Chagas Disease: Seroprevalence and Associated Factors in Indigenous Communities of the Southern Limit of Argentine Chaco
Abstract
1. Introduction
2. Materials and Methods
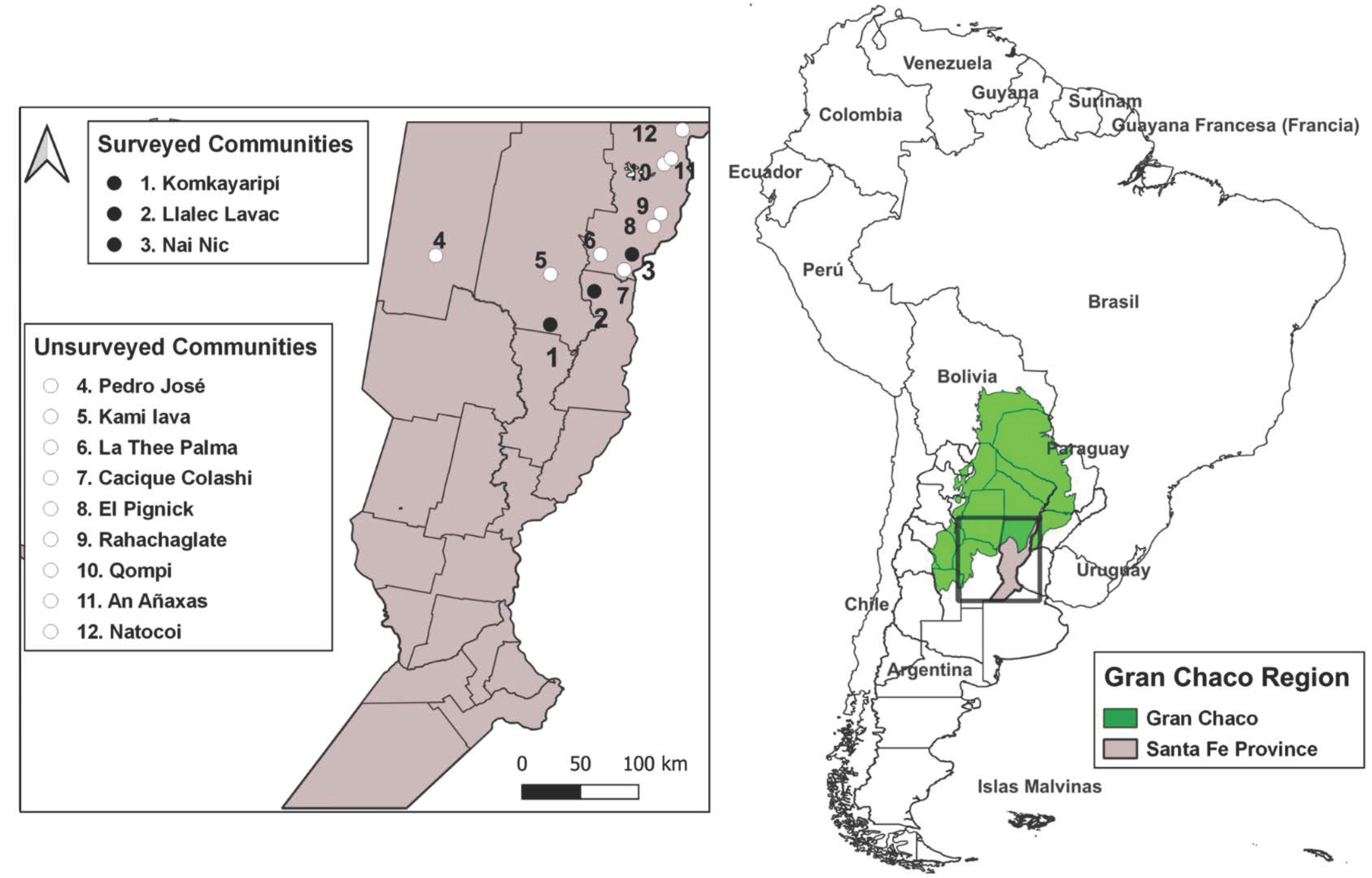
2.1. Study Area
2.2. Data Collection
2.3. Serological Analysis
2.4. Risk Factors Survey
2.5. Statistical Analysis
3. Results
3.1. Study Population
3.2. Seroprevalence of T. cruzi Infection
3.3. Risk Factors Related to T. cruzi Infection
3.4. Association Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. La Enfermedad de Chagas (Tripanosomiasis Americana). 2022. Available online: http://www.who.int/mediacentre/factsheets/fs340/es (accessed on 3 February 2022).
- Gaspe, M.; Provecho, Y.; Cardinal, M.; Fernandez, M.; Gürtler, R. Ecological and Sociodemographic Determinants of House Infestation by Triatoma infestans in Indigenous Communities of the Argentine Chaco. PloS Negl. Trop. Dis. 2015, 9, e0003614. [Google Scholar] [CrossRef] [PubMed]
- Danesi, E.; Olenka Codebó, M.; Sosa-Estani, S. Transmisión congénita de Trypanosoma cruzi: Argentina 2002–2014. Medicina (Buenos Aires) 2019, 79, 81–89. [Google Scholar]
- Schenone, H.; Gaggero, M.; Sapunar, J.; Contreras, M.; Rojas, A. Congenital Chagas disease of second generation in Santiago, Chile. Report of two cases. Rev. Inst. Med. Trop. Sao Paulo 2001, 43, 231–232. [Google Scholar] [CrossRef] [PubMed]
- Negrette, O.; Mora, M.; Basombrío, M. High prevalence of congenital Trypanosoma cruzi infection and family clustering in Salta, Argentina. Pediatrics 2005, 115, e668–e672. [Google Scholar] [CrossRef] [PubMed]
- Streiger, M.; Demonte, M.; Fabbro, D.; del Barco, M.; Miglietta, H.; Denner, S. Multicausalidad y evolución de la prevalencia de infección chagásica humana en la Provincia de Santa Fe, en relación al riesgo de transmisión vectorial. In Actualizaciones en Artropodología Sanitaria Argentina, 1st ed.; Salomon, O., Ed.; Fundación Mundo Sano: Buenos Aires, Argentina, 2002; pp. 221–231. [Google Scholar]
- Colussi, C.; Stafuza, M.; Nepote, M.; Mendicino, D. Seroprevalence of Chagas disease in urban and rural indigenous populations of the south of Gran Chaco. Rev. Soc. Bras. Med. Trop. 2022, 55, e0479–e2021. [Google Scholar] [CrossRef] [PubMed]
- Lovino, M.; Muller, G. Variabilidad y cambio climático en la Provincia de Santa Fe: Observaciones y proyecciones futuras. In Desarrollo Sostenible en el Centro Norte de la Provincia de Santa Fe: Ambiente, 1st ed.; De la Canal, A., Ed.; Universidad Nacional del Litoral: Santa Fe, Argentina, 2021; pp. 132–135. [Google Scholar]
- Ministerio de Justicia y Derechos Humanos de la Provincia de Santa Fe. Registro Especial de Comunidades Aborígenes. Listado de Comunidades Aborígenes. 2020. Available online: https://www.santafe.gov.ar/index.php/web/content/view/full/117260/(subtema)/93808 (accessed on 23 March 2022).
- Pan American Health Organization. Guía Para el Diagnóstico y el Tratamiento de la Enfermedad de Chagas. 2018. Available online: https://iris.paho.org/bitstream/handle/10665.2/49653/9789275320433_spa.pdf (accessed on 23 December 2022).
- Sanmartino, M.; Crocco, L. Conocimientos sobre la enfermedad de Chagas y factores de riesgo en comunidades epidemiológicamente diferentes de Argentina. Rev. Panam. Salud Publica 2000, 7, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Cucunuba, Z.; Florez, A.; Cardenas, A.; Pavia, P.; Montilla, M.; Aldana, R.; Villamizar, K.; Rios, L.; Nichols, R.; Puerta, C. Prevalence and risk factors for Chagas disease in pregnant women in Casanare, Colombia. Am. J. Trop. Med. Hyg. 2012, 87, 837. [Google Scholar] [CrossRef] [PubMed]
- Colussi, C.; Stafuza, M.; Denner, S.; Nepote, M.; Mendicino, D. Epidemiología de la enfermedad de Chagas en comunidades Mocovíes y Criollas en el sur del Chaco Argentino. Salud Publica Mex. 2016, 58, 3–4. [Google Scholar] [CrossRef] [PubMed]
- Crocco, L.; Nattero, J.; Lopez, A.; Cardozo, M.; Soria, C.; Ortiz, V.; Rodriguez, C. Factors associated with the presence of triatomines in rural areas of south Argentine Chaco. Rev. Soc. Bras. Med. Trop. 2019, 52, e20180357. [Google Scholar] [CrossRef] [PubMed]
- Di Rienzo, J.A.; Casanoves, F.; Balzarini, M.G.; Gonzalez, L.; Tablada, M.; Robledo, C.W. InfoStat Versión 2020. Centro de Transferencia InfoStat, FCA, Universidad Nacional de Córdoba, Argentina. Available online: http://www.infostat.com.ar (accessed on 26 December 2022).
- Centers for Disease Control and Prevention. Epi Info, a Database and Statistics Program for Public Health Professionals. Atlanta, GA, USA. 2011. Available online: https://www.cdc.gov/epiinfo/index.html (accessed on 26 December 2022).
- Moreno, M.; Moretti, E.; Basso, B.; Cespedes, M.; Catala, S.; Gorla, D. Seroprevalence of Trypanosoma cruzi infection and vector control activities in rural communities of the southern Gran Chaco (Argentina). Acta Trop. 2010, 113, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Moretti, E.; Castro, I.; Franceschi, C.; Basso, B. Chagas disease: Serological and electrocardiographic studies in Wichí and Creole communities of Misión Nueva Pompeya, Chaco, Argentina. Mem. Inst. Oswaldo Cruz 2010, 105, 621–626. [Google Scholar] [CrossRef] [PubMed]
- Lucero, R.; Bruses, B.; Cura, C.; Formichelli, L.; Juiz, N.; Fernandez, G.; Bisio, M.; Deluca, G.; Besuschio, S.; Hernandez, D.; et al. Chagas’ disease in Aboriginal and Creole communities from the Gran Chaco Region of Argentina: Seroprevalence and molecular parasitological characterization. Infect. Genet. Evol. 2016, 41, 84–92. [Google Scholar] [CrossRef] [PubMed]
- The World Bank. Bringing Forest and Poverty into Focus in the Chaco Ecoregion—Argentina. 2019. Available online: https://www.profor.info/sites/profor.info/files/publication/Annex%203%20-%20Forest%20Dependence2_2.pdf. (accessed on 27 December 2022).
- Chastonay, A.; Chastonay, O. Housing Risk Factors of Four Tropical Neglected Diseases: A Brief Review of the Recent Literature. Trop. Med. Infect. Dis. 2022, 7, 143. [Google Scholar] [CrossRef] [PubMed]
- Spillmann, C.; Burrone, S.; Coto, H. Análisis de la situación epidemiológica de la enfermedad de Chagas en Argentina: Avances en el control, 2012. Rev. Argent. Salud Publica. 2013, 4, 40–44. [Google Scholar]
- Sanmartino, M.; Forsyth, C.; Avaria, A.; Velarde-Rodriguez, M.; Gomez i Prat, J.; Albajar-Viñas, P. The multidimensional comprehension of Chagas disease. Contributions, approaches, challenges and opportunities from and beyond the Information, Education and Communication field. Mem. Inst. Oswaldo Cruz 2021, 117, e200460. [Google Scholar] [CrossRef] [PubMed]
- Viotti, R.; Vigliano, C.; Alvarez, M.; Lococo, B.; Petti, M.; Bertocchi, G.; Armenti, A. El impacto de las condiciones socioeconómicas en la evolución de la enfermedad de Chagas crónica. Rev. Esp. Cardiol. 2009, 62, 1224–1232. [Google Scholar] [CrossRef] [PubMed]
- Pan American Health Organization. El 70% de las Personas con Chagas no Saben que Están Infectadas. Available online: https://www.paho.org/es/noticias/13-4-2021-70-personas-con-chagas-no-saben-que-estan-infectadas (accessed on 28 December 2022).
- Klein, M.; Proaño, A.; Noazin, S.; Sciaudone, M.; Gilman, R.; Bowman, N.M. Risk factors for vertical transmission of Chagas disease: A systematic review and meta-analysis. Int. J. Infect. Dis. 2021, 105, 357–373. [Google Scholar] [CrossRef] [PubMed]
- Mendicino, D.; Bottasso, O. Chagas disease in children from the Gran Chaco region: A bibliographic appraisal. Trop. Doct. 2022, 52, 560–562. [Google Scholar] [CrossRef] [PubMed]
- Sartor, P.; Colaianni, I.; Cardinal, M.V.; Bua, J.; Freilij, H.; Gürtler, R.E. Improving access to Chagas disease diagnosis and etiologic treatment in remote rural communities of the Argentine Chaco through strengthened primary health care and broad social participation. PloS Negl. Trop. Dis. 2017, 11, e0005336. [Google Scholar] [CrossRef] [PubMed]
| Community | % |
|---|---|
| Komkayaripí | 21.1 (39/185) |
| Llalec Lavac | 11.1 (6/54) |
| Nai Nic | 17.0 (10/59) |
| Sex | |
| Female | 17.5 (30/171) |
| Male | 19.7 (25/127) |
| Total | 18.5 (55/298) |
| Communities | Age (Years) | Sex | Schooling | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Median | Rank | Female | Male | I | IP | CP | IS | CS | |
| Komkayaripí | 44.5 | 23-73 | 15.0% (6/40) | 85.0% (34/40) | 17.5% (7/40) | 45.0% (18/40) | 25.0% (10/40) | 7.5% (3/40) | 5.0% (2/40) |
| LlalecLavac | 35.0 | 25-59 | 11.1% (1/9) | 88.9% (8/9) | 11.1% (1/9) | 33.3% (3/9) | 55.6% (5/9) | 0% (0/9) | 0% (0/9) |
| Nai Nic | 38.0 | 28-73 | 26.7% (4/15) | 73.3% (11/15) | 20.0% (3/15) | 46.7% (7/15) | 6.7% (1/15) | 13.3% (2/15) | 13.3% (2/15) |
| Total | 39.0 | 23-73 | 17.2% (11/64) | 82.8% (53/64) | 17.2% (11/64) | 43.8% (28/64) | 25.0% (16/64) | 7.8% (5/64) | 6.3% (4/64) |
| Variable | Positive Housing | Negative Housing | Frequency Total (%) | Odds Ratio | CI 95% | p-Value | ||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | |||||
| Schooling of the head of household | ||||||||
| Incomplete primary | 18 | 46.2 | 21 | 53.8 | 43.8 | 3.43 | 1.11–10.59 | 0.03 |
| Complete primary | 5 | 20.0 | 20 | 80.0 | 25.0 | |||
| Presence of animals | ||||||||
| Yes | 21 | 35.6 | 38 | 64.4 | 87.5 | 0.83 | 0.15–4.57 | 0.84 |
| No | 2 | 40.0 | 3 | 60.0 | 12.5 | |||
| Critical overcrowding | ||||||||
| Yes | 18 | 40.9 | 26 | 59.1 | 68.8 | 2.08 | 0.66–6.49 | 0.22 |
| No | 5 | 25.0 | 15 | 75.0 | 31.3 | |||
| Characteristic of the house | ||||||||
| With risk | 5 | 38.5 | 8 | 61.5 | 20.3 | 1.15 | 0.34–3.86 | 0.83 |
| Without risk | 18 | 35.3 | 33 | 64.7 | 79.7 | |||
| Firewood storage | ||||||||
| Yes | 14 | 46.7 | 16 | 53.3 | 46.9 | 2.43 | 0.87–6.78 | 0.09 |
| No | 9 | 26.5 | 25 | 73.5 | 53.1 | |||
| Observation of kissing bugs | ||||||||
| Yes | 7 | 31.8 | 15 | 68.2 | 12.5 | 0.76 | 0.26–2.20 | 0.61 |
| No | 16 | 38.1 | 26 | 61.9 | 87.5 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Colussi, C.; Nepote, M.; Chiaraviglio, R.; Mendicino, D. Chagas Disease: Seroprevalence and Associated Factors in Indigenous Communities of the Southern Limit of Argentine Chaco. Trop. Med. Infect. Dis. 2023, 8, 64. https://doi.org/10.3390/tropicalmed8010064
Colussi C, Nepote M, Chiaraviglio R, Mendicino D. Chagas Disease: Seroprevalence and Associated Factors in Indigenous Communities of the Southern Limit of Argentine Chaco. Tropical Medicine and Infectious Disease. 2023; 8(1):64. https://doi.org/10.3390/tropicalmed8010064
Chicago/Turabian StyleColussi, Carlina, Marcelo Nepote, Romina Chiaraviglio, and Diego Mendicino. 2023. "Chagas Disease: Seroprevalence and Associated Factors in Indigenous Communities of the Southern Limit of Argentine Chaco" Tropical Medicine and Infectious Disease 8, no. 1: 64. https://doi.org/10.3390/tropicalmed8010064
APA StyleColussi, C., Nepote, M., Chiaraviglio, R., & Mendicino, D. (2023). Chagas Disease: Seroprevalence and Associated Factors in Indigenous Communities of the Southern Limit of Argentine Chaco. Tropical Medicine and Infectious Disease, 8(1), 64. https://doi.org/10.3390/tropicalmed8010064









