Fighting Dog-Mediated Rabies in Namibia—Implementation of a Rabies Elimination Program in the Northern Communal Areas
Abstract
:1. Introduction
2. Materials and Methods
2.1. Development and Implementation of a Rabies Control Strategy
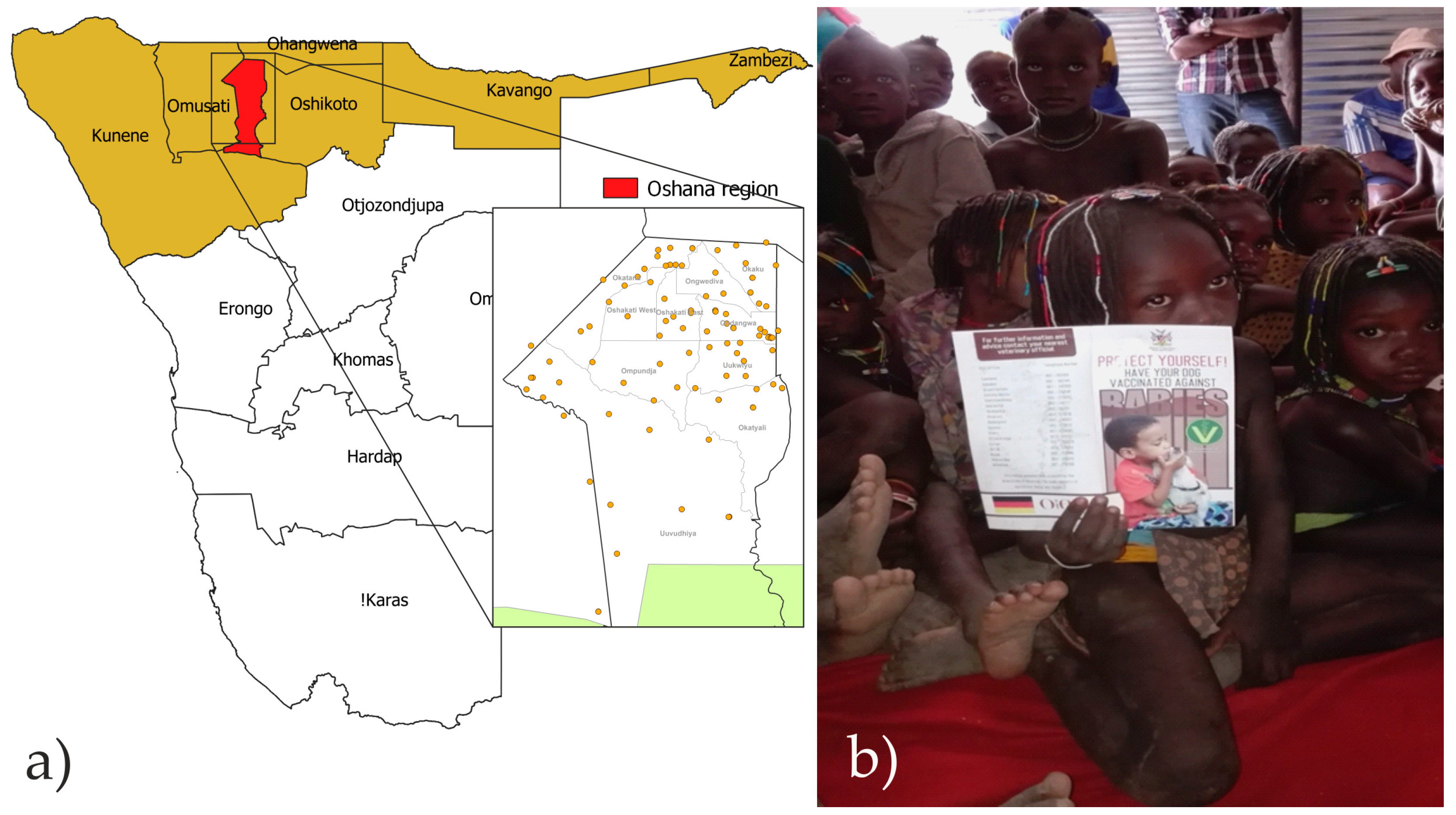
2.2. Program Areas and Implementation
2.3. Program Management
2.4. Awareness and Educational Campaigns
2.5. Training
2.6. Mass Dog Vaccination Campaigns
2.7. Rabies Surveillance and Diagnosis
3. Results
3.1. Pilot Project Phase
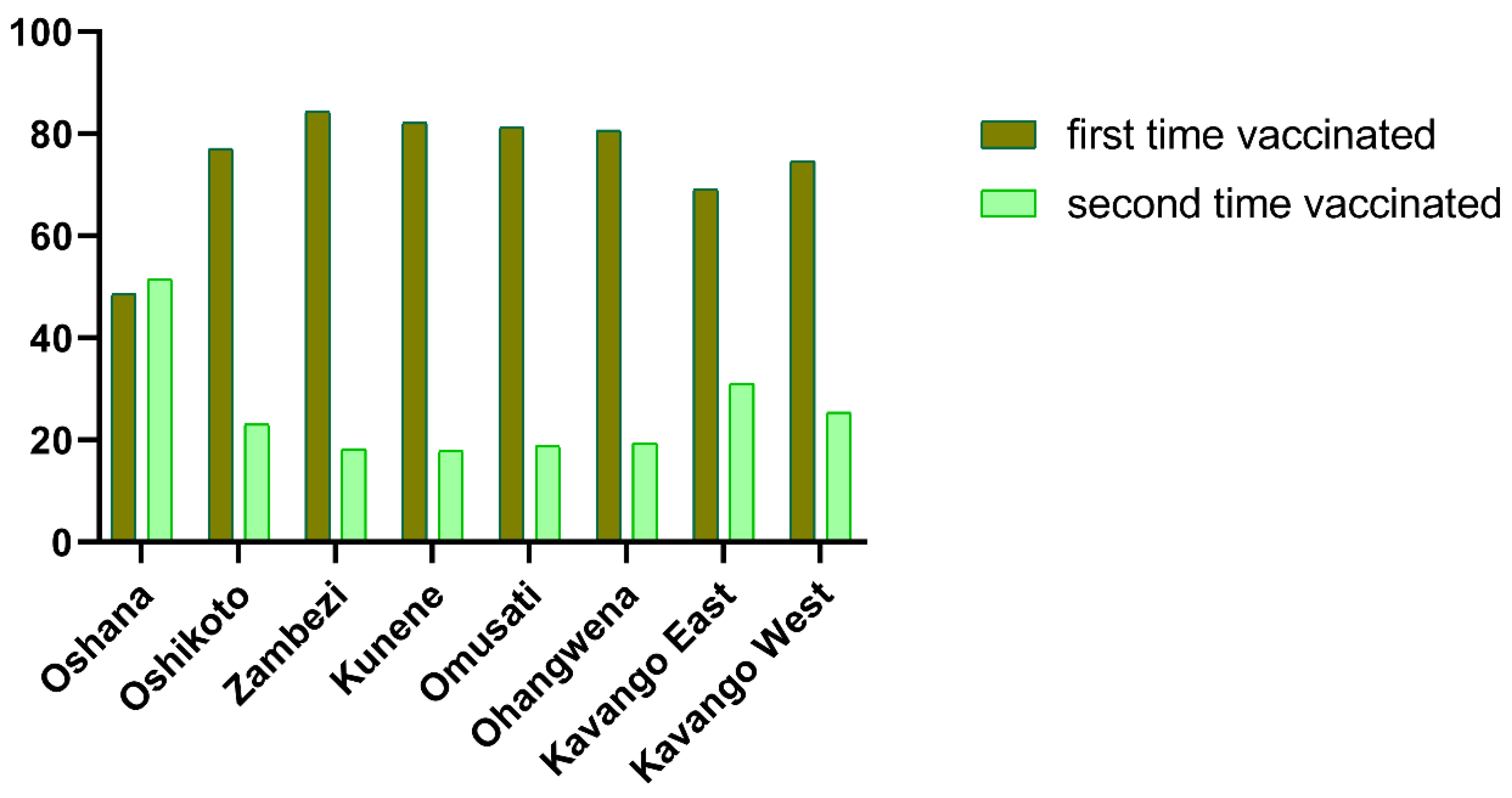
3.2. Rollout Phase
3.3. Rabies Surveillance
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. WHO Expert Consultation on Rabies, Third Report; World Health Organization: Geneva, Switzerland, 2018; Volume 1012, p. 195. [Google Scholar]
- Hampson, K.; Coudeville, L.; Lembo, T.; Sambo, M.; Kieffer, A.; Attlan, M.; Barrat, J.; Blanton, J.D.; Briggs, D.J.; Cleaveland, S.; et al. Estimating the global burden of endemic canine rabies. PLoS. Negl. Trop. Dis. 2015, 9, e0003709. [Google Scholar] [CrossRef] [Green Version]
- Fahrion, A.; Mikhailov, A.; Abela-Ridder, B.; Giacinti, J.; Harries, J. Human rabies transmitted by dogs: Current status of global data, 2015. Wkly. Epidemiol. Rec. 2016, 91, 13–20. [Google Scholar]
- Fahrion, A.S.; Taylor, L.H.; Torres, G.; Müller, T.; Durr, S.; Knopf, L.; de Balogh, K.; Nel, L.H.; Gordoncillo, M.J.; Abela-Ridder, B. The Road to Dog Rabies Control and Elimination-What Keeps Us from Moving Faster? Front. Public Health 2017, 5, 103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Müller, T.; Demetriou, P.; Moynagh, J.; Cliquet, F.; Fooks, A.R.; Conraths, F.J.; Mettenleiter, T.C.; Freuling, C.M. Rabies elimination in Europe—A success story. In Rabies Control—Towards Sustainable Prevention at the Source, Proceedings of the Compendium of the OIE Global Conference on Rabies Control, Seoul, Korea, 7–9 September 2011; Fooks, A.R., Müller, T., Eds.; OIE: Paris, France, 2012; pp. 31–44. [Google Scholar]
- Vigilato, M.A.; Clavijo, A.; Knobl, T.; Silva, H.M.; Cosivi, O.; Schneider, M.C.; Leanes, L.F.; Belotto, A.J.; Espinal, M.A. Progress towards eliminating canine rabies: Policies and perspectives from Latin America and the Caribbean. Philos. Trans. R. Soc. B Biol. Sci. 2013, 368, 20120143. [Google Scholar] [CrossRef]
- Velasco-Villa, A.; Escobar, L.E.; Sanchez, A.; Shi, M.; Streicker, D.G.; Gallardo-Romero, N.F.; Vargas-Pino, F.; Gutierrez-Cedillo, V.; Damon, I.; Emerson, G. Successful strategies implemented towards the elimination of canine rabies in the Western Hemisphere. Antivir. Res. 2017, 143, 1–12. [Google Scholar] [CrossRef]
- Shwiff, S.A.; Hatch, B.; Anderson, A.; Nel, L.H.; Leroux, K.; Stewart, D.; de Scally, M.; Govender, P.; Rupprecht, C.E. Towards Canine Rabies Elimination in KwaZulu-Natal, South Africa: Assessment of Health Economic Data. Transbound. Emerg. Dis. 2016, 63, 408–415. [Google Scholar] [CrossRef]
- Cleaveland, S.; Kaare, M.; Tiringa, P.; Mlengeya, T.; Barrat, J. A dog rabies vaccination campaign in rural Africa: Impact on the incidence of dog rabies and human dog-bite injuries. Vaccine 2003, 21, 1965–1973. [Google Scholar] [CrossRef]
- Hatch, B.; Anderson, A.; Sambo, M.; Maziku, M.; McHau, G.; Mbunda, E.; Mtema, Z.; Rupprecht, C.E.; Shwiff, S.A.; Nel, L. Towards Canine Rabies Elimination in South-Eastern Tanzania: Assessment of Health Economic Data. Transbound. Emerg. Dis. 2017, 64, 951–958. [Google Scholar] [CrossRef]
- Gibson, A.D.; Handel, I.G.; Shervell, K.; Roux, T.; Mayer, D.; Muyila, S.; Maruwo, G.B.; Nkhulungo, E.M.; Foster, R.A.; Chikungwa, P.; et al. The Vaccination of 35,000 Dogs in 20 Working Days Using Combined Static Point and Door-to-Door Methods in Blantyre, Malawi. PLoS Negl. Trop. Dis. 2016, 10, e0004824. [Google Scholar] [CrossRef] [Green Version]
- Lembo, T.; Hampson, K.; Kaare, M.T.; Ernest, E.; Knobel, D.; Kazwala, R.R.; Haydon, D.T.; Cleaveland, S. The feasibility of canine rabies elimination in Africa: Dispelling doubts with data. PLoS Negl. Trop. Dis. 2010, 4, e626. [Google Scholar] [CrossRef] [Green Version]
- Davlin, S.L.; Vonville, H.M. Canine rabies vaccination and domestic dog population characteristics in the developing world: A systematic review. Vaccine 2012, 30, 3492–3502. [Google Scholar] [CrossRef] [PubMed]
- Hikufe, E.H.; Freuling, C.M.; Athingo, R.; Shilongo, A.; Ndevaetela, E.-E.; Helao, M.; Shiindi, M.; Hassel, R.; Bishi, A.; Khaiseb, S.; et al. Ecology and epidemiology of rabies in humans, domestic animals and wildlife in Namibia, 2011–2017. PLoS Negl. Trop. Dis. 2019, 13, e0007355. [Google Scholar] [CrossRef] [PubMed]
- Scott, T.P.; Coetzer, A.; Nel, L.H. Rabies in Namibia, more than a horrendous disease: The social, environmental and economic challenges faced. In Handbook of Africa; Sherman, W., Ed.; Nova Science Publishers: Hauppauge, NY, USA, 2016; pp. 183–209. [Google Scholar]
- Schneider, H.P. Analyse der Tiergesundheitssituation in Südwestafrika/Namibia; Universität Giessen: Giessen, Germany, 1977. [Google Scholar]
- Hübschle, O.J. Rabies in the kudu antelope (Tragelaphus strepsiceros). Rev. Infect. Dis. 1988, 10, 629–633. [Google Scholar] [CrossRef] [PubMed]
- Swanepoel, R.; Barnard, B.J.; Meredith, C.D.; Bishop, G.C.; Bruckner, G.K.; Foggin, C.M.; Hubschle, O.J. Rabies in southern Africa. Onderstepoort J. Vet. Res. 1993, 60, 325–346. [Google Scholar] [PubMed]
- FAO/GARC. Developing a Stepwise Approach for Rabies Prevention and Control. In Proceedings of the FAO/GARC Workshop, Rome, Italy, 6–8 November 2012; FAO: Rome, Italy, 2013. [Google Scholar]
- Coetzer, A.; Kidane, A.H.; Bekele, M.; Hundera, A.D.; Pieracci, E.G.; Shiferaw, M.L.; Wallace, R.; Nel, L.H. The SARE tool for rabies control: Current experience in Ethiopia. Antivir. Res. 2016, 135, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Namibia Statistics Agency. Namibian Population Census 2011; Namibia Statistics Agency: Windhoek, Namiba, 2011. [Google Scholar]
- OIE. OIE Policy Paper on Vaccine Banks; OIE: Paris, France, 2018; p. 16. [Google Scholar]
- Mace, J.; Renaudin, S.; Dieuzy-Labaye, I.; Dehove, A. Vaccine banks for controlling dog-mediated rabies. Rev. Sci. Tech. 2018, 37, 511–518. [Google Scholar] [CrossRef]
- Dean, D.J.; Abelseth, M.K.; Athanasiu, P. The fluorescence antibody test. In Laboratory Techniques in Rabies, 4th ed.; Meslin, F.X., Kaplan, M.M., Koprowski, H., Eds.; World Health Organization: Geneva, Switzerland, 1996; pp. 88–93. [Google Scholar]
- Le Roux, K.; Nel, L. Local governments and municipalities and dog rabies control. In Proceedings of the Global Conference on Rabies Control, Towards Sustainable Prevention at the Source, Incheon, Korea, 7–9 September 2011; p. 37. [Google Scholar]
- Mpolya, E.A.; Lembo, T.; Lushasi, K.; Mancy, R.; Mbunda, E.M.; Makungu, S.; Maziku, M.; Sikana, L.; Jaswant, G.; Townsend, S.; et al. Toward Elimination of Dog-Mediated Human Rabies: Experiences from Implementing a Large-scale Demonstration Project in Southern Tanzania. Front. Vet. Sci. 2017, 4, 21. [Google Scholar] [CrossRef] [Green Version]
- Le Roux, K.; Stewart, D.; Perrett, K.D.; Nel, L.H.; Kessels, J.A.; Abela-Ridder, B. Rabies control in KwaZulu-Natal, South Africa. Bull. World Health Organ. 2018, 96, 360–365. [Google Scholar] [CrossRef]
- Evans, M.J.; Burdon Bailey, J.L.; Lohr, F.E.; Opira, W.; Migadde, M.; Gibson, A.D.; Handel, I.G.; Bronsvoort, B.M.D.; Mellanby, R.J.; Gamble, L.; et al. Implementation of high coverage mass rabies vaccination in rural Uganda using predominantly static point methodology. Vet. J. 2019, 249, 60–66. [Google Scholar] [CrossRef]
- Kasempimolporn, S.; Jitapunkul, S.; Sitprija, V. Moving towards the elimination of rabies in Thailand. J. Med. Assoc. Thail. 2008, 91, 433–437. [Google Scholar]
- Yang, D.K.; Kim, H.H.; Lee, K.K.; Yoo, J.Y.; Seomun, H.; Cho, I.S. Mass vaccination has led to the elimination of rabies since 2014 in South Korea. Clin. Exp. Vaccine Res. 2017, 6, 111–119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nguyen, H.T.T.; Nguyen, H.T.; Nguyen, T.T.T.; Urabe, M.I.; Pham, T.N.; Dang, A.D.; Afriyie, D.O.; Tran, D.N.; Otsu, S. Progress towards rabies control and elimination in Vietnam. Rev. Sci. Tech. 2019, 38, 199–212. [Google Scholar] [CrossRef] [PubMed]
- Wallace, R.M.; Mehal, J.; Nakazawa, Y.; Recuenco, S.; Bakamutumaho, B.; Osinubi, M.; Tugumizemu, V.; Blanton, J.D.; Gilbert, A.; Wamala, J. The impact of poverty on dog ownership and access to canine rabies vaccination: Results from a knowledge, attitudes and practices survey, Uganda 2013. Infect. Dis. Poverty 2017, 6, 97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lembo, T.; Partners for Rabies Prevention. The Blueprint for Rabies Prevention and Control: A Novel Operational Toolkit for Rabies Elimination. PLoS Negl. Trop. Dis. 2012, 6. [Google Scholar] [CrossRef] [Green Version]
- Gsell, A.; Knobel, D.; Kazwala, R.; Vounatsou, P.; Zinsstag, J. Domestic dog demographic structure and dynamics relevant to rabies control planning in urban areas in Africa: The case of Iringa, Tanzania. BMC Vet. Res. 2012, 8, 236. [Google Scholar] [CrossRef] [Green Version]
- Brooks, R. Survey of the Dog-Population of Zimbabwe and Its Level of Rabies Vaccination. Vet. Rec. 1990, 127, 592–596. [Google Scholar]
- Butler, J.R.; Bingham, J. Demography and dog-human relationships of the dog population in Zimbabwean communal lands. Vet. Rec. 2000, 147, 442–446. [Google Scholar] [CrossRef]
- De Balogh, K.K.; Wandeler, A.I.; Meslin, F.X. A dog ecology study in an urban and a semi-rural area of Zambia. Onderstepoort J. Vet. Res. 1993, 60, 437–443. [Google Scholar]
- Lechenne, M.; Oussiguere, A.; Naissengar, K.; Mindekem, R.; Mosimann, L.; Rives, G.; Hattendorf, J.; Moto, D.D.; Alfaroukh, I.O.; Zinsstag, J.; et al. Operational performance and analysis of two rabies vaccination campaigns in N’Djamena, Chad. Vaccine 2016, 34, 571–577. [Google Scholar] [CrossRef] [Green Version]
- Knobel, D.L.; Lembo, T.; Morters, M.; Townsend, S.E.; Cleaveland, S.; Hampson, K. Chapter 17—Dog Rabies and Its Control. In Rabies, 3rd ed.; Jackson, A.C., Ed.; Academic Press: Boston, MA, USA, 2013; pp. 591–615. [Google Scholar]
- Kaare, M.; Lembo, T.; Hampson, K.; Ernest, E.; Estes, A.; Mentzel, C.; Cleaveland, S. Rabies control in rural Africa: Evaluating strategies for effective domestic dog vaccination. Vaccine 2009, 27, 152–160. [Google Scholar] [CrossRef] [Green Version]
- Muthiani, Y.; Traore, A.; Mauti, S.; Zinsstag, J.; Hattendorf, J. Low coverage of central point vaccination against dog rabies in Bamako, Mali. Prev. Vet. Med. 2015, 120, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Gibson, A.D.; Ohal, P.; Shervell, K.; Handel, I.G.; Bronsvoort, B.M.; Mellanby, R.J.; Gamble, L. Vaccinate-assess-move method of mass canine rabies vaccination utilising mobile technology data collection in Ranchi, India. BMC Infect. Dis. 2015, 15, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gibson, A.D.; Mazeri, S.; Lohr, F.; Mayer, D.; Burdon Bailey, J.L.; Wallace, R.M.; Handel, I.G.; Shervell, K.; Bronsvoort, B.M.D.; Mellanby, R.J.; et al. One million dog vaccinations recorded on mHealth innovation used to direct teams in numerous rabies control campaigns. PLoS ONE 2018, 13, e0200942. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aanensen, D.M.; Huntley, D.M.; Menegazzo, M.; Powell, C.I.; Spratt, B.G. EpiCollect+: Linking smartphones to web applications for complex data collection projects. F1000Research 2014, 3, 199. [Google Scholar] [CrossRef] [PubMed]
- Coetzer, A.; Gwenhure, L.; Makaya, P.; Markotter, W.; Nel, L. Epidemiological aspects of the persistent transmission of rabies during an outbreak (2010–2017) in Harare, Zimbabwe. PLoS ONE 2019, 14, e0210018. [Google Scholar] [CrossRef] [PubMed]
- Scott, T.P.; Coetzer, A.; Fahrion, A.S.; Nel, L.H. Addressing the Disconnect between the Estimated, Reported, and True Rabies Data: The Development of a Regional African Rabies Bulletin. Front. Vet. Sci. 2017, 4, 18. [Google Scholar] [CrossRef] [Green Version]


| Region | Human Census 2011 | Area (km2) | Population Density (Persons/km2) | Estimated Pet Population 2016 # | Human:Pet Ratio # | Estimated Human:Dog Ratio | Dogs Vaccinated 2017 | Cats Vaccinated2017 | Vaccination Coverage ∞ |
|---|---|---|---|---|---|---|---|---|---|
| Kavango | 222,500 | 48,742 | 4.56 | 29,600 | 7.5 | 8.4 | 10,175 | 1310 | 39% |
| Kunene | 54,300 | 115,260 | 0.47 | 7100 | 7.6 | 8.5 | 4520 | 264 | 67% |
| Ohangwena | 245,100 | 10,706 | 22.89 | 27,800 | 8.8 | 9.8 | 17,349 | 1724 | 69% |
| Omusati | 242,900 | 26,551 | 9.15 | 34,700 | 7.0 | 7.8 | 33,549 | 2416 | 104% |
| Oshana | 174,900 | 8647 | 20.23 | 27,900 | 6.3 | 7.0 | 12,429 | 798 | 47% |
| Oshikoto | 161,900 | 38,685 | 4.19 | 23,100 | 7.0 | 7.8 | 14,902 | 3468 | 80% |
| Zambezi | 90,100 | 14,785 | 6.09 | 8600 | 10.5 | 11.6 | 6890 | 558 | 87% |
| total | 1,191,700 | 263,376 | 4.52 | 158,800 | 7.5 | 8.3 | 99,814 | 10,538 | 69% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Athingo, R.; Tenzin, T.; Shilongo, A.; Hikufe, E.; Shoombe, K.K.; Khaiseb, S.; van der Westhuizen, J.; Letshwenyo, M.; Torres, G.; Mettenleiter, T.C.; et al. Fighting Dog-Mediated Rabies in Namibia—Implementation of a Rabies Elimination Program in the Northern Communal Areas. Trop. Med. Infect. Dis. 2020, 5, 12. https://doi.org/10.3390/tropicalmed5010012
Athingo R, Tenzin T, Shilongo A, Hikufe E, Shoombe KK, Khaiseb S, van der Westhuizen J, Letshwenyo M, Torres G, Mettenleiter TC, et al. Fighting Dog-Mediated Rabies in Namibia—Implementation of a Rabies Elimination Program in the Northern Communal Areas. Tropical Medicine and Infectious Disease. 2020; 5(1):12. https://doi.org/10.3390/tropicalmed5010012
Chicago/Turabian StyleAthingo, Rauna, Tenzin Tenzin, Albertina Shilongo, Emmanuel Hikufe, Kenneth K. Shoombe, Siegfried Khaiseb, Jolandie van der Westhuizen, Moetapele Letshwenyo, Gregorio Torres, Thomas C. Mettenleiter, and et al. 2020. "Fighting Dog-Mediated Rabies in Namibia—Implementation of a Rabies Elimination Program in the Northern Communal Areas" Tropical Medicine and Infectious Disease 5, no. 1: 12. https://doi.org/10.3390/tropicalmed5010012





