Saudi Consensus Recommendations on the Management of Multiple Sclerosis: Disease-Modifying Therapies and Management of Relapses
Abstract
:1. Introduction
2. Use of Disease-Modifying Therapies for the Management of Multiple Sclerosis
2.1. Need for Early Use of DMTs
2.2. Classification of DMTs
2.3. Currently Available DMTs for MS in Saudi Arabia
2.4. Prescribers of DMTs
General Pre-Treatment Work-Up
2.5. Assessment of Disease Activity in Treated Patients
2.6. Use of Disease-Modifying Therapies in Specific Subgroups of Patients with MS
2.6.1. Radiologically Isolated Syndrome (RIS)
2.6.2. Clinically Isolated Syndrome (CIS)
2.6.3. Inactive Relapsing–Remitting Multiple Sclerosis (RRMS)
2.6.4. Active or Highly-Active RRMS
- Characteristics and medical issues of patients
- Disease severity
- Adverse effects of drugs
- Drug accessibility
2.6.5. Escalation/Switching/Stopping Treatment in a Patient with RRMS
2.6.6. Aggressive MS (Treatment Non-Naïve and Treatment-Naïve)
- EDSS score ≥ 4 within 5 years of starting treatment.
- ≥two relapses with partial resolution over the last 12 months.
- >two MRI scans with new or growing T2-lesions or enhancing lesions, in spite of treatment.
- Lack of improvement while on therapy with one or more DMTs for up to one year.
2.6.7. Progressive MS
2.6.8. Use of Biosimilar Agents and Generic Medications
2.7. COVID-19 and MS DMTs (Recommendations as of July 2020)
- Chronic medical comorbidities, such as bronchial asthma, cardiac disease, diabetes, and malignancy.
- Age older than 65.
- Obesity.
- Restricted mobility.
- Continue interferon-β, glatiramer acetate, dimethyl fumarate, fingolimod, teriflunomide, siponimod, or natalizumab if COVID-19 is present but symptoms are mild.
- Otherwise, in patients with symptomatic, severe COVID-19 (e.g., patients with pneumonia, septic shock, or on mechanical ventilation), temporarily stop all DMTs (injectables, oral, and infusion therapies) until the patient is asymptomatic—especially for patients with an increased risk of complications (older age, greater disability, anti-CD 20 B cell therapy) (be aware of the risk of disease reactivation following the discontinuing of fingolimod and natalizumab) [62].
- Delay additional doses of alemtuzumab, cladribine, ocrelizumab, and rituximab in patients with mild symptoms of COVID-19.
- RIS: Evidence does not support the initiation of DMT in RIS patients.
- CIS: The following DMTs may be considered for CIS: interferons, glatiramer acetate, teriflunomide, and dimethyl fumarate.
- RRMS: For treatment of naïve-inactive RRMS, serial imaging may be recommended for a minimum of once a year for the initial 5 years, and an extended follow-up at least every 6 months, rather than initiating DMT. For treatment of naïve-active/highly active RRMS, early treatment-initiation with any of the DMTs may be considered, with the choice of therapy guided by the severity of the disease, the patient’s comorbidities and the availability and safety of the drug for that patient. For treatment of non-naïve active/highly active RRMS, the decision to escalate/switch DMTs may be driven by the extent of disease activity and tolerability and compliance with medication. The following treatment options can be initiated in both naïve and non-naïve aggressive MS: fingolimod, cladribine, natalizumab, ocrelizumab, rituximab. In addition, treatment escalation to alemtuzumab can be considered if the response to the initial high-efficacy DMT is suboptimal.
- Progressive MS: PPMS: for PPMS patients who are ambulatory, with MRI features showing evidence of inflammatory activity, treatment with ocrelizumab may be considered, except if there are risks outweighing the benefits. SPMS: For active SPMS, any of the following DMTs may be considered: (1) fingolimod, (2) natalizumab, (3) ocrelizumab, (4) cladribine, (5) rituximab (off-label), and (6) siponimod [40].
- The use of DMTs will need to be individualized with consideration of each medication’s expected benefitThe use of approved generic and biosimilar medications to treat and manage patients with MS should be considered. s and risks.
- MS and COVID-19: Counsel patients to avoid infection with COVID-19 (hygiene, social distancing) Do not delay DMT per se in the absence of a positive COVID-19 test or symptoms. Continue interferon-β, glatiramer acetate, dimethyl fumarate, fingolimod, teriflunomide, siponimod, or natalizumab if COVID-19 is present but symptoms are mild. Delay doses of alemtuzumab, cladribine, ocrelizumab, or rituximab for 2 weeks or until a negative COVID-19 test before initiation and follow-up.
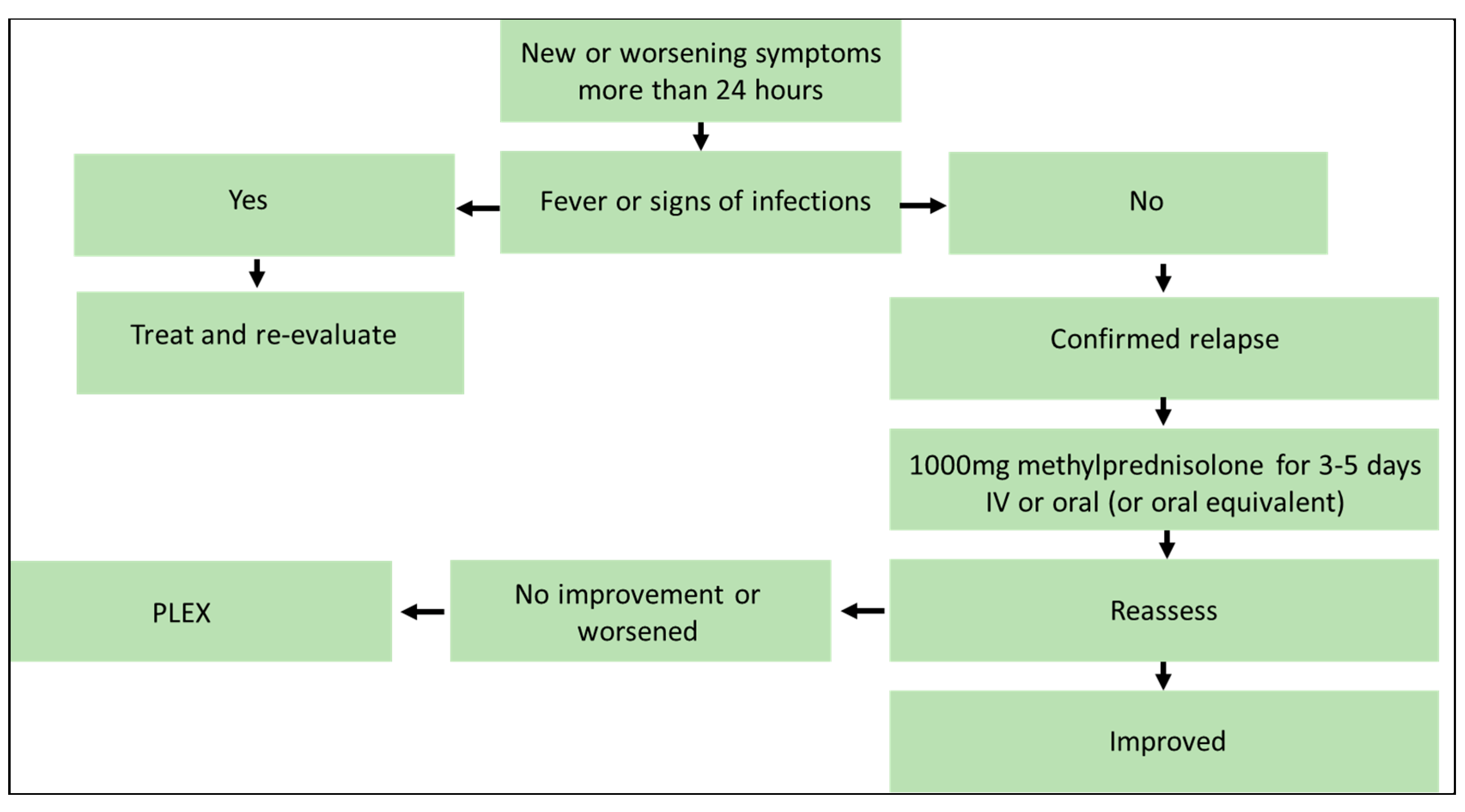
3. Management of Acute Relapse
3.1. Diagnosis of Acute Relapse
3.2. Interventions for Acute Relapse
- A relapse is a new or worsening neurological loss or weakness that lasts a minimum of 24 h, in the absence of fever or infectious disease.
- Clinicians should rule out pseudo-relapse, which is a temporary flare-up in MS symptoms unrelated to the long-term disease course of MS.
- In patients with mild exacerbations, there is a consensus that immediate treatment may not be required.
- In patients with moderate-to-severe confirmed MS relapses, high-dose intravenous/oral methylprednisolone (or the oral equivalent) is recommended as first-line treatment.
- Plasmapheresis may be considered a second-line treatment option.
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yamout, B.; Sahraian, M.; Bohlega, S.; Al-Jumah, M.; Goueider, R.; Dahdaleh, M.; Inshasi, J.; Hashem, S.; Alsharoqi, I.; Khoury, S.; et al. Consensus recommendations for the diagnosis and treatment of multiple sclerosis: 2019 revisions to the MENACTRIMS guidelines. Mult. Scler. Relat. Disord. 2020, 37, 101459. [Google Scholar] [CrossRef] [PubMed]
- Alroughani, R.; Inshasi, J.S.; Deleu, D.; Al-Hashel, J.; Shakra, M.; Elalamy, O.R.; Shatila, A.O.; Al-Asmi, A.; Al Sharoqi, I.; Canibano, B.G.; et al. An overview of high-efficacy drugs for multiple sclerosis: Gulf region expert opinion. Neurol. Ther. 2019, 8, 13–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rae-Grant, A.; Day, G.S.; Marrie, R.A.; Rabinstein, A.; Cree, B.A.; Gronseth, G.S.; Haboubi, M.; Halper, J.; Hosey, J.P.; Jones, D.E.; et al. Practice guideline recommendations summary: Disease-modifying therapies for adults with multiple sclerosis: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology 2018, 90, 777–788. [Google Scholar] [CrossRef] [Green Version]
- Metz, L.M. Clinically isolated syndrome and early relapsing multiple sclerosis. Neurology 2019, 25, 670–688. [Google Scholar] [CrossRef] [PubMed]
- Berntsson, S.A.-O.; Kristoffersson, A.; Boström, I.; Feresiadou, A.; Burman, J.; Landtblom, A.M. Rapidly increasing off-label use of rituximab in multiple sclerosis in Sweden—Outlier or predecessor? Acta Neurol. Scand. 2018, 138, 327–331. [Google Scholar] [CrossRef] [PubMed]
- Sellebjerg, F.; Blinkenberg, M.; Sorensen, P.A.-O. Anti-CD20 Monoclonal Antibodies for Relapsing and Progressive Multiple Sclerosis. CNS Drugs 2020, 34, 269–280. [Google Scholar] [CrossRef]
- Vermersch, P.; Berger, T.; Gold, R.; Lukas, C.; Rovira, A.; Meesen, B.; Chard, D.; Comabella, M.; Palace, J.; Trojano, M. The clinical perspective: How to personalise treatment in MS and how may biomarkers including imaging contribute to this? Mult. Scler. J. 2016, 22, 18–33. [Google Scholar] [CrossRef] [PubMed]
- Supplements and Featured Publications. Individualized Care and Formulary Management in Multiple Sclerosis; Supplements and Featured Publications: Cranbury, NJ, USA, 2020. [Google Scholar]
- Daif, A.K.; Al-Rajeh, S.; Awada, A.; Al Bunyan, M.; Ogunniyi, A.; AbdulJabar, M.; Al Tahan, A. Pattern of presentation of multiple sclerosis in Saudi Arabia: Analysis based on clinical and paraclinical features. Eur. Neurol. 1998, 39, 182–186. [Google Scholar] [CrossRef]
- McMillan, S.S.; King, M.; Tully, M.P. How to use the nominal group and Delphi techniques. Int. J. Clin. Pharm. 2016, 38, 655–662. [Google Scholar] [CrossRef]
- Montalban, X.; Gold, R.; Thompson, A.J.; Otero-Romero, S.; Amato, M.P.; Chandraratna, D.; Clanet, M.; Comi, G.; Derfuss, T.; Fazekas, F.; et al. ECTRIMS/EAN Guideline on the pharmacological treatment of people with multiple sclerosis. Mult. Scler. J. 2018, 24, 96–120. [Google Scholar] [CrossRef]
- Shao, H.; Stoecker, C.; Monnette, A.M.; Shi, L. Cost sharing of disease-modifying treatments (DMTs) as policy lever to improve DMTs’ access in multiple sclerosis. Value Health 2018, 21, 1083–1089. [Google Scholar] [CrossRef] [Green Version]
- Lebrun, C. Radiologically isolated syndrome should be treated with disease-modifying therapy—Commentary. Mult. Scler. J. 2017, 23, 1821–1823. [Google Scholar] [CrossRef] [PubMed]
- Okuda, D.T.; Mowry, E.M.; Beheshtian, A.; Waubant, E.; Baranzini, S.E.; Goodin, D.S.; Hauser, S.L.; Pelletier, D. Incidental MRI anomalies suggestive of multiple sclerosis: The radiologically isolated syndrome. Neurology 2009, 72, 800–805. [Google Scholar] [CrossRef]
- Comi, G.; Filippi, M.; Barkhof, F.; Durelli, L.; Edan, G.; Fernández, O.; Hartung, H.P.; Seeldrayers, P.; Sørensen, P.S.; Rovaris, M.; et al. Effect of early interferon treatment on conversion to definite multiple sclerosis: A randomised study. Lancet 2001, 357, 1576–1582. [Google Scholar] [CrossRef] [PubMed]
- Calabresi, P.A.; Kieseier, B.C.; Arnold, D.L.; Balcer, L.J.; Boyko, A.; Pelletier, J.; Liu, S.; Zhu, Y.; Seddighzadeh, A.; Hung, S.; et al. Pegylated interferon β-1a for relapsing-remitting multiple sclerosis (ADVANCE): A randomised, phase 3, double-blind study. Lancet Neurol. 2014, 13, 657–665. [Google Scholar] [CrossRef] [PubMed]
- Comi, G.; De Stefano, N.; Freedman, M.S.; Barkhof, F.; Polman, C.H.; Uitdehaag, B.M.; Casset-Semanaz, F.; Hennessy, B.; Moraga, M.S.; Rocak, S.; et al. Comparison of two dosing frequencies of subcutaneous interferon beta-1a in patients with a first clinical demyelinating event suggestive of multiple sclerosis (REFLEX): A phase 3 randomised controlled trial. Lancet Neurol. 2012, 11, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Confavreux, C.; O’Connor, P.; Comi, G.; Freedman, M.S.; Miller, A.E.; Olsson, T.P.; Wolinsky, J.S.; Bagulho, T.; Delhay, J.L.; Dukovic, D.; et al. Oral teriflunomide for patients with relapsing multiple sclerosis (TOWER): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Neurol. 2014, 13, 247–256. [Google Scholar] [CrossRef]
- O’Connor, P.; Wolinsky, J.S.; Confavreux, C.; Comi, G.; Kappos, L.; Olsson, T.P.; Benzerdjeb, H.; Truffinet, P.; Wang, L.; Miller, A.; et al. Randomized trial of oral teriflunomide for relapsing multiple sclerosis. N. Engl. J. Med. 2011, 365, 1293–1303. [Google Scholar] [CrossRef] [Green Version]
- Jacobs, L.D.; Beck, R.W.; Simon, J.H.; Kinkel, R.P.; Brownscheidle, C.M.; Murray, T.J.; Simonian, N.A.; Slasor, P.J.; Sandrock, A.W.; CHAMPS Study Group. Intramuscular interferon beta-1a therapy initiated during a first demyelinating event in multiple sclerosis. N. Engl. J. Med. 2000, 343, 898–904. [Google Scholar] [CrossRef] [Green Version]
- Vermersch, P.; Czlonkowska, A.; Grimaldi, L.M.; Confavreux, C.; Comi, G.; Kappos, L.; Olsson, T.P.; Benamor, M.; Bauer, D.; Truffinet, P.; et al. Teriflunomide versus subcutaneous interferon beta-1a in patients with relapsing multiple sclerosis: A randomised, controlled phase 3 trial. Mult. Scler. J. 2014, 20, 705–716. [Google Scholar] [CrossRef]
- Viglietta, V.; Miller, D.; Bar-Or, A.; Phillips, J.T.; Arnold, D.L.; Selmaj, K.; Kita, M.; Hutchinson, M.; Yang, M.; Zhang, R.; et al. Efficacy of delayed-release dimethyl fumarate in relapsing-remitting multiple sclerosis: Integrated analysis of the phase 3 trials. Ann. Clin. Transl. Neurol. 2015, 2, 103–118. [Google Scholar] [CrossRef] [PubMed]
- Freedman, M.S.; Selchen, D.; Arnold, D.L.; Prat, A.; Banwell, B.; Yeung, M.; Morgenthau, D.; Lapierre, Y. Treatment optimization in MS: Canadian MS Working Group updated recommendations. Can. J. Neurol. Sci. 2013, 40, 307–323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jalkh, G.A.-O.; Abi Nahed, R.; Macaron, G.; Rensel, M. Safety of newer disease modifying therapies in multiple sclerosis. Vaccines 2021, 9, 12. [Google Scholar] [CrossRef]
- He, A.; Spelman, T.; Jokubaitis, V.; Havrdova, E.; Horakova, D.; Trojano, M.; Lugaresi, A.; Izquierdo, G.; Grammond, P.; Duquette, P.; et al. Comparison of switch to fingolimod or interferon beta/glatiramer acetate in active multiple sclerosis. AMA Neurol. 2015, 72, 405–413. [Google Scholar] [CrossRef] [PubMed]
- Iaffaldano, P.; Lucisano, G.; Pozzilli, C.; Brescia Morra, V.; Ghezzi, A.; Millefiorini, E.; Patti, F.; Lugaresi, A.; Zimatore, G.B.; Marrosu, M.G.; et al. Fingolimod versus interferon beta/glatiramer acetate after natalizumab suspension in multiple sclerosis. Brain 2015, 138, 3275–3286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Copaxone (Glatiramer Acetate) Prescribing Information. Available online: https://www.copaxone.com/globalassets/copaxone/prescribing-information.pdf (accessed on 29 July 2020).
- O’Connor, P.W.; Li, D.; Freedman, M.S.; Bar-Or, A.; Rice, G.P.; Confavreux, C.; Paty, D.W.; Stewart, J.A.; Scheyer, R. A Phase II study of the safety and efficacy of teriflunomide in multiple sclerosis with relapses. Neurology 2006, 66, 894–900. [Google Scholar] [CrossRef] [PubMed]
- Tecfidera (Dimethyl Fumarate) Prescribing Information. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/204063s023lbl.pdf (accessed on 3 August 2020).
- Roman, C.; Menning, K. Treatment and disease management of multiple sclerosis patients: A review for nurse practitioners. J. Am. Assoc. Nurse Pract. 2017, 29, 629–638. [Google Scholar] [CrossRef]
- Kappos, L.; Radue, E.W.; O’Connor, P.; Polman, C.; Hohlfeld, R.; Calabresi, P.; Selmaj, K.; Agoropoulou, C.; Leyk, M.; Zhang-Auberson, L.; et al. A placebo-controlled trial of oral fingolimod in relapsing multiple sclerosis. N. Engl. J. Med. 2010, 362, 387–401. [Google Scholar] [CrossRef] [Green Version]
- Hauser, S.L.; Bar-Or, A.; Comi, G.; Giovannoni, G.; Hartung, H.P.; Hemmer, B.; Lublin, F.; Montalban, X.; Rammohan, K.W.; Selmaj, K.; et al. Ocrelizumab versus interferon beta-1a in relapsing multiple sclerosis. N. Engl. J. Med. 2017, 376, 221–234. [Google Scholar] [CrossRef]
- Martinelli, V.; Rocca, M.A.; Annovazzi, P.; Pulizzi, A.; Rodegher, M.; Boneschi, F.M.; Scotti, R.; Falini, A.; Sormani, M.P.; Comi, G.; et al. A short-term randomized MRI study of high-dose oral vs intravenous methylprednisolone in MS. Neurology 2009, 73, 1842–1848. [Google Scholar] [CrossRef]
- Butzkueven, H.; Kappos, L.; Pellegrini, F.; Trojano, M.; Wiendl, H.; Patel, R.N.; Zhang, A.; Hotermans, C.; Belachew, S. Efficacy and safety of natalizumab in multiple sclerosis: Interim observational programme results. J. Neurol. Neurosurg. Psychiatry 2014, 85, 1190–1197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonanni, A.; Calatroni, M.; D’Alessandro, M.; Signa, S.; Bertelli, E.; Cioni, M.; Di Marco, E.; Biassoni, R.; Caridi, G.; Ingrasciotta, G.; et al. Adverse events linked with the use of chimeric and humanized anti-CD20 antibodies in children with idiopathic nephrotic syndrome. Br. J. Clin. Pharmacol. 2018, 84, 1238–1249. [Google Scholar] [CrossRef] [PubMed]
- McAtee, C.L.; Lubega, J.; Underbrink, K.; Curry, K.; Msaouel, P.; Barrow, M.; Muscal, E.; Lotze, T.; Srivaths, P.; Forbes, L.R.; et al. Association of rituximab use with adverse events in children, adolescents, and young adults. JAMA Netw. Open 2021, 4, e2036321. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.A.; Lubega, J.; Underbrink, K.; Curry, K.; Msaouel, P.; Barrow, M.; Muscal, E.; Lotze, T.; Srivaths, P.; Forbes, L.R.; et al. Alemtuzumab versus interferon beta 1a as first-line treatment for patients with relapsing-remitting multiple sclerosis: A randomised controlled phase 3 trial. Lancet 2012, 380, 1819–1828. [Google Scholar] [CrossRef] [PubMed]
- Coles, A.J.; Fox, E.; Vladic, A.; Gazda, S.K.; Brinar, V.; Selmaj, K.W.; Skoromets, A.; Stolyarov, I.; Bass, A.; Sullivan, H.; et al. Alemtuzumab more effective than interferon β-1a at 5-year follow-up of CAMMS223 clinical trial. Neurology 2012, 78, 1069–1078. [Google Scholar] [CrossRef]
- Prescribing Information Mavenclad (Cladribine) Tablets. Available online: https://www.emdserono.com/us-en/pi/mavenclad-pi.pdf (accessed on 29 July 2020).
- Prescribing Information Mayzent (Siponimod) Tablets. Available online: https://www.novartis.com/us-en/sites/novartis_us/files/mayzent.pdf (accessed on 29 July 2020).
- Ho, P.R.; Koendgen, H.; Campbell, N.; Haddock, B.; Richman, S.; Chang, I.H. Risk of natalizumab-associated progressive multifocal leukoencephalopathy in patients with multiple sclerosis: A retrospective analysis of data from four clinical studies. Lancet Neurol. 2017, 16, 925–933. [Google Scholar] [CrossRef]
- Rush, C.A.; MacLean, H.J.; Freedman, M.S. Aggressive multiple sclerosis: Proposed definition and treatment algorithm. Nat. Rev. Neurol. 2015, 11, 379–389. [Google Scholar] [CrossRef]
- Menon, S.; Shirani, A.; Zhao, Y.; Oger, J.; Traboulsee, A.; Freedman, M.S.; Tremlett, H. Characterising aggressive multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 2013, 84, 1192–1198. [Google Scholar] [CrossRef]
- Havrdova, E.; Arnold, D.L.; Cohen, J.A.; Hartung, H.P.; Fox, E.J.; Giovannoni, G.; Schippling, S.; Selmaj, K.W.; Traboulsee, A.; Compston, D.A.; et al. Alemtuzumab CARE-MS I 5-year follow-up: Durable efficacy in the absence of continuous MS therapy. Neurology 2017, 89, 1107–1116. [Google Scholar] [CrossRef] [Green Version]
- Coles, A.J.; Twyman, C.L.; Arnold, D.L.; Cohen, J.A.; Confavreux, C.; Fox, E.J.; Hartung, H.P.; Havrdova, E.; Selmaj, K.W.; Weiner, H.L.; et al. Alemtuzumab for patients with relapsing multiple sclerosis after disease-modifying therapy: A randomised controlled phase 3 trial. Lancet 2012, 380, 1829–1839. [Google Scholar] [CrossRef]
- Hartung, H.P.; Gonsette, R.; Konig, N.; Kwiecinski, H.; Guseo, A.; Morrissey, S.P.; Krapf, H.; Zwingers, T. Mitoxantrone in progressive multiple sclerosis: A placebo-controlled, double-blind, randomised, multicentre trial. Lancet 2002, 360, 2018–2025. [Google Scholar] [CrossRef] [PubMed]
- Martinelli Boneschi, F.; Vacchi, L.; Rovaris, M.; Capra, R.; Comi, G. Mitoxantrone for multiple sclerosis. Cochrane Database Syst. Rev. 2013. [Google Scholar] [CrossRef] [PubMed]
- Gavriilaki, M.; Sakellari, I.; Gavriilaki, E.; Kimiskidis, V.K.; Anagnostopoulos, A. Autologous Hematopoietic Cell Transplantation in Multiple Sclerosis: Changing Paradigms in the Era of Novel Agents. Stem Cells Int. 2019, 2019, 5840286. [Google Scholar] [CrossRef] [PubMed]
- Atkins, H.L.; Bowman, M.; Allan, D.; Anstee, G.; Arnold, D.L.; Bar-Or, A.; Bence-Bruckler, I.; Birch, P.; Bredeson, C.; Chen, J.; et al. Immunoablation and autologous haemopoietic stem-cell transplantation for aggressive multiple sclerosis: A multicentre single-group phase 2 trial. Lancet 2016, 388, 576–585. [Google Scholar] [CrossRef]
- Burt, R.K.; Balabanov, R.; Snowden, J.A.; Sharrack, B.; Oliveira, M.C.; Burman, J. Non-myeloablative hematopoietic stem cell transplantation (HSCT) is superior to disease modifying drug (DMD) treatment in highly active Relapsing Remitting Multiple Sclerosis (RRMS): Interim results of the Multiple Sclerosis International Stem cell Transplant (MIST) Randomized Trial (S36.004). Neurology 2018, 90 (Suppl. S15), S36.004. [Google Scholar]
- Grand’Maison, F.; Yeung, M.; Morrow, S.A.; Lee, L.; Emond, F.; Ward, B.J.; Laneuville, P.; Schecter, R. Sequencing of disease-modifying therapies for relapsing-remitting multiple sclerosis: A theoretical approach to optimizing treatment. Curr. Med. Res. Opin. 2018, 34, 1419–1430. [Google Scholar] [CrossRef]
- Gross, R.H.; Corboy, J.R. Monitoring, switching, and stopping multiple sclerosis disease-modifying therapies. Contin. Lifelong Learn. Neurol. 2019, 25, 715–735. [Google Scholar] [CrossRef]
- Wolinsky, J.S.; Montalban, X.; Hauser, S.L.; Giovannoni, G.; Vermersch, P.; Bernasconi, C.; Deol-Bhullar, G.; Garren, H.; Chin, P.; Belachew, S.; et al. Evaluation of no evidence of progression or active disease (NEPAD) in patients with primary progressive multiple sclerosis in the ORATORIO trial. Ann. Neurol. 2018, 84, 527–536. [Google Scholar] [CrossRef] [Green Version]
- Montalban, X.; Hauser, S.L.; Kappos, L.; Arnold, D.L.; Bar-Or, A.; Comi, G.; De Seze, J.; Giovannoni, G.; Hartung, H.P.; Hemmer, B.; et al. Ocrelizumab versus placebo in primary progressive multiple sclerosis. New Engl. J. Med. 2017, 376, 209–220. [Google Scholar] [CrossRef]
- Ontaneda, D. Progressive multiple sclerosis. Continuum 2019, 25, 736–752. [Google Scholar]
- Kappos, L.; Bar-Or, A.; Cree, B.; Fox, R.; Giovannoni, G.; Gold, R.; Vermersch, P.; Arnould, S.; Sidorenko, T.; Wolf, C.; et al. Efficacy and safety of siponimod in secondary progressive multiple sclerosis—Results of the placebo controlled, double-blind, Phase III EXPAND study. In Proceedings of the 2016 meeting of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS), London, UK, 14 September 2016. [Google Scholar]
- Lizak, N.; Malpas, C.B.; Sharmin, S.; Havrdova, E.K.; Horakova, D.; Izquierdo, G.; Eichau, S.; Lugaresi, A.; Duquette, P.; Girard, M.; et al. Association of sustained immunotherapy with disability outcomes in patients with active secondary progressive multiple sclerosis. JAMA Neurol. 2020, 77, 1398–1407. [Google Scholar] [CrossRef] [PubMed]
- Marrie, R.A.; Elliott, L.; Marriott, J.; Cossoy, M.; Blanchard, J.; Tennakoon, A.; Yu, N. Dramatically changing rates and reasons for hospitalization in multiple sclerosis. Neurology 2014, 83, 929–937. [Google Scholar] [CrossRef]
- World Health Organization. Coronavirus Disease (COVID-19) Pandemic. 2020. Available online: http://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 5 August 2020).
- Brownlee, W.; Bourdette, D.; Broadley, S.; Killestein, J.; Ciccarelli, O. Treating multiple sclerosis and neuromyelitis optica spectrum disorder during the COVID-19 pandemic. Neurology 2020, 94, 949–952. [Google Scholar] [CrossRef] [Green Version]
- Coles, A.; Anderson, G.G. Covidms ABN Guidance on DMT in the Times Of COVID-19. 2020. Available online: https://multiple-sclerosis-research.org/2020/03/abn-guidance-on-dmt-in-the-times-of-covid-19 (accessed on 5 August 2020).
- Pistor, M.; Hoepner, R.; Hoepner, A.G.; Lin, Y.; Jung, S.; Bassetti, C.L.; Chan, A.; Salmen, A. Multiple Sclerosis immunotherapies and COVID-19 mortality: An analysis of the FDA Adverse Event Reporting System. Ther. Adv. Neurol. Disord. 2022, 15, 17562864221129383. [Google Scholar] [CrossRef] [PubMed]
- Berkovich, R. Treatment of acute relapses in multiple sclerosis. Neurotherapeutics 2013, 10, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Metz, L.M.; Sabuda, D.; Hilsden, R.J.; Enns, R.; Meddings, J.B. Gastric tolerance of high-dose pulse oral prednisone in multiple sclerosis. Neurology 1999, 53, 2093. [Google Scholar] [CrossRef] [PubMed]
- Strupp, M. The bioavailability of IV methylprednisolone and oral prednisone in multiple sclerosis. Neurology 2005, 64, 1100. [Google Scholar] [CrossRef]
- Morrow, S.A.; Stoian, C.A.; Dmitrovic, J.; Chan, S.C.; Metz, L.M. MS patients report excellent compliance with oral prednisone for acute relapses. Neurology 2004, 63, 1079–1080. [Google Scholar] [CrossRef]
- Ramo-Tello, C.; Grau-López, L.; Tintoré, M.; Rovira, A.; Ramió i Torrenta, L.; Brieva, L.; Cano, A.; Carmona, O.; Saiz, A.; Torres, F.; et al. A randomized clinical trial of oral versus intravenous methylprednisolone for relapse of MS. Mult. Scler. J. 2014, 20, 717–725. [Google Scholar] [CrossRef]
- Le Page, E.; Veillard, D.; Laplaud, D.A.; Hamonic, S.; Wardi, R.; Lebrun, C.; Zagnoli, F.; Wiertlewski, S.; Deburghgraeve, V.; Coustans, M.; et al. Oral versus intravenous high-dose methylprednisolone for treatment of relapses in patients with multiple sclerosis (COPOUSEP): A randomised, controlled, double-blind, non-inferiority trial. Lancet 2015, 386, 974–981. [Google Scholar] [CrossRef]
- Weiner, H.L.; Dau, P.C.; Khatri, B.O.; Petajan, J.H.; Birnbaum, G.; McQuillen, M.P.; Fosburg, M.T.; Feldstein, M.; Orav, E.J. Double-blind study of true vs. sham plasma exchange in patients treated with immunosuppression for acute attacks of multiple sclerosis. Neurology 1989, 39, 1143. [Google Scholar] [CrossRef] [PubMed]
- Weinshenker, B.G.; O’Brien, P.C.; Petterson, T.M.; Noseworthy, J.H.; Lucchinetti, C.F.; Dodick, D.W.; Pineda, A.A.; Stevens, L.N.; Rodriguez, M. A randomized trial of plasma exchange in acute central nervous system inflammatory demyelinating disease. Ann. Neurol. 1999, 46, 878–886. [Google Scholar] [CrossRef] [PubMed]
- Cortese, I.; Chaudhry, V.; So, Y.T.; Cantor, F.; Cornblath, D.R.; Rae-Grant, A. Evidence-based guideline update: Plasmapheresis in neurologic disorders: Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology 2011, 76, 294–300. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Costello, J.; Njue, A.; Lyall, M.; Heyes, A.; Mahler, N.; Philbin, M.; Nazareth, T. Efficacy, safety, and quality-of-life of treatments for acute relapses of multiple sclerosis: Results from a literature review of randomized controlled trials. Degener. Neurol. Neuromuscul. Dis. 2019, 9, 55–78. [Google Scholar] [CrossRef]

| Generic | Brand | Manufacturer | Route | Strengths & Formulations | USFDA Approval | SFDA Registration | Approved Indication a |
|---|---|---|---|---|---|---|---|
| Interferon beta-1a | Avonex | Biogen | Injectable | 30 mcg/0.5 mL pre-filled pen (IM) | ✓ | ✓ | CIS, RRMS, active SPMS |
| Interferon beta-1a | Rebif | EMD Serono/Pfizer | Injectable | 22 or 44 mcg pre-filled pen or 22 or 44 mcg/0.5 mL solution for injection cartridge (SQ) | ✓ | ✓ | CIS, RRMS, active SPMS |
| Interferon beta-1b | Betaseron/Betaferon | Bayer | Injectable | 8 MIU/mL vial (SQ) | ✓ | ✓ | CIS, RRMS, active SPMS |
| Pegylated interferon beta-1a | Plegridy | Biogen | Injectable | 125 mcg or 63–94 mcg solution for injection | ✓ | ✓ | CIS, RRMS, active SPMS in adults |
| Teriflunomide | Aubagio | Sanofi Genzyme | Oral | 7 mg and 14 mg film-coated tablet | ✓ | ✓ | CIS, RRMS, active SPMS in adults |
| Dimethyl Fumarate | Tecfidera | Biogen | Oral | 120 or 240 mg capsule | ✓ | ✓ | CIS, RRMS, active SPMS |
| Dimethyl Fumarate | Sclera b | JPI | Oral | 120 or 240 mg capsule | ✓ | ✓ | CIS, RRMS, active SPMS |
| Diroximel fumarate d | Vumerity | Biogen | Oral | 231 mg capsule | ✓ | X | CIS, RRMS, active SPMS |
| Glatiramer Acetate c | Copaxone | Teva Neuroscience | Injectable | 20 mg/mL or 40 mg/mL solution for injection (SQ) | ✓ | X | CIS, RRMS, active SPMS in adults |
| Fingolimod | Gilenya | Novartis | Oral | 0.5 mg capsule | ✓ | ✓ | CIS, RRMS, active SPMS |
| Fingolimod | Fegona b | Saja | Oral | 0.5 mg capsule | ✓ | ✓ | CIS, RRMS, active SPMS |
| Ocrelizumab | Ocrevus | Roche | IV Infusion | 30 mg/mL concentrate solution for infusion | ✓ | ✓ | CIS, RRMS, active SPMS |
| Natalizumab | Tysabri | Biogen | IV Infusion | 300 mg/15 mL concentrate solution for infusion | ✓ | ✓ | CIS, RRMS, active SPMS |
| Alemtuzumab | Lemtrada | Sanofi | IV Infusion | 12 mg concentrate solution for infusion | ✓ | ✓ | Highly active RRMS |
| Cladribine d | Mavenclad | Merck Serono | Oral | 10 mg tablet | ✓ | RRMS, active SPMS | |
| Siponimod | Mayzent | Novartis | Oral | 0.25 mg tablet | ✓ | ✓ | CIS, RRMS, active SPMS |
| No. | Parameter | Baseline | Comments |
|---|---|---|---|
| 1 | CBC with differential | ✓ | All DMTs |
| 2 | LFT | ✓ | All DMTs |
| 3 | UA | ✓ | Alemtuzumab |
| 4 | TSH | ✓ | All DMTs |
| 5 | VZV: IGG | ✓ | All DMTs except IFNB, GA, Teriflunomide, and DMF |
| 6 | HBV/HCV | ✓ | All DMTs except IFNB, GA, Teriflunomide, and DMF |
| 7 | HIV | ✓ a | All DMTs except IFNB, GA, Teriflunomide, and DMF |
| 8 | JCV | ✓ | Natalizumab |
| 9 | TB (QuantiFERON-TB Gold test) | ✓ | All DMTs except IFNB and GA |
| 10 | Pregnancy test | ✓ a | All DMTs |
| 11 | Chest X-ray | ✓ | All DMTs (in case of positive QuantiFERON-TB Gold test) |
| 12 | Cervical smear | ✓ | Alemtuzumab |
| DMT | Routine-Monitoring Recommendations |
|---|---|
| Interferon beta | LFT, CBC with differentials at months 1 and 3, and every 6–12 months as required after that. TSH every 6–12 months. |
| Glatiramer Acetate | None required. |
| Teriflunomide | LFT, CBC with differentials every month for 3 to 6 months. Repeat every 3–6 months after that. Monitor blood pressure periodically at clinic visits. |
| Dimethyl Fumarate | LFT, CBC with differentials every month for 3–6 months. Repeat every 3–6 months after that. |
| Fingolimod | LFT, RFT, and CBC with differential every month for 3 months; then repeat every 3–4 months. Full ophthalmological assessment 3 months after starting. Monitor blood pressure periodically at clinic visits. |
| Ocrelizumab | Although as per SmPC, there is no required routine monitoring, the following is recommended as per expert opinion: LFT and CBC with differential before each infusion. Pregnancy testing before each infusion. |
| Natalizumab | LFT and CBC with differential every 3 months. JCV testing every 6 months. |
| Alemtuzumab | The following tests to be conducted for 48 months following final dose: CBC with differential, ALT, serum creatinine, and urinalysis every month. TSH every 3 months. |
| Cladribine | Lymphocyte counts at 2 and 6 months after onset treatment in every treatment year. It is necessary to actively follow up patients with lymphocyte counts below 500 cells/mm³ for signs and symptoms suggestive of infections. Particularly herpes zoster. |
| Siponimod | Monitor CBC, including lymphocytes, periodically during treatment. Full ophthalmological assessment 3–4 months after initiation. Blood pressure should be regularly monitored. Monitor liver enzymes periodically during treatment. |
| To | Interferons | GA | Teriflunomide | DMF | Fingolimod | Natalizumab | Ocrelizumab | Alemtuzumab | Cladribine | Siponimod | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| From | |||||||||||
| Interferons | . | None | None | None | None | None | None | None | None | None | |
| GA | None | None | None | None | None | None | None | None | None | ||
| Teriflunomide | None | None | After REP | After REP | After REP | After REP | After REP | After REP | After REP | ||
| DMF | None | None | None a | None a | None a | None a | None a | None a | None a | ||
| Fingolimod | None | None | ALC > 0.8 b | ALC > 0.8 b | ALC > 0.8 b | ALC > 0.8 b | ALC > 0.8 b | ALC ≥ 1.0 b | ALC > 0.8 b | ||
| Natalizumab c | None | None | 4 w | 4 w | 4 w | 4 wks. | 4 w | 4 w | 4 w | ||
| Ocrelizumab | None | None | 6 mo | 6 mo | 6 mo | 6 mos. | 6 mo | 6 mo | 6 mo | ||
| Alemtuzumab | None | None | 1 y d | 1 y d | 1 y d | 1 year d | 1 year d | 1 year d | 1 y d | ||
| Cladribine | None | None | 6 mo e | 6 mo e | 6 mo e | 6 mo e | 6 mo e | 6 mo e | 6 mo e | ||
| Siponimod | None | None | ALC > 0.8 | ALC > 0.8 | ALC > 0.8 | ALC > 0.8 | ALC > 0.8 | ALC > 0.8 | ALC > 0.8 | ||
| DMT | Adverse Event |
|---|---|
| Interferon beta | |
| Glatiramer Acetate | Local injection-site reactions. Less common: transient, systemic, post-injection reactions such as (flushing, chest pain, dyspnea, palpitations) [27] |
| Teriflunomide | Headache, nausea, hair thinning, diarrhea and elevated alanine aminotransferase (ALT)-levels [19,28] Rare: hepatotoxicity, bone-marrow suppression. |
| Dimethyl Fumarate | Common: gastrointestinal symptoms (diarrhea, nausea, and abdominal pain), flushing. Rare: anaphylaxis and angioedema, hepatotoxicity, opportunistic infections (herpes zoster), very low risk of progressive multifocal leukoencephalopathy (PML) and lymphopenia [29]. |
| Fingolimod | Headache, diarrhea, elevated liver-enzymes, sinusitis, pain in the back, abdomen, arms or legs [30]. Increased risk of arrythmia and viral and fungal infections; very low risk of progressive multifocal leukoencephalopathy (PML) [31]. |
| Ocrelizumab | Infusion-related reaction, upper and lower respiratory-tract infections, and skin infections [32,33]. |
| Natalizumab | Common: headache, dizziness, nausea, and flushing during infusion, fatigue, urinary-tract and lower-respiratory-tract infections, arthralgia, gastroenteritis, vaginitis, extremity pain, depression, and rash. Rare: progressive multifocal leukoencephalopathy (PML) due to JC-virus activation [34]. |
| Rituximab | Infusion reactions, anaphylaxis and infections [35]. Rare: prolonged neutropenia, PML [36]. |
| Alemtuzumab | Infusion reactions, infections (herpes viral-infections), and autoimmune disorders (thyroid autoimmunity) [37,38]. Rare: immune thrombocytopenia, nephropathy [37]. |
| Cladribine | Upper-respiratory-tract infections, headache, and lymphocytopenia [39]. |
| Siponimod | Headache, hypertension, and increased transaminase levels [40]. Causes a dose-dependent 20–30% drop in peripheral lymphocyte counts. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al Malik, Y.M.; Al Thubaiti, I.A.; AlAmmari, M.A.; Al Fugham, N.; Ali, E.N.; Alissa, D.A.; Aljarallah, S.A.; Al-Jedai, A.H.; AlKathiri, M.A.; AlKhawajah, M.M.; et al. Saudi Consensus Recommendations on the Management of Multiple Sclerosis: Disease-Modifying Therapies and Management of Relapses. Clin. Transl. Neurosci. 2022, 6, 27. https://doi.org/10.3390/ctn6040027
Al Malik YM, Al Thubaiti IA, AlAmmari MA, Al Fugham N, Ali EN, Alissa DA, Aljarallah SA, Al-Jedai AH, AlKathiri MA, AlKhawajah MM, et al. Saudi Consensus Recommendations on the Management of Multiple Sclerosis: Disease-Modifying Therapies and Management of Relapses. Clinical and Translational Neuroscience. 2022; 6(4):27. https://doi.org/10.3390/ctn6040027
Chicago/Turabian StyleAl Malik, Yaser M., Ibtisam A. Al Thubaiti, Maha A. AlAmmari, Norah Al Fugham, Eman N. Ali, Dema A. Alissa, Salman A. Aljarallah, Ahmed H. Al-Jedai, Maeed A. AlKathiri, Mona M. AlKhawajah, and et al. 2022. "Saudi Consensus Recommendations on the Management of Multiple Sclerosis: Disease-Modifying Therapies and Management of Relapses" Clinical and Translational Neuroscience 6, no. 4: 27. https://doi.org/10.3390/ctn6040027
APA StyleAl Malik, Y. M., Al Thubaiti, I. A., AlAmmari, M. A., Al Fugham, N., Ali, E. N., Alissa, D. A., Aljarallah, S. A., Al-Jedai, A. H., AlKathiri, M. A., AlKhawajah, M. M., Almejally, M. A., Al-Mudaiheem, H. Y., Al Otaibi, H. S., AlTowaijri, G. H., Al Yafeai, R. H., Babakkor, M. A., Bohlega, S. A., Bunyan, R. F., Cupler, E. J., ... Al Jumah, M. A. (2022). Saudi Consensus Recommendations on the Management of Multiple Sclerosis: Disease-Modifying Therapies and Management of Relapses. Clinical and Translational Neuroscience, 6(4), 27. https://doi.org/10.3390/ctn6040027






