Journal Description
Clinical and Translational Neuroscience
Clinical and Translational Neuroscience
is an international, peer-reviewed, open access journal on neuroscience. The journal is owned by the Swiss Federation of Clinical Neuro-Societies and is published quarterly online by MDPI (from Volume 5 Issue 2-2021).
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within ESCI (Web of Science), Scopus, EBSCO, and other databases.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 21.9 days after submission; acceptance to publication is undertaken in 6.1 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
- Journal Cluster of Neurosciences: Brain Sciences, Neurology International, NeuroSci, Clinical and Translational Neuroscience, Neuroglia, Psychiatry International, Clocks & Sleep and Journal of Dementia and Alzheimer's Disease.
Impact Factor:
1.1 (2024)
Latest Articles
Neurorehabilitation as a Cornerstone of the Brain Health Plan
Clin. Transl. Neurosci. 2025, 9(4), 50; https://doi.org/10.3390/ctn9040050 - 14 Oct 2025
Abstract
Background: Neurorehabilitation plays a central role in restoring and maintaining brain health across lifespan. However, its contribution is often underestimated in public health policies. Aim: This paper aims to highlight the importance of neurorehabilitation within the brain health frameworks, advocating for its full
[...] Read more.
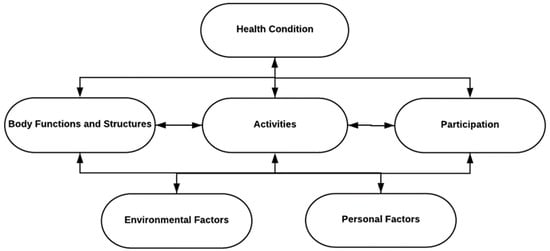
Background: Neurorehabilitation plays a central role in restoring and maintaining brain health across lifespan. However, its contribution is often underestimated in public health policies. Aim: This paper aims to highlight the importance of neurorehabilitation within the brain health frameworks, advocating for its full integration into global and national health strategies. Main content: We discuss the unique characteristics of neurorehabilitation, including its interdisciplinary structure, long-term scope and role in prevention. We underline how the ICF model provides a bridge between clinical practice and public health policy. Key prevention strategies and the potential of digital technologies are also examined. Conclusion: A stronger integration of neurorehabilitation into brain health policy can yield individual and socio-economic benefits. We call for strategic political and structural efforts to expand its availability and recognition.
Full article
(This article belongs to the Section Neurorehabilitation)
►
Show Figures
Open AccessArticle
Incidence, Risk Factors, and Prevention of Deep Vein Thrombosis in Acute Ischemic Stroke Patients (IRIS-DVT Study): A Systematic Review and Meta-Analysis
by
Yuxiang Yang, Darryl Chen and Sonu M. M. Bhaskar
Clin. Transl. Neurosci. 2025, 9(4), 49; https://doi.org/10.3390/ctn9040049 - 9 Oct 2025
Abstract
Background: Deep vein thrombosis (DVT) is a serious thromboinflammatory complication of acute ischemic stroke (AIS). The true incidence, mechanistic risk factors, and optimal prophylactic strategies remain uncertain, particularly in the era of reperfusion therapy. Methods: This systematic review and meta-analysis (IRIS-DVT) searched PubMed,
[...] Read more.
Background: Deep vein thrombosis (DVT) is a serious thromboinflammatory complication of acute ischemic stroke (AIS). The true incidence, mechanistic risk factors, and optimal prophylactic strategies remain uncertain, particularly in the era of reperfusion therapy. Methods: This systematic review and meta-analysis (IRIS-DVT) searched PubMed, Embase, Cochrane, Scopus, and Web of Science for studies reporting DVT incidence, risk factors, or prophylaxis in AIS (2004–2025). Random-effects models were used to generate pooled prevalence and effect estimates, and the certainty of evidence was graded using the GRADE framework. Results: Forty-two studies (n = 6,051,729 patients) were included. The pooled prevalence of DVT was 7% (95% CI, 6–9%), approximately seventy-fold higher than in the general population, with wide heterogeneity influenced by screening timing and diagnostic modality. Pathophysiological risk factors included higher stroke severity (NIHSS; SMD 0.41; 95% CI, 0.38–0.43), older age (SMD 0.32; 95% CI, 0.18–0.46), elevated D-dimer (SMD 0.55; 95% CI, 0.38–0.72), female sex (OR 1.33; 95% CI, 1.19–1.50), and malignancy (OR 2.69; 95% CI, 1.56–5.22), supported by moderate-certainty evidence. Respiratory infection and admission hyperglycemia showed weaker, low-certainty associations. Traditional vascular risk factors (hypertension, diabetes, atrial fibrillation, dyslipidemia) were not significantly related to DVT risk. Evidence for prophylaxis with low-molecular-weight heparin, direct oral anticoagulants, or intermittent pneumatic compression was limited and graded very low certainty. Conclusions: DVT complicates approximately one in fourteen AIS cases, reflecting a distinct thromboinflammatory process driven more by acute neurological severity, systemic hypercoagulability, and malignancy than by conventional vascular risk factors. Early systematic screening (≤72 h) and consistent use of mechanical prophylaxis are warranted. Dedicated AIS-specific mechanistic and interventional trials are urgently needed to refine prevention strategies and improve post-stroke outcomes.
Full article
(This article belongs to the Topic Neurological Updates in Neurocritical Care)
►▼
Show Figures

Figure 1
Open AccessPerspective
The Spectrum of Consciousness on the Borders of Life and Death
by
Calixto Machado and Gerry Leisman
Clin. Transl. Neurosci. 2025, 9(4), 48; https://doi.org/10.3390/ctn9040048 - 7 Oct 2025
Abstract
►▼
Show Figures
We here delve into the intricate and evolving concepts of brain death and consciousness, particularly at the end of life. We examine the historical and technological advancements that have influenced our understanding of death, such as mechanical ventilation and resuscitation techniques. These developments
[...] Read more.
We here delve into the intricate and evolving concepts of brain death and consciousness, particularly at the end of life. We examine the historical and technological advancements that have influenced our understanding of death, such as mechanical ventilation and resuscitation techniques. These developments have challenged traditional definitions of death, leading to the concept of brain death, defined as the irreversible loss of all brain functions, including the brainstem. We emphasize that consciousness exists on a continuum, ranging from full alertness to deep coma and complete cessation of brain activity. It explores various disorders of consciousness, including coma, vegetative state, minimally conscious state, and locked-in syndrome, each with distinct characteristics and levels of awareness. Neuroimaging techniques, such as EEG, fMRI, and DTI, are highlighted for their crucial role in diagnosing and understanding disorders of consciousness. These techniques help to detect covert consciousness, assess brain activity, and predict recovery potential. The phenomenon of the “wave of death,” which includes a paradoxical surge in brain activity at the point of death, is also discussed. We address the challenges in defining and understanding both death and consciousness, calling for biologically grounded, ethically defensible, and culturally sensitive definitions. We advocate for standardized neuroimaging protocols, longitudinal studies, and the integration of artificial intelligence to improve diagnosis and treatment. In conclusion, the document underscores the importance of an integrated, evidence-based approach to understanding the gray zones between life and death, recognizing that consciousness and death are dynamic processes with both biological and experiential dimensions.
Full article

Figure 1
Open AccessCase Report
Ruling Out Internal Carotid Artery Agenesis in a Patient with Chronic Occlusion: A Case Report
by
Merih Can Yilmaz and Keramettin Aydin
Clin. Transl. Neurosci. 2025, 9(4), 47; https://doi.org/10.3390/ctn9040047 - 2 Oct 2025
Abstract
Background/Objectives: This study presents a case of chronic internal carotid artery [ICA] occlusion initially misinterpreted as ICA agenesis on magnetic resonance angiography (MRA). The report underscores the importance of retrospective review of prior imaging, particularly computed tomography angiography [CTA], in establishing the
[...] Read more.
Background/Objectives: This study presents a case of chronic internal carotid artery [ICA] occlusion initially misinterpreted as ICA agenesis on magnetic resonance angiography (MRA). The report underscores the importance of retrospective review of prior imaging, particularly computed tomography angiography [CTA], in establishing the correct diagnosis. Case Report: A 70-year-old man presented with persistent headache, pulsatile tinnitus, and intermittent dizziness. Neurological examination and laboratory results were unremarkable. Initial cranial MRA demonstrated absence of flow in the left ICA, raising suspicion of congenital agenesis. However, retrospective evaluation of a CTA performed nine years earlier revealed a well-formed left carotid canal without ICA opacification, confirming the diagnosis of chronic ICA occlusion. Results: Current imaging again showed lack of enhancement in the left ICA, with adequate cerebral perfusion supplied via the contralateral ICA and vertebrobasilar system. Recognition of the preserved carotid canal on earlier CTA clarified the diagnosis as chronic occlusion rather than agenesis. Although surgical or endovascular revascularization was recommended, the patient opted for conservative management. At three months of follow-up, symptoms had improved and clinical monitoring continues. Conclusions: This case underscores the importance of distinguishing ICA agenesis from chronic occlusion, particularly by evaluating the carotid canal on CT. The presence of a carotid canal strongly indicates prior patency of the ICA and supports a diagnosis of occlusion. Careful differentiation is critical to avoid misinterpretation and to guide appropriate clinical management. In addition, reviewing prior imaging can be valuable when current findings are inconclusive or potentially misleading. Since this is a single case report, these observations should be regarded as hypothesis-generating rather than definitive, and further studies are needed to validate their broader applicability.
Full article
(This article belongs to the Section Neuroimaging)
►▼
Show Figures

Figure 1
Open AccessArticle
SORL1 as a Putative Candidate Gene for a Novel Recessive Form of Complicated Hereditary Spastic Paraplegia: Insights from a Deep Functional Study
by
Ananthapadmanabha Kotambail, Yogananda Shamamandri Markandeya, Raghavendra Mahima, Ramya Sukrutha, Madhura Milind Nimonkar, Suravi Sasmita Dash, Chandrajit Prasad, Ghati Kasturirangan Chetan, Pooja Mailankody and Gautham Arunachal
Clin. Transl. Neurosci. 2025, 9(4), 46; https://doi.org/10.3390/ctn9040046 - 1 Oct 2025
Abstract
Introduction: Genes in the endolysosome and autophagy pathways are major contributors to hereditary spastic paraplegia (HSP). A pathogenetic link between HSP and Alzheimer disease (AD) involving macroautophagy is well established. Sortilin-related receptor 1 (SORL1), an endosomal trafficking protein, plays a
[...] Read more.
Introduction: Genes in the endolysosome and autophagy pathways are major contributors to hereditary spastic paraplegia (HSP). A pathogenetic link between HSP and Alzheimer disease (AD) involving macroautophagy is well established. Sortilin-related receptor 1 (SORL1), an endosomal trafficking protein, plays a key role in glutamatergic neuron homeostasis and white matter tract integrity. Until now, SORL1 has only been associated with dominant AD and cerebral amyloid angiopathy. Methods: A case of HSP with cerebroretinal vasculopathy (CRV) negative on exome sequencing was further investigated using whole-genome sequencing. RNA-seq, Western blot, and immunofluorescence imaging were performed to explore a potential loss-of-function mechanism. Results: Sequencing revealed a biallelic SORL1 splice donor variant (c.1211 + 1G > A). Transcriptomics confirmed nonsense-mediated decay and aberrant splicing, predicting a disrupted reading frame. Reduced SORLA protein levels and significant enlargement of endolysosomes in patient-derived fibroblasts further cemented the pathogenicity of the variant. Conclusions: The probability that SORL1 acts as a recessive disease-causing gene gathers support from the following data: SORL1 genomic constraint score pRec = 1, high meiotic recombination rates on the locus, phenotype of Sorl1−/− mice reminiscent of HSP with CRV, and endolysosomal enlargement in SORL1−/− glutamatergic neurons in vitro. Taken together, SORL1 is probably a new candidate for a recessive form of complicated HSP.
Full article
(This article belongs to the Section Neuroscience/translational neurology)
►▼
Show Figures

Graphical abstract
Open AccessConference Report
Abstracts of the 6th SFCNS Congress—Swiss Federation of Clinical Neuro-Societies Lausanne, Switzerland, 29–31 October 2025—United for Brain Health
by
Swiss Federation of Clinical Neuro-Societies (SFCNS)
Clin. Transl. Neurosci. 2025, 9(4), 45; https://doi.org/10.3390/ctn9040045 - 30 Sep 2025
Abstract
On behalf of the SFCNS, Swiss Federation of Clinical Neuro-Societies, we are pleased to present the Abstracts of the 6th SFCNS Congress, which will be held in Lausanne, Switzerland, 29–31 October 2025. In total, 182 abstracts were selected as ePosters, of which 60
[...] Read more.
On behalf of the SFCNS, Swiss Federation of Clinical Neuro-Societies, we are pleased to present the Abstracts of the 6th SFCNS Congress, which will be held in Lausanne, Switzerland, 29–31 October 2025. In total, 182 abstracts were selected as ePosters, of which 60 abstracts are presented as short presentations during the ePoster Sessions and 2 abstracts are presented at the Neurosurgery Sessions. We congratulate all the presenters on their research work and contributions.
Full article
Open AccessEditorial
The Swiss Brain Health Plan in the International Context
by
Claudio L. A. Bassetti
Clin. Transl. Neurosci. 2025, 9(4), 44; https://doi.org/10.3390/ctn9040044 - 25 Sep 2025
Abstract
While the term mental health officially exists since the foundation of the WHO in 1948 and the related concept of «mental hygiene» was used in the literature already in 1843, the term brain health first appeared only in 1989 [...]
Full article
(This article belongs to the Special Issue Brain Health)
Open AccessPerspective
Bridging Bench to Bedside for Brain Health: Non-Invasive Brain Stimulation for Neurodegenerative Diseases
by
Umberto Nencha and Friedhelm C. Hummel
Clin. Transl. Neurosci. 2025, 9(3), 43; https://doi.org/10.3390/ctn9030043 - 18 Sep 2025
Abstract
The prevalence and the burden of neurodegenerative diseases is projected to increase in the future, but therapeutic options remain limited, relatively invasive, and not readily accessible. In this context, non-invasive brain stimulation (NIBS) techniques, mainly transcranial magnetic stimulation (TMS) and transcranial electrical stimulation
[...] Read more.
The prevalence and the burden of neurodegenerative diseases is projected to increase in the future, but therapeutic options remain limited, relatively invasive, and not readily accessible. In this context, non-invasive brain stimulation (NIBS) techniques, mainly transcranial magnetic stimulation (TMS) and transcranial electrical stimulation (tES), are emerging as safe and reliable instruments to enhance cognitive performance in asymptomatic individuals and patients with cognitive decline. Nevertheless, these techniques face some limitations that delay their deployment in clinical practice. Here, we describe the current status in the development of these technologies for the treatment of neurodegenerative diseases, and we present a novel promising approach for focally and non-invasively target deep brain regions. In light of these technological advances, we then propose a stepwise research roadmap to achieve an effective clinical translation of these techniques. Firstly, the constitution of open-access multimodal databases will allow to inform future interventions and design a new generation of clinical trials. Secondly, research efforts targeting symptomatic patients will need to assess the impact of NIBS techniques in different forms of dementias and probe their efficacy as disease-modifying therapies. In a future step, randomized clinical trials could focus on highly characterized at-risk populations to probe the impact of NIBS in secondary prevention. Once validated on research grounds, these techniques could enter clinical practice, enhancing cognitive performance in asymptomatic individuals and slowing disease progression in symptomatic patients, ultimately lowering the burden of neurodegenerative diseases. Eventually, NIBS techniques could be integrated into clinical practice within the framework of national Brain Health programs to provide early non-invasive interventions against cognitive decline to patients and individuals at risk.
Full article
(This article belongs to the Special Issue Brain Health)
►▼
Show Figures

Figure 1
Open AccessArticle
Exploring Physiotherapists’ Perspectives on Gaps in Care Continuity and Their Training Needs to Address These Gaps for People with Stroke in Saudi Arabia: A Qualitative Study
by
Basema Temehy, Andrew Soundy, Ahmad Sahely and Sheeba Rosewilliam
Clin. Transl. Neurosci. 2025, 9(3), 42; https://doi.org/10.3390/ctn9030042 - 16 Sep 2025
Abstract
Background: Continuity of care is critical for optimal stroke rehabilitation, yet gaps in post-stroke services in Saudi Arabia may undermine long-term patient outcomes and recovery. The therapists who care for people with stroke should be aware of patients’ needs post discharge and possess
[...] Read more.
Background: Continuity of care is critical for optimal stroke rehabilitation, yet gaps in post-stroke services in Saudi Arabia may undermine long-term patient outcomes and recovery. The therapists who care for people with stroke should be aware of patients’ needs post discharge and possess skills to address them. This study explored physiotherapists’ perspectives on gaps in care continuity for stroke patients in Saudi Arabia and identified the training needs required to address these gaps. Methods: An exploratory qualitative study situated within critical realism was conducted using nine semi-structured interviews and three focus groups. Twenty-six physiotherapists who were working in outpatient stroke rehabilitation services participated. Data was analysed using reflexive thematic analysis. Results: Three major themes emerged. Significant gaps in post-stroke care were identified, including the lack of specialised stroke rehabilitation centres and clinical practice guidelines. Participants described both facilitators and barriers to implementing continuity of care approaches, such as telerehabilitation, self-management and home care. Further, physiotherapists highlighted the need for comprehensive training in stroke assessment and management, along with the development of standardised patient and caregiver educational protocols to support care continuity. Conclusion: The study highlights the need for targeted training programmes to enhance physiotherapists’ competencies in stroke care. It also calls for systemic collaboration among healthcare organisations and policymakers to develop structured post-stroke services.
Full article
(This article belongs to the Topic Neurological Updates in Neurocritical Care)
►▼
Show Figures

Graphical abstract
Open AccessOpinion
Training the Brain Health Workforce of Tomorrow: The Role of Trainees in Shaping Integrated, Preventive, and Equitable Brain Care
by
Alice Accorroni, Davide Zani, Iliya Petkov Peyneshki, Umberto Nencha, Valentina Basile, Lukas Sveikata, Katharina Jury, Martina Göldlin, Annaelle Zietz and Violette Corre
Clin. Transl. Neurosci. 2025, 9(3), 41; https://doi.org/10.3390/ctn9030041 - 15 Sep 2025
Abstract
The concept of Brain Health is transforming the neuroscientific landscape, promoting an integrative and preventive approach to care under a unifying vision. This position paper, developed by Swiss junior societies in neurology and psychiatry, presents a trainee perspective on how Brain Health should
[...] Read more.
The concept of Brain Health is transforming the neuroscientific landscape, promoting an integrative and preventive approach to care under a unifying vision. This position paper, developed by Swiss junior societies in neurology and psychiatry, presents a trainee perspective on how Brain Health should be addressed from the earliest stages of postgraduate training. It explores current gaps in postgraduate training, including the continued separation of neurology, psychiatry and other specialties involved in brain disorder care, limited interdisciplinary and interprofessional exposure, and gaps in leadership, public health, and advocacy skills. We highlight promising models such as Switzerland’s integrated training components and the proposed “brain medicine” framework, inspired by internal medicine. Additionally, we examine innovative initiatives from trainee associations that promote collaborative learning, advocacy, and Brain Health awareness through academic and creative channels. The paper also stresses the importance of equitable global access to training, the integration of research into clinical education, and the urgent need to address burnout and working conditions among early-career professionals. By reframing trainees not as passive learners but as active agents of change, we call for systemic reforms that support their role in advancing Brain Health. Ultimately, we advocate for the development of international core competencies, adaptable curricula, and structured interdisciplinary pathways that embed Brain Health into every level of medical training. Only through this comprehensive approach can we equip the next generation of clinicians to promote lifelong Brain Health across specialties, systems, and populations.
Full article
(This article belongs to the Special Issue Brain Health)
Open AccessArticle
Six-Month Brain Health Outcomes in the Geriatric Population After Mild Traumatic Brain Injury: A Prospective Neuroimaging Study
by
Igor Horvat, Jagoš Golubović, Djula Djilvesi, Bojan Jelača and Petar Vuleković
Clin. Transl. Neurosci. 2025, 9(3), 40; https://doi.org/10.3390/ctn9030040 - 12 Sep 2025
Abstract
Introduction: Mild traumatic brain injury (mTBI) in older adults (≥65 years) is often underestimated, despite being associated with significant morbidity. Age-related vulnerability, comorbidities, and medication use may exacerbate outcomes. This study aimed to identify predictors of brain health and functional recovery in older
[...] Read more.
Introduction: Mild traumatic brain injury (mTBI) in older adults (≥65 years) is often underestimated, despite being associated with significant morbidity. Age-related vulnerability, comorbidities, and medication use may exacerbate outcomes. This study aimed to identify predictors of brain health and functional recovery in older adults following mTBI, focusing on acute symptoms, CT imaging findings, and sociodemographic factors. Methods: We analyzed a cohort of 93 older adult patients with mTBI (GCS 13–15) who were prospectively enrolled at a tertiary neurosurgical center. All patients underwent baseline CT, structured clinical assessment, and follow-up at six months with standardized instruments (Glasgow Outcome Scale–Extended-GOSE, 12-Item Short Form Health Survey (quality-of-life measure)-SF-12, Rivermead Post-Concussion Symptoms Questionnaire-RPQ, Patient Health Questionnaire-9 (depression measure)-PHQ-9, PTSD (Post Traumatics Stress Disorder) Checklist for DSM (Diagnostic and Statistical Manual for Mental Disorders)-PCL-5, Timed up and Go Test (mobility measure-TUG test). Multivariate regression was performed to identify independent predictors of recovery. Results: At six months, 94.9% of older adults achieved functional independence (GOSE ≥ 5), though only 43% attained complete recovery (GOSE = 8). Patients with acute intracranial lesions on CT had worse physical outcomes, including slower mobility (mean TUG 17.6 vs. 16.3 s, p = 0.012). Severe acute headache independently predicted poorer recovery (lower GOSE and SF-12 PCS). Lower educational attainment correlated with worse functional and quality-of-life outcomes, consistent with reduced cognitive reserve. Psychological outcomes (PTSD and depression rates) were not associated with CT findings but were influenced by social support and sex. Prompt anticoagulation reversal in patients on anticoagulants markedly reduced hemorrhagic complications. Discussion: Older adults with mTBI generally maintain independence but experience reduced physical health and mobility compared to younger patients. Predictors of poorer outcomes include severe acute symptoms, CT-detected lesions, advanced age, and lower educational levels. Psychosocial support mitigated mental health complications. Conclusions: mTBI in older adults is not benign. Clinical, imaging, and sociodemographic factors collectively shape recovery. Early identification of high-risk patients and targeted interventions are essential to preserve brain health and independence in this growing population.
Full article
(This article belongs to the Special Issue Brain Health)
►▼
Show Figures

Graphical abstract
Open AccessSystematic Review
Enhanced Recovery After Surgery in Elective Craniotomy: A Systematic Review and Meta-Analysis of Perioperative Outcomes
by
Carlos Darcy Alves Bersot, Lucas Ferreira Gomes Pereira, Vitor Alves Felippe, Matheus Reis Rocha Melo Barros, Gustavo Fernandes Nunes, José Eduardo Guimarães Pereira and Luiz Fernando dos Reis Falcão
Clin. Transl. Neurosci. 2025, 9(3), 39; https://doi.org/10.3390/ctn9030039 - 1 Sep 2025
Abstract
Introduction: Craniotomy, a common neurosurgical procedure, is frequently associated with substantial perioperative challenges and delayed recovery. While Enhanced Recovery After Surgery (ERAS) protocols have demonstrated clear benefits in multiple surgical fields, their application in neurosurgery, particularly elective craniotomy, remains emerging. Objective: This systematic
[...] Read more.
Introduction: Craniotomy, a common neurosurgical procedure, is frequently associated with substantial perioperative challenges and delayed recovery. While Enhanced Recovery After Surgery (ERAS) protocols have demonstrated clear benefits in multiple surgical fields, their application in neurosurgery, particularly elective craniotomy, remains emerging. Objective: This systematic review and meta-analysis aimed to evaluate the efficacy and safety of ERAS protocols in adult patients undergoing elective craniotomy, focusing on key outcomes such as length of hospital stay (LOS), postoperative pain, complications, and functional recovery. Methods: Following PRISMA guidelines, a comprehensive search was conducted in PubMed, Embase, Scopus, Web of Science, and the Cochrane Library up to June 2025. Eligible studies included adult patients (≥18 years) undergoing elective craniotomy and compared ERAS protocols to conventional perioperative care. Primary outcomes were LOS, postoperative complications, pain, early oral intake, and early mobilization. Data extraction and risk of bias assessment (RoB 2.0) were independently performed by two reviewers. Results: Nine randomized controlled trials (RCTs), totaling 1453 patients, were included. Meta-analysis showed that ERAS protocols significantly reduced length of hospital stay (mean difference: −2.17 days; 95% CI: −2.92 to −1.42; p < 0.00001) and decreased the incidence of postoperative nausea and vomiting (odds ratio [OR]: 0.29; 95% CI: 0.19 to 0.44; I2 = 0%). ERAS protocols were associated with higher odds of early mobilization (OR: 6.88; 95% CI: 3.46 to 13.68) and early oral intake (OR: 14.04; 95% CI: 7.80 to 25.26). Postoperative complications were significantly reduced in the ERAS group (OR: 0.49; 95% CI: 0.24 to 0.99; p = 0.048; I2 = 0%). While early urinary catheter removal showed a favorable trend (OR: 13.48), high heterogeneity (I2 = 95.7%) limits interpretability. Postoperative pain on day 1 did not differ significantly between groups (mean difference: −0.37; 95% CI: −2.38 to 1.63; p = 0.72). The overall risk of bias was rated low to moderate across studies. Conclusions: ERAS protocols in elective craniotomy are associated with shorter hospital stays, lower complication rates, reduced PONV, and earlier return to function, without increasing adverse events. These findings support broader implementation of ERAS in neurosurgical practice. Further multicenter RCTs are warranted to standardize and refine ERAS components for craniotomy.
Full article
(This article belongs to the Topic Neurological Updates in Neurocritical Care)
►▼
Show Figures

Figure 1
Open AccessArticle
Collaboration and Innovation: A Bibliometric Study of the Rise in MMA Embolization in Neurosurgery
by
Jagoš Golubović, Igor Horvat, Djula Djilvesi, Bojan Jelača and Petar Vuleković
Clin. Transl. Neurosci. 2025, 9(3), 38; https://doi.org/10.3390/ctn9030038 - 25 Aug 2025
Abstract
Chronic subdural hematoma (cSDH) is a common neurosurgical condition in the elderly, often resulting from minor head trauma. Traditional surgical treatments such as burr-hole drainage carry recurrence rates of 10–20% and significant risks in older patients, especially those on anticoagulation therapy. Middle meningeal
[...] Read more.
Chronic subdural hematoma (cSDH) is a common neurosurgical condition in the elderly, often resulting from minor head trauma. Traditional surgical treatments such as burr-hole drainage carry recurrence rates of 10–20% and significant risks in older patients, especially those on anticoagulation therapy. Middle meningeal artery (MMA) embolization has emerged as a minimally invasive alternative, aiming to reduce blood flow to the dura and thereby promote hematoma resolution and lower recurrence. We conducted a bibliometric analysis of publications on MMA embolization for cSDH up to December 2023. The analysis shows a sharp increase in research activity over the past decade. North America, Japan, and Europe are leading contributors, with collaborative networks forming among major institutions. Key journals in neurosurgery and neurointervention have published much of this research, and author collaborations are extensive. Frequently used keywords such as “recurrence” and “treatment outcome” reflect an emphasis on reducing rebleeding and improving patient outcomes. In conclusion, MMA embolization is rapidly gaining attention as a promising treatment for cSDH. While early results are favorable and multi-center efforts are expanding the evidence base, further research is needed to establish long-term efficacy, optimize patient selection, and standardize techniques.
Full article
(This article belongs to the Section Endovascular Neurointervention)
►▼
Show Figures

Figure 1
Open AccessReview
Mind–Body Integration in Brain Health
by
Lydia Maderthaner and Mark J. Edwards
Clin. Transl. Neurosci. 2025, 9(3), 37; https://doi.org/10.3390/ctn9030037 - 14 Aug 2025
Abstract
Physical and mental health are intrinsically linked. However, healthcare systems, training programs, and clinical practice often operate in silos, creating structural disincentives that exacerbate morbidity, mortality, and economic burden. Integrated care models have consistently demonstrated improved outcomes, enhanced quality of life, and greater
[...] Read more.
Physical and mental health are intrinsically linked. However, healthcare systems, training programs, and clinical practice often operate in silos, creating structural disincentives that exacerbate morbidity, mortality, and economic burden. Integrated care models have consistently demonstrated improved outcomes, enhanced quality of life, and greater cost-effectiveness across a range of neuropsychiatric and chronic disorders. With the launch of the World Health Organization Brain Health Framework (2022) and the Swiss Brain Health Plan (2023–2033), important progress has been made toward integrating mental and brain health. However, current brain health concepts could be further strengthened by more explicitly incorporating the role of the body and physical health, including psychosomatic and social aspects, particularly in terms of their dynamic, bidirectional interactions with the brain. This article further outlines the health-related and economic benefits of integrated care, key challenges to the systematic implementation of mind–body integration within healthcare systems, and proposes strategic directions for embedding body–brain dynamics into research, education, and policy. This includes interdisciplinary teaching, harmonized conceptual models, composite clinical metrics, transferable interventions, and the removal of systemic barriers to establish integrated care pathways and reduce stigma through patient-centered empowerment. Ultimately, the “no health without brain health” ethos demands the conceptual and practical integration of dynamic, bidirectional body–brain interactions.
Full article
(This article belongs to the Special Issue Brain Health)
Open AccessObituary
MG Yasargil: A Giant Swiss Clinical Neuroscientist (1925–2025)
by
Karl-Olof Lövblad, Karl Schaller, Raphael Guzman, Claudio Bassetti and Luca Regli
Clin. Transl. Neurosci. 2025, 9(3), 36; https://doi.org/10.3390/ctn9030036 - 13 Aug 2025
Abstract
The Swiss Society of Clinical Neuro-Societies mourns the loss of the former director of the Clinic of Neurosurgery at the University Hospital of Zurich Switzerland. He has pioneered microneurosurgery for lesions of the central nervous system and has had an enormous impact not
[...] Read more.
The Swiss Society of Clinical Neuro-Societies mourns the loss of the former director of the Clinic of Neurosurgery at the University Hospital of Zurich Switzerland. He has pioneered microneurosurgery for lesions of the central nervous system and has had an enormous impact not just on the development of neurosurgery but also on neighboring specialties of clinical neuroscience such as neurology and neuroradiology. He is considered one of the major innovators in his field and his impact is still felt in today’s practice, not only in neurosurgery but also in advanced techniques for the exploration of the central nervous system such as angiography.
Full article
(This article belongs to the Section Neuroscience/translational neurology)
►▼
Show Figures

Figure 1
Open AccessCommunication
The Certificate of Advanced Studies in Brain Health of the University of Bern
by
Simon Jung, David Tanner, Jacques Reis and Claudio Lino A. Bassetti
Clin. Transl. Neurosci. 2025, 9(3), 35; https://doi.org/10.3390/ctn9030035 - 4 Aug 2025
Abstract
Background: Brain health is a growing public health priority due to the high global burden of neurological and mental disorders. Promoting brain health across the lifespan supports individual and societal well-being, creativity, and productivity. Objective: To address the need for specialized education in
[...] Read more.
Background: Brain health is a growing public health priority due to the high global burden of neurological and mental disorders. Promoting brain health across the lifespan supports individual and societal well-being, creativity, and productivity. Objective: To address the need for specialized education in this field, the University of Bern developed a Certificate of Advanced Studies (CAS) in Brain Health. This article outlines the program’s rationale, structure, and goals. Program Description: The one-year, 15 ECTS-credit program is primarily online and consists of four modules: (1) Introduction to Brain Health, (2) Brain Disorders, (3) Risk Factors, Protective Factors and Interventions, and (4) Brain Health Implementation. It offers a multidisciplinary, interprofessional, life-course approach, integrating theory with practice through case studies and interactive sessions. Designed for healthcare and allied professionals, the CAS equips participants with skills to promote brain health in clinical, research, and public health contexts. Given the shortage of trained professionals in Europe and globally, the program seeks to build a new generation of brain health advocates. It aims to inspire action and initiatives that support the prevention, early detection, and management of brain disorders. Conclusions: The CAS in Brain Health is an innovative educational response to a pressing global need. By fostering interdisciplinary expertise and practical skills, it enhances professional development and supports improved brain health outcomes at individual and population levels.
Full article
(This article belongs to the Special Issue Brain Health)
►▼
Show Figures

Figure 1
Open AccessSystematic Review
Exploring the Preventive Effects of Omega-3 Polyunsaturated Fatty Acids Supplementation on Global Cognition: A Systematic Review and Meta-Analysis of Cognitively Unimpaired Older Adults
by
Roberta Mulargia, Federica Ribaldi, Sophie Mutel, Ozge Sayin, Giorgi Khachvani, Gabriele Volpara, Giulia Remoli, Umberto Nencha, Stefano Gianonni-Luza, Stefano Cappa, Giovanni B. Frisoni and Augusto J. Mendes
Clin. Transl. Neurosci. 2025, 9(3), 34; https://doi.org/10.3390/ctn9030034 - 4 Aug 2025
Abstract
Dementia prevention is a global public health priority, and lifestyle interventions, including nutrition, have gained interest for their potential to maintain cognitive health. Among nutritional interventions, omega-3 polyunsaturated fatty acids (n-3 FA), particularly eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), have been widely
[...] Read more.
Dementia prevention is a global public health priority, and lifestyle interventions, including nutrition, have gained interest for their potential to maintain cognitive health. Among nutritional interventions, omega-3 polyunsaturated fatty acids (n-3 FA), particularly eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), have been widely studied for their potential to support cognitive health. This systematic review evaluated whether n-3 FA supplementation improves global cognition in cognitively unimpaired older adults. Nineteen randomized controlled trials (RCTs) met inclusion criteria, of which five reported significant improvements in global cognition. A random-effects meta-analysis of 11 placebo-controlled RCTs showed no significant effect (SMD = −0.02, 95% CI: −0.07 to 0.04). Heterogeneity in supplement type, dosage, duration, and outcome measures may have contributed to inconsistent findings and limited comparability. Furthermore, methodological quality of the trials was generally low. While current evidence does not demonstrate a significant effect of n-3 FA supplementation on global cognition, future research should prioritize well-powered, longer-duration RCTs that incorporate biomarker monitoring and more appropriate doses. Clarifying the role of n-3 FA in cognitive aging remains essential for informing nutrition-based dementia prevention strategies.
Full article
(This article belongs to the Special Issue Brain Health)
►▼
Show Figures

Figure 1
Open AccessArticle
Perception of Quality of Life, Brain Regions, and Cognitive Performance in Hispanic Adults: A Canonical Correlation Approach
by
Juan C. Lopez-Alvarenga, Jesus D. Melgarejo, Jesus Rivera-Sanchez, Lorena Velazquez-Alvarez, Isabel Omaña-Guzmán, Carlos Curtis-Lopez, Rosa V. Pirela, Luis J. Mena, John Blangero, Jose E. Cavazos, Michael C. Mahaney, Joseph D. Terwilliger, Joseph H. Lee and Gladys E. Maestre
Clin. Transl. Neurosci. 2025, 9(3), 33; https://doi.org/10.3390/ctn9030033 - 23 Jul 2025
Abstract
►▼
Show Figures
The quality of life (QoL) perception has been studied in neurological diseases; however, there is limited information linking brain morphological characteristics, QoL, and cognition. Human behavior and perception are associated with specific brain areas that interact through diffuse electrochemical networking. We used magnetic
[...] Read more.
The quality of life (QoL) perception has been studied in neurological diseases; however, there is limited information linking brain morphological characteristics, QoL, and cognition. Human behavior and perception are associated with specific brain areas that interact through diffuse electrochemical networking. We used magnetic resonance imaging (MRI) to analyze the brain region volume (BRV) correlation with the scores of Rand’s 36-item Short Form Survey (SF-36) and cognitive domains (memory and dementia status). We analyzed data from 420 adult participants in the Maracaibo Aging Study (MAS). Principal component analysis with oblimin axis rotation was used to gather redundant information from brain parcels and SF-36 domains. Canonical correlation was used to analyze the relationships between SF-36 domains and BRV (adjusted for intracranial cavity), as well as sex, age, education, obesity, and hypertension. The average age (±SD) of subjects was 56 ± 11.5 years; 71% were female; 39% were obese; 12% had diabetes, 52% hypertension, and 7% dementia. No sex-related differences were found in memory and orientation scores, but women had lower QoL scores. The 1st and 2nd canonical correlation roots support the association of SF-36 domains (except social functioning and role emotional) and total brain volume, frontal lobe volume, frontal pole, lateral orbital lobe, cerebellar, and entorhinal areas. Other variables, including age, dementia, memory score, and systolic blood pressure, had a significant influence. The results of this study demonstrate significant correlations between BRV and SF-36 components, adjusted for covariates. The frontal lobe and insula were associated with the mental health component; the lateral-orbital frontal lobe and entorhinal area were correlated with the physical component.
Full article

Graphical abstract
Open AccessReview
Implications of AAV Serotypes in Neurological Disorders: Current Clinical Applications and Challenges
by
Sachin Sharma, Vibhuti Joshi and Vivek Kumar
Clin. Transl. Neurosci. 2025, 9(3), 32; https://doi.org/10.3390/ctn9030032 - 15 Jul 2025
Abstract
►▼
Show Figures
Adeno-associated virus (AAV) vectors have emerged as powerful tools for in vivo gene therapy, enabling long-term transgene expression in targeted tissues with minimal pathogenicity. This review examines the AAV serotypes used in clinical gene therapy trials for neurodegenerative (central nervous system, CNS) diseases,
[...] Read more.
Adeno-associated virus (AAV) vectors have emerged as powerful tools for in vivo gene therapy, enabling long-term transgene expression in targeted tissues with minimal pathogenicity. This review examines the AAV serotypes used in clinical gene therapy trials for neurodegenerative (central nervous system, CNS) diseases, highlighting their tropisms, engineering advances, and translational progress. We discuss how capsid modifications, cell-specific promoters, and novel delivery routes are enhancing AAV tropism and reducing immunogenicity to overcome current limitations. Key clinical trials in neurodegenerative disorders (such as Parkinson’s, Alzheimer’s, and Huntington’s disease) are summarized, including delivery methods (intravenous, intracoronary, intrathecal, etc.) and outcomes. We further outline the regulatory landscape with recent approvals of AAV-based therapies and ongoing efforts to address safety challenges like immune responses and vector dose toxicity. A more translational, forward-looking perspective is adopted to consider combination therapies (e.g., AAV with immune modulation or genome editing) and strategic directions to improve the next generation of AAV vectors. Overall, continued innovation in AAV vector design and delivery, alongside careful clinical evaluation, is accelerating the translation of gene therapies for neurodegenerative diseases.
Full article
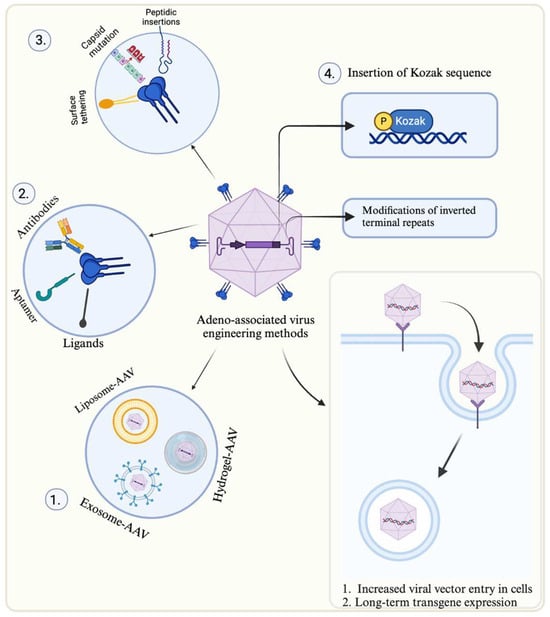
Figure 1
Open AccessCase Report
Delayed Diagnosis of a Low-Flow Temporal Arteriovenous Malformation in a Child Presenting with Recurrent Intracerebral Hemorrhage
by
Merih C. Yilmaz and Keramettin Aydin
Clin. Transl. Neurosci. 2025, 9(3), 31; https://doi.org/10.3390/ctn9030031 - 10 Jul 2025
Abstract
Background: Arteriovenous malformations (AVMs) are rare vascular anomalies that can cause intracerebral hemorrhage, particularly in pediatric patients. Low-flow AVMs may not be visualized on initial non-invasive imaging modalities such as MR angiography. Methods: We report a 6-year-old boy who presented with intracerebral hemorrhage
[...] Read more.
Background: Arteriovenous malformations (AVMs) are rare vascular anomalies that can cause intracerebral hemorrhage, particularly in pediatric patients. Low-flow AVMs may not be visualized on initial non-invasive imaging modalities such as MR angiography. Methods: We report a 6-year-old boy who presented with intracerebral hemorrhage and initially had no detectable vascular anomaly on MR angiography and MR venography. Two years later, he was re-admitted with a recurrent hemorrhage. Repeating MR angiography again failed to reveal any vascular pathology. Results: Digital subtraction angiography (DSA) performed later identified a grade 3 low-flow AVM in the left posterior temporal region. The patient underwent successful endovascular treatment with no subsequent neurological deficits. Conclusions: This case underscores the limitations of MR angiography in detecting low-flow AVMs and highlights the essential role of DSA in the definitive diagnosis and management of unexplained intracerebral hemorrhages in pediatric patients.
Full article
(This article belongs to the Section Endovascular Neurointervention)
►▼
Show Figures

Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Brain Sciences, CTN, Neurology International, NeuroSci
Neurological Updates in Neurocritical Care
Topic Editors: Gabriele Melegari, Elisabetta BertelliniDeadline: 28 February 2026