A Short Review on Chondroitin Sulphate and Its Based Nanomaterials for Bone Repair and Bone Remodelling Applications
Abstract
:1. Introduction
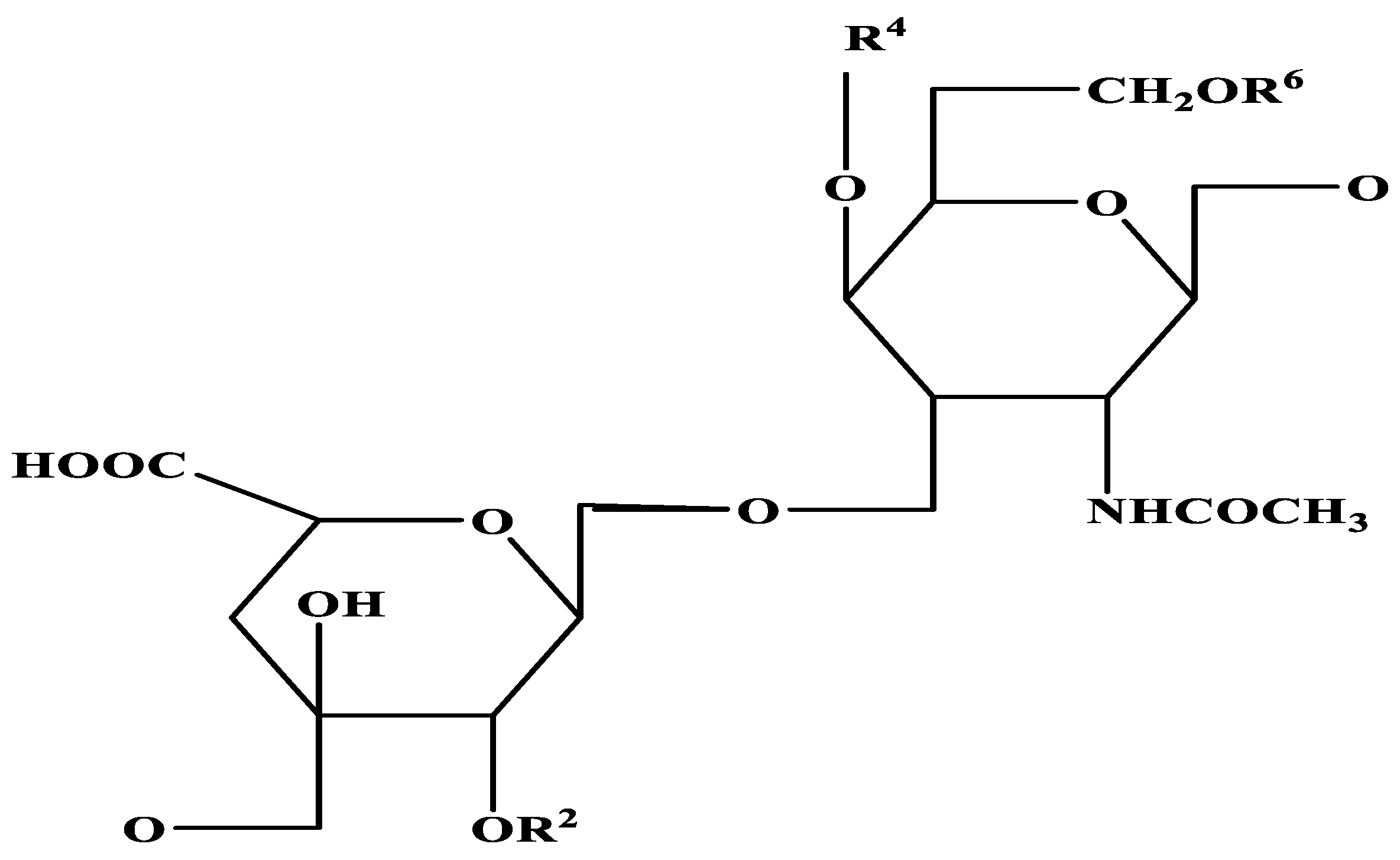
2. Structure of Chondroitin Sulphate
3. Chondroitin Sulphate Based Nanoparticle Production
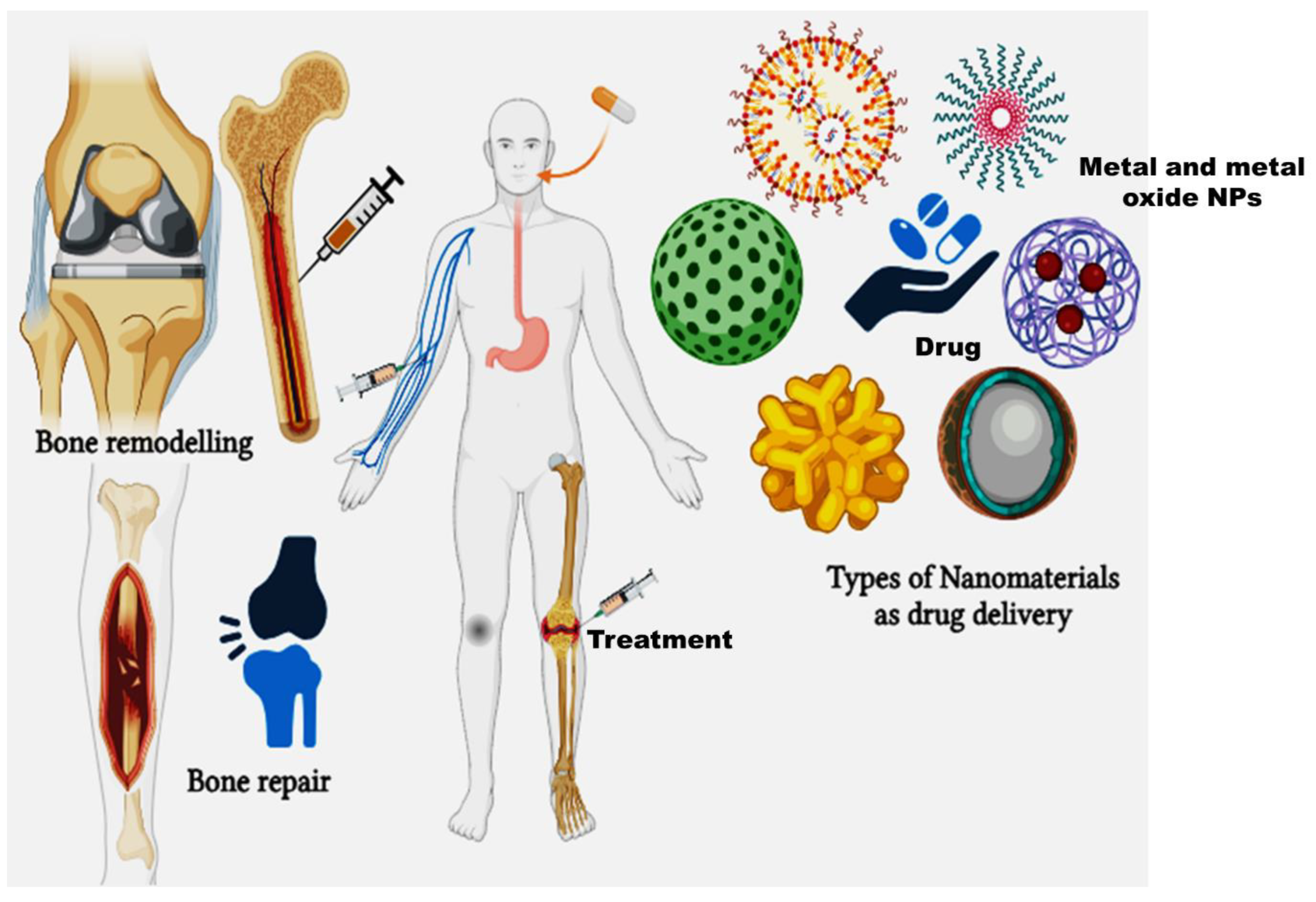
3.1. Drug Delivery and Biomedical Application
| S.No | Combination of Biomaterials and Chondroitin Sulphate | Application | References |
|---|---|---|---|
| 1. | Titanium coated type I collagen and chondroitin sulphate | Cellular reaction and New Bone Formation | [55] |
| 2. | Glucosamine and Chondroitin sulphate | Cartilage regeneration microfracture or autologous chondrocyte transplantation | [56] |
| 3. | Carboxymethylated Pullulan/Chondroitin Sulphate Hydrogel | Regenerating cartilage tissue | [57] |
| 4. | N-acetyl glucosamine and chondroitin sulphate | Japanese adults with knee pain and/or stiffness | [58] |
| 5. | Chondroitin sulphate and hyaluronic acid | Clinical trial studies in tendon ruptures | [59] |
| 6. | Bedaquiline fumarate BDQ loaded Chondroitin Sulphate Modified PLGA NPs | Invitro drug release | [60] |
| 7. | Gelatin-chondroitin sulphate/polycaprolactone nanofibrous scaffolds | Chondrogenesis differentiation, cartilage tissue engineering application | [61] |
| 8. | Chondroitin sulphate micro granules embedded with oligochitosan-calcium complexes | Osteoporosis in OVX rats | [62] |
| 9. | photo-cross-linkable methacryloyl groups microgels anchored with liquiritin loaded liposomes | Osteoarthritis treatment | [43] |
| 10. | Extracellular matrices based on collagen and chondroitin sulphate | Bone remodelling and de novo bone formation in vivo | [63] |
| 11. | Silk fibroin/chondroitin sulphate/hyaluronic acid ternary scaffolds | Dermal tissue regeneration | [64] |
| 12. | Hyaluronic acid, chondroitin 6 sulphate and dermatan sulphate | Healing bone regenerate bone in defect model | [65] |
| 13. | Electrospun fiber membranes by LbL-collagen/ chondroitin sulphate nanocoating | Bone repair and regeneration | [66] |
| 14. | Biomimetic synthesis of chondroitin sulphate-analogue hydrogels | Potential bone and cartilage regeneration | [67] |
| 15. | Chondroitin sulphate/poly(vinyl alcohol)/bovine bone powder porous biocomposite | Potential skin tissue and bone tissue engineering | [68] |
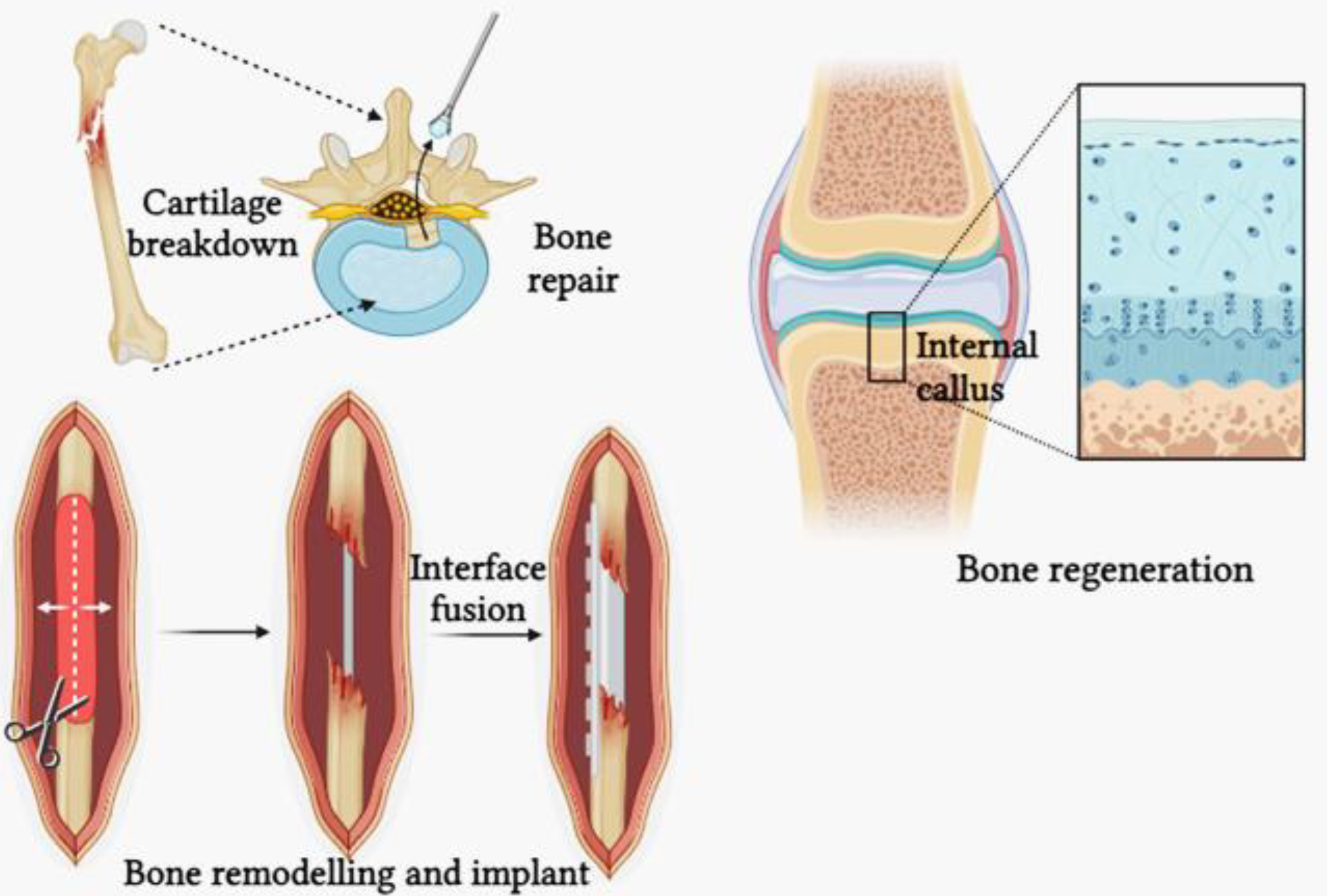
3.2. Bone Repair and Remodelling
4. Summary
5. Future Trends
6. Pros and Cons of the Study
7. Limitations of the Study
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Xu, L.; Ma, F.; Leung, F.K.L.; Qin, C.; Lu, W.W.; Tang, B. Chitosan-strontium chondroitin sulfate scaffolds for reconstruction of bone defects in aged rats. Carbohydr. Polym. 2021, 273, 118532. [Google Scholar] [CrossRef] [PubMed]
- Kubo, M.; Ando, K.; Mimura, T.; Matsusue, Y.; Mori, K. Chondroitin sulfate for the treatment of hip and knee osteoarthritis: Current status and future trends. Life Sci. 2009, 85, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Yunus Basha, R.; Sampath, S.K.; Doble, M. Design of biocomposite materials for bone tissue regeneration. Mater. Sci. Eng. C 2015, 57, 452–463. [Google Scholar] [CrossRef] [PubMed]
- Kandiah, K.; Venkatachalam, R.; Wang, C.; Valiyaveettil, S.; Ganesan, K. In vitro and preliminary in vivo toxicity screening of high-surface-area TiO2-chondroitin-4-sulfate nanocomposites for bone regeneration application. Colloids Surf. B Biointerfaces 2015, 128, 347–356. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Chen, J.; Fan, T.; Zhang, Y.; Zhao, Y.; Shi, X.; Zhang, Q. Biomimetic mineralized hierarchical hybrid scaffolds based on in situ synthesis of nano-hydroxyapatite/chitosan/chondroitin sulfate/hyaluronic acid for bone tissue engineering. Colloids Surf. B Biointerfaces 2017, 157, 93–100. [Google Scholar] [CrossRef]
- Yang, J.; Shen, M.; Wen, H.; Luo, Y.; Huang, R.; Rong, L.; Xie, J. Recent advance in delivery system and tissue engineering applications of chondroitin sulfate. Carbohydr. Polym. 2020, 230, 115650. [Google Scholar] [CrossRef]
- Cheng, K.M.; Hung, Y.W.; Chen, C.C.; Liu, C.C.; Young, J.J. Green synthesis of chondroitin sulfate-capped silver nanoparticles: Characterization and surface modification. Carbohydr. Polym. 2014, 110, 195–202. [Google Scholar] [CrossRef]
- Henrotin, Y.; Marty, M.; Mobasheri, A. What is the current status of chondroitin sulfate and glucosamine for the treatment of knee osteoarthritis? Maturitas 2014, 78, 184–187. [Google Scholar] [CrossRef]
- Zhou, L.; Fan, L.; Zhang, F.M.; Jiang, Y.; Cai, M.; Dai, C.; Luo, Y.A.; Tu, L.J.; Zhou, Z.N.; Li, X.J.; et al. Hybrid gelatin/oxidized chondroitin sulfate hydrogels incorporating bioactive glass nanoparticles with enhanced mechanical properties, mineralization, and osteogenic differentiation. Bioact. Mater. 2021, 6, 890–904. [Google Scholar] [CrossRef]
- Muzzarelli, R.A.A.; Greco, F.; Busilacchi, A.; Sollazzo, V.; Gigante, A. Chitosan, hyaluronan and chondroitin sulfate in tissue engineering for cartilage regeneration: A review. Carbohydr. Polym. 2012, 89, 723–739. [Google Scholar] [CrossRef]
- Young, J.J.; Cheng, K.M.; Young, Y.A.; Chen, X.A.; Chen, Y.H.; Chang, T.Y.; Yen, H.J.; Chen, C.C. Chondroitin sulfate-stabilized silver nanoparticles: Improved synthesis and their catalytic, antimicrobial, and biocompatible activities. Carbohydr. Res. 2018, 457, 14–24. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Liu, M.; Wang, J.; Zhai, G. Chondroitin sulfate-based nanocarriers for drug/gene delivery. Carbohydr. Polym. 2015, 133, 391–399. [Google Scholar] [CrossRef] [PubMed]
- Meng, D.; Leng, X.; Zhang, Y.; Luo, J.; Du, H.; Takagi, Y.; Dai, Z.; Wei, Q. Comparation of the structural characteristics and biological activities of chondroitin sulfates extracted from notochord and backbone of Chinese sturgeon (Acipenser sinensis). Carbohydr. Res. 2022, 522, 108685. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.T.; Dang, L.H.; Nguyen, P.; Pham, T.L.B.; Le, H.K.; Nguyen, M.T.; Nhi, T.T.Y.; Feng, S.; Chen, J.; Tran, N.Q. Dual composition Chondroitin Sulfate and gelatin biomimetic hydrogel based on tyramine crosslinking for tissue regenerative medicine. Eur. Polym. J. 2023, 189, 111975. [Google Scholar] [CrossRef]
- Nair, M.B.; Baranwal, G.; Vijayan, P.; Keyan, K.S.; Jayakumar, R. Composite hydrogel of chitosan-poly(hydroxybutyrate-co-valerate) with chondroitin sulfate nanoparticles for nucleus pulposus tissue engineering. Colloids Surf. B Biointerfaces 2015, 136, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Abdallah, M.M.; Fernández, N.; Matias, A.A.; do Bronze, M.R. Hyaluronic acid and Chondroitin sulfate from marine and terrestrial sources: Extraction and purification methods. Carbohydr. Polym. 2020, 243, 116441. [Google Scholar] [CrossRef]
- Cimini, D.; Bedini, E.; Schiraldi, C. Biotechnological advances in the synthesis of modified chondroitin towards novel biomedical applications. Biotechnol. Adv. 2023, 67, 108185. [Google Scholar] [CrossRef]
- Wytrwal, M.; Szmajnta, K.; Kucharski, M.; Nowak, J.; Oclon, E.; Kepczynski, M. Kartogenin-loaded liposomes coated with alkylated chondroitin sulfate for cartilage repair. Int. J. Pharm. 2023, 646, 123436. [Google Scholar] [CrossRef]
- Xi, J.; Zhou, L.; Dai, H. Drug-loaded chondroitin sulfate-based nanogels: Preparation and characterization. Colloids Surf. B Biointerfaces 2012, 100, 107–115. [Google Scholar] [CrossRef]
- Kandiah, K.; Duraisamy, N.; Amirthalingam, V.; Ramasamy, B. Scavenging free radicals and soaring osteoinduction by extra cellular matrix protein–based nanocomposites on degenerative bone treatments. Mater. Sci. Eng. C 2017, 77, 1189–1195. [Google Scholar] [CrossRef]
- Radwan-Oczko, M.; Dus-Ilnicka, I.; Richards, P.; Thomsen, A.M.; Rasmussen, C. Evaluation of oral health status and oral care of patients with rheumatoid arthritis. Int. J. Dent. 2020, 2020, 8896766. [Google Scholar] [CrossRef] [PubMed]
- Radwan-Oczko, M.; Duś-Ilnicka, I.; Richards, P.; Thomsen, A.M.; Rasmussen, C. Rheumatoid arthritis patients’ oral health and disease activity. Int. J. Rheum. Dis. 2019, 22, 1538–1543. [Google Scholar] [CrossRef] [PubMed]
- Wiȩckiewicz, M.; Paradowska, A.; Kawala, B.; Wiȩckiewicz, W. SAPHO syndrome as a possible cause of masticatory system anomalies—A review of the literature. Adv. Clin. Exp. Med. 2011, 20, 521–525. [Google Scholar]
- Sharma, R.; Kuche, K.; Thakor, P.; Bhavana, V.; Srivastava, S.; Mehra, N.K.; Jain, S. Chondroitin Sulfate: Emerging biomaterial for biopharmaceutical purpose and tissue engineering. Carbohydr. Polym. 2022, 286, 119305. [Google Scholar] [CrossRef] [PubMed]
- Mahtab, A.; Rabbani, S.A.; Neupane, Y.R.; Pandey, S.; Ahmad, A.; Khan, M.A.; Gupta, N.; Madaan, A.; Jaggi, M.; Sandal, N.; et al. Facile functionalization of Teriflunomide-loaded nanoliposomes with Chondroitin sulphate for the treatment of Rheumatoid arthritis. Carbohydr. Polym. 2020, 250, 116926. [Google Scholar] [CrossRef] [PubMed]
- Suganya, P.; Vaseeharan, B.; Vijayakumar, S.; Balan, B.; Govindarajan, M.; Alharbi, N.S.; Kadaikunnan, S.; Khaled, J.M.; Benelli, G. Biopolymer zein-coated gold nanoparticles: Synthesis, antibacterial potential, toxicity and histopathological effects against the Zika virus vector Aedes aegypti. J. Photochem. Photobiol. B Biol. 2017, 173, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Sattelle, B.M.; Shakeri, J.; Roberts, I.S.; Almond, A. A 3D-structural model of unsulfated chondroitin from high-field NMR: 4-sulfation has little effect on backbone conformation. Carbohydr. Res. 2010, 345, 291–302. [Google Scholar] [CrossRef]
- Valcarcel, J.; García, M.R.; Sampayo, L.F.; Vázquez, J.A. Marine chondroitin sulfate of defined molecular weight by enzymatic depolymerization. Carbohydr. Polym. 2020, 229, 115450. [Google Scholar] [CrossRef]
- Zhang, W.; Xu, R.; Chen, J.; Xiong, H.; Wang, Y.; Pang, B.; Du, G.; Kang, Z. Advances and challenges in biotechnological production of chondroitin sulfate and its oligosaccharides. Int. J. Biol. Macromol. 2023, 253, 126551. [Google Scholar] [CrossRef]
- Zheng, K.; Bai, J.; Yang, H.; Xu, Y.; Pan, G.; Wang, H.; Geng, D. Nanomaterial-assisted theranosis of bone diseases. Bioact. Mater. 2023, 24, 263–312. [Google Scholar] [CrossRef]
- Leite, Á.J.; Sher, P.; Mano, J.F. Chitosan/chondroitin sulfate multilayers as supports for calcium phosphate biomineralization. Mater. Lett. 2014, 121, 62–65. [Google Scholar] [CrossRef]
- Yu, Z.; Yu, D.; Dong, J.; Xia, W. Ultrasound-reinforced encapsulation of proanthocyanidin by chitosan-chondroitin sulfate nanosystem. Food Hydrocoll. 2022, 132, 107872. [Google Scholar] [CrossRef]
- Carvalho, D.N.; Gelinsky, M.; Williams, D.S.; Mearns-Spragg, A.; Reis, R.L.; Silva, T.H. Marine collagen-chitosan-fucoidan/chondroitin sulfate cryo-biomaterials loaded with primary human cells envisaging cartilage tissue engineering. Int. J. Biol. Macromol. 2023, 241, 124510. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Ma, F.; Pang, X.; Tang, B.; Lin, L. Synthesis of chondroitin sulfate magnesium for osteoarthritis treatment. Carbohydr. Polym. 2019, 212, 387–394. [Google Scholar] [CrossRef] [PubMed]
- Keskin, D.S.; Tezcaner, A.; Korkusuz, P.; Korkusuz, F.; Hasirci, V. Collagen-chondroitin sulfate-based PLLA-SAIB-coated rhBMP-2 delivery system for bone repair. Biomaterials 2005, 26, 4023–4034. [Google Scholar] [CrossRef]
- Rammelt, S.; Illert, T.; Bierbaum, S.; Scharnweber, D.; Zwipp, H.; Schneiders, W. Coating of titanium implants with collagen, RGD peptide and chondroitin sulfate. Biomaterials 2006, 27, 5561–5571. [Google Scholar] [CrossRef]
- Wang, S.; Ji, X.; Chen, S.; Zhang, C.; Wang, Y.; Lin, H.; Zhao, L. Study of double-bonded carboxymethyl chitosan/cysteamine-modified chondroitin sulfate composite dressing for hemostatic application. Eur. Polym. J. 2022, 162, 110875. [Google Scholar] [CrossRef]
- Yahya, R.; Alharbi, N.M. Biosynthesized silver nanoparticles-capped chondroitin sulfate nanogel targeting microbial infections and biofilms for biomedical applications. Int. J. Biol. Macromol. 2023, 253, 127080. [Google Scholar] [CrossRef]
- Han, J.; Deng, H.; Li, Y.; Qiao, L.; Jia, H.; Zhang, L.; Wang, L.; Qu, C. Nano-elemental selenium particle developed via supramolecular self-assembly of chondroitin sulfate A and Na2SeO3 to repair cartilage lesions. Carbohydr. Polym. 2023, 316, 121047. [Google Scholar] [CrossRef]
- Holmborn, K.; Habicher, J.; Kasza, Z.; Eriksson, A.S.; Filipek-Gorniok, B.; Gopal, S.; Couchman, J.R.; Ahlberg, P.E.; Wiweger, M.; Spillmann, D.; et al. On the roles and regulation of chondroitin sulfate and heparan sulfate in zebrafish pharyngeal cartilage morphogenesis. J. Biol. Chem. 2012, 287, 33905–33916. [Google Scholar] [CrossRef]
- Lopes, D.; Martins-Cruz, C.; Oliveira, M.B.; Mano, J.F. Bone physiology as inspiration for tissue regenerative therapies. Biomaterials 2018, 185, 240–275. [Google Scholar] [CrossRef] [PubMed]
- Dinoro, J.; Maher, M.; Talebian, S.; Jafarkhani, M.; Mehrali, M.; Orive, G.; Foroughi, J.; Lord, M.S.; Dolatshahi-Pirouz, A. Sulfated polysaccharide-based scaffolds for orthopaedic tissue engineering. Biomaterials 2019, 214, 119214. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Sun, M.; Wang, J.; Yang, X.; Lin, C.; Ge, L.; Ying, C.; Xu, K.; Liu, A.; Wu, L. Chondroitin sulfate microspheres anchored with drug-loaded liposomes play a dual antioxidant role in the treatment of osteoarthritis. Acta Biomater. 2022, 151, 512–527. [Google Scholar] [CrossRef] [PubMed]
- Han, J.; Guo, X.; Lei, Y.; Dennis, B.S.; Wu, S.; Wu, C. Synthesis and characterization of selenium-chondroitin sulfate nanoparticles. Carbohydr. Polym. 2012, 90, 122–126. [Google Scholar] [CrossRef]
- Anisha, B.S.; Sankar, D.; Mohandas, A.; Chennazhi, K.P.; Nair, S.V.; Jayakumar, R. Chitosan-hyaluronan/nano chondroitin sulfate ternary composite sponges for medical use. Carbohydr. Polym. 2013, 92, 1470–1476. [Google Scholar] [CrossRef]
- Shimojo, A.A.M.; Perez, A.G.M.; Galdames, S.E.M.; Brissac, I.C.S.; Santana, M.H.A. Stabilization of porous chitosan improves the performance of its association with platelet-rich plasma as a composite scaffold. Mater. Sci. Eng. C 2016, 60, 538–546. [Google Scholar] [CrossRef] [PubMed]
- Raeissadat, S.A.; Babaee, M.; Rayegani, S.M.; Hashemi, Z.; Hamidieh, A.A.; Mojgani, P.; Vanda, H.F. An overview of platelet products (PRP, PRGF, PRF, etc.) in the Iranian studies. Futur. Sci. OA 2017, 3, FSO231. [Google Scholar] [CrossRef] [PubMed]
- KhaliliJafarabad, N.; Behnamghader, A.; Khorasani, M.T.; Mozafari, M. Platelet-rich plasma-hyaluronic acid/chondrotin sulfate/carboxymethyl chitosan hydrogel for cartilage regeneration. Biotechnol. Appl. Biochem. 2022, 69, 534–547. [Google Scholar] [CrossRef]
- Thomas, V.; Mercuri, J. In vitro and in vivo Efficacy of Naturally Derived Scaffolds for Cartilage Repair and Regeneration. Acta Biomater. 2023, 171, 1–18. [Google Scholar] [CrossRef]
- Zhu, Y.; Zhao, T.; Liu, M.; Wang, S.; Liu, S.; Yang, Y.; Yang, Y.; Nan, Y.; Huang, Q.; Ai, K. Rheumatoid arthritis microenvironment insights into treatment effect of nanomaterials. Nano Today 2022, 42, 101358. [Google Scholar] [CrossRef]
- Guo, L.; Chen, H.; Li, Y.; Zhou, J.; Chen, J. Biocompatible scaffolds constructed by chondroitin sulfate microspheres conjugated 3D-printed frameworks for bone repair. Carbohydr. Polym. 2023, 299, 120188. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.; Mishra, S.K.; Vuddanda, P.R.; Singh, S.K.; Singh, R.; Singh, S. Targeting of diacerein loaded lipid nanoparticles to intra-articular cartilage using chondroitin sulfate as homing carrier for treatment of osteoarthritis in rats. Nanomed. Nanotechnol. Biol. Med. 2014, 10, e1031–e1040. [Google Scholar] [CrossRef] [PubMed]
- Rani, A.; Baruah, R.; Goyal, A. Physicochemical, antioxidant and biocompatible properties of chondroitin sulphate isolated from chicken keel bone for potential biomedical applications. Carbohydr. Polym. 2017, 159, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Fenbo, M.; Xingyu, X.; Bin, T. Strontium chondroitin sulfate/silk fibroin blend membrane containing microporous structure modulates macrophage responses for guided bone regeneration. Carbohydr. Polym. 2019, 213, 266–275. [Google Scholar] [CrossRef] [PubMed]
- Rammelt, S.; Heck, C.; Bernhardt, R.; Bierbaum, S.; Scharnweber, D.; Goebbels, J.; Ziegler, J.; Biewener, A.; Zwipp, H. In vivo effects of coating loaded and unloaded Ti implants with collagen, chondroitin sulfate, and hydroxyapatite in the sheep tibia. J. Orthop. Res. 2007, 25, 1052–1061. [Google Scholar] [CrossRef] [PubMed]
- DiNubile, N.A. Glucosamine and chondroitin sulfate in the management of osteoarthritis. Postgrad. Med. 2009, 121, 48–50. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; Yu, S.; Liu, B.; Ni, Y.; Yu, C.; Su, Y.; Zhu, X.; Yu, X.; Zhou, Y.; Yan, D. An Injectable Enzymatically Crosslinked Carboxymethylated Pullulan/Chondroitin Sulfate Hydrogel for Cartilage Tissue Engineering. Sci. Rep. 2016, 6, 1–12. [Google Scholar] [CrossRef]
- Tsuji, T.; Yoon, J.; Kitano, N.; Okura, T.; Tanaka, K. Effects of N-acetyl glucosamine and chondroitin sulfate supplementation on knee pain and self-reported knee function in middle-aged and older Japanese adults: A randomized, double-blind, placebo-controlled trial. Aging Clin. Exp. Res. 2016, 28, 197–205. [Google Scholar] [CrossRef]
- Yudistira, A.; Risantoso, T.; Asmiragani, S.; Basunanda, T.A.; Putera, M.A. Combination of chondroitin sulfate and hyaluronic acid increases amount of fibroblast, collagen and decreases adhesion of achilles tendon after repair. J. Arthrosc. Jt. Surg. 2020, 7, 211–215. [Google Scholar] [CrossRef]
- Mazahir, F.; Sahoo, R.K.; Gupta, U.; Yadav, A.K. Chondroitin sulfate anchored biodegradable nanoparticles: Design, synthesis, and in-vitro anti-tubercular efficacy. Mater. Today Commun. 2023, 34, 105364. [Google Scholar] [CrossRef]
- Sharifi, F.; Irani, S.; Azadegan, G.; Pezeshki-Modaress, M.; Zandi, M.; Saeed, M. Co-electrospun gelatin-chondroitin sulfate/polycaprolactone nanofibrous scaffolds for cartilage tissue engineering. Bioact. Carbohydr. Diet. Fibre 2020, 22, 100215. [Google Scholar] [CrossRef]
- Chen, L.; Li, J.; Bi, X.; Ji, J.; Wang, L.; Cheng, J. Chondroitin sulfate micro granules embedded with oligochitosan-calcium complexes for potential osteoporosis prevention. J. Funct. Foods 2022, 90, 104984. [Google Scholar] [CrossRef]
- Dudeck, J.; Rehberg, S.; Bernhardt, R.; Schneiders, W.; Zierau, O.; Inderchand, M.; Goebbels, J.; Vollmer, G.; Fratzl, P.; Scharnweber, D.; et al. Increased bone remodelling around titanium implants coated with chondroitin sulfate in ovariectomized rats. Acta Biomater. 2014, 10, 2855–2865. [Google Scholar] [CrossRef] [PubMed]
- Yan, S.; Zhang, Q.; Wang, J.; Liu, Y.; Lu, S.; Li, M.; Kaplan, D.L. Silk fibroin/chondroitin sulfate/hyaluronic acid ternary scaffolds for dermal tissue reconstruction. Acta Biomater. 2013, 9, 6771–6782. [Google Scholar] [CrossRef] [PubMed]
- Zanchetta, P.; Lagarde, N.; Uguen, A.; Marcorelles, P. Mixture of hyaluronic acid, chondroitin 6 sulphate and dermatan sulphate used to completely regenerate bone in rat critical size defect model. J. Cranio-Maxillofac. Surg. 2012, 40, 783–787. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.; Rahman, N.; Li, L.; Zhang, J.; Tan, H.; Xue, Y.; Zhao, Y.; Zhai, J.; Zhao, N.; Xu, F.; et al. Biofunctionalization of electrospun fiber membranes by LbL-collagen/chondroitin sulfate nanocoating followed by mineralization for bone regeneration. Mater. Sci. Eng. C 2021, 128, 112295. [Google Scholar] [CrossRef] [PubMed]
- Cheng, K.; Zhu, Y.; Wang, D.; Li, Y.; Xu, X.; Cai, H.; Chu, H.; Li, J.; Zhang, D. Biomimetic synthesis of chondroitin sulfate-analogue hydrogels for regulating osteogenic and chondrogenic differentiation of bone marrow mesenchymal stem cells. Mater. Sci. Eng. C 2020, 117, 111368. [Google Scholar] [CrossRef] [PubMed]
- da Silva, G.T.; Voss, G.T.; Kaplum, V.; Nakamura, C.V.; Wilhelm, E.A.; Luchese, C.; Fajardo, A.R. Development, characterization and biocompatibility of chondroitin sulfate/poly(vinyl alcohol)/bovine bone powder porous biocomposite. Mater. Sci. Eng. C 2017, 72, 526–535. [Google Scholar] [CrossRef]
- García-Gareta, E.; Coathup, M.J.; Blunn, G.W. Osteoinduction of bone grafting materials for bone repair and regeneration. Bone 2015, 81, 112–121. [Google Scholar] [CrossRef]
- Brown, A.; Zaky, S.; Ray, H.; Sfeir, C. Porous magnesium/PLGA composite scaffolds for enhanced bone regeneration following tooth extraction. Acta Biomater. 2015, 11, 543–553. [Google Scholar] [CrossRef]
- Li, M.; Yang, X.; Wang, W.; Zhang, Y.; Wan, P.; Yang, K.; Han, Y. Evaluation of the osteo-inductive potential of hollow three-dimensional magnesium-strontium substitutes for the bone grafting application. Mater. Sci. Eng. C 2017, 73, 347–356. [Google Scholar] [CrossRef] [PubMed]
- Lei, C.; Song, J.H.; Li, S.; Zhu, Y.N.; Liu, M.Y.; Wan, M.C.; Mu, Z.; Tay, F.R.; Niu, L.N. Advances in materials-based therapeutic strategies against osteoporosis. Biomaterials 2023, 296, 122066. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Yu, F.; Zheng, L.; Wang, R.; Yan, W.; Wang, Z.; Xu, J.; Wu, J.; Shi, D.; Zhu, L.; et al. Natural hydrogels for cartilage regeneration: Modification, preparation and application. J. Orthop. Transl. 2019, 17, 26–41. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Wu, S.; Chen, W.; Hu, Y.; Geng, Z.; Su, J. Bone/cartilage targeted hydrogel: Strategies and applications. Bioact. Mater. 2023, 23, 156–169. [Google Scholar] [CrossRef] [PubMed]
- Malliappan, S.P.; Yetisgin, A.A.; Sahin, S.B.; Demir, E.; Cetinel, S. Bone tissue engineering: Anionic polysaccharides as promising scaffolds. Carbohydr. Polym. 2022, 283, 119142. [Google Scholar] [CrossRef]
- Henriksen, K.; Neutzsky-Wulff, A.V.; Bonewald, L.F.; Karsdal, M.A. Local communication on and within bone controls bone remodeling. Bone 2009, 44, 1026–1033. [Google Scholar] [CrossRef] [PubMed]
- Evans, C.H. Advances in regenerative orthopedics. Mayo Clin. Proc. 2013, 88, 1323–1339. [Google Scholar] [CrossRef]
- Gaur, A.; Dhillon, M.; Puri, N.; Ahuja, U.S.; Rathore, A. Questionable accuracy of CBCT in determining bone density: A comparative CBCT–CT in vitro study. Dent. Med. Probl. 2022, 59, 413–419. [Google Scholar] [CrossRef]
- Parfitt, A.M. Targeted and nontargeted bone remodeling: Relationship to basic multicellular unit origination and progression. Bone 2002, 30, 5–7. [Google Scholar] [CrossRef]
- Yang, G.; Liu, J.; Li, F.; Pan, Z.; Ni, X.; Shen, Y.; Xu, H.; Huang, Q. Bioactive calcium sulfate/magnesium phosphate cement for bone substitute applications. Mater. Sci. Eng. C 2014, 35, 70–76. [Google Scholar] [CrossRef]
- Rayat Pisheh, H.; Ansari, M.; Eslami, H. How is mechanobiology involved in bone regenerative medicine? Tissue Cell 2022, 76, 101821. [Google Scholar] [CrossRef] [PubMed]
- Soliman, T.; Ali, Z.; Zayed, M.; Sabry, D.; Abubakr, N. Assessing the bone-healing potential of bone marrow mesenchymal stem cells in jawbone osteoporosis in albino rats. Dent. Med. Probl. 2022, 59, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Allen, M.R.; Burr, D.B. Bone Modeling and Remodeling. In Basic and Applied Bone Biology; Academic Press: Cambridge, MA, USA, 2014; pp. 75–90. [Google Scholar] [CrossRef]
- Chalmers, T.C.; Smith, H.; Blackburn, B.; Silverman, B.; Schroeder, B.; Reitman, D.; Ambroz, A. A method for assessing the quality of a randomized control trial. Control. Clin. Trials 1981, 2, 31–49. [Google Scholar] [CrossRef] [PubMed]
- Reichenbach, S.; Sterchi, R.; Scherer, M.; Trelle, S.; Bürgi, E.; Bürgi, U.; Dieppe, P.A.; Jüni, P. Meta-analysis: Chondroitin for osteoarthritis of the knee or hip. Ann. Intern. Med. 2007, 146, 580–590. [Google Scholar] [CrossRef] [PubMed]
- Sivakumar, P.M.; Yetisgin, A.A.; Demir, E.; Sahin, S.B.; Cetinel, S. Polysaccharide-bioceramic composites for bone tissue engineering: A review. Int. J. Biol. Macromol. 2023, 250, 126237. [Google Scholar] [CrossRef] [PubMed]
- Qiao, K.; Xu, L.; Tang, J.; Wang, Q.; Lim, K.S.; Hooper, G.; Woodfield, T.B.F.; Liu, G.; Tian, K.; Zhang, W.; et al. The advances in nanomedicine for bone and cartilage repair. J. Nanobiotechnol. 2022, 20, 141. [Google Scholar] [CrossRef]
- Shen, Q.; Guo, Y.; Wang, K.; Zhang, C.; Ma, Y. A Review of Chondroitin Sulfate’s Preparation, Properties, Functions, and Applications. Molecules 2023, 28, 7093. [Google Scholar] [CrossRef]
- Wen, J.; Li, H.; Dai, H.; Hua, S.; Long, X.; Li, H.; Ivanovski, S.; Xu, C. Intra-articular nanoparticles based therapies for osteoarthritis and rheumatoid arthritis management. Mater. Today Bio 2023, 19, 100597. [Google Scholar] [CrossRef]
- Zhang, M.; Xu, F.; Cao, J.; Dou, Q.; Wang, J.; Wang, J.; Yang, L.; Chen, W. Research advances of nanomaterials for the acceleration of fracture healing. Bioact. Mater. 2024, 31, 368–394. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Divya, M.; Vijayakumar, S.; Chen, J. A Short Review on Chondroitin Sulphate and Its Based Nanomaterials for Bone Repair and Bone Remodelling Applications. J. Compos. Sci. 2024, 8, 6. https://doi.org/10.3390/jcs8010006
Divya M, Vijayakumar S, Chen J. A Short Review on Chondroitin Sulphate and Its Based Nanomaterials for Bone Repair and Bone Remodelling Applications. Journal of Composites Science. 2024; 8(1):6. https://doi.org/10.3390/jcs8010006
Chicago/Turabian StyleDivya, Mani, Sekar Vijayakumar, and Jingdi Chen. 2024. "A Short Review on Chondroitin Sulphate and Its Based Nanomaterials for Bone Repair and Bone Remodelling Applications" Journal of Composites Science 8, no. 1: 6. https://doi.org/10.3390/jcs8010006
APA StyleDivya, M., Vijayakumar, S., & Chen, J. (2024). A Short Review on Chondroitin Sulphate and Its Based Nanomaterials for Bone Repair and Bone Remodelling Applications. Journal of Composites Science, 8(1), 6. https://doi.org/10.3390/jcs8010006






