High-Risk Areas for Congenital Zika Syndrome in Rio de Janeiro: Spatial Cluster Detection
Abstract
:1. Introduction
2. Materials and Methods
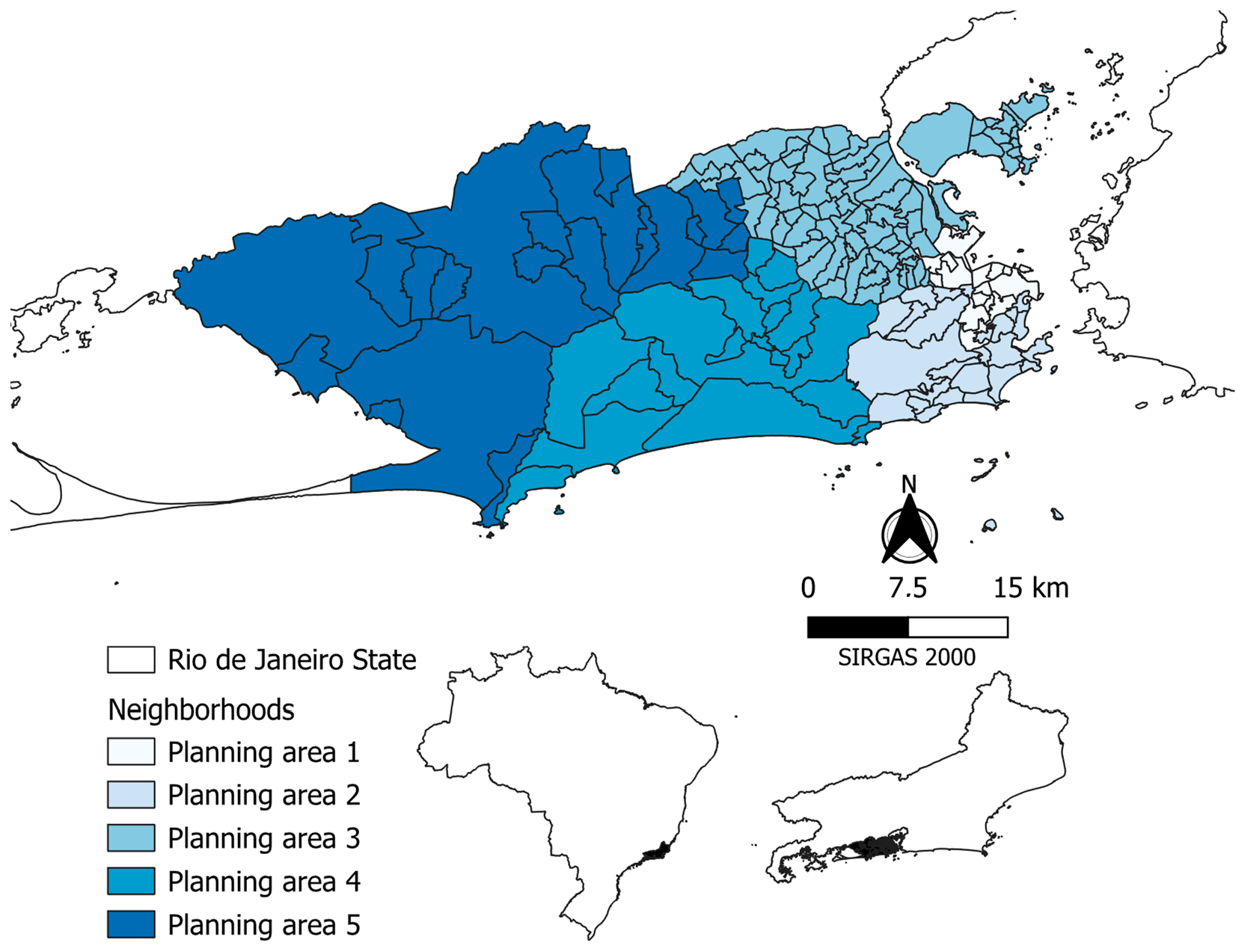
2.1. Design and Study Area
2.2. Data Source and Analysis
2.3. Congenital Zika Syndrome Notification
2.4. Maternal and Child Profile Associated with Congenital Zika Syndrome
2.5. High-Risk Clusters of Children with CZS: Spatial Distribution in the Socioeconomic Context
3. Results
4. Discussion
4.1. Maternal and Child Profile Associated with Congenital Zika Syndrome
4.2. High-Risk Clusters of Children with CZS: Spatial Distribution in the Socioeconomic Context
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gardner, L.M.; Bóta, A.; Gangavarapu, K.; Kraemer, M.U.G.; Grubaugh, N.D. Inferring the Risk Factors behind the Geographical Spread and Transmission of Zika in the Americas. PLoS Negl. Trop. Dis. 2018, 12, 6194. [Google Scholar] [CrossRef] [PubMed]
- Musso, D.; Gubler, D.J. Zika Virus. Clin. Microbiol. Rev. 2016, 29, 487–524. [Google Scholar] [CrossRef]
- Shuaib, W.; Stanazai, H.; Abazid, A.G.; Mattar, A.A. Re-Emergence of Zika Virus: A Review on Pathogenesis, Clinical Manifestations, Diagnosis, Treatment, and Prevention. Am. J. Med. 2016, 129, 879–891. [Google Scholar] [CrossRef]
- Freitas, D.A.; Souza-Santos, R.; Carvalho, L.M.A.; Barros, W.B.; Neves, L.M.; Brasil, P.; Wakimoto, M.D. Congenital Zika Syndrome: A Systematic Review. PLoS ONE 2020, 15, e0242367. [Google Scholar] [CrossRef] [PubMed]
- de Araujo, T.V.B.; Rodrigues, L.C.; de Alencar Ximenes, R.A.; de Barros Miranda-Filho, D.; Montarroyos, U.R.; de Melo, A.P.L.; Valongueiro, S.; de Albuquerque, M.d.F.P.M.; Souza, W.V.; Braga, C.; et al. Association between Zika Virus Infection and Microcephaly in Brazil, January to May, 2016: Preliminary Report of a Case-Control Study. Lancet Infect. Dis. 2016, 16, 1356–1363. [Google Scholar] [CrossRef] [PubMed]
- Ministério da Saúde. Atenção Ao Pré-Natal de Baixo Risco. (Cadernos de Atenção Básica, N° 32), 1st ed.; Ministério da Saúde: Brasília, Brazil, 2013; Volume 1.
- Nahmias, A.J.; Walls, K.W.; Stewart, J.A.; Herrmann, K.L.; Flynt, W.J., Jr. The ToRCH Complex-Perinatal Infections Associated with Toxoplasma and Rubella, Cytomegol- and Herpes Simplex Viruses. Pediatr. Res. 1971, 5, 405–406. [Google Scholar] [CrossRef]
- Pomar, L.; Malinger, G.; Benoist, G.; Carles, G.; Ville, Y.; Rousset, D.; Hcini, N.; Pomar, C.; Jolivet, A.; Lambert, V. Association between Zika Virus and Fetopathy: A Prospective Cohort Study in French Guiana. Ultrasound Obstet. Gynecol. Off. J. Int. Soc. Ultrasound Obstet. Gynecol. 2017, 49, 729–736. [Google Scholar] [CrossRef] [PubMed]
- WHO. Zika Cases and Congenital Syndrome Associated with Zika Virus Reported by Countries and Territories in the Americas, 2015–2018: Cumulative Cases—Data as of 4 January 2018—PAHO/WHO|Pan American Health Organization. Available online: https://www.paho.org/en/node/60231 (accessed on 10 April 2024).
- Brasil. Boletim Epidemiológico No 5: Situação Epidemiológica Da Síndrome Congênita Associada à Infecção Pelo Vírus Zika: Brasil, 2015 a 2022. Available online: http://plataforma.saude.gov.br/anomalias-congenitas/boletim-epidemiologico-SVSA-05-2023.pdf (accessed on 4 April 2023).
- Duttine, A.; Smythe, T.; Ribiero Calheiro de Sá, M.; Ferrite, S.; Zuurmond, M.; Moreira, M.E.; Collins, A.; Milner, K.; Kuper, H. Congenital Zika Syndrome—Assessing the Need for a Family Support Programme in Brazil. Int. J. Environ. Res. Public. Health 2020, 17, 3559. [Google Scholar] [CrossRef]
- Campos, M.C.; Dombrowski, J.G.; Phelan, J.; Marinho, C.R.F.; Hibberd, M.; Clark, T.G.; Campino, S. Zika Might Not Be Acting Alone: Using an Ecological Study Approach to Investigate Potential Co-Acting Risk Factors for an Unusual Pattern of Microcephaly in Brazil. PLoS ONE 2018, 13, e0201452. [Google Scholar] [CrossRef]
- Gonçalves, A.E.; Tenório, S.D.B.; da Silva Ferraz, P.C. Aspectos socioeconômicos dos genitores de crianças com microcefalia relacionada ao Zika vírus. Rev. Pesqui. Em Fisioter. 2018, 8, 155–166. [Google Scholar] [CrossRef]
- Souza, A.I.; de Siqueira, M.T.; Ferreira, A.L.C.G.; de Freitas, C.U.; Bezerra, A.C.V.; Ribeiro, A.G.; Nardocci, A.C. Geography of Microcephaly in the Zika Era: A Study of Newborn Distribution and Socio-Environmental Indicators in Recife, Brazil, 2015–2016. Public Health Rep. 2018, 133, 461–471. [Google Scholar] [CrossRef]
- de Souza, W.V.; de Albuquerque, M.d.F.P.M.; Vazquez, E.; Bezerra, L.C.A.; da Cruz Gouveia Mendes, A.; Lyra, T.M.; de Araujo, T.V.B.; de Oliveira, A.L.S.; Braga, M.C.; de Alencar Ximenes, R.A.; et al. Microcephaly Epidemic Related to the Zika Virus and Living Conditions in Recife, Northeast Brazil. BMC Public Health 2018, 18, 130. [Google Scholar] [CrossRef] [PubMed]
- Mocelin, H.J.S.; Catão, R.C.; Freitas, P.S.S.; Prado, T.N.; Bertolde, A.I.; Castro, M.C.; Maciel, E.L.N. Analysis of the Spatial Distribution of Cases of Zika Virus Infection and Congenital Zika Virus Syndrome in a State in the Southeastern Region of Brazil: Sociodemographic Factors and Implications for Public Health. Int. J. Gynaecol. Obstet. Off. Organ Int. Fed. Gynaecol. Obstet. 2020, 148 (Suppl. S2), 61–69. [Google Scholar] [CrossRef] [PubMed]
- IBGE. IBGE Cidades—Panorama Do Rio de Janeiro/Rio de Janeiro. Available online: https://cidades.ibge.gov.br/brasil/rj/rio-de-janeiro/panorama (accessed on 15 April 2024).
- Ministério da Saúde Orientações Integradas de Vigilância e Atenção à Saúde No Âmbito da Emergência de Saúde Pública de Importância Nacional. Available online: http://portalarquivos.saude.gov.br/images/pdf/2016/dezembro/12/orientacoes-integradas-vigilancia-atencao.pdf (accessed on 19 November 2017).
- Ministério da Saúde. Protocolo de Vigilância e Resposta à Ocorrência de Microcefalia Relacionada à Infecção Pelo Vírus Zika; Ministério da Saúde: Brasília, Brazil, 2016.
- The Global Health Network INTERGROWTH-21st Applications and Calculators—INTERGROWTH-21st. Available online: https://intergrowth21.tghn.org/intergrowth-21st-applications/ (accessed on 17 March 2020).
- Villar, J.; Ismail, L.C.; Victora, C.G.; Ohuma, E.O.; Bertino, E.; Altman, D.G.; Lambert, A.; Papageorghiou, A.T.; Carvalho, M.; Jaffer, Y.A.; et al. International Standards for Newborn Weight, Length, and Head Circumference by Gestational Age and Sex: The Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet 2014, 384, 857–868. [Google Scholar] [CrossRef] [PubMed]
- Kulldorff, M. SaTScanTM Manual Do Usuário. Available online: https://www.satscan.org/SaTScan_TM_Manual_do_Usu%C3%A1rio_v9.4_Portugues.pdf (accessed on 18 April 2018).
- Kulldorff, M. SaTScanTM User Guide. Available online: https://www.satscan.org/cgi-bin/satscan/register.pl/SaTScan_Users_Guide.pdf?todo=process_userguide_download (accessed on 30 July 2020).
- IPP Número de Nascidos Vivos, Segundo a Idade da Mãe, Áreas de Planejamento (AP) e Regiões Administrativas (RA) de Residência no Município do Rio de Janeiro, 2002/2006-2017. Available online: https://www.data.rio/documents/8a0fb5d7ecf04c6eae26a619863871c6/about (accessed on 22 February 2020).
- Souza, E.C.D.O.; Santos, E.S.D.; Rosa, A.M.; Botelho, C. Varredura espaço-temporal para identificação de áreas de risco para hospitalização de crianças por asma em Mato Grosso. Rev. Bras. Epidemiol. 2019, 22, e190019. [Google Scholar] [CrossRef] [PubMed]
- IPP. Índice de Desenvolvimento Social. Available online: https://www.data.rio/documents/fa85ddc76a524380ad7fc60e3006ee97/about (accessed on 17 February 2020).
- Santos, J.P.C.D.; Honório, N.A.; Nobre, A.A. Definition of Persistent Areas with Increased Dengue Risk by Detecting Clusters in Populations with Differing Mobility and Immunity in Rio de Janeiro, Brazil. Cad. Saúde Pública 2019, 35, e00248118. [Google Scholar] [CrossRef]
- de Almeida Avelino, M.O.; da Silva Ferraz, P.C. Análise do desenvolvimento neuropsicomotor em crianças com síndrome pós–zika vírus: Um estudo transversal. Rev. Pesqui. Em Fisioter. 2018, 8, 147–154. [Google Scholar] [CrossRef]
- Lima, G.P.; Rozenbaum, D.; Pimentel, C.; Frota, A.C.C.; Vivacqua, D.; Machado, E.S.; Sztajnbok, F.; Abreu, T.; Soares, R.A.; Hofer, C.B. Factors Associated with the Development of Congenital Zika Syndrome: A Case-Control Study. BMC Infect. Dis. 2019, 19, 277. [Google Scholar] [CrossRef] [PubMed]
- Brasil, P.; Pereira, J.P., Jr.; Moreira, M.E.; Ribeiro Nogueira, R.M.; Damasceno, L.; Wakimoto, M.; Rabello, R.S.; Valderramos, S.G.; Halai, U.-A.; Salles, T.S.; et al. Zika Virus Infection in Pregnant Women in Rio de Janeiro. N. Engl. J. Med. 2016, 375, 2321–2334. [Google Scholar] [CrossRef]
- Honein, M.A.; Dawson, A.L.; Petersen, E.E.; Jones, A.M.; Lee, E.H.; Yazdy, M.M.; Ahmad, N.; Macdonald, J.; Evert, N.; Bingham, A.; et al. Birth Defects Among Fetuses and Infants of US Women With Evidence of Possible Zika Virus Infection During Pregnancy. JAMA 2017, 317, 59–68. [Google Scholar] [CrossRef]
- Zin, A.A.; Tsui, I.; Rossetto, J.; Vasconcelos, Z.; Adachi, K.; Valderramos, S.; Halai, U.-A.; Pone, M.V.d.S.; Pone, S.M.; Silveira Filho, J.C.B.; et al. Screening Criteria for Ophthalmic Manifestations of Congenital Zika Virus Infection. JAMA Pediatr. 2017, 171, 847–854. [Google Scholar] [CrossRef] [PubMed]
- Secretaria Municipal de Saúde do Rio de Janeiro. Boletim Epidemiológico: Sífilis no Município do Rio de Janeiro—2023, 1st ed.; Prefeitura do Rio de Janeiro: Rio de Janeiro, Brazil, 2023. [Google Scholar]
- Bandeira, A.C.; Gois, L.L.; Campos, G.S.; Sardi, S.; Yssel, H.; Vieillard, V.; Autran, B.; Grassi, M.F.R. Clinical and Laboratory Findings of Acute Zika Virus Infection in Patients from Salvador during the First Brazilian Epidemic. Braz. J. Infect. Dis. 2020, 24, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Ospina, M.L.; Tong, V.T.; Gonzalez, M.; Valencia, D.; Mercado, M.; Gilboa, S.M.; Rodriguez, A.J.; Tinker, S.C.; Rico, A.; Winfield, C.M.; et al. Zika Virus Disease and Pregnancy Outcomes in Colombia. N. Engl. J. Med. 2020, 383, 537–545. [Google Scholar] [CrossRef] [PubMed]
- IPP. Nascidos vivos Residentes no Município do Rio de Janeiro Segundo a Duração da Gravidez, Percentual de Prematuridade por Áreas de Planejamento (AP) e Regiões Administrativas (RA) de Residência 2002/2006-2017. Available online: https://www.data.rio/documents/31780b02ef7447f9b645c7583dc3b2b3/about (accessed on 15 April 2024).
- Cragan, J.D.; Mai, C.T.; Petersen, E.E.; Liberman, R.F.; Forestieri, N.E.; Stevens, A.C.; Delaney, A.; Dawson, A.L.; Ellington, S.R.; Shapiro-Mendoza, C.K.; et al. Baseline Prevalence of Birth Defects Associated with Congenital Zika Virus Infection—Massachusetts, North Carolina, and Atlanta, Georgia, 2013–2014. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 219–222. [Google Scholar] [CrossRef] [PubMed]
- Culjat, M.; Darling, S.E.; Nerurkar, V.R.; Ching, N.; Kumar, M.; Min, S.K.; Wong, R.; Grant, L.; Melish, M.E. Clinical and Imaging Findings in an Infant With Zika Embryopathy. Clin. Infect. Dis. 2016, 63, 805–811. [Google Scholar] [CrossRef] [PubMed]
- De Paula Freitas, B.; De Oliveira Dias, J.R.; Prazeres, J.; Sacramento, G.A.; Ko, A.I.; Maia, M.; Belfort, R. Ocular Findings in Infants with Microcephaly Associated with Presumed Zika Virus Congenital Infection in Salvador, Brazil. JAMA Ophthalmol. 2016, 134, 529–535. [Google Scholar] [CrossRef]
- Del Campo, M.; Feitosa, I.M.L.; Ribeiro, E.M.; Horovitz, D.D.G.; Pessoa, A.L.S.; Franca, G.V.A.; Garcia-Alix, A.; Doriqui, M.J.R.; Wanderley, H.Y.C.; Sanseverino, M.V.T.; et al. The Phenotypic Spectrum of Congenital Zika Syndrome. Am. J. Med. Genet. A 2017, 173, 841–857. [Google Scholar] [CrossRef]
- Martines, R.B.; Bhatnagar, J.; de Oliveira Ramos, A.M.; Davi, H.P.F.; Iglezias, S.D.; Kanamura, C.T.; Keating, M.K.; Hale, G.; Silva-Flannery, L.; Muehlenbachs, A.; et al. Pathology of Congenital Zika Syndrome in Brazil: A Case Series. Lancet 2016, 388, 898–904. [Google Scholar] [CrossRef] [PubMed]
- Meneses, J.D.A.; Ishigami, A.C.; de Mello, L.M.; de Albuquerque, L.L.; Antunes de Brito, C.A.; Cordeiro, M.T.; Pena, L.J. Lessons Learned at the Epicenter of Brazil’s Congenital Zika Epidemic: Evidence From 87 Confirmed Cases. Clin. Infect. Dis. 2017, 64, 1302–1308. [Google Scholar] [CrossRef]
- Moron, A.F.; Cavalheiro, S.; Milani, H.J.F.; Sarmento, S.G.P.; Tanuri, C.; de Souza, F.F.; Richtmann, R.; Witkin, S.S. Microcephaly Associated with Maternal Zika Virus Infection. BJOG Int. J. Obstet. Gynaecol. 2016, 123, 1265–1269. [Google Scholar] [CrossRef]
- Norero Vega, X.; Castaño G, E.; Estripeaut C, D.; Sáez-Llorens, X.; Reyes, O.; Bissot, A. Zika y defecto del tubo neural. Pediátr Panamá 2016, 45, 23–25. [Google Scholar]
- Rodó, C.; Suy, A.; Sulleiro, E.; Soriano-Arandes, A.; Maiz, N.; García-Ruiz, I.; Arévalo, S.; Rando, A.; Anton, A.; Vázquez Méndez, É.; et al. Pregnancy Outcomes after Maternal Zika Virus Infection in a Non-Endemic Region: Prospective Cohort Study. Clin. Microbiol. Infect. 2019, 25, 633.e5–633.e9. [Google Scholar] [CrossRef] [PubMed]
- Schaub, B.; Vouga, M.; Najioullah, F.; Gueneret, M.; Monthieux, A.; Harte, C.; Muller, F.; Jolivet, E.; Adenet, C.; Dreux, S.; et al. Analysis of Blood from Zika Virus-Infected Fetuses: A Prospective Case Series. Lancet Infect. Dis. 2017, 17, 520–527. [Google Scholar] [CrossRef] [PubMed]
- van der Linden, V.; Rolim Filho, E.L.; Lins, O.G.; van der Linden, A.; Viana Vasco Aragao, M.D.F.; Brainer-Lima, A.M.; Sousa Cruz, D.D.C.; Wanderley Rocha, M.A.; Sobral da Silva, P.F.; Costa Gomes Carvalho, M.D.; et al. Congenital Zika Syndrome with Arthrogryposis: Retrospective Case Series Study. Br. Med. J. 2016, 354, i3899. [Google Scholar] [CrossRef] [PubMed]
- Van Der Linden, V.; Pessoa, A.; Dobyns, W.; Barkovich, A.J.; van der Linden Júnior, H.; Filho, E.L.R.; Ribeiro, E.M.; Leal, M.D.C.; Coimbra, P.P.D.A.; Aragao, M.D.F.V.V.; et al. Description of 13 Infants Born During October 2015-January 2016 With Congenital Zika Virus Infection Without Microcephaly at Birth—Brazil. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 1343–1348. [Google Scholar] [CrossRef] [PubMed]
- van der Linden, V.; van der Linden Junior, H.; de Carvalho Leal, M.; Rolim, E.L.F.; van der Linden, A.; Aragao, M.D.F.V.V.; Brainer-Lima, A.M.; Cruz, D.D.C.S.; Ventura, L.O.; Florencio, T.L.T.; et al. Discordant Clinical Outcomes of Congenital Zika Virus Infection in Twin Pregnancies. Arq. Neuropsiquiatr. 2017, 75, 381–386. [Google Scholar] [CrossRef] [PubMed]
- Ventura, L.O.; Ventura, C.V.; Lawrence, L.; van der Linden, V.; van der Linden, A.; Gois, A.L.; Cavalcanti, M.M.; Barros, E.A.; Dias, N.C.; Berrocal, A.M.; et al. Visual Impairment in Children with Congenital Zika Syndrome. J. AAPOS 2017, 21, 295–299.e2. [Google Scholar] [CrossRef] [PubMed]
- Werner, H.; Fazecas, T.; Guedes, B.; Lopes Dos Santos, J.; Daltro, P.; Tonni, G.; Campbell, S.; Araujo Junior, E. Intrauterine Zika Virus Infection and Microcephaly: Correlation of Perinatal Imaging and Three-Dimensional Virtual Physical Models. Ultrasound Obstet. Gynecol. Off. J. Int. Soc. Ultrasound Obstet. Gynecol. 2016, 47, 657–660. [Google Scholar] [CrossRef]
- de Siqueira, I.C.; de Almeida, B.L.; Lage, M.L.C.; Serra, L.; Carvalho, A.; de Lima, M.M.; Góes, M.D.F.N.; Crispim, M.D.S.I.N.; da Costa Pereira, M.M.; Costa, B.G.G.; et al. Perinatal Characteristics and Longer-Term Outcomes in Brazilian Children with Confirmed or Suspected Congenital Zika Infection: ZIKAction Paediatric Registry. Dialogues Health 2023, 2, 100104. [Google Scholar] [CrossRef]
- Aragão, M.F.; Van Der Linden, V.; Brainer-Lima, A.M.; Coeli, R.R.; Rocha, M.A.; Da Silva, P.S.; de Carvalho, M.D.C.G.; Van Der Linden, A.; De Holanda, A.C.; Valenca, M.M. Clinical Features and Neuroimaging (CT and MRI) Findings in Presumed Zika Virus Related Congenital Infection and Microcephaly: Retrospective Case Series Study. BMJ Online 2016, 353, i1901. [Google Scholar] [CrossRef]
- Bastos, L.F.C.S. OPAS/OMS Brasil—OMS Declara Fim de Emergência de Saúde Pública Internacional, Mas Diz Que Resposta Ao Zika e Suas Consequências Deve Continuar|OPAS/OMS. Available online: http://www.paho.org/bra/index.php?option=com_content&view=article&id=5297:oms-declara-fim-de-emergencia-de-saude-publica-internacional-mas-diz-que-resposta-ao-zika-e-suas-consequencias-deve-continuar&Itemid=812 (accessed on 23 October 2017).
- Braga, J.U.; Bressan, C.; Dalvi, A.P.R.; Calvet, G.A.; Daumas, R.P.; Rodrigues, N.; Wakimoto, M.; Nogueira, R.M.R.; Nielsen-Saines, K.; Brito, C.; et al. Accuracy of Zika Virus Disease Case Definition during Simultaneous Dengue and Chikungunya Epidemics. PLoS ONE 2017, 12, e0179725. [Google Scholar] [CrossRef] [PubMed]
- Faluyi, U.; Obadare, O.; Sangem, A.; Onuegbu, C.A.; Medavarapu, S. Complications Associated with Zika Virus Infection: A Systematic Review Study. Am. Sci. Res. J. Eng. Technol. Sci. 2016, 24, 151–161. [Google Scholar]
- Faria, N.R.; Azevedo, R.D.S.D.S.; Kraemer, M.U.G.; Souza, R.; Cunha, M.S.; Hill, S.C.; Theze, J.; Bonsall, M.B.; Bowden, T.A.; Rissanen, I.; et al. Zika Virus in the Americas: Early Epidemiological and Genetic Findings. Science 2016, 352, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Leal, M.C.; van der Linden, V.; Bezerra, T.P.; de Valois, L.; Borges, A.C.G.; Antunes, M.M.C.; Brandt, K.G.; Moura, C.X.; Rodrigues, L.C.; Ximenes, C.R. Characteristics of Dysphagia in Infants with Microcephaly Caused by Congenital Zika Virus Infection, Brazil, 2015. Emerg. Infect. Dis. 2017, 23, 1253–1259. [Google Scholar] [CrossRef] [PubMed]
- Marinho, F.; de Araújo, V.E.M.; Porto, D.L.; Ferreira, H.L.; Coelho, M.R.S.; Lecca, R.C.R.; de Oliveira, H.; Poncioni, I.P.D.A.; Maranhão, M.H.N.; Mendes, Y.M.M.B.; et al. Microcefalia no Brasil: Prevalência e caracterização dos casos a partir do Sistema de Informações sobre Nascidos Vivos (Sinasc), 2000–2015. Epidemiol. Serv. Saúde 2016, 25, 701–712. [Google Scholar] [CrossRef] [PubMed]
- Musso, D.; Nilles, E.J.; Cao-Lormeau, V.-M. Rapid Spread of Emerging Zika Virus in the Pacific Area. Clin. Microbiol. Infect. 2014, 20, O595–O596. [Google Scholar] [CrossRef] [PubMed]
- WHO. Zika Virus. Available online: https://www.who.int/news-room/fact-sheets/detail/zika-virus (accessed on 1 October 2019).
- Aragão, M.F.V.V.; Brainer-Lima, A.M.; Holanda, A.C.; van der Linden, V.; Vasco Aragao, L.; Silva Junior, M.L.M.; Sarteschi, C.; Petribu, N.C.L.; Valenca, M.M. Spectrum of Spinal Cord, Spinal Root, and Brain MRI Abnormalities in Congenital Zika Syndrome with and without Arthrogryposis. Am. J. Neuroradiol. 2017, 38, 1045–1053. [Google Scholar] [CrossRef]
- Parra-Saavedra, M.; Reefhuis, J.; Piraquive, J.P.; Gilboa, S.M.; Badell, M.L.; Moore, C.A.; Mercado, M.; Valencia, D.; Jamieson, D.J.; Beltran, M.; et al. Serial Head and Brain Imaging of 17 Fetuses With Confirmed Zika Virus Infection in Colombia, South America. Obstet. Gynecol. 2017, 130, 207–212. [Google Scholar] [CrossRef]
- Perez, S.; Tato, R.; Cabrera, J.J.; Lopez, A.; Robles, O.; Paz, E.; Coira, A.; Sanchez-Seco, M.P.; Vazquez, A.; Carballo, R.; et al. Confirmed Case of Zika Virus Congenital Infection, Spain, March 2016. Eurosurveillance 2016, 21, 30261. [Google Scholar] [CrossRef]
- Van der Linden, V.; Petribu, N.C.D.L.; Pessoa, A.; Faquini, I.; Paciorkowski, A.R.; van der Linden, H.; Silveira-Moriyama, L.; Cordeiro, M.T.; Hazin, A.N.; Barkovich, A.J.; et al. Association of Severe Hydrocephalus With Congenital Zika Syndrome. JAMA Neurol. 2019, 76, 203–210. [Google Scholar] [CrossRef]
- Hamanaka, T.; Ribeiro, C.T.M.; Pone, S.; Gomes, S.C.; Nielsen-Saines, K.; Brickley, E.B.; Moreira, M.E.; Pone, M. Longitudinal Follow-Up of Gross Motor Function in Children with Congenital Zika Virus Syndrome from a Cohort in Rio de Janeiro, Brazil. Viruses 2022, 14, 1173. [Google Scholar] [CrossRef] [PubMed]
- Paixão, E.S.; Fernandes, Q.H.R.F.; Cardim, L.L.; Pescarini, J.M.; Costa, M.C.N.; Falcão, I.R.; Brickley, E.B.; Santos, A.C.; Portela Souza, A.; Carvalho-Sauer, R.D.C.O.; et al. Socioeconomic Risk Markers of Congenital Zika Syndrome: A Nationwide, Registry-Based Study in Brazil. BMJ Glob. Health 2022, 7, e009600. [Google Scholar] [CrossRef] [PubMed]
- Mattos, A.M.; Rastely-Junior, V.N.; Pires, M.M.; Aguilar, J.P.; Lessa, M.S.A.; Regis, C.; Wanderley, M.; Leony, J.; Bouzon, J.; Ballalai, V.; et al. Predictors of Neurodevelopment in Microcephaly Associated with Congenital Zika Syndrome: A Prospective Study. Child. Basel Switz. 2023, 10, 1831. [Google Scholar] [CrossRef] [PubMed]
- de Melo, A.P.L.; Lyra, T.M.; Barbosa, J.M.V.; Araújo, T.V.B. de Congenital zika syndrome and family impacts: An integrative review. Cienc. Saude Coletiva 2023, 28, 1425–1441. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, F.A.; da Silva, A.M.; da Hora, S.S.; de Oliveira, S.A.; da Silva Junior, A.G.; Cardoso, C.A.A. Healthcare for Children with Congenital Zika Syndrome: Analysis of Access to Social Rights. Ciênc. Saúde Coletiva 2022, 27, 3679–3688. [Google Scholar] [CrossRef]
- Peiter, P.C.; Pereira, R.D.S.; Nunes Moreira, M.C.; Nascimento, M.; Tavares, M.D.F.L.; Franco, V.D.C.; Carvajal Cortês, J.J.; Campos, D.D.S.; Barcellos, C. Zika Epidemic and Microcephaly in Brazil: Challenges for Access to Health Care and Promotion in Three Epidemic Areas. PLoS ONE 2020, 15, e0235010. [Google Scholar] [CrossRef] [PubMed]
- Coêlho, B.P.; Miranda, G.M.D.; da Silva, M.C.N.A.; Torres, T.C.D.O.; Oliveira, T.F. Primary care in the context of the Zika epidemic and congenital Zika syndrome in the state of Pernambuco, Brazil: Context, bond and care. Cienc. Saude Coletiva 2022, 27, 861–870. [Google Scholar] [CrossRef] [PubMed]
- Roma, J.H.F.; Alves, R.C.; da Silva, V.S.; Ferreira, M.J.; de Araújo, C.; Pavoni, J.H.C.; Roma, J.H.F.; Alves, R.C.; da Silva, V.S.; Ferreira, M.J.; et al. Descriptive Study of Suspected Congenital Zika Syndrome Cases during the 2015–2016 Epidemic in Brazil. Rev. Soc. Bras. Med. Trop. 2019, 52, e20190105. [Google Scholar] [CrossRef]
- Ambrogi, I.G.; Brito, L.; Diniz, D. The Vulnerabilities of Lives: Zika, Women and Children in Alagoas State, Brazil. Cad. Saude Publica 2021, 36, e00032020. [Google Scholar] [CrossRef]
- Acharya, B.K.; Cao, C.; Xu, M.; Chen, W.; Pandit, S. Spatiotemporal Distribution and Geospatial Diffusion Patterns of 2013 Dengue Outbreak in Jhapa District, Nepal. Asia Pac. J. Public Health 2018, 30, 396–405. [Google Scholar] [CrossRef]
- Carvalho, F.R.; Medeiros, T.; Vianna, R.A.D.O.; Douglass-Jaimes, G.; Nunes, P.C.G.; Quintans, M.D.S.; Souza, C.F.; Cavalcanti, S.M.B.; dos Santos, F.B.; de Oliveira, S.A.; et al. Simultaneous Circulation of Arboviruses and Other Congenital Infections in Pregnant Women in Rio de Janeiro, Brazil. Acta Trop. 2019, 192, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Costa, S.D.S.B.; Branco, M.D.R.F.C.; Aquino Junior, J.; Rodrigues, Z.M.R.; Queiroz, R.C.D.S.; Araujo, A.S.; Câmara, A.P.B.; dos Santos, P.S.; Pereira, E.D.A.; Silva, M.D.S.D.; et al. Spatial Analysis of Probable Cases of Dengue Fever, Chikungunya Fever and Zika Virus Infections in Maranhao State, Brazil. Rev. Inst. Med. Trop. São Paulo 2018, 60, e62. [Google Scholar] [CrossRef] [PubMed]
- Freitas, L.P.; Cruz, O.G.; Lowe, R.; Sá Carvalho, M. Space–Time Dynamics of a Triple Epidemic: Dengue, Chikungunya and Zika Clusters in the City of Rio de Janeiro. Proc. R. Soc. B Biol. Sci. 2019, 286, 20191867. [Google Scholar] [CrossRef] [PubMed]
- Albuquerque, M.S.V.; Lyra, T.M.; Melo, A.P.L.; Valongueiro, S.A.; Araújo, T.V.B.; Pimentel, C.; Moreira, M.C.N.; Mendes, C.H.F.; Nascimento, M.; Kuper, H.; et al. Access to Healthcare for Children with Congenital Zika Syndrome in Brazil: Perspectives of Mothers and Health Professionals. Health Policy Plan. 2019, 34, 499–507. [Google Scholar] [CrossRef] [PubMed]
- Duarte, J.D.S.; Santos, L.O.F.; Sette, G.C.S.; Santos, T.D.F.C.; Alves, F.A.P.; Coriolano-Marinus, M.W.D.L.; Duarte, J.D.S.; Santos, L.O.F.; Sette, G.C.S.; Santos, T.D.F.C.; et al. Necessidades de crianças com síndrome congênita pelo Zika vírus no contexto domiciliar. Cad. Saúde Coletiva 2019, 27, 249–256. [Google Scholar] [CrossRef]
- Freitas, P.D.S.S.; Soares, G.B.; Mocelin, H.J.S.; Lacerda, L.C.X.; do Prado, T.N.; Sales, C.M.M.; Perez, F.; Bussinger, E.C.D.A.; Maciel, E.L.N. Congenital Zika syndrome: Sociodemographic profile of mothersSindrome congenito por el virus del Zika: Perfil sociodemografico de las madres. Rev. Panam. Salud Publica Pan Am. J. Public Health 2019, 43, e24. [Google Scholar] [CrossRef] [PubMed]
- Mendes, A.G. Enfrentando Uma Nova Realidade a Partir Da Síndrome Congênita Do Vírus Zika: A Perspectiva Das Famílias. Available online: http://www.cienciaesaudecoletiva.com.br/artigos/enfrentando-uma-nova-realidade-a-partir-da-sindrome-congenita-do-virus-zika-a-perspectiva-das-familias/17145?id=17145 (accessed on 16 February 2020).
- Souza, M.P.A.; da Natividade, M.S.; Werneck, G.L.; Dos Santos, D.N. Congenital Zika Syndrome and Living Conditions in the Largest City of Northeastern Brazil. BMC Public Health 2022, 22, 1231. [Google Scholar] [CrossRef] [PubMed]
- Cavallieri, F. Índice de Desenvolvimento Social. Available online: https://www.rio.rj.gov.br/dlstatic/10112/6165511/4162027/analise_ids_rio_compur.pdf (accessed on 27 April 2020).
- ISP Letalidade Violenta. Available online: https://www.ispvisualizacao.rj.gov.br/Letalidade.html (accessed on 22 March 2020).
- Cunha, L.S.; Medeiros, W.R.; Lima Junior, F.A.V.; Pereira, S.A. Relação dos indicadores de desigualdade social na distribuição espacial dos casos de Zika Vírus. Ciênc. Saúde Coletiva 2020, 25, 1839–1850. [Google Scholar] [CrossRef] [PubMed]
- Akter, R.; Naish, S.; Gatton, M.; Bambrick, H.; Hu, W.; Tong, S. Spatial and Temporal Analysis of Dengue Infections in Queensland, Australia: Recent Trend and Perspectives. PLoS ONE 2019, 14, e0220134. [Google Scholar] [CrossRef]
- Li, J.; Jia, K.; Liu, Y.; Yuan, B.; Xia, M.; Zhao, W. Spatiotemporal Distribution of Zika Virus and Its Spatially Heterogeneous Relationship with the Environment. Int. J. Environ. Res. Public. Health 2021, 18, 290. [Google Scholar] [CrossRef]
- Banu, S.; Hu, W.; Hurst, C.; Guo, Y.; Islam, M.Z.; Tong, S. Space-Time Clusters of Dengue Fever in Bangladesh. Trop. Med. Int. Health 2012, 17, 1086–1091. [Google Scholar] [CrossRef] [PubMed]
- Cofré, F.; Delpiano, L.; Labraña, Y.; Reyes, A.; Sandoval, A.; Izquierdo, G. Síndrome de TORCH: Enfoque Racional Del Diagnóstico y Tratamiento Pre y Post Natal.: Recomendaciones Del Comité Consultivo de Infecciones Neonatales Sociedad Chilena de Infectología, 2016. Rev. Chil. Obstet. Ginecol. 2017, 82, 171–211. [Google Scholar] [CrossRef]
- Mussi-Pinhata, M.M.; Yamamoto, A.Y. Infecções congênitas e perinatais. J. Pediatr. 1999, 75 (Suppl. S1), 15–30. [Google Scholar] [CrossRef] [PubMed]
- de Barros, S.M.M.; Monteiro, P.A.L.; Neves, M.B.; Maciel, G.T.D.S. Fortalecendo a rede de apoio de mães no contexto da síndrome congênita do vírus Zika: Relatos de uma intervenção psicossocial e sistêmica. Nova Perspect. Sistêmica 2017, 26, 38–59. [Google Scholar]
- Diniz, D. Zika virus and women. Cad. Saude Publica 2016, 32, e00046316. [Google Scholar] [CrossRef]

| Mother Characteristics | |||||
| Neighborhood Residence (PA) | n | % | Pregnancy in Which Zika Infection Occurred (Trimester) | n | % |
| 1 | 5 | 11 | First | 35 | 75 |
| 2 | 3 | 6 | Second | 6 | 13 |
| 3 | 20 | 43 | Third | 1 | 2 |
| 4 | 4 | 9 | Ignored | 5 | 11 |
| 5 | 15 | 32 | |||
| Total | 47 | 100 | |||
| Age (years) | n | % | Race/color | n | % |
| ≤20 | 6 | 13 | Non-White | 27 | 58 |
| 21 to 30 | 22 | 47 | White | 19 | 40 |
| 31 to 40 | 16 | 34 | Ignored | 1 | 2 |
| >40 | 3 | 6 | |||
| Children with CZS characteristics | |||||
| Gestational age at birth | n | % | Weight | n | % |
| Term | 34 | 72 | <2500 g | 20 | 43 |
| Premature | 13 | 28 | 2500 g or more | 27 | 57 |
| Height | n | % | Cephalic perimeter | n | % |
| <48 cm | 34 | 72 | <31.5 cm | 38 | 81 |
| 48 cm or more | 13 | 28 | >31.5 | 7 | 15 |
| Ignored | 2 | 4 | |||
| Z-score | n | % | Evolution | n | % |
| <−3 | 23 | 49 | In follow-up | 41 | 87 |
| −2 to −3 | 7 | 15 | Death | 6 | 13 |
| −1.9 to 1.9 | 7 | 15 | Early neonatal | 1 | |
| 2 to 3 | 1 | 2 | Late neonatal | 1 | |
| Ignored | 9 | 19 | Post-neonatal | 4 | |
| Congenital abnormalities | n | % | |||
| Brain | 42 | 89 | |||
| Microcephaly | 40 | 85 | |||
| Osteoarticular | 9 | 19 | |||
| Ocular | 9 | 19 | |||
| Auditory | 7 | 15 | |||
| Development | 7 | 15 | |||
| Hydrocephalus | 6 | 13 | |||
| Kidneys | 3 | 6 | |||
| Uterine growth restriction | 3 | 6 | |||
| Hepatosplenomegaly | 3 | 6 | |||
| Lungs | 2 | 4 | |||
| Cardiac | 1 | 2 | |||
| Liver | 1 | 2 | |||
| Final diagnosis | n | % | |||
| Microcephaly, brain changes, and changes in other systems | 20 | 43 | |||
| Microcephaly and brain changes | 21 | 45 | |||
| No microcephaly, with other congenital changes. | 6 | 13 | |||
| PA | CZS | Social Development Index | |||||
|---|---|---|---|---|---|---|---|
| Districts | Average | SD | Median | Minimum | Maximum | ||
| 1 | 5 | 15 | 0.59 | 0.03 | 0.60 | 0.54 | 0.64 |
| 2 | 3 | 25 | 0.71 | 0.07 | 0.72 | 0.53 | 0.82 |
| 3 | 20 | 80 | 0.60 | 0.04 | 0.59 | 0.50 | 0.72 |
| 4 | 4 | 19 | 0.60 | 0.11 | 0.59 | 0.28 | 0.77 |
| 5 | 15 | 21 | 0.56 | 0.05 | 0.56 | 0.49 | 0.70 |
| Total | 47 | 160 | 0.61 | 0.07 | 0.59 | 0.28 | 0.82 |
| Cluster 1 | Cluster 2 | Cluster 3 | |
|---|---|---|---|
| Radius | 1.47 km | 4.11 km | 4.25 km |
| Live births (population) | 695 | 8630 | 3463 |
| CZS | 3 | 7 | 4 |
| Relative risk | 7.86 | 1.46 | 2.08 |
| Likelihood ratio | 3,490,937 | 3,482,130 | 2,894,695 |
| p-value | 0.71 | 0.71 | 0.84 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Freitas, D.A.d.; Wakimoto, M.D.; Dias, S.; Souza-Santos, R. High-Risk Areas for Congenital Zika Syndrome in Rio de Janeiro: Spatial Cluster Detection. Trop. Med. Infect. Dis. 2024, 9, 105. https://doi.org/10.3390/tropicalmed9050105
Freitas DAd, Wakimoto MD, Dias S, Souza-Santos R. High-Risk Areas for Congenital Zika Syndrome in Rio de Janeiro: Spatial Cluster Detection. Tropical Medicine and Infectious Disease. 2024; 9(5):105. https://doi.org/10.3390/tropicalmed9050105
Chicago/Turabian StyleFreitas, Danielle Amaral de, Mayumi Duarte Wakimoto, Sónia Dias, and Reinaldo Souza-Santos. 2024. "High-Risk Areas for Congenital Zika Syndrome in Rio de Janeiro: Spatial Cluster Detection" Tropical Medicine and Infectious Disease 9, no. 5: 105. https://doi.org/10.3390/tropicalmed9050105
APA StyleFreitas, D. A. d., Wakimoto, M. D., Dias, S., & Souza-Santos, R. (2024). High-Risk Areas for Congenital Zika Syndrome in Rio de Janeiro: Spatial Cluster Detection. Tropical Medicine and Infectious Disease, 9(5), 105. https://doi.org/10.3390/tropicalmed9050105







