The Swiss Brain Health Plan 2023–2033
Abstract
1. Introduction
2. Section 1: The Fundamental Considerations of the Swiss Brain Health Plan
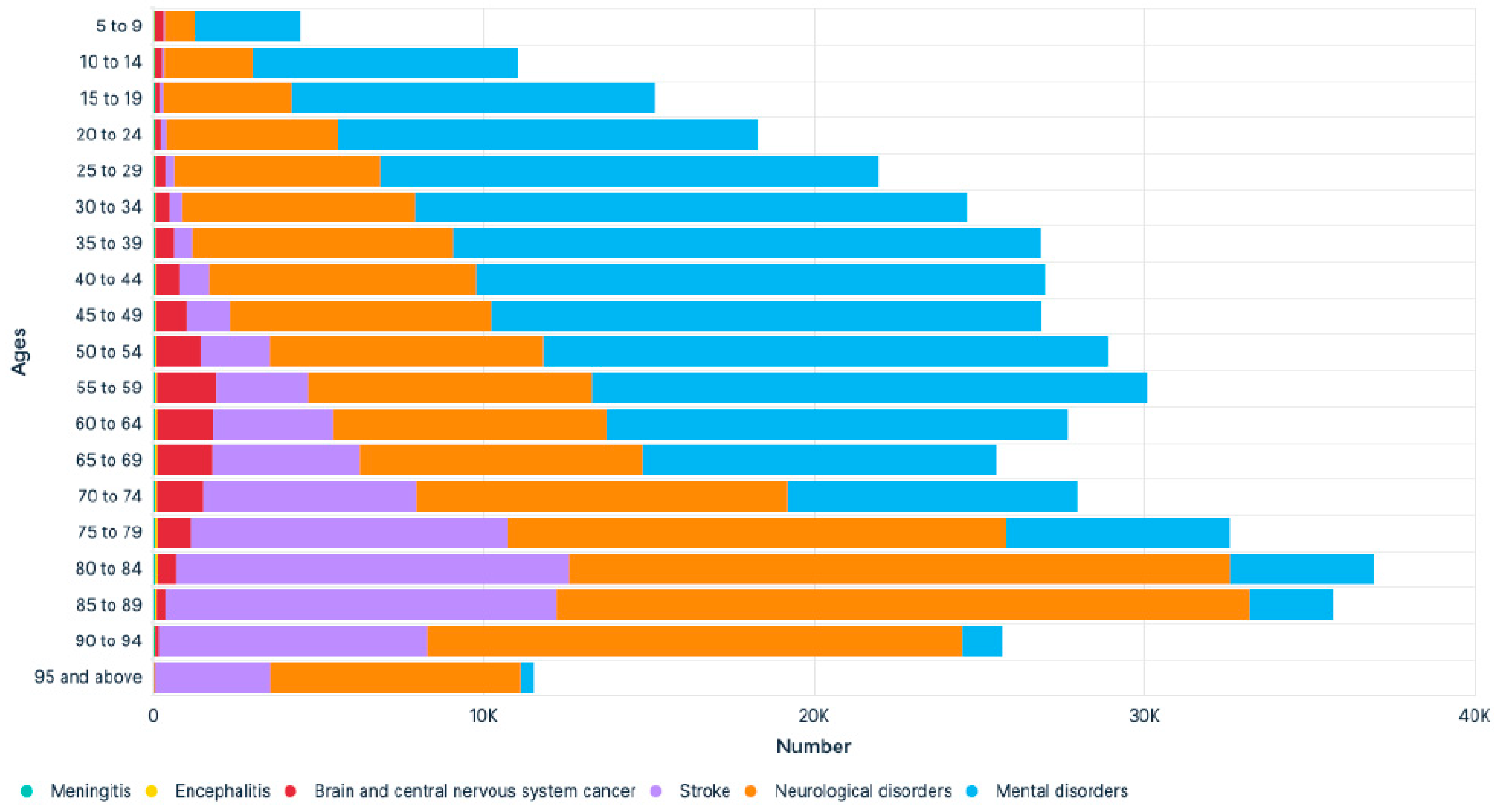
2.1. The Burden of Brain Disorders
2.2. The Burden of Neurological Disorders
2.3. The Burden of Mental (Psychiatric) Disorders
2.4. The Burden of Brain (Neurological and Mental) Disorders in Switzerland
3. Prevention of Brain Disorders
4. Brain Health: Definition and Relevance (“No Health without Brain Health”)
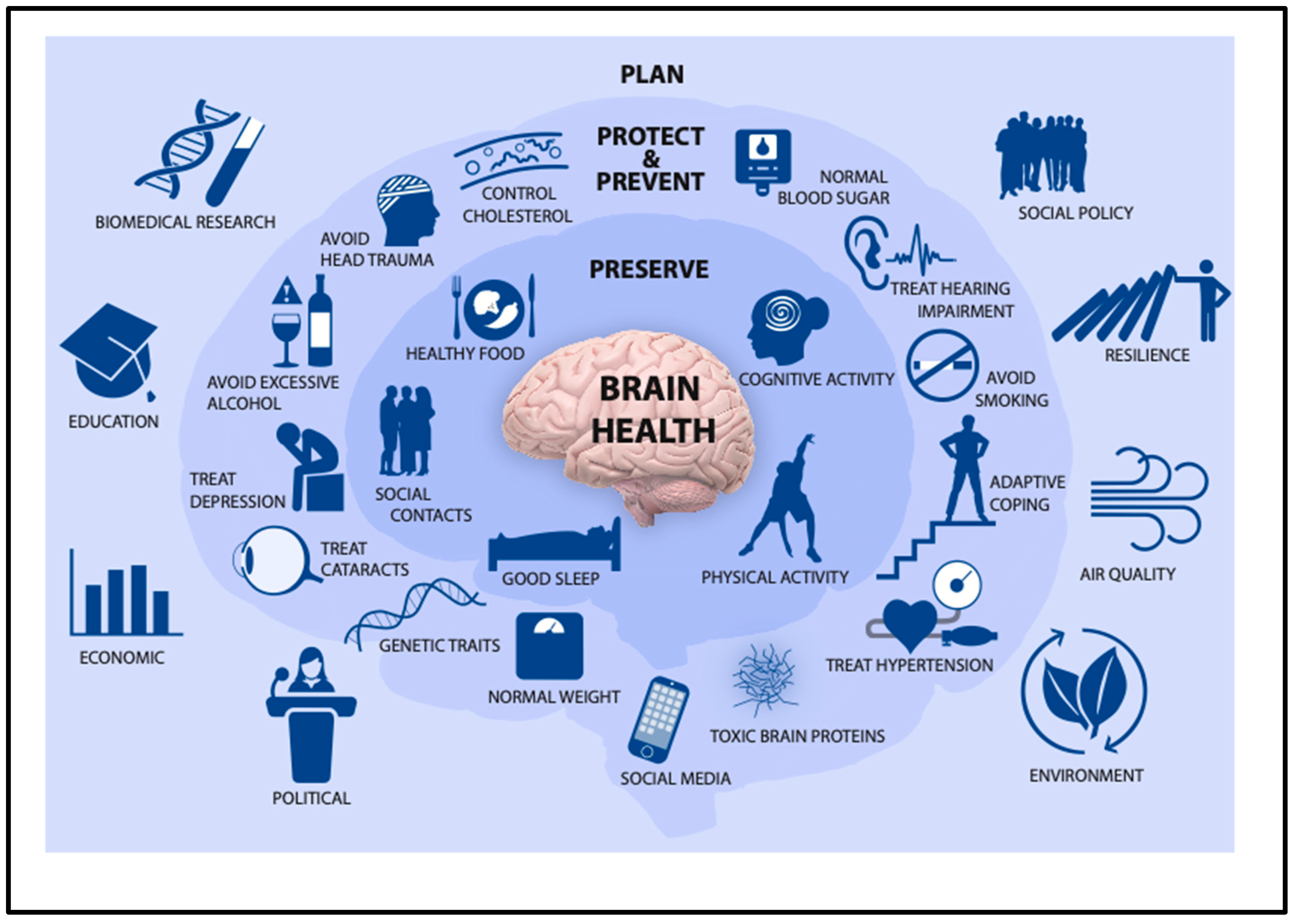
5. Brain Health: Determinants
6. International Initiatives to Promote Brain Health
6.1. Neurological Disorders
6.2. Mental (Psychiatric) Disorders
6.3. Brain (Neurological and Mental) Disorders
7. Section 2: The Swiss Brain Health Plan
- (1)
- To raise awareness about brain health and the burden of brain disorders.
- (2)
- To strengthen the cross-disciplinary and interprofessional training/education of healthcare professionals.
- (3)
- To foster research on brain health determinants and the individualized prevention of brain disorders.
- (4)
- To prioritize a holistic and concerted (synergistic) public health approach to promote brain health and prevent brain disorders.
- (5)
- To support, empower, and engage patients, caregivers, and patient organizations
8. Section 3: The Next Steps in the Implementation of the Swiss Brain Health Plan
9. Section 4: Concise Executive Summary of the Swiss Brain Health Plan (SBHP)
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
Appendix A.1. The Burden of Seven Illustrative Groups of Brain Disorders
Dementia
|
Stroke
|
Depression
|
Addiction
|
Headache
|
Epilepsy
|
Sleep disorders
|
Appendix A.2. Five Healthy Behaviors to Enhance Brain Resilience/Promote Brain Health
Healthy diet
|
Good/sufficient sleep
|
Physical activity/exercise/sport
|
Cognitive/mental activity
|
Social activity/interactions
|
References
- Owolabi, M.O.; Leonardi, M.; Bassetti, C.; Jaarsma, J.; Hawrot, T.; Makanjuola, A.I.; Dhamija, R.K.; Feng, W.; Straub, V.; Camaradou, J.; et al. Global synergystic actions to improve brain health for human development. Nat. Rev. Neurol. 2023, 19, 371–383. [Google Scholar] [CrossRef] [PubMed]
- Feigin, A.; Vos, T.; Nicholas, E.; Owolabi, M.O.; Carroll, W.M.; Dichgans, M.; Deuschl, G.; Parmar, P.; Brainin, M.; Murray, C. The global burden of neurological disorders: Translating evidence into policy. Lancet Neurol. 2020, 19, 255–265. [Google Scholar] [CrossRef] [PubMed]
- Deuschl, G.; Beghi, E.; Fazekas, F.; Varga, T.; Christoforidi, K.A.; Sipido, E.; Bassetti, C.L.; Vos, T.; Feigin, V.L. The burden of neurological diseases in Europe: An analysis for the Global Burden of Disease Study 2017. Lancet Public Health 2020, 5, e551–e567. [Google Scholar] [CrossRef] [PubMed]
- WHO. Optimizing Brain Health Across The Life Course: WHO Position Paper; WHO: Geneva, Switzerland, 2022. Available online: https://www.who.int/publications/i/item/9789240054561 (accessed on 12 October 2023).
- Global Burden of Disease 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 2022, 9, 137–150. [Google Scholar] [CrossRef]
- Jacobi, F.; Höfler, M.; Siegert, J.; Mack, S.; Gerschler, A.; Scholl, L.; Busch, M.A.; Hapke, U.; Maske, U.; Seiffert, I.; et al. Twelve-month prevalence, comorbidity and correlates of mental disorders in Germany: The Mental Health Module of the German Health Interview and Examination Survey for Adults (DEGS1-MH). Int. J. Methods Psychiatr. Res. 2014, 23, 304–319. [Google Scholar] [CrossRef]
- Dall, T.M.; Storm, M.V.; Chakrabarti, R.; Drogan, O.; Keran, C.M.; Donofrio, P.D.; Henderson, V.W.; Kaminski, H.J.; Stevens, J.C.; Vidic, T.R. Supply and demand analysis of the current and future US neurology workforce. Neurology 2013, 81, 470–478. [Google Scholar] [CrossRef]
- Bassetti, C.L.A.; Accordoni, A.; Arnesen, A.; EAN General Neurology Task Force. The present and the future of General Neurology. A white paper of the EAN General Neurology Task Force in collaboration with representatives of AAN, AFAN, ANZAN, EFNA, PAFNS, RRFS, and WFN. submitted. 2023. [Google Scholar]
- Reichmann, H. Nursing Shortage in Neurological Hospitals. Fortschr. Neurol. Psychiatr. 2023, 91, 349–350. [Google Scholar]
- Satiani, A.; Niedermeier, J.; Sataina, B.; Svendsen, D.P. Projected Workforce of Psychiatrists in the United States: A Population Analysis. Psychiatr. Serv. 2018, 69, 710–713. [Google Scholar] [CrossRef]
- Luengo-Fernandez, R.; Leal, J.; Gray, M. UK research expenditure on dementia, heart disease, stroke and cance: Are levels of spending realted to disease burden? Eur. J. Neurol. 2011, 19, 149–154. [Google Scholar] [CrossRef]
- Gaebel, W.; Falkei, P. Brain Health und Mental Health: Zewi Seiten einer Medaille. Fortschr. Neurol. Psychiatr. 2022, 90, 201–203. [Google Scholar] [CrossRef]
- Bassetti, C.L.A.; Lyrer, P.; Sandor, P.S.; Walther, S.; Hackenberg, A.; Egger, M.; Zeltner, T.; Sarikaya, H.; Lövblad, K.O.; Klein, A.; et al. Dem Gehirn Sorge Tragen: Brain Health: Eine gesundheitspolitische Priorität für die Schweiz. Schweiz. Aerztezeitung 2022, 103, 38–41. [Google Scholar]
- MacDonald, B.K.; Cockerell, O.C.; Sander, J.W.A.S.; Shorvon, S.D. The incidence and life time prevalence of neurlogical disorders in a propsective community-based study in the UK. Brain 2000, 123, 665–676. [Google Scholar] [CrossRef] [PubMed]
- Shakir, R.; Norvving, B. Stroke in ICD-11: The end of a long exile. Lancet Neurol. 2017, 389, 2373. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gustavsson, A.; Svensson, M.; Jacobi, F.; Allgulander, C.; Alonso, J.; Beghi, E.; Dodel, R.; Ekman, M.; Faravelli, C.; Fratiglioni, L.; et al. Cost of Disorders of the Brain in Europe 2010. Eur. Neuropsychopharmacol. 2011, 21, 718–779. [Google Scholar] [CrossRef]
- Morris, R.G.M.; Oertel, W.H.; Gaebel, W.; Goodwin, G.M.; Little, A.; Montellano, P.; Westphal, M.; Nutt, D.J.; Di Luca, M. Consensus Statement on European Brain Research: The need to expand brain research* in Europe—2015. Eur. J. Neurosci. 2016, 44, 1919–1926. [Google Scholar] [CrossRef]
- Zhang, P.; Zhang, X.; Brown, J.; Vistisen, D.; Sicree, R.; Shaw, J.; Nichols, G. Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes Res. Clin. Pract. 2010, 87, 293–301. [Google Scholar] [CrossRef]
- Luengo-Fernandez, R.; Leal, J.; Gray, A.; Sullivan, R. Economic burden of cancer across the European Union: A population-based cost analysis. Lancet Oncol. 2013, 14, 1165–1174. [Google Scholar] [CrossRef]
- Nichols, M.S.; Townsend Scarborough, P.; Rayner, M. Cardiovascular disease in Europe: Epidemiological update. Eur. Heart J. 2013, 35, 3028–3034. [Google Scholar] [CrossRef] [PubMed]
- Bassetti, C.L.A.; Endres, M.; Sander, A.; Crean, M.; Subramaniam, S.; Carvalho, V.; Di Liberto, G.; Franco, O.H.; Pijnenburg, V.; Leonardi, M.; et al. The EAN Brain Health Strategy: One Brain, One Life, One Approach. A strategy to reduce the burden of neurological disorders and to promote the health of the brain. Eur. J. Neurol. 2022, 29, 2559–2566. [Google Scholar] [CrossRef]
- Global Burden of Disease 2016 Neurology Collaborators. Global, regional, and national burden of neurological disorders, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 459–480. [Google Scholar] [CrossRef]
- WHO. Intersectorial Global Action Plan on Epilepsy and Other Neurological Disorders 2022–2031; WHO: Geneva, Switzerland, 2023. Available online: https://www.who.int/publications/i/item/9789240076624 (accessed on 12 October 2023).
- Taquet, M.; Geddes, J.R.; Husain, M.; Luciano, S.; Harrison, P.J. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: A retrospective cohort study using electronic health records. Lancet Psychiatry 2021, 8, 416–427. [Google Scholar] [CrossRef]
- Beghi, E.; Helbok, R.; Ozturk, S.; Karadas, O.; Lisnic, V.; Grosu, O.; Kovács, T.; Dobronyi, L.; Bereczki, D.; Cotelli, M.S.; et al. Short-and long-term outcome and predictors in an international cohort of patients with neuro-COVID-19. Eur. J. Neurol. 2022, 29, 1663–1684. [Google Scholar] [CrossRef]
- Hafner, M.; Stepanek, M.; Taylor, J.P.; Troxel, W.M.; Van Stolk, C. Why Sleep Matters-The Economic Costs of Insufficient Sleep: A Cross-Country Comparative Analysis. RAND Health Q. 2017, 6, 11. [Google Scholar]
- Kessler, R.C.; Angermeyer, M.; Anthny, J.C.; De Graaf, R.; Demyttenaere, K.; Gasquet, I.; De Girolamo, G.; Gluzman, S.; Gureje, O.; Haro, J.M.; et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry 2007, 6, 168–176. [Google Scholar] [PubMed]
- Dykxhoorn, J.; Osborn, D.; Walters, K.; Kirkbride, J.B.; Gnani, S.; Lazzarino, A.I. Temporal patterns in the recorded annual incidence of common mental disorders over two decades in the United Kingdom: A primary care cohort study. Psychol. Med. 2023, 1–12. [Google Scholar] [CrossRef]
- WHO. Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact: Scientific Brief; WHO: Geneva, Switzerland, 2022. Available online: https://iris.who.int/bitstream/handle/10665/352189/WHO-2019-nCoV-Sci-Brief-Mental-health-2022.1-eng.pdf (accessed on 12 October 2023).
- WHO. Preventing Suicide: A Global Imperative; WHO: Geneva, Switzerland, 2014. Available online: https://www.who.int/publications/i/item/9789241564779 (accessed on 12 October 2023).
- Roberts, L.W.; Louie, A.K.; Guerrero, A.P.S.; Balon, R.; Beresin, E.V.; Brenner, A.; Coverdale, J. Premature mortality among people with mental illness: Advocacy in academic psychiatry. Acad. Psychiatry 2017, 41, 441–446. [Google Scholar] [CrossRef] [PubMed]
- Maercker, A.; Perkonigg, A.; Preisig, M.; Schaller, K.; Weller, M.; Cost of Disorders of the Brain in Europe Study Group. The costs of disorders of the brain in Switzerland: An update from the European Brain Council study for 2010. Swiss Med. Wkly. 2013, 143. [Google Scholar] [CrossRef] [PubMed]
- Global Burden of Disease 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Bassetti, C.L.A.; Du Pasquier, R.; Kappos, L.; Kleinschmidt, A.; Weller, M. Neurologie: Eine therapeutische Disziplin. Swiss Med. Forum 2020, 20, 514. [Google Scholar] [CrossRef]
- Fischer, U.; Humm, A. Vom diagnostischen zum therapeutischen Fach. Swiss Medical Forum 2022, 22, 94–96. [Google Scholar] [CrossRef]
- Lin, C.C.; Callaghan, B.C.; Burke, J.F.; Skolarus, L.; Hill, C.E.; Magliocco, B.; Esper, G.J.; Kerber, K.A. Geographic variation in neurologist density and neurological care in the United States. Neurology 2021, 96, e309–e321. [Google Scholar] [CrossRef]
- Aguiar de Sousa, D.; Wilkie, A.; Norrving, B.; Macey, C.; Bassetti, C.; Tiu, C.; Roth, G.; Lunde, G.; Christensen, H.; Fiehler, J.; et al. Delivery of acute ischaemic stroke treatments in the European region in 2019 and 2020. Eur. Stroke J. 2023, 8, 618–628. [Google Scholar] [CrossRef]
- Gutzwiler, F.; Paccaud, F. Sozial- und Präventivmedizin, 4th ed.; Huber: Bern, Switzerland, 2011. [Google Scholar]
- Egger, M.; Razum, O.; Rieder, A. Public Health Kompakt, 4th ed.; De Guryter: Berlin, Germany, 2021. [Google Scholar]
- Sabayan, B.; Isaacson, R.; Rost, N. Opinion and special article: Preventive Neurology. Neurology 2021, 97, 916–919. [Google Scholar] [CrossRef]
- Fusar-Poli, P.; Correll, C.U.; Arango, C.; Berk, M.; Patel, V.; Ioannidis, J.P.A. Preventive psychiatry: A blueprint for improving the mental health of young people. World Psychiatry 2021, 20, 200–221. [Google Scholar] [CrossRef] [PubMed]
- Kleindorfer, D.O.; Towfighi, A.; Chaturvedi, S.; Cockroft, K.M.; Gutierrez, J.; Lombardi-Hill, D.; Kamel, H.; Kernan, W.N.; Kittner, S.J.; Leira, E.C.; et al. 2021 Guideline for the Prevention of Stroke in Patients with Stroke and Transient Ischemic Attack. A Guideline From the American Heart Association/American Stroke Association. Stroke 2021, 52, e364–e467. [Google Scholar] [CrossRef]
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banarjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C.; et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef]
- Gorelick, P.B.; Furie, K.L.; Iadecola, C.; Smith, E.E.; Waddy, S.P.; Lloyd-Jones, D.M.; Bae, H.-J.; Bauman, M.A.; Dichgans, M.; Duncan, P.W.; et al. Defining optimal brain health in adults. Stroke 2017, 48, e284–e303. [Google Scholar] [CrossRef]
- Chen, Y.; Demnitz, N.; Yamamoto, S.; Yaffe, K.; Lawlor, B.; Leroi, I. Defining brain health: A concept analysis. Int. J. Geriatr. Psychiatry 2021, 37. Online ahead of print. [Google Scholar] [CrossRef]
- Avan, A.; Hachinski, V.; Brain Health Learn and Act Group. Brain health: Key to health, productivity, and well-being. Alzheimer’s Dement. 2021, 18, 1396–1407. [Google Scholar] [CrossRef] [PubMed]
- Bassetti, C.L.A.; Helbok, R.; Adorkan, K.; Falkei, P. EPA-EAN Statement on Post-COVID syndrome. Eur. J. Neurol. 2023, 30, 294–295. [Google Scholar] [CrossRef] [PubMed]
- García-García, I.; Donica, O.; Cohen, A.A.; Nusslé, S.G.; Heini, A.; Nusslé, S.; Pichard, C.; Rietschel, E.; Tanackovic, G.; Folli, S.; et al. Maintaining brain health across the lifespan. Neurosci. Biobehav. Rev. 2023, 153, 105365. [Google Scholar] [CrossRef]
- Wu, Y.-T.; Prina, A.M.; Brayne, C. The association between community environment and cognitive function: A systematic review. Soc. Psychiatry Psychiatr. Epidemiol. 2015, 50, 351–362. [Google Scholar] [CrossRef]
- Burzynska, A.Z.; Malinin, L.H. Enriched Environments for Healthy Aging: Qualities of Seniors Housing Designs Promoting Brain and Cognitive Health. Sr. Hous. Care J. 2017, 25, 15–37. [Google Scholar]
- Khalaf, A.M.; Alubied, A.A.; Klalaf, A.M.; Rifae, A.A. The Impact of Social Media on the Mental Health of Adolescents and Young Adults: A Systematic Review. Cunes 2023, 15, e42990. [Google Scholar] [CrossRef] [PubMed]
- Gostin, L.O.; Monahan, J.T.; Kaldor, J.; DeBartolo, M.; Friedman, E.A.; Gottschalk, K.; Kim, S.C.; Alwan, A.; Binagwaho, A.; Burci, G.L. The legal determinants of health: Harnessing the power of law for global health and sustainable development. Lancet 2019, 393, 1857–1910. [Google Scholar] [CrossRef] [PubMed]
- Friel, S.; Collin, J.; Daube, S.; Depoux, A.; Freudenberg, N.; Gilmore, A.B.; Johns, P.; Laar, A.; Marten, R.; McKee, M.; et al. Commercial determinants of health: Future directions. Lancet 2023, 401, 1229–1240. [Google Scholar] [CrossRef]
- Brill, E.; Klusmann-Weisskopf, V.; Klöppel, S. Wenn Werte motivieren. Schweiz. Aerztezeitung 2023, 104, 34–35. [Google Scholar] [CrossRef]
- Haldane, V.; De Foo, C.; Abdalla, S.M.; Jung, A.S.; Tan, M.; Wu, S.; Chua, A.; Verma, M.; Shrestha, P.; Singh, S.; et al. Health systems resilience in managing the COVID-19 pandemic: Lessons from 28 countries. Nat. Med. 2021, 27, 964–980. [Google Scholar] [CrossRef]
- Frisoni, G.B.; Molinuevo, K.L.; Altomare, D.; Carrera, E.; Barkhof, F.; Berkhof, J.; Delrieu, J.; Dubois, B.; Kivipelto, M.; Nordberg, A.; et al. Precision prevention of Alzheimer’s and other dementias: Anticipating future needs in the control of risk factors and implementation of disease-modifying therapies. Alzheimer’s Dement. 2020, 16, 1457–1468. [Google Scholar] [CrossRef]
- Owolabi, M.O.; Thrift, A.G.; Mahal, A.; Ishida, M.; Martins, S.; Johnson, W.D.; Pandian, J.; Abd-Allah, F.; Yaria, J.; Phan, H.T.; et al. Primary stroke prevention worldwide: Translating evidence into action. Lancet Public Health 2022, 7, e74–e85. [Google Scholar] [CrossRef]
- Boon, P.; Aleksovaks, K.; Konti, M.; Berger, T.; Leonardi, M.; Marson, T.; Kalweit, U.; Moro, E.; Toscano, A.; Rektorova, I.; et al. A Strategic Neurological Research Agenda for Europe: Towards clinically and societally relevant neurological research priorities. 2023; submitted. [Google Scholar]
- Norrving, B.; Barrick, J.; Davalos, A.; Dichgans, M.; Cordonnier, C.; Guekht, A.; Kutluk, K.; Mikulik, R.; Wardlaw, J.; Richard, E.; et al. Action Plan for Stroke in Europe 2018–2030. Eur. Stroke J. 2018, 3, 309–336. [Google Scholar] [CrossRef]
- Frisoni, G.B.; Altomare, D.; Ribaldi, F.; Villain, N.; Brayne, C.; Mukadam, N.; Abramowicz, M.; Barkhof, F.; Berthier, M.; Bieler-Aeschlimann, M.; et al. Dementia prevention in memory clinics: Recommendations from the European task force for brain health servcies. Lancet Reg. Health Eur. 2023, 26, 10057. [Google Scholar] [CrossRef]
- The Lancet Neurology. A decisive year for the neurological community. Lancet Neurol. 2022, 21, 103. [Google Scholar] [CrossRef]
- Wjeratne, T.; Bassetti, C.L.A.; Grisold, W.; Dodick, D.; Rouleau, G.; Lewis, S.L.; Stark, R.; Freedman, M.; Guekht, A.; Gouider, R.; et al. Brain health for all on World Brain Day 2022. Lancet Neurol. 2022, 9, 772–773. [Google Scholar] [CrossRef]
- WHO. Comprehensive Mental Health Action Plan 2013–2030; WHO: Geneva, Switzerland, 2021. Available online: https://www.emro.who.int/mnh/mental-health-action-plan/index.html (accessed on 12 October 2023).
- WHO. Global Alcohol Action Plan 2022–2030; WHO: Geneva, Switzerland, 2023. Available online: https://www.who.int/teams/mental-health-and-substance-use/alcohol-drugs-and-addictive-behaviours/alcohol/our-activities/towards-and-action-plan-on-alcohol (accessed on 12 October 2023).
- European Commission. Healthier Together EU Non-Communicable Diseases Initiative; European Commission: Geneva, Switzerland, 2022. Available online: https://eurohealthnet.eu/publication/eurohealthnet-provides-input-for-the-eu-ncd-initiative-healthier-together/?gclid=CjwKCAiA6byqBhAWEiwAnGCA4HtK824G_QEqbgLldSEsCOrgFFI-fxYObqpXEcw-StyXb9x6EHbY4RoC7iUQAvD_BwE (accessed on 12 October 2023).
- The Lancet Neurology. Sustainable development demands brain health. Lancet Neurol. 2023, 22, 871. [Google Scholar] [CrossRef] [PubMed]
- Rost, N.S.; Salinas, J.; Jordan, J.T.; Banwell, B.; Correra, D.J.; Said, R.R.; Selwa, L.M.; Song, S.; Evans, D.A. The Brain Health Imperative in the 21st Century-A call to action. Neurology 2023, 101, 1–10. [Google Scholar] [CrossRef]
- Bassetti, C.; Merlo, A.; Steinlin, M.; Valavanis, A.; Weder, B. SFCNS: Eine starke Allianz der klinischen Neurodisiplinen. SAEZ 2013, 94, 870–872. [Google Scholar]
- Budin-Ljøsne, I.; Mowinckel, A.M.; Friedman, B.B.; Ebmeier, K.P.; Drevon, C.A.; Carver, R.B.; Zsoldos, E.; Fredheim, N.A.G.; Sørensen, Ø.; Baaré, W.F.C.; et al. Public perceptions of brain health: An international, online cross-sectional survey. BMJ Open 2022, 12, e057999. [Google Scholar] [CrossRef] [PubMed]
- Probasco, J.C.; Greene, J.; Harrison, A.; Jensen, J.; Khot, S.; Klein, J.P.; Simpson, J.; Wold, J.; Josephson, S.A.; Likosky, D. Neurohospitalist Practice, Perspectives, and Burnout. Neurohospitalist 2019, 9, 85–92. [Google Scholar] [CrossRef]
- Di Liberto, G.; Baldizzi, G.; Carvalho, V.; Cuffaro, L.; Sauerbier, A.; Klingelhoefer, L.; Vashchenko, N.; Pavlakova, L.; Sander, A.; De Visser, M.; et al. Impact of Burnout on Neurology Residents and Research Fellows in Europe. Neurol. Educ. 2022, 1, e200035. [Google Scholar] [CrossRef]
- Di Luca, M.; Baker, M.; Corradetti, R.; Kettenmann, H.; Mendlewicz, J.; Olesen, J.; Ragan, I.; Westphal, M. Consensus Document on European Brain Research. Eur. J. Neurosci. 2011, 33, 768–818. [Google Scholar] [CrossRef]
- Südhof, T.C. Molecular Neuroscience in the 21st Century: A Personal Perspective. Neuron 2017, 96, 536–541. [Google Scholar] [CrossRef]
- Winter, B.; Oertel, W.H.; Dodel, R. Is there underfunding in brain research? The UK research expenditure. Eur. J. Neurol. 2012, 19, 4–5. [Google Scholar] [CrossRef]
- Chinthapalli, K. Brain disorders cost the most overall but attract the least research funding. BMJ 2013, 347, f4766. [Google Scholar] [CrossRef]
- MoNAM. Expenditures for Health Promotion and Prevention by Services; MoNAM: Bern, Switzerland, 2023; Available online: https://ind.obsan.admin.ch/indicator/monam/ausgaben-fuer-gesundheitsfoerderung-und-praevention-nach-leistungen (accessed on 12 October 2023).
- Fiest, K.M.; Jetté, N.; Roberts, J.; Maxwell, C.J.; Smith, E.E.; Black, S.E.; Blaikie, L.; Cohen, A.; Day, L.; Holroyd-Leduc, J.; et al. The Prevalence and Incidence of Dementia: A Systematic Review and Meta-analysis. Can. J. Neurol. Sci. 2017, 43, S3–S50. [Google Scholar] [CrossRef] [PubMed]
- Global Burden of Disease 2019 Dementia Forecasting Collaborators. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: An analysis for the Global Burden of Disease Study 2019. Lancet Public Health 2022, 7, e105–e125. [Google Scholar] [CrossRef]
- Meijer, E.; Casanova, M.; Kim, H.; Llena-Nozal, A.; Lee, J. Economic costs of dementia in 11 countries in Europe: Estimates from nationally representative cohorts of a panel study. Lancet Reg. Health-Eur. 2022, 20, 100445. [Google Scholar] [CrossRef]
- WHO. Global Status Report on the Public Health Response to Dementia; WHO: Geneva, Switzerland, 2021. Available online: https://www.who.int/publications/i/item/9789240033245 (accessed on 12 October 2023).
- Peters, R.; Xu, Y.; Fitzgerald, O.; Aung, H.L.; Beckett, N.; Bulpitt, C.; Chalmers, J.; Forette, F.; Gong, J.; Harris, K.; et al. Blood pressure lowering and prevention of dementia: An individual patient data meta-analysis. Eur. Heart J. 2022, 43, 4980–4990. [Google Scholar] [CrossRef]
- Global Burden of Disease 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its isk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021, 20, 795–820. [Google Scholar] [CrossRef]
- Feigin, V.L.; Nguyen, G.; Cercy, K.; Johnson, C.O.; Alam, T.; Parmar, P.G.; Abajobir, A.A.; Abate, K.H.; Abd-Allah, F.; Abejie, A.N.; et al. Global, Regional, and Country-Specific Lifetime Risks of Stroke, 1990 and 2016. N. Engl. J. Med. 2018, 379, 2429–2437. [Google Scholar]
- O’Donnell, M.J.; Chin, S.L.; Rangarajan, S.; Xavier, D.; Liu, L.; Zhang, H.; Rao-Melacini, P.; Zhang, X.; Pais, P.; Agapay, S.; et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): A case-control study. Lancet 2016, 388, 761–775. [Google Scholar] [CrossRef]
- Global Burden of Disease 2016 Stroke Collaborators. Global, regional, and national burden of stroke, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2019, 18, 439–458. [Google Scholar] [CrossRef]
- Loechner, J.; Starman, K.; Galuschka, K.; Tamm, J.; Schulte-Körne, G.; Rubel, J.; Platt, B. Preventing depression in the offspring of parents with depression: A systematic review and meta-analysis of randomized controlled trials. Clin. Psychol. Rev. 2018, 60, 1–14. [Google Scholar] [CrossRef]
- Merikangas, K.R.; McClair, V.L. Epidemiology of substance use disorders. Hum. Genet. 2012, 131, 779–789. [Google Scholar] [CrossRef]
- Nelson, L.F.; Weitzman, E.R.; Levy, S. Prevention of Substance Use Disorders. Med. Clin. North. Am. 2022, 106, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Safiri, S.; Pourfathi, H.; Eagan, A.; Mansournia, M.A.; Khodayari, M.T.; Sullman, M.J.M.; Kaufman, J.; Collins, G.; Dai, H.; Bragazzi, N.L.; et al. Global, regional, and national burden of migraine in 204 countries and territories, 1990 to 2019. Pain 2022, 163, e293–e309. [Google Scholar] [CrossRef] [PubMed]
- Goadsby, P.J.; Lantéri-Minet, M.; Michel, M.C.; Peres, M.; Shibata, M.; Straube, A.; Wijeratne, T.; Ebel-Bitoun, C.; Constantin, L.; Hitier, S. 21st century headache: Mapping new territory. J. Headache Pain 2021, 22. [Google Scholar] [CrossRef]
- Eigenbrodt, A.K.; Ashina, H.; Khan, S.; Diener, H.C.; Mitsikostas, D.D.; Sinclair, A.J.; Pozo-Rosisch, P.; Martelletti, P.; Ducros, A.; Lantéri-Minet, M.; et al. Diagnosis and management of migraine in ten steps. Nat. Rev. Neurol. 2021, 17, 501–514. [Google Scholar] [CrossRef] [PubMed]
- Fiest, K.M.; Sauro, K.M.; Wiebe, S.; Patten, S.B.; Kwon, C.S.; Dykeman, J.; Pringsheim, T.; Lorenzetti, D.L.; Jetté, N. Prevalence and incidence of epilpesy. A systematic review and meta-analysis of international studies. Neurology 2017, 88, 296–303. [Google Scholar] [CrossRef]
- Global Burden of Disease 2016 Epilepsy Collaborators. Global, regional, and national burden of epilepsy, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 357–375, Erratum in: Lancet Neurol. 2019, 30418, e30454. [Google Scholar] [CrossRef]
- Begley, C.; Wagner, R.G.; Abraham, A.; Beghi, E.; Newton, C.; Kwon, C.S.; Labiner, D.; Winkler, A.S. The global cost of epilepsy: A systematic review and extrapolation. Epilepsia 2022, 63, 892–903. [Google Scholar] [CrossRef]
- Thurman, D.J.; Begley, C.E.; Carpio, A.; Helmers, S.; Hesdorffer, D.C.; Mu, J.; Touré, K.; Parko, K.L.; Newton, C.R. The primary prevention of epilepsy: A report of the Prevention Task Force of the International League Against Epilepsy. Epilepsia 2018, 59, 905–914. [Google Scholar] [CrossRef]
- Tai, X.Y.; Torzillo, E.; Lyall, D.M.; Manohar, S.; Husain, M.; Sen, A. Association of Dementia Risk with Focal Epilepsy and Modifiable Cardiovascular Risk Factors. JAMA Neurol. 2023, 80, 445–454. [Google Scholar] [CrossRef]
- Kerkhof, G.A. Epidemiology of sleep and sleep disorders in The Netherlands. Sleep. Med. 2017, 30, 229–239. [Google Scholar] [CrossRef] [PubMed]
- Kocevska, D.; Lysen, T.S.; Dotinga, A.; Koopman-Verhoeff, M.E.; Luijk, M.P.C.M.; Antypa, N.; Biermasz, N.R.; Blokstra, A.; Brug, J.; Burk, W.J.; et al. Sleep characteristics across the lifespan in 1.1 million people from the Netherlands, United Kingdom and United States: A systematic review and meta-analysis. Nat. Hum. Behav. 2021, 5, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Paruthi, S.; Brooks, L.J.; D’Ambrosio, C.; Hall, W.A.; Kotagal, S.; Lloyd, R.M.; Malow, B.A.; Maski, K.; Nichols, C.; Quan, S.F.; et al. Recommended amount of sleep for pediatric populations: A consensus statement of the American Academy of Sleep Medicine. J. Clin. Sleep. Med. 2016, 12, 785–786. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.W.; Stein, M.B.; Nishimi, K.M.; Ge, T.; Coleman, J.R.I.; Chen, C.Y.; Ratanatharathorn, A.; Zheutlin, A.B.; Dunn, E.C.; 23andMe Research Team; et al. An Exposure-Wide and Mendelian Randomization Approach to Identifying Modifiable Factors for the Prevention of Depression. Am. J. Psychiatry 2020, 177, 944–954. [Google Scholar] [CrossRef]
- Bubu, O.M.; Andrade, A.G.; Umasabor-Bubu, O.Q.; Hogan, M.M.; Turner, A.D.; de Leon, M.J.; Ogedegbe, G.; Ayappa, I.; Jean-Louis, G.G.; Jackson, M.L.; et al. Obstructive sleep apnea, cognition and Alzheimer’s disease: A systematic review integrating three decades of multidisciplinary research. Sleep. Med. Rev. 2020, 50, 101250. [Google Scholar] [CrossRef]
- Lim, D.C.; Najafi, A.; Afifi, L.; Bassetti, C.; Buysse, D.J.; Han, F.; Högl, B.; Melaku, Y.A.; Morin, C.M.; Pack, A.I.; et al. The Urgent Need to Promote Sleep Health Across the Globe. Lancet Public Health 2023, 8, e820–e826. [Google Scholar] [CrossRef]
- Huang, S.-Y.; Li, Y.Z.; Zhang, Y.R.; Huang, Y.Y.; Wu, B.S.; Zhang, W.; Deng, Y.T.; Chen, S.D.; He, X.Y.; Chen, S.F.; et al. Sleep, physical activity, sedentary behavior, and risk of incident dementia: A prospective cohort study of 431,924 UK Biobank participants. Mol. Psychiatry 2022, 27, 4343–4354. [Google Scholar] [CrossRef]
- WHO. Guideline: Sodium Intake for Adults and Children; WHO: Geneva, Switzerland, 2012. Available online: https://www.who.int/publications/i/item/9789241504836 (accessed on 12 October 2023).
- Hooper, L.; Abdelhamid, A.; Bunn, D. Effects of total fat intake on body weight. Cochrane Database Syst. Rev. 2015, 8, CD011834. [Google Scholar] [CrossRef] [PubMed]
- WHO. Guideline: Sugars Intake for Adults and Children; WHO: Geneva, Switzerland, 2015. Available online: https://www.who.int/publications/i/item/9789241549028 (accessed on 12 October 2023).
- Swiss Nutrition Policy. Available online: https://www.blv.admin.ch/blv/en/home/das-blv/strategien/schweizer-ernaehrungsstrategie.html (accessed on 12 October 2023).
- Fidler Mis, N.; Braegger, C.; Bronsky, J.; Campoy, C.; Domellöf, M.; Embleton, N.D.; Hojsak, I.; Hulst, J.; Indrio, F.; Lapillonne, A.; et al. Sugar in Infants, Children and Adolescents: A Position Paper of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2017, 65, 681–696. [Google Scholar] [CrossRef]
- Roberts, M.; Tolar-Peterson, T.; Reynolds, A.; Wall, C.; Reeder, N.; Mendez, G.R. The Effects of Nutritional Interventions on the Cognitive Development of Preschool-Age Children: A Systematic Review. Nutrients 2022, 14, 532. [Google Scholar] [CrossRef]
- Global Burden of Disease 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [PubMed]
- US Department of Health and Human Services. Physical Activity Guidelines AC. 2018 Physical Activity Guidelines Advisory Committee Scientific Report; Department of Health and Human Services: Washington, DC, USA, 2018. Available online: https://health.gov/sites/default/files/2019-09/PAG_Advisory_Committee_Report.pdf (accessed on 12 October 2023).
- WHO. WHO Guidelines on Physical Activity and Sedentary Behaviour: At a Glance; WHO: Geneva, Switzerland, 2020. Available online: https://www.who.int/publications/i/item/9789240015128 (accessed on 12 October 2023).
- Najar, J.; Östling, S.; Gudmundsson, P.; Sundh, V.; Johansson, L.; Kern, S.; Guo, X.; Hällström, T.; Skoog, I. Cognitive and physical activity and dementia. Neurology 2019, 92, e1322–e1330. [Google Scholar] [CrossRef]
- Rodriguez-Ayllon, M.; Cadenas-Sánchez, C.; Estévez-López, F.; Muñoz, N.E.; Mora-Gonzalez, J.; Migueles, J.H.; Molina-García, P.; Henriksson, H.; Mena-Molina, A.; Martínez-Vizcaíno, V.; et al. Role of Physical Activity and Sedentary Behavior in the Mental Health of Preschoolers, Children and Adolescents: A Systematic Review and Meta-Analysis. Sports Med. 2019, 49, 1383–1410. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Lee, E.Y.; Rosernbaum, S.; Khan, S.R.; Thremblay, M.S. Dose-dependent and joint associations between screen time, physical activity, and mental wellbeing in adolescents: An international observational study. Lancet Child. Adolesc. Health 2021, 5, 729–738. [Google Scholar] [CrossRef]
- Stern, Y. Cognitive reserve in ageing and Alzheimer’s disease. Lancet Neurol. 2012, 11, 1006–1012. [Google Scholar] [CrossRef]
- Ngandu, T.; Lehtisalo, J.; Solomon, A.; Levälahti, E.; Ahtiluoto, S.; Antikainen, R.; Bäckman, L.; Hänninen, T.; Jula, A.; Laatikainen, T.; et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomised controlled. Lancet 2015, 385, 2255–2263. [Google Scholar] [CrossRef]
- Wickramaratne, P.J.; Yangchen, T.; Lepow, L.; Patra, B.G.; Glicksburg, B.; Talati, A.; Adekkanattu, P.; Ryu, E.; Biernacka, J.M.; Charney, A.; et al. Social connectedness as a determinant of mental health: A scoping review. PLoS ONE 2022, 17, e0275004. [Google Scholar] [CrossRef]
- Shen, C.; Rolls, E.; Cheng, W.; Kang, J.; Dong, G.; Xie, C.; Zhao, X.M.; Sahakian, B.; Feng, J. Associations of Social Isolation and Loneliness with Later Dementia. Neurology, 2022; Online ahead of print. [Google Scholar] [CrossRef]
- Zhong, B.L.; Chen, S.L.; Conwell, Y. Effects of Transient Versus Chronic Loneliness on Cognitive Function in Older Adults: Findings From the Chinese Longitudinal Healthy Longevity Survey. Am. J. Geriatr. Psychiatry 2016, 24, 389–398. [Google Scholar] [CrossRef]



 Interaction between the regional neuro-organizations and the primary care level. New models of care linking primary, secondary, and tertiary prevention are needed to promote brain health in healthy subjects and in patients with brain disorders and to coordinate interactions between the different stakeholders at local, regional, and national levels.
Interaction between the regional neuro-organizations and the primary care level. New models of care linking primary, secondary, and tertiary prevention are needed to promote brain health in healthy subjects and in patients with brain disorders and to coordinate interactions between the different stakeholders at local, regional, and national levels.
 Interaction between the regional neuro-organizations and the primary care level. New models of care linking primary, secondary, and tertiary prevention are needed to promote brain health in healthy subjects and in patients with brain disorders and to coordinate interactions between the different stakeholders at local, regional, and national levels.
Interaction between the regional neuro-organizations and the primary care level. New models of care linking primary, secondary, and tertiary prevention are needed to promote brain health in healthy subjects and in patients with brain disorders and to coordinate interactions between the different stakeholders at local, regional, and national levels.

The following five factors are essential for brain health: physical health, healthy environments, safety and security, learning and social connection, and access to quality services.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bassetti, C.L.A.; Heldner, M.R.; Adorjan, K.; Albanese, E.; Allali, G.; Arnold, M.; Bègue, I.; Bochud, M.; Chan, A.; do Cuénod, K.Q.; et al. The Swiss Brain Health Plan 2023–2033. Clin. Transl. Neurosci. 2023, 7, 38. https://doi.org/10.3390/ctn7040038
Bassetti CLA, Heldner MR, Adorjan K, Albanese E, Allali G, Arnold M, Bègue I, Bochud M, Chan A, do Cuénod KQ, et al. The Swiss Brain Health Plan 2023–2033. Clinical and Translational Neuroscience. 2023; 7(4):38. https://doi.org/10.3390/ctn7040038
Chicago/Turabian StyleBassetti, Claudio L. A., Mirjam R. Heldner, Kristina Adorjan, Emiliano Albanese, Gilles Allali, Marcel Arnold, Indrit Bègue, Murielle Bochud, Andrew Chan, Kim Q. do Cuénod, and et al. 2023. "The Swiss Brain Health Plan 2023–2033" Clinical and Translational Neuroscience 7, no. 4: 38. https://doi.org/10.3390/ctn7040038
APA StyleBassetti, C. L. A., Heldner, M. R., Adorjan, K., Albanese, E., Allali, G., Arnold, M., Bègue, I., Bochud, M., Chan, A., do Cuénod, K. Q., Du Pasquier, R., Draganski, B., Eshmawey, M., Felbecker, A., Fischer, U., Frahsa, A., Frisoni, G. B., Grossmann, H., Guzman, R., ... Remonda, L. (2023). The Swiss Brain Health Plan 2023–2033. Clinical and Translational Neuroscience, 7(4), 38. https://doi.org/10.3390/ctn7040038

















