A Systematic Review of Applications of Machine Learning and Other Soft Computing Techniques for the Diagnosis of Tropical Diseases
Abstract
1. Introduction
2. Related Works
- A.
- Soft-computing technologies used for disease diagnosis: The first effort at developing decision support tools for medical diagnosis started with the application of statistical techniques for medical diagnosis, introduced by Lipkin, Hardy, and Engle in the 1950s [15]. By the early 1970s, the ML tools created for medical diagnosis showed evidence that statistical tools were not capable of handling complex clinical problems [16]. They laid the foundation for exploring artificial intelligence (AI) concepts in medical diagnosis. This era began with Kulikowski’s exertions in 1970 [17], which were directed at deviating from engineering approaches to intense attention of the ‘cognitive model’. Kulikowski explored the physicians’ reasoning procedures and perception in medical diagnosis [18]. Pattern recognition techniques focused on the application of AI in medical diagnosis up until Shortliffe published the first rule-based method for therapy recommendation in infectious diseases in 1974 [19]. Rule-based programs utilize the “if-then rules” in series of inferences to make conclusions. However, it was later observed that rule-based systems were only effective in facile medical domains because most critical diagnostic problems were so extensive and convoluted. Forthright attempts to link together comparatively large series of rules resulted in significant difficulties; hence, such systems were deficient of clinical reasoning [20]. As research in the application of soft computing in medical diagnosis evolved, the attention shifted to the depiction and application of imprecise, dynamic, and unstructured knowledge. The sources of information obtainable in medical DSS are characterized with imprecision and uncertainty [21,22]. These sources comprise the physician, laboratory, patient and additional technical evaluation approaches, as well as the mathematical models that mimic the diagnostic process; thus, making medical DSS researchers turn to soft computing approaches to handle imprecision and uncertainty in medical diagnosis [23]. It has been shown in [24] that AI could significantly increase frontline health workers’ diagnostic effectiveness and efficiency, especially in rural communities. A few medical decision support models have attempted to provide diagnostic advice without a physician [25,26,27]. However, these systems are largely ineffective for diagnosing tropical febrile diseases due to: (i) soft focus on tropical conditions, (ii) poor handling of confusable symptoms, (iii) unfriendly user interfaces, (iv) high reliance on internet availability, and (v) non-consideration of asymptomatic factors.
- B.
- Tropical disease diagnosis using ML algorithms: The tropical zones of the world are more susceptible to infectious diseases than the temperate part of the world. The primary reasons why infectious diseases thrive in the tropics are due to biological and environmental influences that hold up a range of vectors, pathogens and hosts, and social drivers that weaken attempts to manage these diseases. These infectious diseases, also known as tropical diseases, are predominant in tropical regions [28]. Several tropical (especially febrile) diseases present symptoms that are very much alike, thus making these diseases “confusable.” These diseases are of immense concern to physicians, medical institutions, and the community as a whole due to the complexities of the conditions they present in early diagnosis and their mortality rates. Therefore, the use of soft computing and ML algorithms can help to prevent any misdiagnosis.
- Care management of febrile diseases
- Finding host relationships in the cell
- Diagnosing
3. Materials and Methods
3.1. Overview
- Planning the review:
- Identifying the need for a review.
- Specifying the research questions.
- Developing a review protocol.
- Evaluating the review protocol.
- Conducting the review:
- Identification of research.
- Selection of primary sources.
- Quality assessment.
- Data extraction and monitoring.
- Data synthesis, Meta-Analysis (MA)
3.2. Goal and Research Questions
- RQ 1—What soft computing techniques are adopted for tropical disease diagnosis?
- RQ 2—What types of diseases are current ML systems used for?
- RQ 3—What are the characteristics of the data used for validating tropical diseases?
- RQ 3.1—What are the common sample sizes used in the studies?
- RQ 3.2—What are the current demographic concentrations for ML systems?
- RQ 3.3—What are the geographical regions covered in the studies?
- RQ 3.4—Do the validation samples contain records of both patients and non-patients?
- RQ 3.5—Is the data publicly available?
- RQ 4—What features (symptoms and characteristics) have been used for each type of disease?
- RQ 5—How efficient are the algorithms relative to the specific diseases and symptoms; how predictive are these algorithms?
- RQ 6—What are the critical limitations reported in studies related to tropical diseases?
3.3. Article Selection
- Source selection and search keywords: This review employs the use of the following digital and grey libraries for the search results: (1) Google Scholar 1, (2) ACM Digital Library 2, (3) PubMed 3, (4) Science Direct 4, and (5) Digital Object Identifier (DOI) Registration Agency 5. These search engines have been used in other similar studies. We used the Publish and Perish [50] tool to extract the papers. We also manually searched for the other databases (such as ACM and Science Direct) that were not supported by Publish and Perish.
- 2.
- Application of inclusion/exclusion criteria:
- Relevance of the topic of each study to the tropical disease diagnosis concepts
- The level of comprehensiveness and evaluation followed in the study
- Whether the study was peer-reviewed
- Conference/poster abstract
- Duplicate instances of the same study
- Focus of the study does not answer RQs
- Focus is not ML for tropical disease
- Not written in English
3.4. Final Pool of Articles and the Online Repository
4. Results and Discussion
- A.
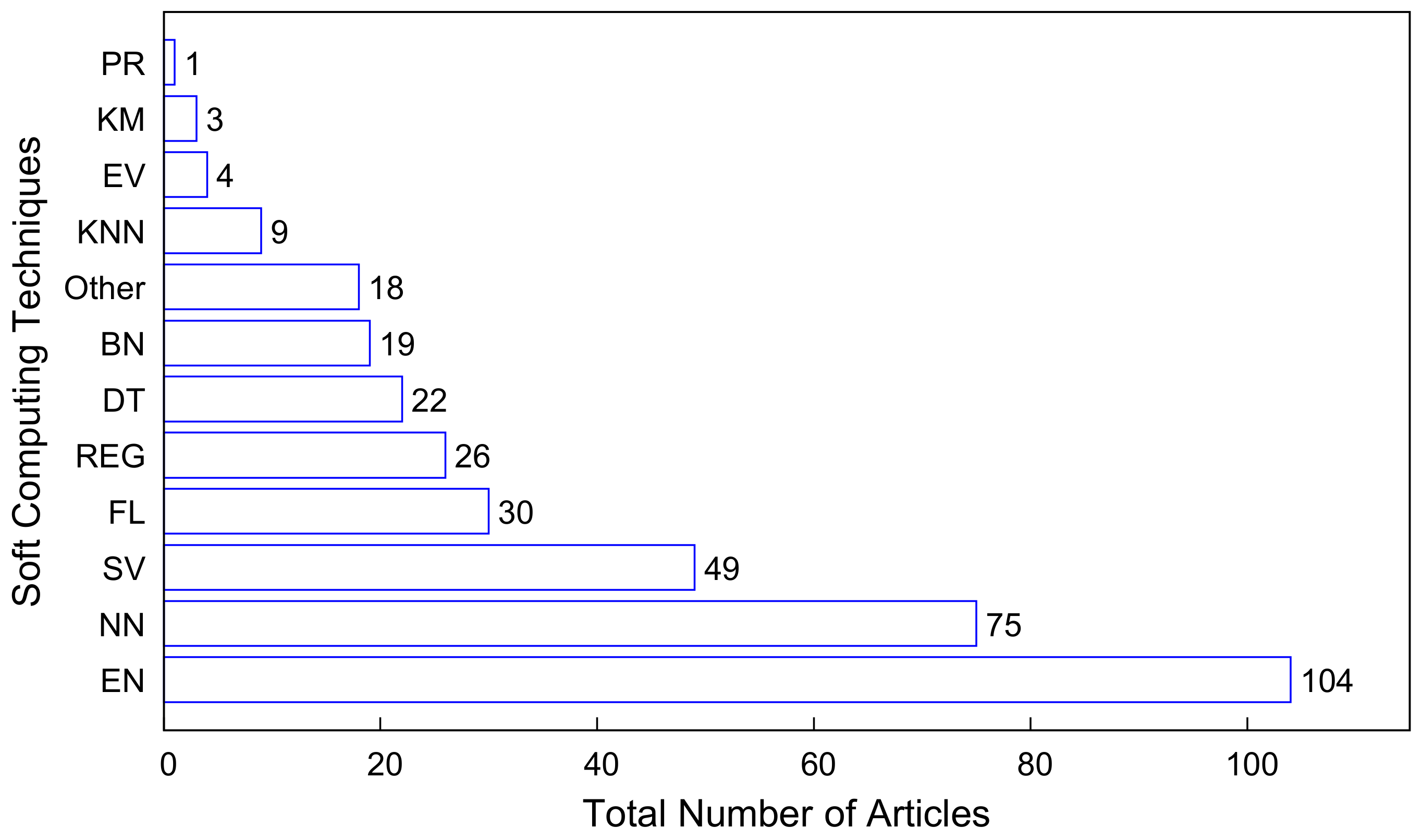
- RQ 1—What soft computing techniques are adopted to diagnose tropical diseases?
- B.
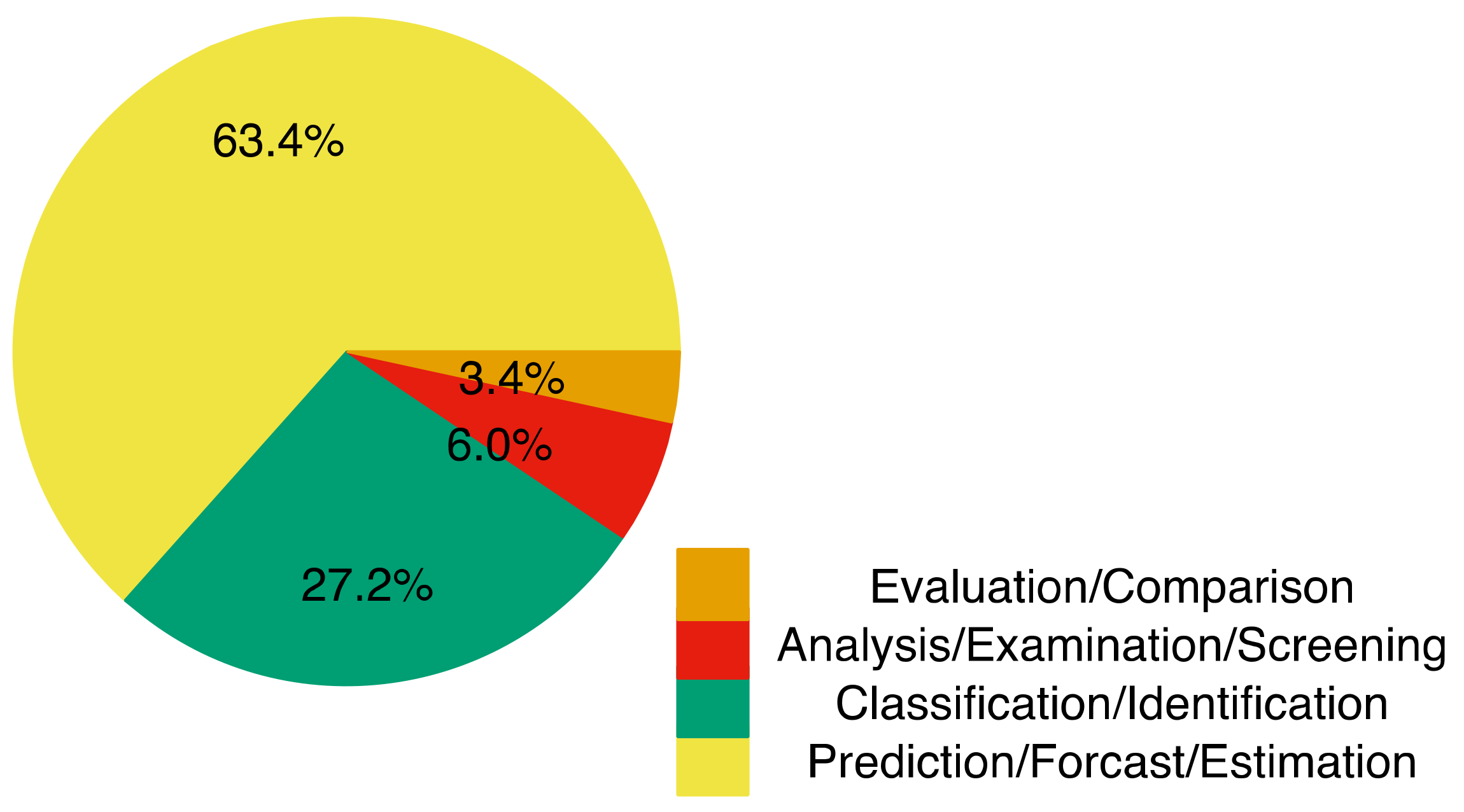
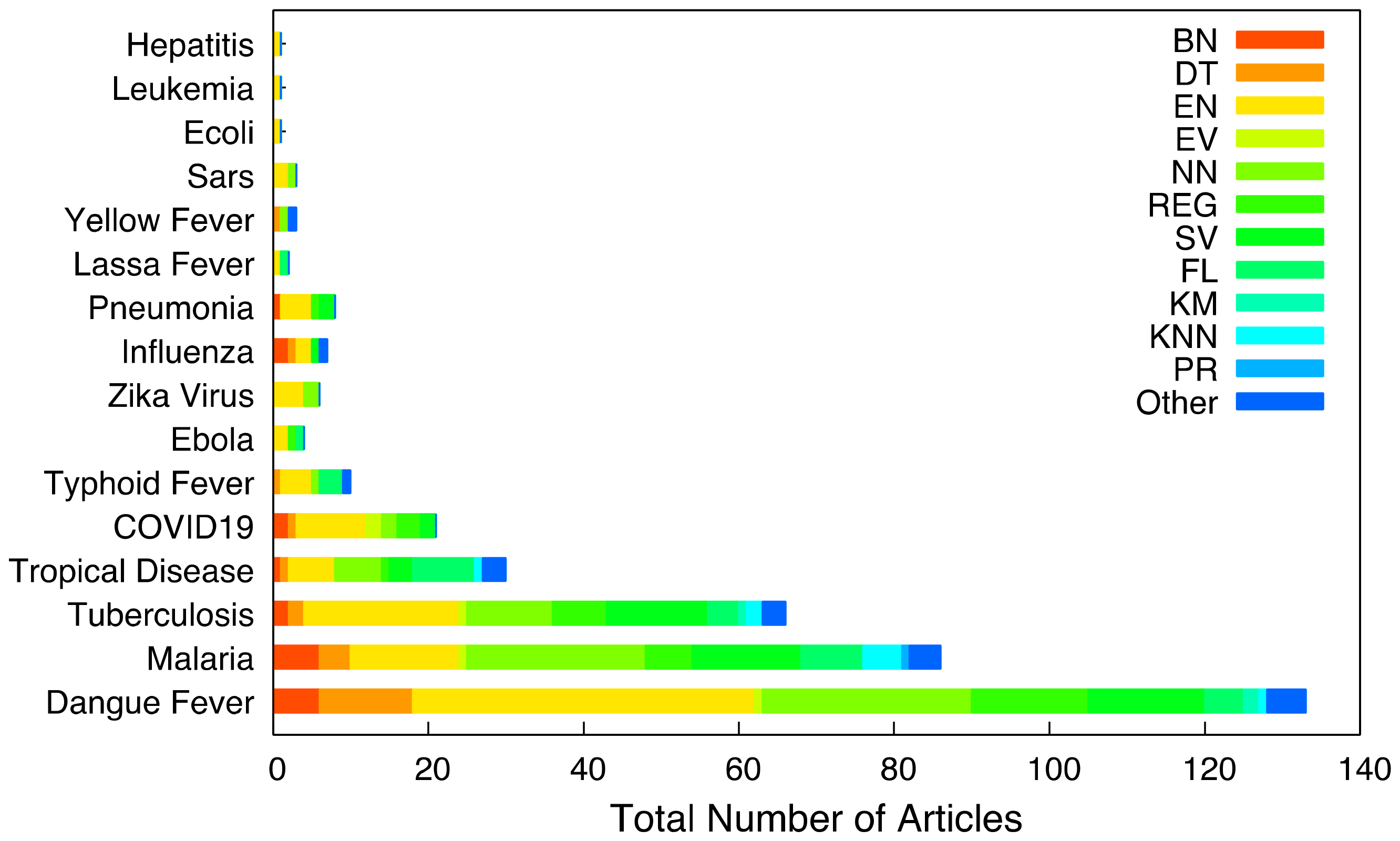
- RQ 2—What types of diseases are current ML systems used for?
- C.
- RQ 3—What are the characteristics of the data used for validating tropical diseases?
- RQ 3.1—What are the common sample sizes used in the studies?
- 2.
- RQ 3.2—What are the current demographic concentrations for ML systems?
- 3.
- RQ 3.3—What are the geographical regions covered in the studies?
- 4.
- RQ 3.4—Do the validation samples contain records of both positive and negative patients?
- 5.
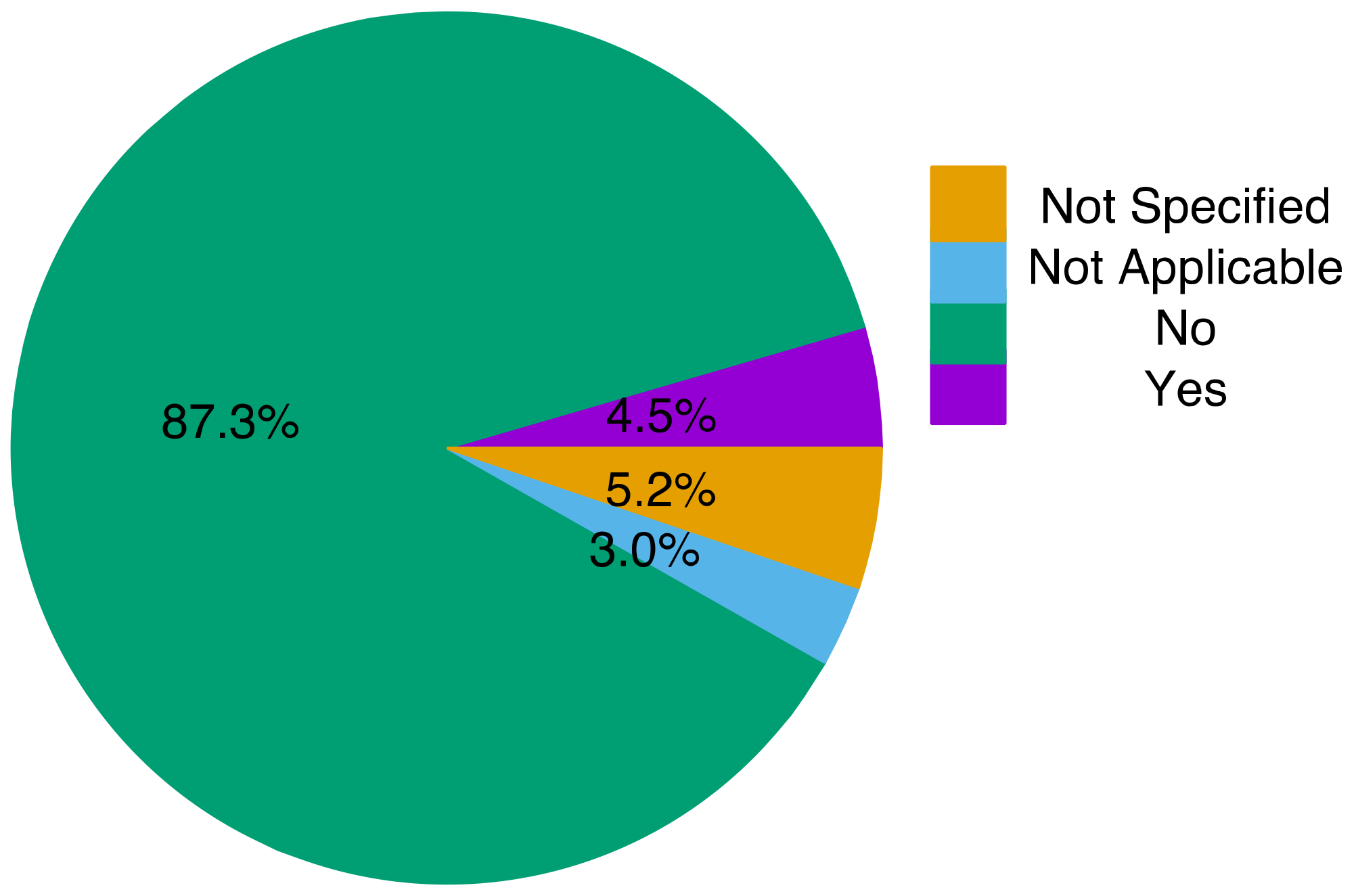
- RQ 3.5—Is the data publicly available?
- D.
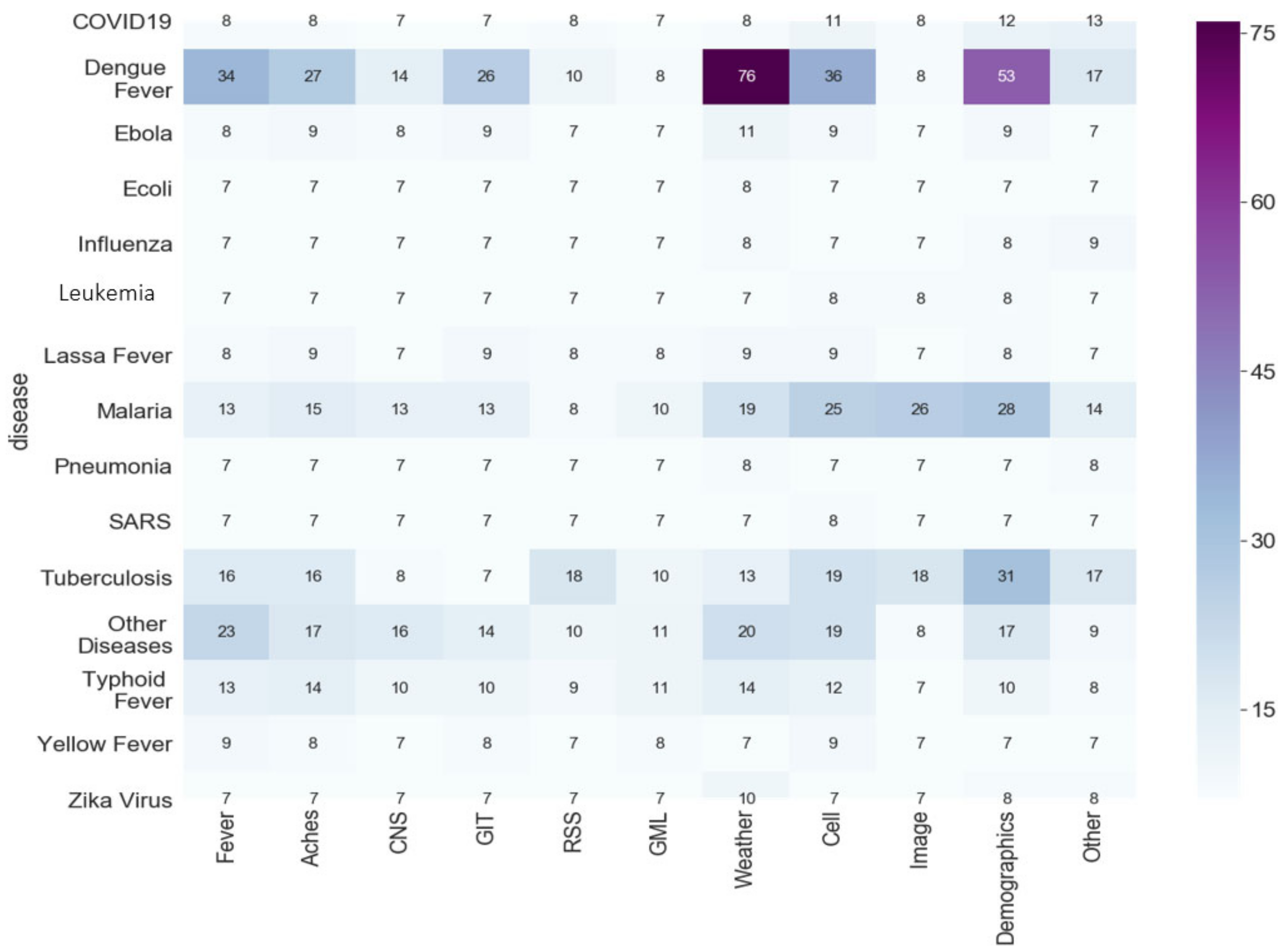
- RQ 4—What features (symptoms and characteristics) have been used for each type of disease?
- Symptomatic Features: 6 Symptomatic features were mainly included in the studies: Fever, Aches, Central Nervous System (CNS), Gastrointestinal Tract (GIT), Respiratory System (RSS), and General Malaise (GML). Among all of the studies, 69 included fever and 60 included ache-related features, whereas CNS, GIT, RSS and GML were included in 28, 17, 23 and 40 articles, respectively. Each subcategory is defined as follows:
- Febrile: Fever, Sweating, Shivering
- Aches: Headache, Muscle ache, Backache, Joint Pain
- CNS: Chills, Nausea, Delirium, Tiredness, Excessive Sleeping, Dizziness
- GIT: Vomiting, Diarrhea, Dehydration, Stomach Discomfort
- RSS: Abnormal Breathing, Coughing
- GML: Loss of Appetite, Yellowish Eyes, State of unwellness
- 2.
- Meteorological Features: Meteorological features mainly included humidity, rainfall, temperature, month, wind speed, altitude, and climate. Overall, 120 studies included weather data features.
- 3.
- Other Features: All other features are categorized as follows.
- Cell: Blood, Cell, URI, Hematocrit, Platelet, Protein, Gene, Genotype, Globulin, Albumin, and any other feature used in the body parts.
- Demographics: Age, Gender
- Image: Use of images of lungs as the input data and use of these image features to diagnose disease.
- Other: Any other features that could not be categorized into the mentioned categories
- E.
- RQ 5—How efficient are the algorithms relative to the specific diseases and symptoms; how predictive are these algorithms?
- F.
- RQ 6—What are the critical limitations reported in studies related to tropical diseases?
- Stated Limitations: Among all 268 papers, only 56 stated their work limitations. The following are the three main categories discussed throughout the papers:
- Data Limitation, which includes lack of resources due to resource-poor countries as well as small samples of data and image resolution for image-based models. According to Table 4, which shows the data size range used in the study, 14% of the articles used data sizes less than 101.
- Model Limitation which includes model parameter assumption, applying a single model on the dataset, is not generalizable, and focuses on the part of data features due to the model’s nature. Among 270 papers, 13% of the articles focused on some data features, and 29% used a single model for training. Given these limitations, we may conclude that the prediction results could be more generalizable if the papers used more data features. Additionally, as many articles suggested, considering different models, and predicting the results through different models can lead us to a better result. Therefore, considering more techniques can be suggested for improving model performance.
- Performance Limitation, which includes inconsistent model replication and case-dependent results. According to the performance metrics in Figure 13, 7% of the articles were categorized as “Not Specified” because those articles did not quantify the performance metric used. 5% of the articles were categorized as “Other” because some of the studies used custom metrics and other metrics that were used did not fall under the categories of ML performance metrics listed in the study.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zadeh, L.A. Fuzzy Logic, Neural Networks, and Soft Computing. Fuzzy Sets, Fuzzy Logic, and Fuzzy Systems: Selected Papers by Lotfi A Zadeh; World Scientific: Singapore, 1996; pp. 775–782. [Google Scholar]
- Ibrahim, D. An Overview of Soft Computing. Procedia Comput. Sci. 2016, 102, 34–38. [Google Scholar] [CrossRef]
- Yassin, N.I.; Omran, S.; Houby, E.M.; Allam, H. Machine learning techniques for breast cancer computer aided diagnosis using different image modalities: A systematic review. Comput. Methods Programs Biomed. 2018, 156, 25–45. [Google Scholar] [CrossRef] [PubMed]
- Martin-Isla, C.; Campello, V.M.; Izquierdo, C.; Raisi-Estabragh, Z.; Baeßler, B.; Petersen, S.E.; Lekadir, K. Image-Based Cardiac Diagnosis with Machine Learning: A Review. Front. Cardiovasc. Med. 2020, 7, 1. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, I.; Abdulazeez, A. The Role of Machine Learning Algorithms for Diagnosing Diseases. J. Appl. Sci. Technol. Trends 2021, 2, 10–19. [Google Scholar] [CrossRef]
- Samant, P.; Agarwal, R. Machine learning techniques for medical diagnosis of diabetes using iris images. Comput. Methods Programs Biomed. 2018, 157, 121–128. [Google Scholar] [CrossRef]
- Tumuluru, P.; Lakshmi, C.P.; Sahaja, T.; Prazna, R. A review of Machine Learning techniques for breast cancer diagnosis in medical applications. In Proceedings of the 2019 Third International Conference on I-SMAC (IoT in Social, Mobile, Analytics and Cloud) (I-SMAC), Palladam, India, 12–14 December 2019; pp. 618–623. [Google Scholar]
- Pham, D.T.; Afify, A.A. Machine-learning techniques and their applications in manufacturing. Proc. Inst. Mech. Eng. Part B J. Eng. Manuf. 2005, 219, 395–412. [Google Scholar] [CrossRef]
- Dieudonne, T. Faculty of Engineering and Technology. Ph.D. Thesis, University of Buea, Buea, Cameroon.
- Camargo, E.P. Tropical Diseases. Estud. Avançados 2008, 22, 95–110. [Google Scholar] [CrossRef]
- Pujara, P.; Parmar, M.; Rupakar, P.; Asawa, K.; Patel, S. An introduction to Tropical Disease: A review article. Int. J. Med. Microbiol. Trop. Dis. 2016, 2, 81–83. [Google Scholar] [CrossRef]
- Rupali, P. Introduction to Tropical Medicine. Infect. Dis. Clin. North Am. 2019, 33, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Zumla, A.; Ustianowski, A. Tropical diseases: Definition, geographic distribution, transmission, and classification. Infect. Dis. Clin. 2012, 26, 195–205. [Google Scholar] [CrossRef] [PubMed]
- Oyong, S.B.; Uzoka, F.-M.E.; Obot, U.O.; Ekong, E.E.; Ejodamen, P.U. Application of Soft Computing Techniques in The Diagnosis of Tropical Diseases: A Systematic Review. J. Trop. Dis. Public Health 2020, 8, 358. [Google Scholar]
- Kulikowski, C.A. Artificial intelligence in medicine: A personal retrospective on its emergence and early function. In Proceedings of the 1974 Annual ACM Conference—Volume 2 (ACM '74); Association for Computing Machinery: New York, NY, USA, 1987; p. 199. [Google Scholar] [CrossRef]
- Schwartz, W.B.; Gorry, G.; Kassirer, J.P.; Essig, A. Decision analysis and clinical judgment. Am. J. Med. 1973, 55, 459–472. [Google Scholar] [CrossRef] [PubMed]
- Kulikowski, C. Pattern Recognition Approach to Medical Diagnosis. IEEE Trans. Syst. Sci. Cybern. 1970, 6, 173–178. [Google Scholar] [CrossRef]
- Kulikowski, J.J.; Murray, I.J.; Parry, N.R. Human visual evoked potentials to chromatic and achromatic gratings. Clin. Vis. Sci. 1987, 1, 231–244. [Google Scholar]
- Shortliffe, E.H. A rule-based computer program for advising physicians regarding antimicrobial therapy selection. In Proceedings of the 1974 Annual ACM Conference—Volume 2; Association for Computing Machinery: New York, NY, USA, 1974; p. 739. [Google Scholar] [CrossRef]
- Szolovits, P.; Patil, R.S.; Schwartz, W.B. Artificial Intelligence in Medical Diagnosis. Ann. Intern. Med. 1988, 108, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Szolovits, P. Uncertainty and Decisions in Medical Informatics. Methods Inf. Med. 1995, 34, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Kaeding, A.K.; Flor, T. Processing unexact information in a medical used multiparadigm system. In Proceedings of the 1995 ACM Symposium on Applied Computing (SAC '95); Association for Computing Machinery: New York, NY, USA, 1995; pp. 590–592. [Google Scholar]
- Cohen, A.; Hegg, D.; De Michele, M.; Song, Q.; Kasabov, N. An intelligent controller for automated operation of sequencing batch reactors. Water Sci. Technol. 2003, 47, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Wallis, L.; Hasselberg, M.; Barkman, C.; Bogoch, I.; Broomhead, S.; Dumont, G.; Groenewald, J.; Lundin, J.; Bergendahl, J.N.; Nyasulu, P.; et al. A roadmap for the implementation of mHealth innovations for image-based diagnostic support in clinical and public-health settings: A focus on front-line health workers and health-system organizations. Glob. Health Action 2017, 10, 1340254. [Google Scholar] [CrossRef]
- Uzoka, F.-M.E.; Nwokoro, C.; Debele, F.; Akinnuwesi, B.; Olaniyan, M. AHP model for diagnosis of tropical confusable diseases. In Proceedings of the 2017 International Conference on Computational Science and Computational Intelligence (CSCI), Las Vegas, NV, USA, 14–16 December 2017; pp. 1758–1763. [Google Scholar] [CrossRef]
- Tsegay, G.; Anusuya, R. Decision Support Diagnosis System Using Artificial Neural Network and Fuzzy Logic Modeling in Case of Malaria. Artif. Intell. Syst. Mach. Learn. 2017, 9, 16–20. [Google Scholar]
- Akinnuwesi, B.A.; Adegbite, B.A.; Adelowo, F.; Ima-Edomwonyi, U.; Fashoto, G.; Amumeji, O.T. Decision support system for diagnosing rheumatic-musculoskeletal disease using fuzzy cognitive map technique. Inform. Med. Unlocked 2020, 18, 100279. [Google Scholar] [CrossRef]
- Meunier, Y.A. Tropical Diseases: A Practical Guide for Medical Practitioners and Students; Oxford University Press: Oxford, UK, 2013. [Google Scholar]
- Keitel, K.; D'Acremont, V. Electronic clinical decision algorithms for the integrated primary care management of febrile children in low-resource settings: Review of existing tools. Clin. Microbiol. Infect. 2018, 24, 845–855. [Google Scholar] [CrossRef]
- Agany, D.D.; Pietri, J.E.; Gnimpieba, E.Z. Assessment of vector-host-pathogen relationships using data mining and machine learning. Comput. Struct. Biotechnol. J. 2020, 18, 1704–1721. [Google Scholar] [CrossRef]
- Otambo, W.O.; Olumeh, J.O.; Ochwedo, K.O.; Magomere, E.O.; Debrah, I.; Ouma, C.; Onyango, P.; Atieli, H.; Mukabana, W.R.; Wang, C.; et al. Health care provider practices in diagnosis and treatment of malaria in rural communities in Kisumu County, Kenya. Malar. J. 2022, 21, 129. [Google Scholar] [CrossRef]
- Poostchi, M.; Silamut, K.; Maude, R.J.; Jaeger, S.; Thoma, G. Image analysis and machine learning for detecting malaria. Transl. Res. 2018, 194, 36–55. [Google Scholar] [CrossRef] [PubMed]
- Oguntimilehin, A.; Adetunmbi, A.O.; Abiola, O.B. A review of predictive models on diagnosis and treatment of malaria fever. Int. J. Comput. Sci. Mob. Comput. 2015, 4, 1087–1093. [Google Scholar]
- Boruah, I.; Kakoty, S. Analytical study of data mining applications in malaria prediction and diagnosis. Int. J. Comput. Sci. Mob. Comput. 2019, 8, 275–284. [Google Scholar]
- Roster, K.; Connaughton, C.; Rodrigues, F.A. Machine-Learning–Based Forecasting of Dengue Fever in Brazilian Cities Using Epidemiologic and Meteorological Variables. Am. J. Epidemiology 2022, 191, 1803–1812. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, N.; Islam, M. Machine learning for Dengue outbreak prediction: An outlook. Int. J. Adv. Res. Comput. Sci. 2017, 8, 93–102. [Google Scholar]
- Sundari, B.; Krishnamoorthy, M. Factors to Predict Dengue Fever using Data Mining Techniques: A Review. Int. J. Sci. Res. Eng. Dev. 2019, 2, 154–160. [Google Scholar]
- Sivaprasad, A.; Beevi, N.S.; Manojkumar, T. Dengue and Early Warning Systems: A review based on Social Network Analysis. Procedia Comput. Sci. 2020, 171, 253–262. [Google Scholar] [CrossRef]
- Ahmed, N.; Shoaib, M.; Ishaq, A.; Wahab, A. Role of Expert Systems in Identification and Overcoming of Dengue Fever. Int. J. Adv. Comput. Sci. Appl. 2017, 8, 10. [Google Scholar] [CrossRef][Green Version]
- Gill, C.M.; Dolan, L.; Piggott, L.M.; McLaughlin, A.M. New developments in tuberculosis diagnosis and treatment. Breathe 2022, 18, 210149. [Google Scholar] [CrossRef]
- Weiner, J.; Kaufmann, S.H. High-throughput and computational approaches for diagnostic and prognostic host tuberculosis biomarkers. Int. J. Infect. Dis. 2017, 56, 258–262. [Google Scholar] [CrossRef]
- Doshi, R.; Falzon, D.; Thomas, B.V.; Temesgen, Z.; Sadasivan, L.; Migliori, G.B.; Raviglione, M. Tuberculosis control, and the where and why of artificial intelligence. ERJ Open Res. 2017, 3, 00056–02017. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.L.; Espinoza, L.M.; Vannice, K.S.; Tadesse, B.T.; Owusu-Dabo, E.; Rakotozandrindrainy, R.; Jani, I.V.; Teferi, M.; Soura, A.B.; Lunguya, O.; et al. The Burden of Typhoid Fever in Sub-Saharan Africa: A Perspective. Res. Rep. Trop. Med. 2022, 13, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Oguntimilehin, A.; Abiola, O.B.; Olatunji, K.A. Computer aided diagnostic systems for managing typhoid fever: A review of diagnosis techniques. Int. J. Comput. Appl. 2015, 126, 6. [Google Scholar]
- Akinsolu, F.T.; Nemieboka, P.O.; Njuguna, D.W.; Ahadji, M.N.; Dezso, D.; Varga, O. Emerging resistance of neglected tropical diseases: A scoping review of the literature. Int. J. Environ. Res. Public Health 2019, 16, 1925. [Google Scholar] [CrossRef] [PubMed]
- Boyce, M.R.; Katz, R.; Standley, C.J. Risk factors for infectious diseases in urban environments of sub-Saharan Africa: A systematic review and critical appraisal of evidence. Trop. Med. Infect. Dis. 2019, 4, 123. [Google Scholar] [CrossRef] [PubMed]
- Elduma, A.H.; LaBeaud, A.D.A.; Plante, J.; Plante, K.S.; Ahmed, A. High seroprevalence of dengue virus infection in Sudan: Systematic review and meta-analysis. Trop. Med. Infect. Dis. 2020, 5, 120. [Google Scholar] [CrossRef] [PubMed]
- Kitchenham, B.; Charters, S. Guidelines for Performing Systematic Literature Reviews in Software Engineering; 2007. Available online: https://www.researchgate.net/profile/Barbara-Kitchenham/publication/302924724_Guidelines_for_performing_Systematic_Literature_Reviews_in_Software_Engineering/links/61712932766c4a211c03a6f7/Guidelines-for-performing-Systematic-Literature-Reviews-in-Software-Engineering.pdf (accessed on 25 November 2022).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef]
- Harzing, A.W. The Publish or Perish Book; Tarma Software Research Pty Limited: London, UK, 2010. [Google Scholar]
- Reddy, G.T.; Bhattacharya, S.; Ramakrishnan, S.S.; Chowdhary, C.L.; Hakak, S.; Kaluri, R.; Reddy, M.P. An ensemble base machine-learning model for diabetic retinopathy classification. In Proceedings of the 2020 International Conference on Emerging Trends in Information Technology and Engineering (ic-ETITE), Vellore, India, 24–25 February 2020; pp. 1–6. [Google Scholar]
- Atallah, R.; Al-Mousa, A. Heart disease detection using machine learning majority voting ensemble method. In Proceedings of the 2019 2nd International Conference on New Trends in Computing Sciences (ictcs), Amman, Jordan, 9–11 October 2019; pp. 1–6. [Google Scholar]
- Zhang, Z.; Beck, M.W.; Winkler, D.A.; Huang, B.; Sibanda, W.; Goyal, H. Opening the black box of neural networks: Methods for interpreting neural network models in clinical applications. Ann. Transl. Med. 2018, 6, 216. [Google Scholar] [CrossRef]
- Vairale, V.S.; Shukla, S. Classification of Hypothyroid Disorder using Optimized SVM Method. In Proceedings of the 2019 International Conference on Smart Systems and Inventive Technology (ICSSIT), Tirunelveli, India, 27–29 November 2019; pp. 258–263. [Google Scholar]
- Iqbal, N.; Islam, M. Machine learning for dengue outbreak prediction: A performance evaluation of different prominent classifiers. Informatica 2019, 43, 1548. [Google Scholar] [CrossRef]
- Amadin, F.I.; Bello, M.E. Prediction of yellow fever using multilayer perceptron neural network classifier. J. Emerg. Trends Eng. Appl. Sci. 2018, 9, 282–286. [Google Scholar]
- Adeyemo, O.O.; Adeyeye, T.O.; Ogunbiyi, D. Comparative study of ID3/C4. 5 decision tree and multilayer perceptron algorithms for the prediction of typhoid fever. Afr. J. Comput. ICT 2015, 8, 103–112. [Google Scholar]
- Farooqi, W.; Ali, S.; Wahab, A. Classification of Dengue fever using decision tree. VAWKUM Trans. Comput. Sci. 2014, 3, 15–22. [Google Scholar]
- Nordin, N.I.; Sobri, N.M.; Ismail, N.A.; Zulkifli, S.N.; Abd Razak, N.F.; Mahmud, M. The classification performance using support vector machine for endemic dengue cases. J. Phys. Conf. Ser. 2020, 1496, 012006. [Google Scholar] [CrossRef]
- Rosnelly, R.; Wahyuni, L. Tropical Diseases Identification Using Neural Network Adaptive Resonance Theory 2. In Proceedings of the 2018 6th International Conference on Cyber and IT Service Management (CITSM), Parapat, Indonesia, 7–9 August 2018; pp. 1–4. [Google Scholar] [CrossRef]
- Yang, X.; Kumagai, K.; Sun, G.; Ishibashi, K.; Trung, N.V.; Van Kinh, N. Dengue fever screening using vital signs by contactless microwave radar and machine learning. In Proceedings of the 2019 IEEE Sensors Applications Symposium (SAS), Sophia Antipolis, France, 11–13 March 2019; pp. 1–6. [Google Scholar] [CrossRef]
- Lenka, R.; Dutta, K.; Khandual, A.; Nayak, S.R. Bio-medical image processing: Medical image analysis for malaria with deep learning. In Examining Fractal Image Processing and Analysis; IGI Global: Hershey, PA, USA, 2020; pp. 158–169. [Google Scholar] [CrossRef]
- Song, S.H.; Choi, Y.; Yoon, T. Comparison of episodes of mosquito-borne disease: Dengue, yellow fever, west Nile, and filariasis with decision tree, apriori algorithm. In Proceedings of the 2016 18th International Conference on Advanced Communication Technology (ICACT), PyeongChang, Republic of Korea, 31 January–3 February 2016; pp. 455–458. [Google Scholar] [CrossRef]
- Sedor, K. The Law of Large Numbers and Its Applications; Lakehead University: Thunder Bay, ON, Canada, 2015. [Google Scholar]
- Kim, S.-Y. Effects of sample size on robustness and prediction accuracy of a prognostic gene signature. BMC Bioinform. 2009, 10, 147. [Google Scholar] [CrossRef] [PubMed]
- Ajiboye, A.R.; Arshah, R.A.; Qin, H.; Isah-Kebbe, H. Evaluating the effect of dataset size on predictive model using supervised learning technique. Int. J. Softw. Eng. Comput. Syst. 2015, 1, 75–84. [Google Scholar] [CrossRef]
- Figueroa, R.L.; Zeng-Treitler, Q.; Kandula, S.; Ngo, L.H. Predicting Sample Size Required for Classification Performance. BMC Med. Inform. Decis. Mak. 2012, 12, 8. [Google Scholar] [CrossRef] [PubMed]
- Rácz, A.; Bajusz, D.; Héberger, K. Effect of dataset size and train/test split ratios in QSAR/QSPR multiclass classification. Molecules 2021, 26, 1111. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Fan, E.; Wang, P. Comparative analysis of image classification algorithms based on traditional machine learning and deep learning. Pattern Recognit. Lett. 2021, 141, 61–67. [Google Scholar] [CrossRef]
- Díaz, A.; Beleña, Á.; Zueco, J. The Role of Age and Gender in Perceived Vulnerability to Infectious Diseases. Int. J. Environ. Res. Public Health 2020, 17, 485. [Google Scholar] [CrossRef]
- Vera Cruz, G.; Bucourt, E.; Réveillère, C.; Martaillé, V.; Juncker-Vannier, I.; Goupille, P.; Mulleman, D.; Courtois, R. Machine learning reveals the most important psychological and social variables predicting the differential diagnosis of rheumatic and musculoskeletal diseases. Rheumatol. Int. 2022, 42, 1053–1062. [Google Scholar] [CrossRef] [PubMed]
- Asare, K.O.; Terhorst, Y.; Vega, J.; Peltonen, E.; Lagerspetz, E.; Ferreira, D. Predicting Depression from Smartphone Behavioral Markers Using Machine Learning Methods, Hyperparameter Optimization, and Feature Importance Analysis: Exploratory Study. JMIR mHealth uHealth 2021, 9, e26540. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Berger, N.A.; Xu, R. Analyses of Risk, Racial Disparity, and Outcomes Among US Patients with Cancer and COVID-19 Infection. JAMA Oncol. 2021, 7, 220. [Google Scholar] [CrossRef] [PubMed]
- Pourhomayoun, M.; Shakib, M. Predicting mortality risk in patients with COVID-19 using machine learning to help medical decision-making. Smart Health 2021, 20, 100178. [Google Scholar] [CrossRef]
- World Health Organization. Statistics. List of Who Regions. Available online: https://www.who.int/countries (accessed on 25 November 2022).
- Dessie, T.; Jemal, M.; Maru, M.; Tiruneh, M. Multiresistant Bacterial Pathogens Causing Bacterial Pneumonia and Analyses of Potential Risk Factors from Northeast Ethiopia. Int. J. Microbiol. 2021, 2021, 6680343. [Google Scholar] [CrossRef] [PubMed]
- Ticona, J.H.; Zaccone, V.M.; McFarlane, I.M. Community-acquired pneumonia: A focused review. Am. J. Med. Case Rep. 2021, 9, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Bielicki, J.A.; Stöhr, W.; Barratt, S.; Dunn, D.; Naufal, N.; Roland, D.; Sturgeon, K.; Finn, A.; Rodriguez-Ruiz, J.P.; Malhotra-Kumar, S.; et al. Effect of amoxicillin dose and treatment duration on the need for antibiotic Re-treatment in children with community-acquired pneumonia: The CAP-IT randomized clinical trial. JAMA 2021, 326, 1713–1724. [Google Scholar] [CrossRef] [PubMed]
- Mahesh, B. Machine learning algorithms—A review. Int. J. Sci. Res. (IJSR) 2020, 9, 381–386. [Google Scholar]
- Wu, C.C.; Yeh, W.C.; Hsu, W.D.; Islam, M.M.; Nguyen, P.A.; Poly, T.N.; Wang, Y.C.; Yang, H.C.; Li, Y.C. Prediction of fatty liver disease using machine learning algorithms. Comput. Methods Programs Biomed. 2019, 170, 23–29. [Google Scholar] [CrossRef]
- Li, J.P.; Haq, A.U.; Din, S.U.; Khan, J.; Khan, A.; Saboor, A. Heart disease identification method using machine learning classification in e-healthcare. IEEE Access 2020, 8, 107562–107582. [Google Scholar] [CrossRef]
- Luque, A.; Carrasco, A.; Martín, A.; de Las Heras, A. The impact of class imbalance in classification performance metrics based on the binary confusion matrix. Pattern Recognit. 2019, 91, 216–231. [Google Scholar] [CrossRef]
- Nadda, W.; Boonchieng, W.; Boonchieng, E. Weighted extreme learning machine for dengue detection with class-imbalance classification. In Proceedings of the 2019 IEEE Healthcare Innovations and Point of Care Technologies, (HI-POCT), Bethesda, MD, USA, 20–22 November 2019; pp. 151–154. [Google Scholar] [CrossRef]
- Jeon, J.; Joo, Y.; Yoon, T. Finding difference between west and east yellow fever by apriori and decision tree. J. Data Min. Knowl. Manag. Process 2018, 8, 6. [Google Scholar]
- Siriyasatien, P.; Phumee, A.; Ongruk, P.; Jampachaisri, K.; Kesorn, K. Analysis of significant factors for dengue fever incidence prediction. BMC Bioinform. 2016, 17, 166. [Google Scholar] [CrossRef]
- Hossin, M.; Sulaiman, M.N. A review on evaluation metrics for data classification evaluations. Int. J. Data Min. Knowl. Manag. Process 2015, 5, 1–11. [Google Scholar]
- Liu, Y.; Zhou, Y.; Wen, S.; Tang, C. A Strategy on Selecting Performance Metrics for Classifier Evaluation. Int. J. Mob. Comput. Multimedia Commun. 2014, 6, 20–35. [Google Scholar] [CrossRef]
- Hossin, M.; Sulaiman, M.N.; Mustapha, A.; Mustapha, N.; Rahmat, R.W. A hybrid evaluation metric for optimizing classifier. In Proceedings of the 2011 3rd Conference on Data Mining and Optimization (DMO), Putrajaya, Malaysia, 28–29 June 2011; pp. 165–170. [Google Scholar] [CrossRef]
- Chawla, N.V.; Japkowicz, N.; Kotcz, A. Special issue on learning from imbalanced data sets. ACM SIGKDD Explor. Newsl. 2004, 6, 1–6. [Google Scholar] [CrossRef]
- Ranawana, R.; Palade, V. Optimized precision-a new measure for classifier performance evaluation. In Proceedings of the 2006 IEEE International Conference on Evolutionary Computation, Vancouver, BC, Canada, 16–21 July 2006; pp. 2254–2261. [Google Scholar] [CrossRef]
- Akobeng, A.K. Understanding diagnostic tests 2: Likelihood ratios, pre- and post-test probabilities and their use in clinical practice. Acta Paediatr. 2007, 96, 487–491. [Google Scholar] [CrossRef] [PubMed]
- Trevethan, R. Sensitivity, Specificity, and Predictive Values: Foundations, Pliabilities, and Pitfalls in Research and Practice. Front. Public Health 2017, 5, 307. [Google Scholar] [CrossRef] [PubMed]
- Letcher, T. Comprehensive Renewable Energy; Elsevier Ltd.: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Willmott, C.J.; Matsuura, K. Advantages of the mean absolute error (MAE) over the root mean square error (RMSE) in assessing average model performance. Clim. Res. 2005, 30, 79–82. [Google Scholar] [CrossRef]
- Chai, T.; Draxler, R.R. Root mean square error (RMSE) or mean absolute error (MAE)?—Arguments against avoiding RMSE in the literature. Geosci. Model Dev. 2014, 7, 1247–1250. [Google Scholar] [CrossRef]
- Pourhoseingholi, M.A.; Vahedi, M.; Rahimzadeh, M. Sample size calculation in medical studies. Gastroenterol. Hepatol. Bed Bench 2013, 6, 14. [Google Scholar] [PubMed]








| (“Machine learning” OR “Computer-aided” OR “Neural Network” OR “Fuzzy Logic”) AND (Tropical OR Neglected) AND (Febrile OR Fever) (“Machine learning” OR “Soft Computing” OR “Decision Tree” OR “Decision Support System”) AND (Tropical OR Neglected) AND (Febrile OR Fever) (“Machine learning”) AND (“Yellow fever” OR “Dengue fever” OR “AIDS” OR “Ebola” OR “Marburg virus” OR “Lassa fever” OR “Measles” OR “Rubella (German Measles)”) (“Machine learning”) AND (“Meningococcal infection” OR “Leptospirosis” OR “Melioidosis” OR “Escherichia coli” OR “Tuberculosis” OR “Hansen’s disease” OR “Malaria” OR “Cerebral malaria”) (“Machine learning”) AND (“Hantavirus” OR “H1N1” OR “Encephalitis” OR “Meningitis” OR “Cholera” OR “Scrub typhus” OR “Typhoid fever” OR “Rickettsia infections”) (“Machine learning”) AND (“Leishmaniasis” OR “Schistosomiasis”) (“Machine learning”) AND (“Diagnosis” OR “Consultation” OR “Assessment”) AND (Tropical OR Neglected) AND (Febrile OR Fever) AND (“Symptoms”) (“Machine learning”) AND (“Information” OR “Record” OR “Informatics”) AND (Tropical OR Neglected) AND (Febrile OR Fever) AND (“Symptoms”) (“Machine learning”) AND (“Performance” OR “Effectiveness” OR “Efficiency”) AND (Tropical OR Neglected) AND (Febrile OR Fever) AND (“Signs”) |
| Database | Articles |
|---|---|
| Google Scholar | 2130 |
| ACM | 1924 |
| Science Direct | 1600 |
| PubMed | 733 |
| CrossRef | 400 |
| Total | 6787 |
| Year | Total of Papers |
|---|---|
| 2010 | 6 |
| 2011 | 13 |
| 2012 | 11 |
| 2013 | 15 |
| 2014 | 9 |
| 2015 | 21 |
| 2016 | 25 |
| 2017 | 33 |
| 2018 | 46 |
| 2019 | 41 |
| 2020 | 40 |
| Sample Size | Frequency |
|---|---|
| 1–30 | 9 |
| 31–100 | 27 |
| 101–1000 | 68 |
| 1001–5000 | 37 |
| 5001–10,000 | 14 |
| Above 10,000 | 25 |
| Not Specified | 88 |
| Demographic | Frequency (%) |
|---|---|
| Age | 11 |
| Gender | 5.6 |
| Time Frame | 6.3 |
| Not Specified | 77 |
| Region | Countries |
|---|---|
| African Region (AFRO) | Nigeria, South Africa, Gambia, Uganda, Tanzania, Ethiopia, Central African Republic, Zambia, Madagascar, Sierra Leone, Ghana, Senegal, Liberia. |
| Region of the Americas (PHOTO) | United States, Brazil, Colombia, Peru, Venezuela, Ecuador, Canada, Paraguay, Mexico. |
| South-East Asia Region (SEARS) | India, Indonesia, Thailand, Bangladesh, Sri Lanka |
| European Region (EURO) | Turkey, Portugal, Kazakhstan, Israel, Finland, Moldova, Germany, Azerbaijan, Romania, Belarus, Georgia. |
| Eastern Mediterranean Region (MORE) | Pakistan, Sudan, Iran |
| Western Pacific Region (WPRO) | China, Malaysia, Singapore, Taiwan, Vietnam, South Korea, Cambodia, Philippines, Japan |
| Disease | Year | Total Number of Cases (Million) | Papers |
|---|---|---|---|
| Malaria | 2019 | 229 | 49 |
| Typhoid fever | 2019 | 21 | 9 |
| Dengue | 2019 | 4.2 | 107 |
| Tuberculosis | 2019 | 10 | 43 |
| HIV | 2019 | 38 | 0 |
| Leukemia | 2016 | 60.3 | 1 |
| Pneumonia | 2019 | 150.7 | 2 |
| Ebola | 2016 | 28.616 | 4 |
| COVID 19 | 2020 | 103.7 | 13 |
| SARS | 2003 | 8.096 | 1 |
| Hepatitis B | 2015 | 257 | 1 |
| Hepatitis C | 2015 | 71 | 0 |
| Zika Virus | 2018 | 1.8 | 4 |
| Feature | Used Features | Total Features |
|---|---|---|
| Fever | 69 | 69 |
| Aches | 60 | 60 |
| CNS | 27 | 27 |
| GML | 17 | 17 |
| RSS | 22 | 22 |
| GIT | 40 | 40 |
| Weather | 120 | 120 |
| Image | 34 | 36 |
| Demographics | 115 | 119 |
| Cell | 88 | 91 |
| Other | 40 | 40 |
| Performance Metrics | Techniques | Frequency | The Efficiency of the Algorithms |
|---|---|---|---|
| Accuracy (ACC) | BN, EN, FL, DT, NN, SV, EV, KNN, REG, Other | 47.8% | 85% of the studies had 75–100% accuracy, 13% of the studies had 51–74% accuracy and 2% of the studies had accuracy below 50% |
| Specificity (SPE) | BN, PR, NN, EN, REG, SV, KNN | 14.6% | 89% of the studies had specificity of 75% and above while the remaining two studies had specificity of 69% and 12%, respectively |
| Not Specified | FL, EN, BN, KM, NN, SV | 7.3% | N/A |
| Sensitivity (SEN) | SV, EN, NN, KNN, BN, REG, DT, PR | 6.7% | 94% of the studies had sensitivity of 75% and above while the remaining 6% of the study had a sensitivity of between 69 and 72% |
| Root Mean Square Error (RMSE) | EN, REG, EN, SV, NN, EV | 4.8% | 80% of the studies had RMSE below 0.95 and the remaining 20% had MSE below 0.05 |
| Mean Absolute Error (MAE) | EN, NN, REG | 4.5% | 69% of the study had a MAE value less than 20%, 23% had values between 22 and 30% and 8% had above 77% |
| Area Under the Curve (AUC) | REG, EN, DT, SV | 3.8% | 90% of the studies had AUC above 80% and the remaining 10% had an AUC of 73% and 65% |
| Mean Square Error (MSE) | REG, NN, EN | 2.2% | 75% of the studies had MSE below 0.07 and the remaining 25% had MSE below 0.82 |
| R Squared (R2) | NN, EN, REG | 1.3% | R2 values in the study where above 75% and the remaining were 10.64% and 14.9% respectively |
| Receiver Operating Characteristic Curve (ROC) | SV, NN, EN | 1% | The study had 78%, 80% and 89% ROC values |
| Mean Absolute Percent- age Error (MAPE) | NN, REG | 0.6% | The study had MAPE values of 0.1048 and 3.2027 |
| Other | EN, NN | 5.4% | N/A |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Attai, K.; Amannejad, Y.; Vahdat Pour, M.; Obot, O.; Uzoka, F.-M. A Systematic Review of Applications of Machine Learning and Other Soft Computing Techniques for the Diagnosis of Tropical Diseases. Trop. Med. Infect. Dis. 2022, 7, 398. https://doi.org/10.3390/tropicalmed7120398
Attai K, Amannejad Y, Vahdat Pour M, Obot O, Uzoka F-M. A Systematic Review of Applications of Machine Learning and Other Soft Computing Techniques for the Diagnosis of Tropical Diseases. Tropical Medicine and Infectious Disease. 2022; 7(12):398. https://doi.org/10.3390/tropicalmed7120398
Chicago/Turabian StyleAttai, Kingsley, Yasaman Amannejad, Maryam Vahdat Pour, Okure Obot, and Faith-Michael Uzoka. 2022. "A Systematic Review of Applications of Machine Learning and Other Soft Computing Techniques for the Diagnosis of Tropical Diseases" Tropical Medicine and Infectious Disease 7, no. 12: 398. https://doi.org/10.3390/tropicalmed7120398
APA StyleAttai, K., Amannejad, Y., Vahdat Pour, M., Obot, O., & Uzoka, F.-M. (2022). A Systematic Review of Applications of Machine Learning and Other Soft Computing Techniques for the Diagnosis of Tropical Diseases. Tropical Medicine and Infectious Disease, 7(12), 398. https://doi.org/10.3390/tropicalmed7120398









