Puig, R., Badenes-Marques, G., Aparisi-Esteve, L., Domènech-León, C., Romeu-Garcia, M. A., & Arnedo-Pena, A. (2025). Vitamin D Status and Incidence of SARS-CoV-2 Reinfections in the Borriana COVID-19 Cohort: A Population-Based Prospective Cohort Study. Tropical Medicine and Infectious Disease, 10(4), 98. https://doi.org/10.3390/tropicalmed10040098









