Abstract
There are many causes of ST-elevation on electrocardiogram (ECG). ECG changes in the setting of intra-abdominal pathology is a rare and under characterised and includes the “spiked helmet sign”. We report a rare case of the “spiked helmet sign” that presented with ST-elevation in the precordial leads due to post-operative ileus.
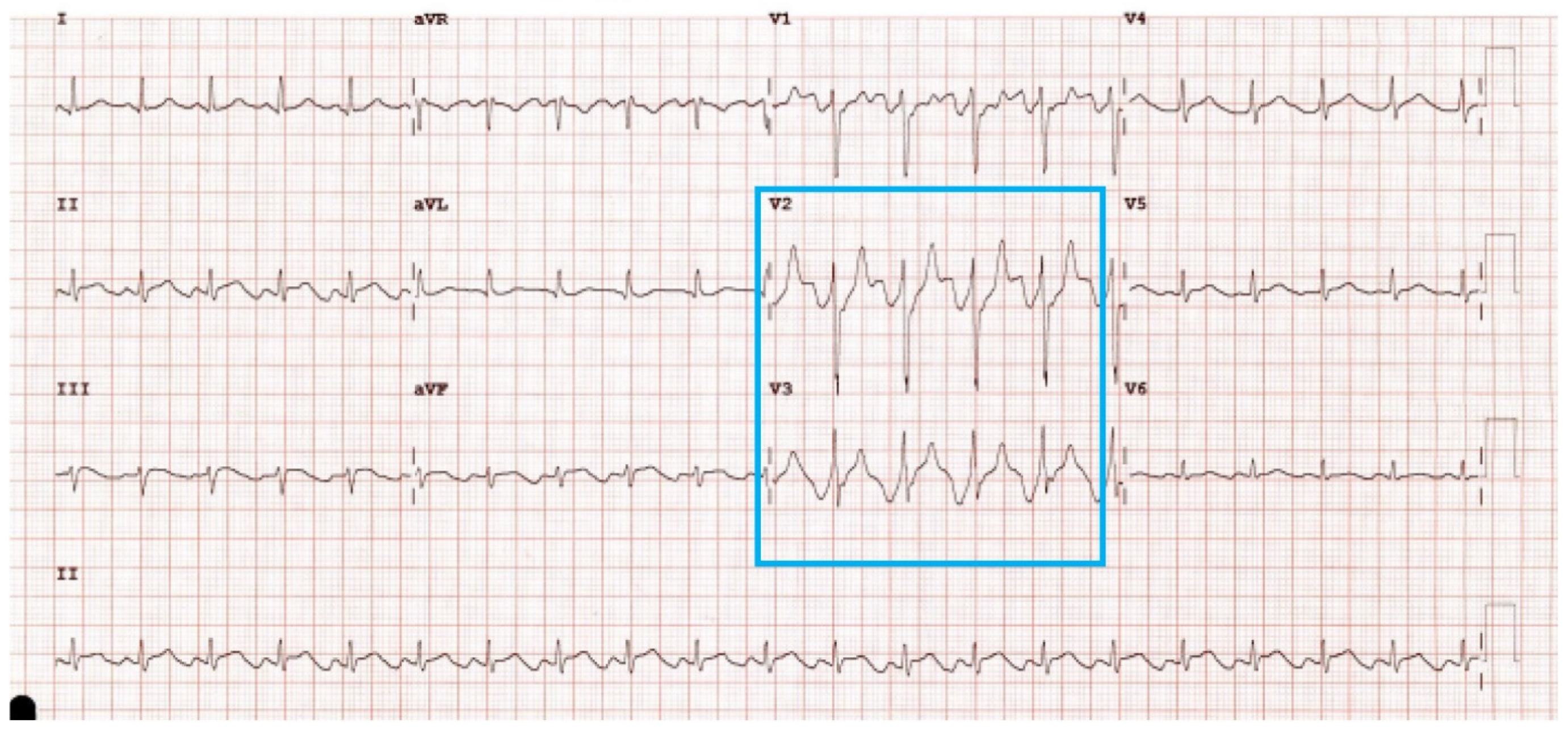
A 64-year-old man who underwent an open left radical nephrectomy for renal cell carcinoma was reviewed on day three post-operatively for dyspnoea (SpO2 85% on room air), tachycardia (120 bpm), nausea, and abdominal distension. He was found to have ST-elevation on bedside ECG (Figure 1). Cardiac investigations, including serum troponins and coronary angiography, were unremarkable.
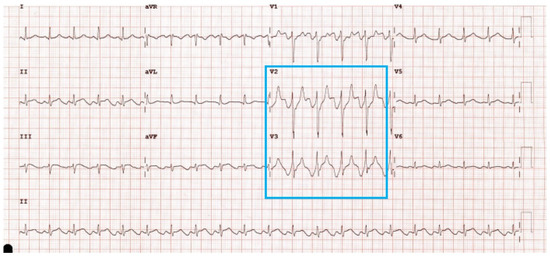
Figure 1.
ECG with ST-elevation, consistent with spiked helmet sign in precordial leads (blue box).
An upward baseline shift starting prior to the onset of the QRS complex prior to ST-elevation was seen on ECG (Figure 1). This dome and spike morphology has led to the naming of this ECG variant the “spiked helmet sign” (SHS), as it has a similar appearance to the German military spiked helmet, the Pickelhaube [1].
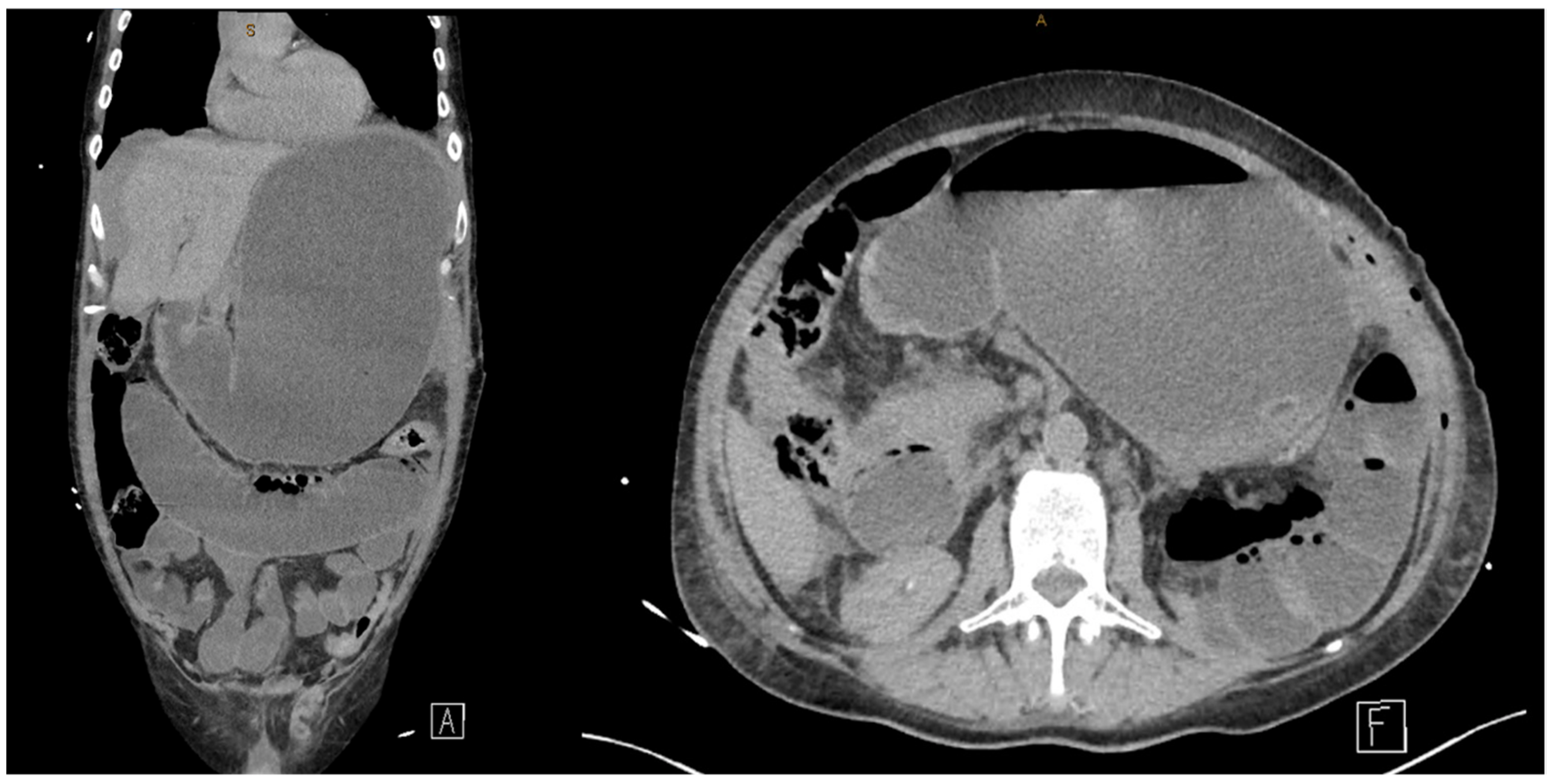
Computed tomography (CT) of the abdomen demonstrated a grossly distended fluid-filled stomach and small bowel, consistent with ileus (Figure 2). Following nasogastric decompression, the patient stabilised, and the ECG changes normalized (Figure 3).
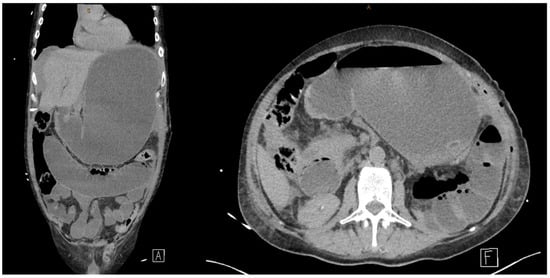
Figure 2.
Sagittal and axial views of distended stomach and small bowel on CT, consistent with ileus.
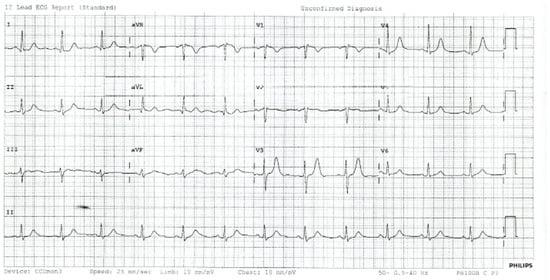
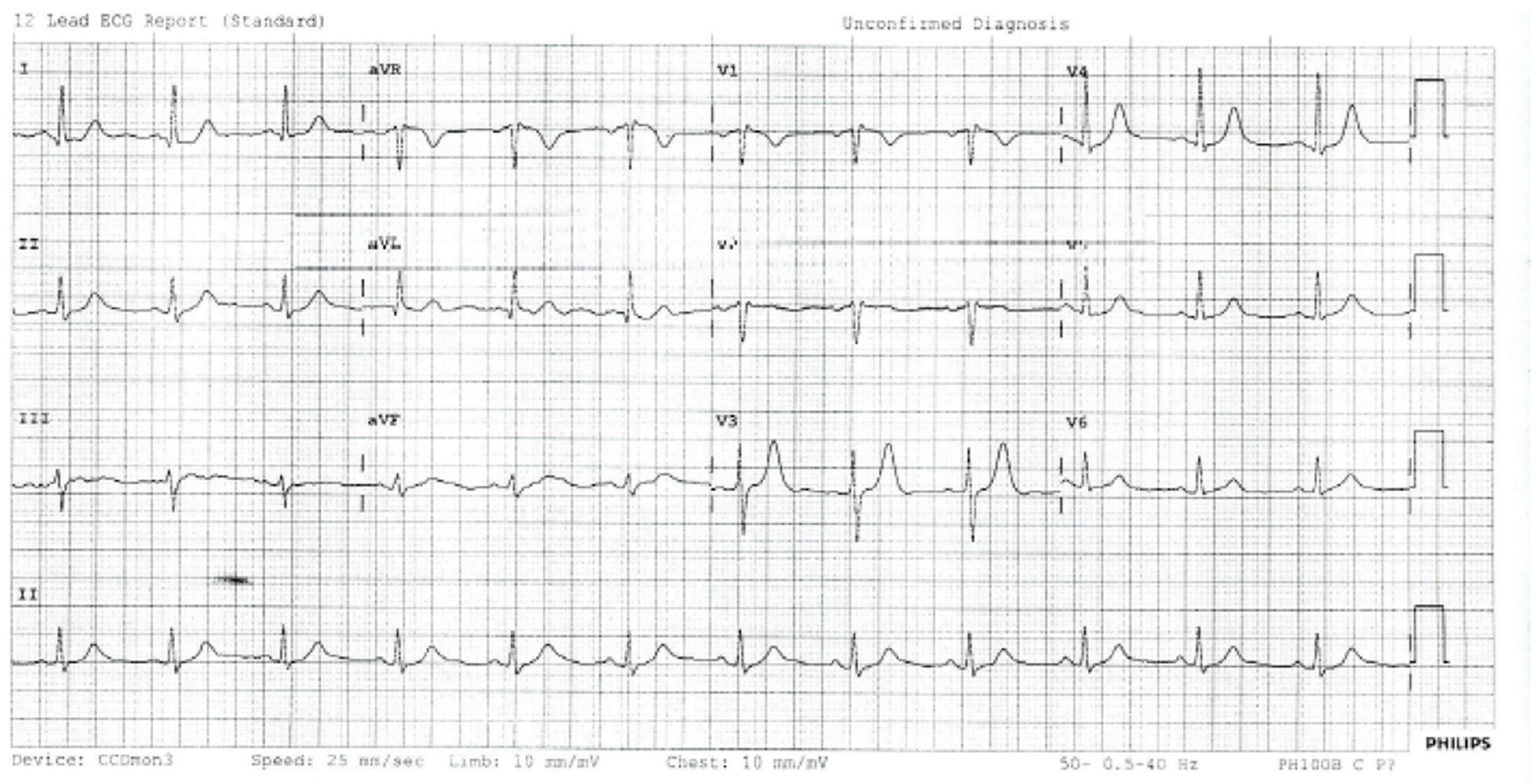
Figure 3.
Resolution of ECG findings after treatment of ileus.
SHS is described as a marker of non-cardiac critical disease [1], with intra-abdominal and intra-thoracic pathology with ST changes found in inferior and precordial ECG, respectively [2,3,4,5,6,7,8,9]. This example shows precordial SHS with an intra-abdominal rather than intra-thoracic cause. Gastric distension, ileus, small bowel obstruction, and bowel perforation are all intra-abdominal pathologies that have been linked to SHS [2,3,4,5,6,7]. Intra-thoracic pathologies associated with SHS include pneumothorax and aortic dissection [7,8,9]. Although the mechanism of SHS is not well understood, intra-thoracic or intra-abdominal pressure resulting in pulsatile epidermal stretch [1] and marked prolongation of the QT interval [10] are both postulated mechanisms of SHS. In all reported cases, SHS changes on ECG resolve upon treatment of the underlying pathology [2,3,4,5,6,7,8,9].
Post-operative patients with ST-elevation on ECG must first undergo cardiac investigation to rule out life-threatening STEMI. Ileus is a common post-operative complication following abdominal surgery and SHS due to ileus demonstrates the importance of considering wide differential diagnoses for ST-elevation in the post-operative setting.
Author Contributions
Writing—original draft preparation, J.W.; writing—review and editing, J.M.; resources, J.M.; supervision, R.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical approval was not required since anonymity is assured in this study and there are no risks associated.
Informed Consent Statement
Informed consent has been obtained to have this case published from the patient.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Littmann, L.; Monroe, M.H. The “spiked helmet” sign: A new electrocardiographic marker of critical illness and high risk of death. Mayo Clin. Proc. 2011, 86, 1245–1246. [Google Scholar] [CrossRef] [PubMed]
- De Bernardi, C.; Halasz, G.; Cattaneo, M. Spiked Helmet Electrocardiographic Sign in a Patient with a Diagnosis of Thoracoabdominal Aortic Dissection. JACC Case Rep. 2020, 2, 2353–2357. [Google Scholar] [CrossRef] [PubMed]
- Salvador-Casabón, J.; Escota-Villanueva, J.; Casanova-Esteban, P.; Ortiz-Giménez, R.; Cantero-Lozano, D.; Pelegrín-Diaz, J. Cardiac extrinsic compression due to abdominal distension as a cause of electrocardiographic abnormality in a critically ill patient. J. Mol. Clin. Med. 2020, 3, 87. [Google Scholar] [CrossRef]
- Cisewski, D.H.; Madias, J.E.; Wong, L. Utilization of the Electrocardiographic “Spiked Helmet” Sign in the Diagnosis of Intra-Abdominal Pathology Within the Emergency Setting. J. Emerg. Med. 2019, 57, 390–394. [Google Scholar] [CrossRef] [PubMed]
- Herath, H.M.; Thushara Matthias, A.; Keragala, B.S.; Udeshika, W.A.; Kulatunga, A. Gastric dilatation and intestinal obstruction mimicking acute coronary syndrome with dynamic electrocardiographic changes. BMC Cardiovasc. Disord. 2016, 16, 245. [Google Scholar] [CrossRef] [PubMed]
- Reddy, M.J.R.; Johnson, B.; Garg, J. Spiked Helmet Sign. Am. J. Med. 2021, 134, 60–62. [Google Scholar] [CrossRef] [PubMed]
- Tomcsanyi, J.; Fresz, T.; Proctor, P.; Littmann, L. Emergence and resolution of the electrocardiographic spiked helmet sign in acute noncardiac conditions. Am. J. Emerg. Med. 2015, 33, 127.e5–127.e7. [Google Scholar] [CrossRef] [PubMed]
- Littmann, L.; Proctor, P. Real time recognition of the electrocardiographic “spiked helmet” sign in a critically ill patient with pneumothorax. Int. J. Cardiol. 2014, 173, e51–e52. [Google Scholar] [CrossRef] [PubMed]
- Tomcsanyi, J.; Fresz, T.; Bozsik, B. ST elevation anterior “spiked helmet” sign. Mayo Clin. Proc. 2012, 87, 309, author reply. [Google Scholar] [CrossRef] [PubMed]
- Laundon, R.K.; Littmann, L. Spiked helmet pattern ST elevation in subarachnoid hemorrhage. J. Electrocardiol. 2019, 52, 96–98. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).