Highlights
What are the main findings?
- This comprehensive analysis meticulously examined 51 studies, pinpointing 27 that rigorously adhered to stringent criteria. The incorporation of diverse studies afforded a panoramic perspective on COVID-19 reinfection.
- Emphasis was placed on the effectiveness of vaccination, showcasing a remarkable risk reduction of up to 66% with the administration of two vaccine doses.
What is the implication of the main finding?
- In spite of an overall low reinfection rate, the findings unveiled noteworthy patterns. Factors such as non-vaccination, advanced age, and the presence of comorbidities emerged as significant contributors to the likelihood of reinfection.
- While the review furnished valuable insights, it underscored the persistent necessity for more nuanced observational studies. Special attention was urged, particularly regarding emerging variants and the duration of immunity post-infection or post-vaccination.
Abstract
This article aims to systematize the evidence regarding risk factors associated with COVID-19 reinfection. We conducted a systematic review of all the scientific publications available until August 2022. To ensure the inclusion of the most recent and relevant information, we searched the PubMed and Scopus databases. Thirty studies were reviewed, with a significant proportion being analytical observational case-control and cohort studies. Upon qualitative analysis of the available evidence, it appears that the probability of reinfection is higher for individuals who are not fully immunized when exposed to a new variant, females, those with pre-existing chronic diseases, individuals aged over 60, and those who have previously experienced severe symptoms of the disease or are immunocompromised. In conclusion, further analytical observational case-control studies are necessary to gain a better understanding of the risk factors associated with SARS-CoV-2 (COVID-19) reinfection.
1. Background
SARS-CoV-2, the causative agent of COVID-19, has precipitated a global pandemic [1]. The immune system responds swiftly in infectious processes, and the infection by SARS-CoV-2 (COVID-19) is no exception. Studies from early 2021 initially suggested natural immunity could protect against reinfection for at least 8 to 12 months [2,3]. However, real-world cases have contradicted this, reporting reinfection occurring within 3 to 6 months [4,5]. Furthermore, the understanding of sustainable, long-lasting protective immunity post-COVID-19 infection remains uncertain, and the underlying mechanisms are not yet fully comprehended [6,7]. Immunity following infection is often established through immune responses involving IgG antibodies and orchestrated by specialized T cells. When assessing post-infection immunity, primary considerations encompass the identification of protective functions, delineation of measurable biological markers, and precise definition of terms, such as reinfection, recurrence, readmission, mortality, and transmission to others [8].
In the initial phase of the 2020 pandemic, the first documented instances of SARS-CoV-2 reinfection emerged in Hong Kong. The interval between the two episodes was observed to be 142 days, marked by mild symptoms during the initial infection and an absence of symptoms in the subsequent episode [9]. This discovery prompted the identification of suspected and confirmed cases of reinfection globally [10].
The current concept of reinfection lacks consistency [11]. The European Center for Disease Prevention and Control defines reinfection as confirmed by laboratory studies of two infections by different strains with a minimum distance, as supported by phylogenetic and epidemiological evidence [12]. Vaccination against SARS-CoV-2 has shown promise in reducing infection rates, but there is still ambiguity regarding reinfection cases among fully vaccinated, partially vaccinated, and unvaccinated individuals. The primary obstacle in probing leaky protection within SARS-CoV-2 immunity lies in the inherent difficulty in measuring the viral dose, whether incident or cumulative over time. Current investigations often resort to assessing proxies, such as the proximity and duration of exposure to an infected index case. However, the utility of these proxies is constrained by the scarcity of reliable information at the necessary scales and the potential for misclassification owing to movement and social interactions in real-world settings [13].
Despite explicit safety measures recommending full vaccination, mask-wearing, and social distancing for all, including rehabilitated patients, there are studies suggesting the possibility of reinfection among this group [14]. An intriguing study conducted within a prison population underscores the imperative for stratified interventions to curtail the spread of SARS-CoV-2, particularly in dense settings, such as congregate environments. This necessity is emphasized in situations where prolonged contact is probable, such as households with infected individuals [13].
Reports of possible reinfections by COVID-19 after the initial recovery have increased over time [15]. Recent studies have highlighted the unknown degree of protective immunity conferred by SARS-CoV-2 infection, making the understanding of reinfection possibilities crucial [16]. This comprehension is pivotal for informing global health and government policies and may contribute to evaluating the feasibility of the concept of herd immunity, a topic discussed by some scientists [17,18,19].
Early risk stratification in COVID-19 remains challenging [7]. Thus, understanding reinfection by COVID-19 becomes a critical element guiding government and public health policies [6,20]. The present study aims to systematically present the most relevant evidence on the risk factors associated with COVID-19 reinfection. Investigating factors linked to COVID-19 reinfections is essential for assessing the past pandemic’s landscape, as ignorance on this matter could complicate vaccine development and perpetuate viral outbreaks worldwide. This study addresses the existing gaps in the understanding of COVID-19 reinfections by conducting a systematic review of currently available clinical cases.
2. Methodology
This systematic review adhered to the guidelines outlined in the preferred reporting items for systematic reviews and meta-analyses (PRISMA) protocols [21].
2.1. Bibliographic Search Strategy
The selection of scientific articles involved a comprehensive search of research articles within the databases of the PubMed and Scopus repositories. To structure the bibliographic search strategy, specific descriptors related to factors such as reinfection, COVID-19, and SARS-CoV-2 were employed. The search was confined to studies published from 2019 onward, coinciding with the occurrence of the first COVID-19 case. Inclusivity extended to all the studies providing substantial data on COVID-19 reinfection, without imposing restrictions based on language, age, or sex (Table S1). In this investigation, COVID-19 reinfection was delineated as the emergence of a new infection after the declaration of recovery from a prior infection. References within the included articles were scrutinized as potential sources for additional studies.
2.2. Eligibility Criteria
The nature of the study guided a systematic review following specific criteria. The inclusion criteria encompassed analytical observational designs, including cases and controls, cohorts, and, when necessary, descriptive studies. It is important to highlight that case reports were deliberately excluded from the systematic review. Furthermore, the study emphasized the inclusion of evaluation studies that investigated elements associated with risk factors for COVID-19 reinfection or studies focused on the recurrence of the disease.
2.3. Selection of Studies and Data Extraction
The titles and abstracts of the pertinent articles, extracted from the databases, were transferred to the Rayyan online software for the systematic organization of the literature search results. Following the elimination of duplicates, the process for selecting articles based on the title and abstract was conducted independently by two reviewers (WGG and HMZ). Any disagreements were resolved through discussions to achieve consensus. Subsequently, the ultimate inclusion of articles was determined based on the full texts, independently assessed by all the authors.
2.4. Summary of Results
The outcome of this review enabled a qualitative analysis of factors associated with COVID-19 reinfection.
2.5. Synthesis of Results
A formal narrative synthesis of the gathered data was performed, while a formal statistical synthesis was not pursued. Syntheses primarily focused on qualitatively analyzing clinical manifestations mentioned in each country of the published studies.
2.6. Study Quality Assessment
Given the enduring nature of the COVID-19 pandemic, our focus was on studies conducted between 2020 and 2022, a period marked by the highest concentration of cases. The quality assessment of the included articles was independently conducted by two reviewers, CGB and MGL, utilizing established criteria. By employing the Joanna Briggs Institute critical appraisal tools for use in JBI systematic reviews, studies were evaluated for methodological quality and assigned a score of either present (1) or absent (0), which was then tallied to derive a final value [22]. The two reviewers reached a consensus on the quality assessment results through discussion. The Newcastle-Ottawa scale (NOS) was used to analyze the risk of bias [23].
3. Results
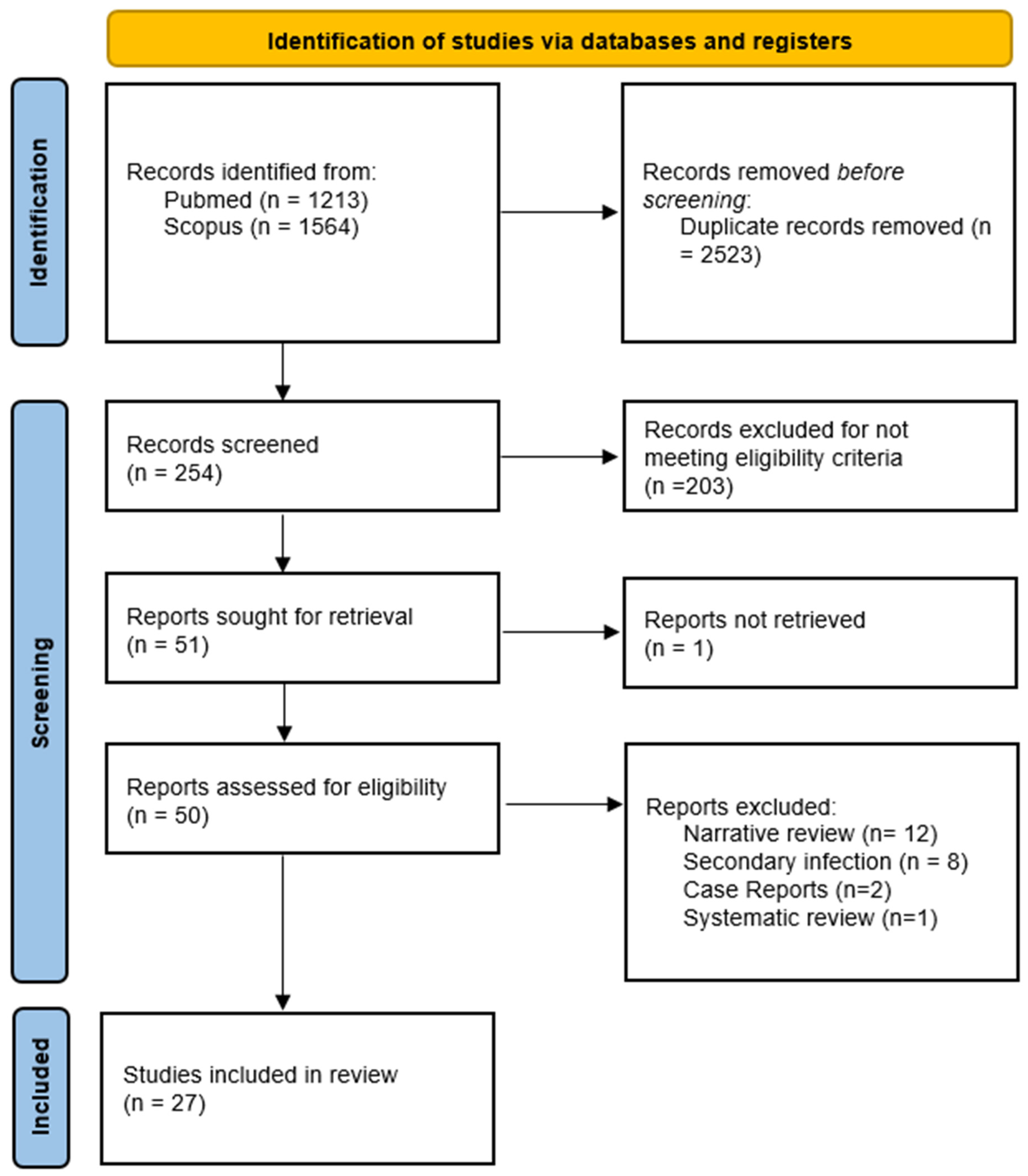
In the initial phase of the literature search, a total of 2777 records were identified. After the removal of 2523 duplicate entries, a subsequent screening process, which involved assessing titles and abstracts, resulted in 254 articles under consideration. Following this, 203 articles were excluded, leaving 51 studies for an in-depth evaluation of their full texts. Following a meticulous review, 30 articles were ultimately determined to meet the pre-established inclusion criteria and were subjected to detailed analysis as a part of the systematic review (Figure 1).
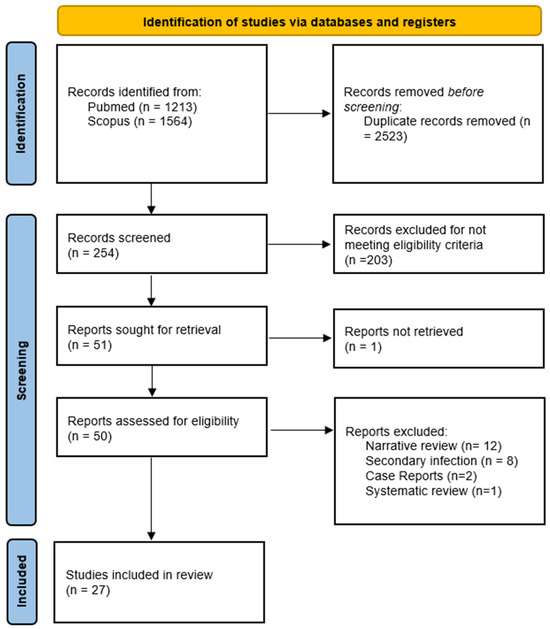
Figure 1.
PRISMA flowchart to show the study selection process.
The systematization of the analyzed articles is shown in Table 1.

Table 1.
Analytical observational studies from the beginning of COVID-19 to August 2022.
A total of 27 articles were included in this systematic review, with 20 corresponding to case-control studies and cohorts. Most of the reviewed literature originated from European countries, indicating a biomedical research focus on the relationship between previous COVID-19 episodes and reinfection by SARS-CoV-2. Following Europe, studies from America, Asia, the Middle East, and other locations were considered.
The evaluation of the manuscript quality was conducted using the Joanna Briggs Institute critical appraisal tools designed for JBI systematic reviews, and the comprehensive results are outlined in Table S2. Additionally, an in-depth analysis of the risk of bias using the NOS scale is meticulously presented in Table S3.
A commonality among the selected studies is the association with intrinsic aspects, such as non-immunization, incomplete immunization, and their correlation with the female gender. In the analyzed cases, a prevailing element is the low rates of reinfection.
Concerning associated risks in healthcare workers during the COVID-19 pandemic, it was determined that intrahospital infections and reinfections were mostly associated with the Omicron variant, with few cases linked to the Delta variant [42,44] in different geographical locations.
Factors contributing to greater recurrence in the analyzed studies include aspects related to immunocompromised patients and an increase in age. The risk, with or without booster doses, tends to rise with age. Comorbidities, such as obesity, asthma, HIV, and diabetes mellitus, were also significant, with the association of more than two factors increasing the risk of reinfection.
For the unvaccinated, studies revealed reinfection probabilities ranging from 2 to 4 times, establishing non-vaccination as a significant risk factor. This risk was consistently elevated in the female gender across various locations, indicating a gender-based propensity for reinfection. The reviewed studies concurred in stating that individuals with only one vaccine dose exhibited the highest reinfection rates. In contrast, those with two vaccine doses had an average of a 66% lower risk of reinfection. It was also affirmed that the female gender manifested a higher recurrence rate. Overall, vaccination demonstrated a positive and significant effect against potential reinfection.
Additionally, it was disclosed that children had a lower probability of reinfection compared to adults. These findings collectively contribute to our understanding of the complex dynamics of COVID-19 reinfections and highlight the protective impact of vaccination across different demographics.
4. Discussion
Based on the findings from the analyzed studies, definitive conclusions regarding an increased probability of reinfection in relation to factors such as incomplete immunization and exposure to new variants are challenging to draw [35]. However, being of the female gender, having a pre-existing chronic disease, belonging to the age group of over 60 years, and having previously experienced severe symptoms associated with COVID-19, or in some cases, being immunocompromised, can be considered as factors associated with reinfection [8,11,20,30]. Moreover, the simultaneous presence of more than one of these factors appears to exacerbate the risk of reinfection. It is crucial to note that there is substantial evidence, as supported by the reviewed medical literature, suggesting a high likelihood of association between the aforementioned factors and cases of reinfection by SARS-CoV-2. Additionally, cases linked to the Delta and Omicron variants were directly related to the analyzed factors.
Although China plays a significant role in the pandemic, some studies from there were excluded owing to the language barrier because they were published only in Mandarin Chinese or the equivalent. China’s experience, characterized by stringent control measures and a proactive research approach, holds valuable lessons [30,36]. The swift execution of containment protocols and thorough surveillance has the potential to unveil successful strategies applicable on a global scale. The consideration of these studies in future research is recommended for a more comprehensive and objective understanding of reinfection cases by COVID-19.
Delving deeply into the mechanisms that underpin the efficacy of vaccines in preventing reinfections emerges as a pivotal stride in grasping the intricacies of immunization dynamics [37,38]. Substantial variations in effectiveness have become evident across diverse vaccine types and dosing regimens. mRNA-based vaccines, exemplified by those developed by Pfizer-BioNTech and Moderna, have shown noteworthy efficacy, particularly in countering the challenges posed by emerging variants. In contrast, viral vector vaccines, such as those produced by AstraZeneca and Johnson & Johnson, have yielded somewhat distinct outcomes [13,43,44,47]. The issue of waning effectiveness over time has garnered significant attention. Several studies propose a gradual attenuation of protective measures over time, sparking dialogs on the necessity of booster doses. These insights underscore the critical importance of continuous monitoring and the adaptive refinement of vaccination strategies in response to the ever-evolving epidemiological landscape and the nuanced dynamics of immune responses as time unfolds.
Based on the reviewed literature, it can be concluded that to date, instances of potential reinfection by COVID-19 have been observed, albeit at a low overall rate of reinfection across various global locations. Access to updated data has the potential to offer a more precise understanding of regional trends, enabling a more thorough evaluation of how factors such as socioeconomics and public health strategies interact with the incidence of reinfections [3,25,32]. This detailed exploration goes beyond enhancing the accuracy of our assessments—it becomes a pivotal step toward tailoring control measures more effectively. Moreover, it unveils insights into local determinants that may play a crucial role in shaping the incidence of reinfections within the ongoing context of the pandemic. In essence, staying abreast of the latest data not only refines our strategic responses but also unveils nuanced perspectives that are invaluable in navigating the complexities of the current public health landscape [12,28,33].
Despite the valuable insights provided by the studies included in this systematic review, it is important to acknowledge and address their inherent limitations. One notable concern is the potential for bias in study selection, given that most of the studies originate from European countries, raising the possibility of geographical bias in the results. Additionally, the diverse definitions of reinfection across these studies may have affected the data homogeneity, making direct comparisons challenging. Variations in inclusion and exclusion criteria, as well as methodological differences, could also introduce systematic biases. These potential limitations underscore the need for cautious interpretation of the results and emphasize the significance of future research to reconcile methodological variations, ensuring a more nuanced and comprehensive understanding of COVID-19 and SARS-CoV-2 reinfection rates.
To enhance our understanding of the risk factors associated with SARS-CoV-2 reinfection, there is a clear need for more studies employing an observational analytical design, including cases and controls. Molecular studies on the viral genome and its variants, as well as investigations into immune responses stratified by age, gender, and geographic location should not be overlooked. These complementary analyses can provide more precise data, contributing to a comprehensive understanding of the current landscape surrounding cases of COVID-19 and reinfection by SARS-CoV-2.
5. Conclusions
In conclusion, this systematic exploration is designed to unravel the intricate mechanisms associated with COVID-19 and SARS-CoV-2 on a global scale. Anticipating future research endeavors, we expect ongoing efforts to enhance and refine our understanding, offering progressively more accurate data in this dynamic and evolving field.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/arm91060041/s1, Table S1: Search strategy; Table S2: JBI assessment results of studies; Table S3: Newcastle–Ottawa Scale (NOS) Risk of Bias Assessment Results.
Author Contributions
The conception and design of the study were orchestrated by W.G.-G. and H.M.-Z., with meticulous data collection executed by L.A.C.-A., C.G.-B., J.M.-V. and J.Z.-O. The nuanced analysis and interpretation of the data were spearheaded by W.G.-G. and H.M.-Z. The manuscript preparation was skillfully undertaken by M.G.-L. and L.V.-P., while M.E.A.-C. and W.G.-G. provided critical intellectual contributions during the manuscript’s review. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Given that this study entailed a systematic review of pre-existing data without direct engagement with human participants or animals, ethical approval was deemed unnecessary. Despite the absence of formal ethical clearance, we emphasize that this systematic review adhered rigorously to the highest ethical standards, upholding a steadfast commitment to ethical principles throughout its execution.
Informed Consent Statement
Not applicable.
Data Availability Statement
Upon a reasonable request, the corresponding author can provide the study’s data.
Conflicts of Interest
The authors affiliated with this systematic review openly declare the absence of any conflict of interest, affirming the impartiality and integrity of the research process.
References
- Gaudreault, N.N.; Carossino, M.; Morozov, I.; Trujillo, J.D.; Meekins, D.A.; Madden, D.W.; Cool, K.; Artiaga, B.L.; McDowell, C.; Bold, D.; et al. Experimental Re-Infected Cats Do Not Transmit SARS-CoV-2. Emerg. Microbes Infect. 2021, 10, 638–650. [Google Scholar] [CrossRef]
- Rahman, S.; Rahman, M.M.; Miah, M.; Begum, M.N.; Sarmin, M.; Mahfuz, M.; Hossain, M.E.; Rahman, M.Z.; Chisti, M.J.; Ahmed, T.; et al. COVID-19 Reinfections among Naturally Infected and Vaccinated Individuals. Sci. Rep. 2022, 12, 1438. [Google Scholar] [CrossRef]
- Almadhi, M.; Alsayyad, A.S.; Conroy, R.; Atkin, S.; Awadhi, A.A.; Al-Tawfiq, J.A.; AlQahtani, M. Epidemiological Assessment of SARS-CoV-2 Reinfection. Int. J. Infect. Dis. 2022, 123, 9–16. [Google Scholar] [CrossRef]
- Pecho-Silva, S.; Navarro-Solsol, A.C.; Panduro-Correa, V.; Rodriguez-Morales, A.J. COVID-19 Reinfection in a Bolivian Patient. Report of the First Possible Case. Microbes Infect. Chemother. 2021, 1, e1171. [Google Scholar] [CrossRef]
- Arteaga-Livias, K.; Panduro-Correa, V.; Pinzas-Acosta, K.; Perez-Abad, L.; Pecho-Silva, S.; Espinoza-Sánchez, F.; Dámaso-Mata, B.; Rodriguez-Morales, A.J. COVID-19 Reinfection? A Suspected Case in a Peruvian Patient. Travel. Med. Infect. Dis. 2021, 39, 101947. [Google Scholar] [CrossRef]
- West, J.; Everden, S.; Nikitas, N. A Case of COVID-19 Reinfection in the UK. Clin. Med. 2021, 21, e52–e53. [Google Scholar] [CrossRef]
- Pujadas, E.; Chaudhry, F.; McBride, R.; Richter, F.; Zhao, S.; Wajnberg, A.; Nadkarni, G.; Glicksberg, B.S.; Houldsworth, J.; Cordon-Cardo, C. SARS-CoV-2 Viral Load Predicts COVID-19 Mortality. Lancet Respir. Med. 2020, 8, e70. [Google Scholar] [CrossRef]
- Sotoodeh Ghorbani, S.; Taherpour, N.; Bayat, S.; Ghajari, H.; Mohseni, P.; Hashemi Nazari, S.S. Epidemiologic Characteristics of Cases with Reinfection, Recurrence, and Hospital Readmission Due to COVID-19: A Systematic Review and Meta-Analysis. J. Med. Virol. 2022, 94, 44–53. [Google Scholar] [CrossRef]
- To, K.K.-W.; Hung, I.F.-N.; Ip, J.D.; Chu, A.W.-H.; Chan, W.-M.; Tam, A.R.; Fong, C.H.-Y.; Yuan, S.; Tsoi, H.-W.; Ng, A.C.-K.; et al. Coronavirus Disease 2019 (COVID-19) Re-Infection by a Phylogenetically Distinct Severe Acute Respiratory Syndrome Coronavirus 2 Strain Confirmed by Whole Genome Sequencing. Clin. Infect. Dis. 2021, 73, e2946–e2951. [Google Scholar] [CrossRef]
- Santos, V.M.; dos Santos, L.A.M.; dos Modesto, L.C.; Modesto, J.C. Reinfection with SARS-CoV-2: A Challenging Event. Microbes Infect. Chemother. 2021, 1, e1189. [Google Scholar] [CrossRef]
- Ren, X.; Zhou, J.; Guo, J.; Hao, C.; Zheng, M.; Zhang, R.; Huang, Q.; Yao, X.; Li, R.; Jin, Y. Reinfection in Patients with COVID-19: A Systematic Review. Glob. Health Res. Policy 2022, 7, 12. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Reinfection with SARS-CoV: Considerations for Public Health Response; ECDC: Solna, Sweden, 2020. [Google Scholar]
- Lind, M.L.; Dorion, M.; Houde, A.J.; Lansing, M.; Lapidus, S.; Thomas, R.; Yildirim, I.; Omer, S.B.; Schulz, W.L.; Andrews, J.R.; et al. Evidence of Leaky Protection Following COVID-19 Vaccination and SARS-CoV-2 Infection in an Incarcerated Population. Nat. Commun. 2023, 14, 5055. [Google Scholar] [CrossRef] [PubMed]
- Roberts, T.; Keddie, S.H.; Rattanavong, S.; Gomez, S.R.; Bradley, J.; Keogh, R.H.; Bärenbold, O.; Falconer, J.; Mens, P.F.; Hopkins, H.; et al. Accuracy of the Direct Agglutination Test for Diagnosis of Visceral Leishmaniasis: A Systematic Review and Meta-Analysis. BMC Infect. Dis. 2023, 23, 782. [Google Scholar] [CrossRef] [PubMed]
- Arafkas, M.; Khosrawipour, T.; Kocbach, P.; Zielinski, K.; Schubert, J.; Mikolajczyk, A.; Celinska, M.; Khosrawipour, V. Current Meta-Analysis Does Not Support the Possibility of COVID-19 Reinfections. J. Med. Virol. 2021, 93, 1599–1604. [Google Scholar] [CrossRef]
- Tillett, R.L.; Sevinsky, J.R.; Hartley, P.D.; Kerwin, H.; Crawford, N.; Gorzalski, A.; Laverdure, C.; Verma, S.C.; Rossetto, C.C.; Jackson, D.; et al. Genomic Evidence for Reinfection with SARS-CoV-2: A Case Study. Lancet Infect. Dis. 2021, 21, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R.; Cooper, L.A. COVID-19 and Health Equity-A New Kind of “Herd Immunity”. JAMA 2020, 323, 2478–2480. [Google Scholar] [CrossRef]
- Plans-Rubió, P. Percentages of Vaccination Coverage Required to Establish Herd Immunity against SARS-CoV-2. Vaccines 2022, 10, 736. [Google Scholar] [CrossRef]
- Al-Hatamleh, M.A.I.; Abusalah, M.A.; Hatmal, M.M.; Alshaer, W.; Ahmad, S.; Mohd-Zahid, M.H.; Rahman, E.N.S.E.A.; Yean, C.Y.; Alias, I.Z.; Uskoković, V.; et al. Understanding the Challenges to COVID-19 Vaccines and Treatment Options, Herd Immunity and Probability of Reinfection. J. Taibah Univ. Med. Sci. 2022, 18, 600–638. [Google Scholar] [CrossRef] [PubMed]
- SeyedAlinaghi, S.; Afsahi, A.M.; MohsseniPour, M.; Behnezhad, F.; Salehi, M.A.; Barzegary, A.; Mirzapour, P.; Mehraeen, E.; Dadras, O. Late Complications of COVID-19; a Systematic Review of Current Evidence. Arch. Acad. Emerg. Med. 2021, 9, e14. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. Rev. Esp. Cardiol. 2021, 74, 790–799. [Google Scholar] [CrossRef]
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetcu, R.; Currie, M.; Qureshi, R.; Mattis, P.; Lisy, K.; et al. Chapter 7: Systematic Reviews of Etiology and Risk. In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBI: Adelaide, Australia, 2020; Available online: https://Synthesismanual.Jbi.Global (accessed on 3 December 2023).
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses; NOS: Oxford, UK, 2000. [Google Scholar]
- Sacco, C.; Petrone, D.; Del Manso, M.; Mateo-Urdiales, A.; Fabiani, M.; Bressi, M.; Bella, A.; Pezzotti, P.; Rota, M.C.; Riccardo, F.; et al. Risk and Protective Factors for SARS-CoV-2 Reinfections, Surveillance Data, Italy, August 2021 to March 2022. Euro Surveill. 2022, 27, 2200372. [Google Scholar] [CrossRef]
- Flacco, M.E.; Soldato, G.; Acuti Martellucci, C.; Di Martino, G.; Carota, R.; Caponetti, A.; Manzoli, L. Risk of SARS-CoV-2 Reinfection 18 Months After Primary Infection: Population-Level Observational Study. Front. Public Health 2022, 10, 884121. [Google Scholar] [CrossRef] [PubMed]
- Shaheen, N.A.; Sambas, R.; Alenezi, M.; Alharbi, N.K.; Aldibasi, O.; Bosaeed, M. COVID-19 Reinfection: A Multicenter Retrospective Study in Saudi Arabia. Ann. Thorac. Med. 2022, 17, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Nordström, P.; Ballin, M.; Nordström, A. Risk of SARS-CoV-2 Reinfection and COVID-19 Hospitalisation in Individuals with Natural and Hybrid Immunity: A Retrospective, Total Population Cohort Study in Sweden. Lancet Infect. Dis. 2022, 22, 781–790. [Google Scholar] [CrossRef] [PubMed]
- Slezak, J.; Bruxvoort, K.; Fischer, H.; Broder, B.; Ackerson, B.; Tartof, S. Rate and Severity of Suspected SARS-CoV-2 Reinfection in a Cohort of PCR-Positive COVID-19 Patients. Clin. Microbiol. Infect. 2021, 27, 1860.e7–1860.e10. [Google Scholar] [CrossRef] [PubMed]
- Mensah, A.A.; Lacy, J.; Stowe, J.; Seghezzo, G.; Sachdeva, R.; Simmons, R.; Bukasa, A.; O’Boyle, S.; Andrews, N.; Ramsay, M.; et al. Disease Severity during SARS-CoV-2 Reinfection: A Nationwide Study. J. Infect. 2022, 84, 542–550. [Google Scholar] [CrossRef]
- Yao, M.-Q.; Zheng, Q.-X.; Xu, J.; Deng, J.-W.; Ge, T.-T.; Zhou, H.-B.; Wu, F.-T.; Gu, X.-Y.; Yang, Q.; Ren, Y.-L.; et al. Factors Associated with a SARS-CoV-2 Recurrence after Hospital Discharge among Patients with COVID-19: Systematic Review and Meta-Analysis. J. Zhejiang Univ. Sci. B 2020, 21, 940–947. [Google Scholar] [CrossRef]
- Pulliam, J.R.C.; van Schalkwyk, C.; Govender, N.; von Gottberg, A.; Cohen, C.; Groome, M.J.; Dushoff, J.; Mlisana, K.; Moultrie, H. Increased Risk of SARS-CoV-2 Reinfection Associated with Emergence of Omicron in South Africa. Science 2022, 376, eabn4947. [Google Scholar] [CrossRef] [PubMed]
- Al-Otaiby, M.; Krissaane, I.; Al Seraihi, A.; Alshenaifi, J.; Qahtani, M.H.; Aljeri, T.; Zaatari, E.; Hassanain, M.; Algwizani, A.; Albarrag, A.; et al. SARS-CoV-2 Reinfection Rate and Outcomes in Saudi Arabia: A National Retrospective Study. Int. J. Infect. Dis. 2022, 122, 758–766. [Google Scholar] [CrossRef]
- Murillo-Zamora, E.; Mendoza-Cano, O.; Delgado-Enciso, I.; Hernandez-Suarez, C.M. Predictors of Severe Symptomatic Laboratory-Confirmed SARS-CoV-2 Reinfection. Public Health 2021, 193, 113–115. [Google Scholar] [CrossRef]
- Garduño-Orbe, B.; Sánchez-Rebolledo, J.M.; Cortés-Rafael, M.; García-Jiménez, Y.; Perez-Ortiz, M.; Mendiola-Pastrana, I.R.; López-Ortiz, E.; López-Ortiz, G. SARS-CoV-2 Reinfection among Healthcare Workers in Mexico: Case Report and Literature Review. Medicina 2021, 57, 442. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Varela, N.; Cinza-Sanjurjo, S.; Portela-Romero, M. Reinfection by the Omicron variant in patients previously infected with the Delta variant of the SARS-CoV-2 coronavirus: An increasingly frequent reality in Primary Care. Semergen 2022, 48, e35–e36. [Google Scholar] [CrossRef]
- Hu, R.; Jiang, Z.; Gao, H.; Huang, D.; Jiang, D.; Chen, F.; Li, J. Recurrent Positive Reverse Transcriptase-Polymerase Chain Reaction Results for Coronavirus Disease 2019 in Patients Discharged from a Hospital in China. JAMA Netw. Open 2020, 3, e2010475. [Google Scholar] [CrossRef] [PubMed]
- Quattrocchi, A.; Tsioutis, C.; Demetriou, A.; Kyprianou, T.; Athanasiadou, M.; Silvestros, V.; Mamais, I.; Demetriou, C.A.; Theophanous, F.; Soteriou, S.; et al. Effect of Vaccination on SARS-CoV-2 Reinfection Risk: A Case-Control Study in the Republic of Cyprus. Public Health 2022, 204, 84–86. [Google Scholar] [CrossRef] [PubMed]
- Cavanaugh, A.M.; Spicer, K.B.; Thoroughman, D.; Glick, C.; Winter, K. Reduced Risk of Reinfection with SARS-CoV-2 After COVID-19 Vaccination—Kentucky, May-June 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1081–1083. [Google Scholar] [CrossRef]
- Medić, S.; Anastassopoulou, C.; Lozanov-Crvenković, Z.; Vuković, V.; Dragnić, N.; Petrović, V.; Ristić, M.; Pustahija, T.; Gojković, Z.; Tsakris, A.; et al. Risk and Severity of SARS-CoV-2 Reinfections during 2020-2022 in Vojvodina, Serbia: A Population-Level Observational Study. Lancet Reg. Health Eur. 2022, 20, 100453. [Google Scholar] [CrossRef]
- Pilz, S.; Chakeri, A.; Ioannidis, J.P.; Richter, L.; Theiler-Schwetz, V.; Trummer, C.; Krause, R.; Allerberger, F. SARS-CoV-2 Re-Infection Risk in Austria. Eur. J. Clin. Investig. 2021, 51, e13520. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, L.A.; de Góis Filho, P.G.; Silva, A.M.F.; Santos, J.V.G.; Santos, D.S.; Aquino, M.M.; de Jesus, R.M.; Almeida, M.L.D.; da Silva, J.S.; Altmann, D.M.; et al. Recurrent COVID-19 Including Evidence of Reinfection and Enhanced Severity in Thirty Brazilian Healthcare Workers. J. Infect. 2021, 82, 399–406. [Google Scholar] [CrossRef]
- Havervall, S.; Ng, H.; Jernbom Falk, A.; Greilert-Norin, N.; Månberg, A.; Marking, U.; Laurén, I.; Gabrielsson, L.; Salomonsson, A.-C.; Aguilera, K.; et al. Robust Humoral and Cellular Immune Responses and Low Risk for Reinfection at Least 8 Months Following Asymptomatic to Mild COVID-19. J. Intern. Med. 2022, 291, 72–80. [Google Scholar] [CrossRef]
- Nisha, B.; Dakshinamoorthy, K.; Padmanaban, P.; Jain, T.; Neelavarnan, M. Infection, Reinfection, and Postvaccination Incidence of SARS-CoV-2 and Associated Risks in Healthcare Workers in Tamil Nadu: A Retrospective Cohort Study. J. Fam. Community Med. 2022, 29, 49–55. [Google Scholar] [CrossRef]
- Levin-Rector, A.; Firestein, L.; McGibbon, E.; Sell, J.; Lim, S.; Lee, E.H.; Weiss, D.; Geevarughese, A.; Zucker, J.R.; Greene, S.K. Reduced Odds of Severe Acute Respiratory Syndrome Coronavirus 2 Reinfection After Vaccination Among New York City Adults, July 2021-November 2021. Clin. Infect. Dis. 2023, 76, e469–e476. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.N.; Houhamdi, L.; Hoang, V.T.; Delerce, J.; Delorme, L.; Colson, P.; Brouqui, P.; Fournier, P.-E.; Raoult, D.; Gautret, P. SARS-CoV-2 Reinfection and COVID-19 Severity. Emerg. Microbes Infect. 2022, 11, 894–901. [Google Scholar] [CrossRef] [PubMed]
- Mensah, A.A.; Campbell, H.; Stowe, J.; Seghezzo, G.; Simmons, R.; Lacy, J.; Bukasa, A.; O’Boyle, S.; Ramsay, M.E.; Brown, K.; et al. Risk of SARS-CoV-2 Reinfections in Children: A Prospective National Surveillance Study between January, 2020, and July, 2021, in England. Lancet Child Adolesc. Health 2022, 6, 384–392. [Google Scholar] [CrossRef] [PubMed]
- Ochoa-Hein, E.; Leal-Morán, P.E.; Nava-Guzmán, K.A.; Vargas-Fernández, A.T.; Vargas-Fernández, J.F.; Díaz-Rodríguez, F.; Rayas-Bernal, J.A.; González-González, R.; Vázquez-González, P.; Huertas-Jiménez, M.A.; et al. Significant Rise in SARS-CoV-2 Reinfection Rate in Vaccinated Hospital Workers during the Omicron Wave: A Prospective Cohort Study. Rev. Investig. Clin. 2022, 74, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Jang, E.J.; Choe, Y.J.; Yun, G.-W.; Wang, S.; Cho, U.J.; Yi, S.; Lee, S.; Park, Y.-J. Reinfection with SARS-CoV-2 in General Population, South Korea; Nationwide Retrospective Cohort Study. J. Med. Virol. 2022, 94, 5589–5592. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).