Awake Prone-Positioning in Patients on Non-Invasive Ventilation for Management of SARS-CoV-2 Pneumonia: A Systematic Review
Abstract
:Highlights
- Awake proning has an established role in both COVID and non-COVID acute hypoxemic respiratory failure (AHRF).
- Patients with COVID AHRF are often on NIV, and the use of awake prone positioning may pose concerns regarding feasibility, efficacy and side effects.
- This systematic review was undertaken to evaluate the feasibility and efficacy of awake proving along with NIV in NIV patients.
- Awake proning in NIV patients had a feasibility ranging from 36 to 100% and an increased efficacy in terms of improvement in oxygenation with no significant side effects.
- We observed a moderate-to-serious risk of bias amongst the included non-randomized observational studies and heterogeneity in terms of respiratory supports and/or the interface used by the patients.
Abstract
1. Introduction
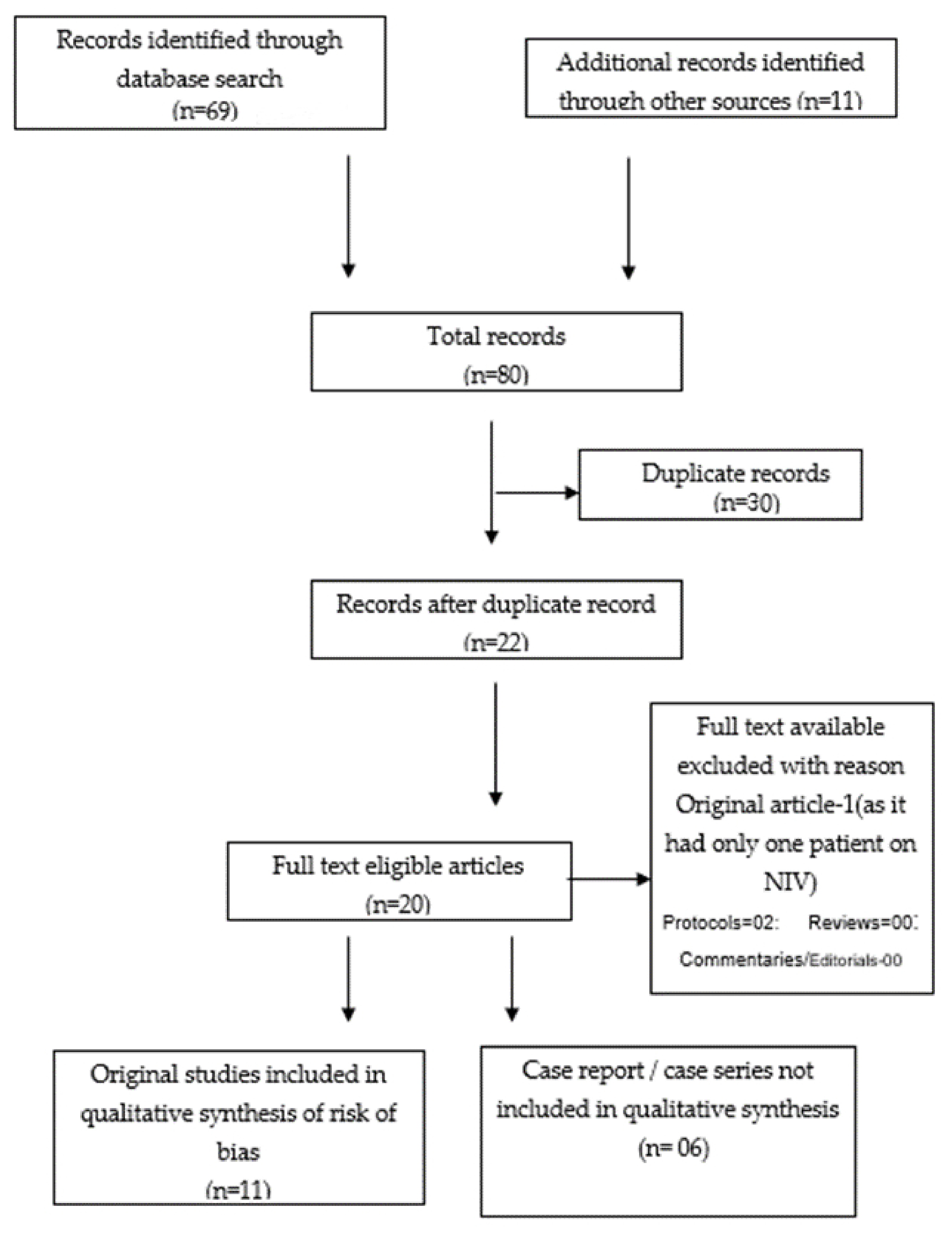
2. Literature Search and Data Source
3. Results
3.1. Awake PP along with NIV in Patients with COVID-19 Pneumonia in Different Setups i.e., ICU and Non-ICU Setups
3.2. Awake PP with Helmet CPAP
3.3. Risk of Bias (Quality) Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gordon, A.; Rabold, E.; Thirumala, R.; Husain, A.A.; Patel, S.; Cheema, T. Prone Positioning in ARDS. Crit. Care Nurs. Q. 2019, 42, 371–375. [Google Scholar] [CrossRef] [PubMed]
- Munshi, L.; Del Sorbo, L.; Adhikari, N.K.; Hodgson, C.L.; Wunsch, H.; Meade, M.O.; Uleryk, E.; Mancebo, J.; Pesenti, A.; Ranieri, V.M.; et al. Prone Position for Acute Respiratory Distress Syndrome. A Systematic Review and Meta-Analysis. Ann. Am. Thorac. Soc. 2017, 14, S280–S288. [Google Scholar] [CrossRef] [PubMed]
- Sodhi, K.; Chanchalani, G. Awake Proning: Current Evidence and Practical Considerations. Indian J. Crit. Care Med. 2020, 24, 1236–1241. [Google Scholar]
- Bamford, P.; Bentley, A.; Dean, J.; Whitmore, D. ICS Guidance for Prone Positioning of the Conscious COVID Patient; Intensive Care Society: London, UK, 2020. [Google Scholar]
- Chad, T.; Sampson, C. Prone positioning in conscious patients on medical wards: A review of the evidence and its relevance to patients with COVID-19 infection. Clin. Med. 2020, 20, e97–e103. [Google Scholar] [CrossRef]
- Winck, J.C.; Ambrosino, N. COVID-19 pandemic and non invasive respiratory management: Every Goliath needs a David. An evidence based evaluation of problems. Pulmonology 2020, 26, 213–220. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. Guidance for the Role and Use of Non-Invasive Respiratory Support in Adult Patients with COVID-19 (Confirmed or Suspected); NICE: Ra’anana, Israel, 2020; Available online: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/specialty-guide-NIV-respiratory-support-and-coronavirus-v3.pdf (accessed on 25 November 2021).
- Coppo, A.; Bellani, G.; Winterton, D.; Di Pierro, M.; Soria, A.; Faverio, P.; Cairo, M.; Mori, S.; Messinesi, G.; Contro, E.; et al. Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): A prospective cohort study. Lancet Respir. Med. 2020, 8, 765–774. [Google Scholar] [CrossRef]
- Sartini, C.; Tresoldi, M.; Scarpellini, P.; Tettamanti, A.; Carcò, F.; Landoni, G.; Zangrillo, A. Respiratory Parameters in Patients With COVID-19 After Using Noninvasive Ventilation in the Prone Position Outside the Intensive Care Unit. JAMA 2020, 323, 2338–2340. [Google Scholar] [CrossRef] [PubMed]
- Retucci, M.; Aliberti, S.; Ceruti, C.; Santambrogio, M.; Tammaro, S.; Cuccarini, F.; Carai, C.; Grasselli, G.; Oneta, A.M.; Saderi, L. Prone and Lateral Positioning in Spontaneously Breathing Patients With COVID-19 Pneumonia Undergoing Noninvasive Helmet CPAP Treatment. Chest 2020, 158, 2431–2435. [Google Scholar] [CrossRef]
- Hallifax, R.J.; Porter, B.M.; Elder, P.J.; Evans, S.B.; Turnbull, C.D.; Hynes, G.; Lardner, R.; Archer, K.; Bettinson, H.V.; Nickol, A.H.; et al. Successful awake proning is associated with improved clinical outcomes in patients with COVID-19: Single-centre high-dependency unit experience. BMJ Open Respir. Res. 2020, 7, e000678. [Google Scholar] [CrossRef]
- Khanum, I.; Samar, F.; Fatimah, Y.; Safia, A.; Adil, A.; Kiren, H.; Nosheen, N.; Faisal, M.; Bushra, J. Role of awake prone positioning in patients with moderate-to-severe COVID-19: An experience from a developing country. Monaldi Arch. Chest Dis. 2021, 91, 10. [Google Scholar] [CrossRef]
- Tonelli, R.; Pisani, L.; Tabbì, L.; Comellini, V.; Prediletto, I.; Fantini, R.; Marchioni, A.; Andrisani, D.; Gozzi, F.; Bruzzi, G.; et al. Early awake proning in critical and severe COVID-19 patients undergoing noninvasive respiratory support: A retrospective multicenter cohort study. Pulmonology 2021, 28, 181–192. [Google Scholar] [CrossRef] [PubMed]
- Burton-Papp, H.C.; Jackson, A.I.; Beecham, R.; Ferrari, M.; Nasim-Mohi, M.; Grocott, M.P.; Chambers, R.; Dushianthan, A.; REACT COVID Investigators. Conscious prone positioning during non-invasive ventilation in COVID-19 patients: Experience from a single centre. F1000Research 2020, 9, 859. [Google Scholar] [CrossRef] [PubMed]
- Paternoster, G.; Sartini, C.; Pennacchio, E.; Lisanti, F.; Landoni, G.; Cabrini, L. Awake pronation with helmet continuous positive airway pressure for COVID-19 acute respiratory distress syndrome patients outside the ICU: A case series. Med. Intensiva (Engl. Ed.) 2020, 46, 65–71. [Google Scholar] [CrossRef]
- Winearls, S.; Swingwood, E.L.; Hardaker, C.L.; Smith, A.M.; Easton, F.M.; Millington, K.J.; Hall, R.S.; Smith, A.; Curtis, K.J. Early conscious prone positioning in patients with COVID-19 receiving continuous positive airway pressure: A retrospective analysis. BMJ Open Respir. Res. 2020, 7, e000711. [Google Scholar] [CrossRef] [PubMed]
- Simioli, F.; Annunziata, A.; Langella, G.; Martino, M.; Musella, S.; Fiorentino, G. Early Prone Positioning and Non-Invasive Ventilation in a Critical COVID-19 Subset. A Single Centre Experience in Southern Italy. Turk. Thorac. J. 2021, 22, 57–61. [Google Scholar] [CrossRef]
- Rosén, J.; von Oelreich, E.; Fors, D.; Jonsson Fagerlund, M.; Taxbro, K.; Skorup, P.; Eby, L.; Campoccia Jalde, F.; Johansson, N.; Bergström, G.; et al. Awake prone positioning in patients with hypoxemic respiratory failure due to COVID-19: The PROFLO multicenter randomized clinical trial. Crit. Care 2021, 25, 209. [Google Scholar] [CrossRef]
- Jouffroy, R.; Darmon, M.; Isnard, F.; Geri, G.; Beurton, A.; Fartoukh, M.; Tudesq, J.-J.; Nemlaghi, S.; Demoule, A.; Azoulay, E.; et al. Impact of prone position in non-intubated spontaneously breathing patients admitted to the ICU for severe acute respiratory failure due to COVID-19. J. Crit. Care 2021, 64, 199–204. [Google Scholar] [CrossRef]
- Ripoll-Gallardo, A.; Grillenzoni, L.; Bollon, J.; Della Corte, F.; Barone-Adesi, F. Prone Positioning in Non-Intubated Patients with COVID-19 Outside of the Intensive Care Unit: More Evidence Needed. Disaster Med. Public Health Prep. 2020, 14, e22–e24. [Google Scholar] [CrossRef]
- Bastoni, D.; Poggiali, E.; Vercelli, A.; Demichele, E.; Tinelli, V.; Iannicelli, T.; Magnacavallo, A. Prone positioning in patients treated with non-invasive ventilation for COVID-19 pneumonia in an Italian emergency department. Emerg. Med. J. 2020, 37, 565–566. [Google Scholar] [CrossRef]
- Golestani-Eraghi, M.; Mahmoodpoor, A. Early application of prone position for management of Covid-19 patients. J. Clin. Anesth. 2020, 66, 109917. [Google Scholar] [CrossRef]
- Rauseo, M.; Mirabella, L.; Caporusso, R.R.; Cantatore, L.P.; Perrini, M.P.; Vetuschi, P.; Cinnella, G. SARS-CoV-2 pneumonia succesfully treated with cpap and cycles of tripod position: A case report. BMC Anesthesiol. 2021, 21, 9. [Google Scholar] [CrossRef] [PubMed]
- Sellmann, T.; Maurer, C.; Thal, S.C. Nichtinvasive Beatmungs- und Lagerungstherapie bei COVID-19: Kasuistik und Literaturübersicht [Noninvasive ventilation and positional therapy in COVID-19: Case report and literature review]. Anaesthesist 2021, 70, 649–654. [Google Scholar] [CrossRef] [PubMed]
- Cruz Salcedo, E.M.; Rodriguez, L.M.; Patel, J.; Seevaratnam, A.R. Use of Dexmedetomidine in Early Prone Positioning Combined With High-Flow Nasal Cannula and Non-Invasive Positive Pressure Ventilation in a COVID-19 Positive Patient. Cureus 2020, 12, e10430. [Google Scholar] [CrossRef] [PubMed]
- Kandasamy, S.; Rao, S.V.; Udhayachandar, R.; Rao, V.B.; Raju, N.A.; Nesaraj, J.J.; Samuel, P. Voluntary Prone Position for Acute Hypoxemic Respiratory Failure in Unintubated Patients. Indian J. Crit. Care Med. 2020, 24, 557–562. [Google Scholar] [CrossRef]
- Tavernier, E.; McNicholas, B.; Pavlov, I.; Roca, O.; Perez, Y.; Laffey, J.; Mirza, S.; Cosgrave, D.; Vines, D.; Frat, J.-P.; et al. Awake prone positioning of hypoxaemic patients with COVID-19: Protocol for a randomised controlled open-label superiority meta-trial. BMJ Open 2020, 10, e041520. [Google Scholar] [CrossRef]
- Ibarra-Estrada, M.Á.; Marín-Rosales, M.; García-Salcido, R.; Aguirre-Díaz, S.A.; Vargas-Obieta, A.; Chávez-Peña, Q.; Aguirre-Avalos, G. Prone positioning in non-intubated patients with COVID-19 associated acute respiratory failure, the PRO-CARF trial: A structured summary of a study protocol for a randomised controlled trial. Trials 2020, 21, 940. [Google Scholar] [CrossRef]
- McGuiness, L.A. Robvis: An R Package and Web Application for Visualizing Risk-of-Bias Assessments. 2019. Available online: https://github.com/mcguinlu/robvis (accessed on 15 December 2020).
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Chilkoti, G.T.; Mohta, M.; Saxena, A.K.; Ahmad, Z.; Sharma, C.S. Awake prone positioning in the management of COVID-19 pneumonia: A systematic review. Indian Crit. Care Med. 2021, 25, 897–906. [Google Scholar]
- Touchon, F.; Trigui, Y.; Prud’Homme, E.; Lefebvre, L.; Giraud, A.; Dols, A.M.; Elharrar, X. Awake prone positioning for hypoxaemic respiratory failure: Past, COVID-19 and perspectives. Eur. Respir. Rev. 2021, 30, 210022. [Google Scholar] [CrossRef]
- Conti, G.; Costa, R.; Antonelli, M. Non-invasive ventilation in immunocompromised patients. Minerva Anestesiol. 2011, 77, 342–348. [Google Scholar]
- Huang, H.B.; Xu, B.; Liu, G.Y.; Lin, J.D.; Du, B. Use of non-invasive ventilation in immunocompromised patients with acute respiratory failure: A systematic review and meta-analysis. Crit. Care 2017, 21, 4. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Khanna, P.; Sarkar, S. High-Flow Nasal Cannula, a Boon or a Bane for COVID-19 Patients? An Evidence-Based Review. Curr. Anesthesiol. Rep. 2021, 11, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Hani, C.; Trieu, N.H.; Saab, I.; Hani, C.; Trieu, N.H.; Saab, I. COVID-19 pneumonia: A review of typical CT findings and differential diagnosis. Diagn. Interv. Imaging 2020, 101, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Patel, B.K.; Wolfe, K.S.; Pohlman, A.S.; Hall, J.B.; Kress, J.P. Effect of noninvasive ventilation delivered by helmet vs face mask on the rate of endotracheal intubation in patients with acute respiratory distress syndrome: A randomized clinical trial. JAMA 2016, 315, 2435–2441. [Google Scholar] [CrossRef] [PubMed]
- Patel, B.K.; Wolfe, K.S.; MacKenzie, E.; Salem, D.; Esbrook, C.L.; Pawlik, A.S.; Kress, J.P. One-year outcomes in patients with acute respiratory distress syndrome enrolled in a randomized clinical trial of helmet versus facemask noninvasive ventilation. Crit. Care Med. 2018, 46, 1078–1084. [Google Scholar] [CrossRef]


| Authors | Type of Study/Single or Multicentric | Set Up | N | Mean Age (SD/IQR) of Patients in PP | Mode of Oxygen Therapy Interface Used | Measure/ Outcomes and Their Interval of Measurements | Duration of Proning | Feasibility | Efficacy | Complications | Conclusion | Limitations |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coppo et al., 2020 [8] | Single centre, prospective cohort, feasibility study, Single centric | Ward/ED/Resp HDU | 56 | 57·4 (7·4) | Patients on either Helmet CPAP or COT | PaO2/FiO2 at 10 min after PP and 1 h after resupination; Safety, Feasibility, PaCO2 | Initially 3 h, up to 7 h | Feasible in 83.9% of patients (i.e., for at least 3 h). Unfeasible in rest due to discomfort, coughing, non-cooperation, worsening oxygenation | ETI rate similar in responders vs. non-responders (26% vs. 30%) P/F ratio increased after PP (180.5 mm Hg vs. 285.5 mm Hg). 50% were labelled ‘’ responders’’ who maintained oxygenation after resupination | - | Prone positioning in awake, spontaneously breathing patients is feasible outside of the critical care environment in most patients. | Lack of control group; lack of randomisation, Selection bias; Single centre data |
| Sartini et al., 2020 [9] | Cross-sectional, before-after study Single centric | Non-ICU | 15 | 59 (SD 6.5) | Patients on NIV | SpO2, P/F ratio, RR, and patients’ comfort were assessed at 3 time points while on NIV in PP i.e., baseline, at 60 min after starting NIV, and after 60 min of end of NIV session | Median number of NIV cycles in the PP was 2 (IQR- 1-3 cycles) for a total duration of 3 h (IQR: 1-6 h) | Feasible in all | Significant reduction in RR both during and after pronation; significant improvement in SpO2 and P/F during pronation in all. Sustained improvement in SpO2 and PaO2/FiO2 in 80% (n = 12); unchanged 13.3% (n = 2); and worsened in 6.7% (n = 1) | - | NIV in the prone position to patients with COVID-19 and ARDS on the general wards was feasible with higher oxygenation was higher during and after pronation. | Small sample size; Short duration of NIV in PP; No control group; Selection bias |
| Retucci et al., 2020 [10] | Pilot, observational, & prospective study Single centric | Resp HDU | 26 | 62 (IQR: 56-69); | Patients on helmet CPAP treatment with P/F ratio <250 for more than 48 h | (Assessment in both PP and Lateral position) Success of proning trial i.e., a decrease of the A-a O2 gradient of at least 20%; Equal or reduced RR and dyspnoea; SBP ≥90 mm Hg | One hour | Feasible in 92% (n = 24), not feasible in two, reason was discomfort | Among trials in PP, 33.3% succeeded; 41.7% showed decreased A-a O2 by <20%, and 25% failed. Among trials conducted in lateral positioning, 8% succeeded; 52% showed decreased A-a O2 by <20%, and 40% failed | - | Prone positioning had greater benefit than lateral position in patients on NIV The increase in A-a O2 was <20% and was not sustained in the semi-recumbent position. | Did not assess the clinical outcome or confounders such as FiO2 or length of CPAP trial before PP; Evaluation of response was conducted after only one hour |
| Hallifax et al., 2020 [11] | Retrospective study Single centric | Resp HDU | Total 48 PP-30 | 69 (IQR 54-80) | Patients on CPAP/HFNC | Feasibility Death with PP | >2 h, twice daily for at least 2 days | Proning was achieved in 36.7% of patients and semiproning in 56.7% of patients. 6.7% of patients refused proning after initial attempt | Achievement of full PP associated with lower mortality than failed or semi-proning (0.0% vs. 63.2%.) | - | Patients on CPAP more likely to be able to successfully prone than those on HFNC (52.9% vs. 15.4%) | Potential selection bias, lack of control group |
| Khanum et al., 2021 [12] | Retrospective, observational study Single centric | Special Care Unit | 23 | 54.5 (SD 11.7) | Oxygen therapy with or without NIV | Avoidance of intubation, mortality, length of hospital stay | No prefixed targeted duration but for >1 day | Feasible in all patients | Only one patient required intubation and died, rest 22 improved after 3–5 days Mean hospital stay 12 days. | - | All discharged home on room air or minimal oxygen requirement | Small and heterogenous sample size, no defined duration of PP, no control group |
| Tonelli et al., 2021 [13] | Retrospective observational study Multicentric cohort | ICU | 114 (Standard treatment = 76 PP = 38) | PP = 61 (IQR 32–75) Standard treatment = 70 (IQR 33-80) | Patients either on NIV/HFNC/CPAP | Intubation rate, in-hospital mortality, time to intubation, tracheostomy, length of ICU and hospital stay | 3 h (1–4 sessions/day) | - | Reduced intubation rate with PP (18% vs. 39.5%, Less time spent in PP independently associated with IMV. Respiratory support free days with PP vs. standard (20 vs. 15), length of ICU (10 vs. 15 days) and hospital stay (20 vs. 24 days) shorter in PP than standard care | - | PP significantly reduces intubation rate in patients on HFNC but not NIV or CPAP. Time to intubation, tracheostomy, mortality rates did not differ between standard care and PP groups | Different SOPs in both centres; duration of PP was variable; non-randomised sample; patients in PP group was significantly younger |
| Burton et al.2020 [14] | Retrospective observational study Single centric | ICU | 20 | 53.4 ± 8.3 | Patients on NIV (CPAP mask) | P/F ratio, changes in HR & RR before, during and after proning | 5 cycles (IQR 6.3) with mean duration of 3 h (IQR 2) | Feasibility in 65% (7 out of 20 non-compliant) | P/F ratio increased by 28.7 mm Hg, no significant change in HR, RR was noted | - | PP in conjunction with NIV can improve oxygenation without significant adverse effect | Median age <60 yr (results can not be translated to older age group), small sample size, no set criteria for PP or intubation |
| Paternoster et al. 2020 [15] | Retrospective observational single centric study | HDU | 11 | 62 (10) | Helmet CPAP in prone after failing CPAP trial in supine position (PF < 150) | P/F ratio, SpO2, RR baseline, then after 24, 48 and 72 h of PP | 12 h proning followed by 6 h supination | Feasible in all patients. Sedation (Dexmedetomidine) improved comfort. Mean duration 7 ± 2.7 days | P/F increased from prior to proning 10.75 ± 20.8 to 244.4 ± 106.2 after 72 h of proning (p < 0.001), SpO2 increased from 90.6 + 2.3 to 96 + 3.1 (p < 0.001). RR decreased from 27.6 ± 4.3 to 20.1 ± 4.7 after 72 h. | - | 27% of patients required IMV Overall 28-day survival rate was 82%. | Non -randomized, small sample size, no control group |
| Winearls et al. 2020 [16] | Retrospective study Single centric | Resp HDU | 24 | 62 (13) | CPAP full face mask | P/F ratio & ROX index at baseline, 15 min after PP initiation, one hour after PP while on CPAP | 8 ± 5 h in first 24 h (mean of 10 ± 5 days) | Feasibility- 92% (2 failed to tolerate PP; 12 able to fully prone, 10 semiprone) | ROX index (7.0 ± 2.5 baseline vs. 11.4 ± 3.7 on CPAP with PP) and P/F ratio increased significantly on CPAP with PP (from 252 ± 87 mm Hg vs. 252 ± 87 mm Hg). Increase maintained only for one hour after cessation of PP | No complications | PP along with CPAP therapy is feasible, safe and improves oxygenation No difference in outcome with fully prone vs. semiprone position | Non-randomized, no control, small sample size, no defined proning protocol |
| Simioli et al., 2021 [17] | Retrospective Case control study Single centric | Resp HDU | 29 | 64 (±22.5) | Helmet/CPAP full face mask/HFNC (10 Helmet CPAP, 13 full CPAP face mask, and 6 HFNC) | P/F ratio at baseline, 2 h after NIV and after 10 h of initiating PP feasibility | At least 10 h/day with cycling every 2 h alternately between prone, right and left lateral and semiupright position | Feasibility—62% (11 patients were noncompliant Tolerability better in CPAP full face masks than helmet. Causes of non-compliance are interface displacement, oxygen desaturation, worsening of dyspnea, chest tightness, neck pain, and agitation | P/F ratio increased significantly during PP (288 ± 80 vs. 202 + 122), duration of respiratory failure significantly shorter with PP (median 14 vs. 21 days). Need for IMV less in PP group (5.5% vs. 18%) | No complications | PP along with NIV efficacious when started early and for at least 10 h/day. | Small sample size |
| Rosen et al., 2021 [18] | Randomised clinical trial Multicentric trial | - | 75 (36-PP 39-Controls) | 65 (53–74) | HFNC/NIV with P/F ratio ≤ 20 kPa or corresponding values of SpO2 and FiO2 | Intubation within 30 days after enrolment | At least 16 h PP per day. Prone and semi-PP allowed | Feasibility-17% (Only 6% of patients able to adhere to the 16 h of proning as defined in this study | 30-day intubation rate not different between cases with PP and controls. (33 & vs. 33%) | 6% of patients had pressure sores in PP group vs. 23% in control group. | No difference in intubation rate, ventilator free days, days free of NIV/HFNC, hospital or ICU stay or organ support with the use of PP. 8% of deaths in control group vs. 17% in PP group. | non blinded |
| Jouffroy et al., 2021 [19] | Retrospective observation study Multicentric trial | ICU | Total 379 patients, 40 PP | 59.5 (56; 64) | HFNC/CPAP/COT (37/1/2) | Intubation within 28 days; mortality within 28 days; rate of ICU discharge | PP for 3–6 h, twice a day | Feasible | After adjusting for factors, neither risk of intubation or 28-day survival showed benefit in PP | - | 58% in the PP group were discharged alive without intubation, 40% required invasive ventilation | Limited proning duration |
| Authors | N/Gender | Age (Yrs) | Set-Up | Mode of Oxygen Therapy/Interface Used | Duration of Proning | Outcome | Conclusion |
|---|---|---|---|---|---|---|---|
| Ripoll-Gallardo et al., 2020 [20] | 13 (85%, males) | 66 | General ward | Patients on helmet NIV CPAP | Maintained as long as patient tolerated | PaO2/FiO2; respiratory rate | Feasible in all; Improved P/F compared to baseline in 12 patients (p = 0.003); No difference was found in the RR before and after PP (p = 0.20) |
| Bastoni et al., 2020 [21] | 10 (80% males) | 73 (62–87) | Emergency department | Patients on helmet NIV CPAP with no clinical improvement | 1 h | P/F ratio; Lung USG | Feasibility—60%; An improvement in P/F ratio from 68 ± 5 mm Hg to 97 ± 8 mm Hg after 1 h of PP in all; No change in B-line quantity and distribution in lung USG after 1 h |
| Golestani Eraghi M et al., 2020 [22] | 10 | - | ICU | Patients with P/F ratio <150 and on helmet NIV | 9 h | PaO2/FiO2 ratio after 1 and 12 h of PP | Feasible in all: 60% of patients had sustained improvement in P/F ratio after 1 h; 30% of patients had delayed positive result and one patient was intubated |
| Rauseo et al. 2021 [23] | 1 (Male) | 77 | ICU | Mild SARS-CoV-2 pneumonia on helmet CPAP | 3 h cycles of semi recumbent and tripod position for three days | Improved P/F ratio, RR and hemodynamic | Tripod position can be safety applied with NIV |
| Sellmann et al. 2021 [24] | 2 (males) | 63 and 77 | ICU | Severe refractory hypoxemia receiving NIV | - | Improved P/F ratio | Prone and lateral positioning is efficacious in improving oxygenation |
| Salcedo et al.2020 [25] | Male | 73 | ICU | Refractory hypoxemia on alternating HFNC and IPPV | 4 h alternate cycles of supine and prone | Improved P/F ratio | Dexmedetomidine may be used effectively to assist with compliance and tolerance with the use of awake PP in patients on NIV |
| Kandasamy et al.2020 [26] | 13 (4 male, 9 females) | 40.7 | ICU | Mild to moderate disease on NIV, HFNC, venturi mask, Nasal cannula | - | P/F ratio improved with PP from 328 ± 65 vs. 154 ± 52 mmHg; A-a O2 gradient improved from a median of 170.5 mm Hg (127.8309) to 49.1 mm Hg IQR (45.0, 56.6) | Favourable and feasible results |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chilkoti, G.T.; Mohta, M.; Ahmad, Z.; Saxena, A.K. Awake Prone-Positioning in Patients on Non-Invasive Ventilation for Management of SARS-CoV-2 Pneumonia: A Systematic Review. Adv. Respir. Med. 2022, 90, 362-375. https://doi.org/10.3390/arm90040046
Chilkoti GT, Mohta M, Ahmad Z, Saxena AK. Awake Prone-Positioning in Patients on Non-Invasive Ventilation for Management of SARS-CoV-2 Pneumonia: A Systematic Review. Advances in Respiratory Medicine. 2022; 90(4):362-375. https://doi.org/10.3390/arm90040046
Chicago/Turabian StyleChilkoti, Geetanjali Tolia, Medha Mohta, Zainab Ahmad, and Ashok Kumar Saxena. 2022. "Awake Prone-Positioning in Patients on Non-Invasive Ventilation for Management of SARS-CoV-2 Pneumonia: A Systematic Review" Advances in Respiratory Medicine 90, no. 4: 362-375. https://doi.org/10.3390/arm90040046
APA StyleChilkoti, G. T., Mohta, M., Ahmad, Z., & Saxena, A. K. (2022). Awake Prone-Positioning in Patients on Non-Invasive Ventilation for Management of SARS-CoV-2 Pneumonia: A Systematic Review. Advances in Respiratory Medicine, 90(4), 362-375. https://doi.org/10.3390/arm90040046





