“Harms” Associated with Breast Cancer Screening and Reliability of Frozen Section in Older Women: In the Case of an 80 Year Old Woman
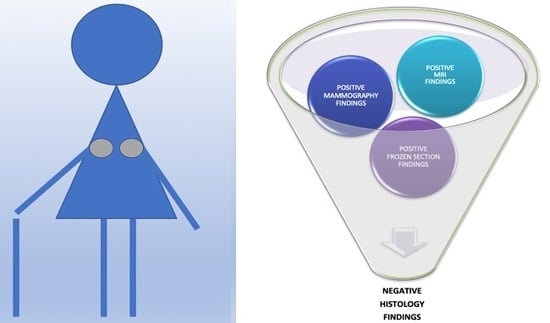
Abstract
1. Introduction
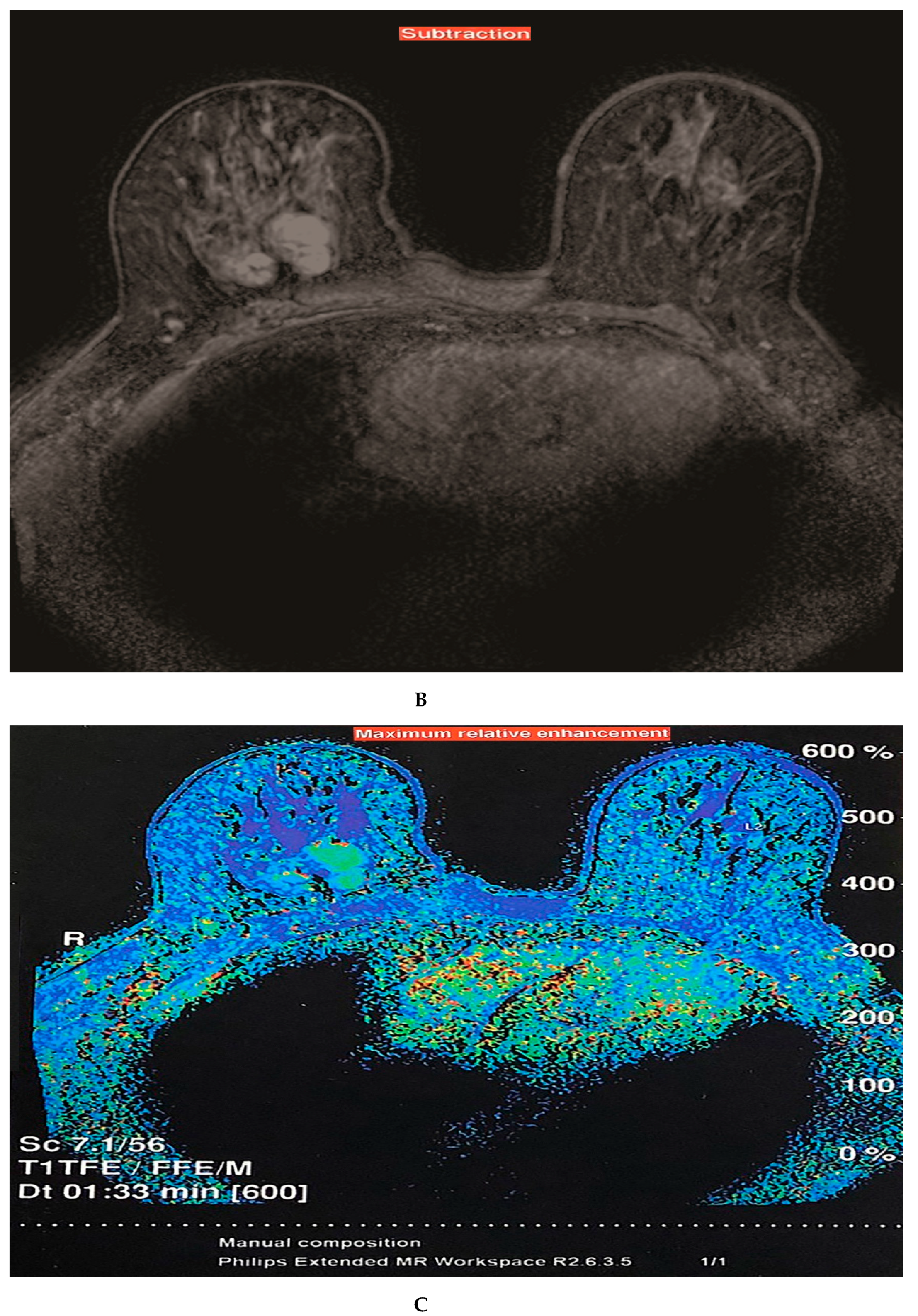
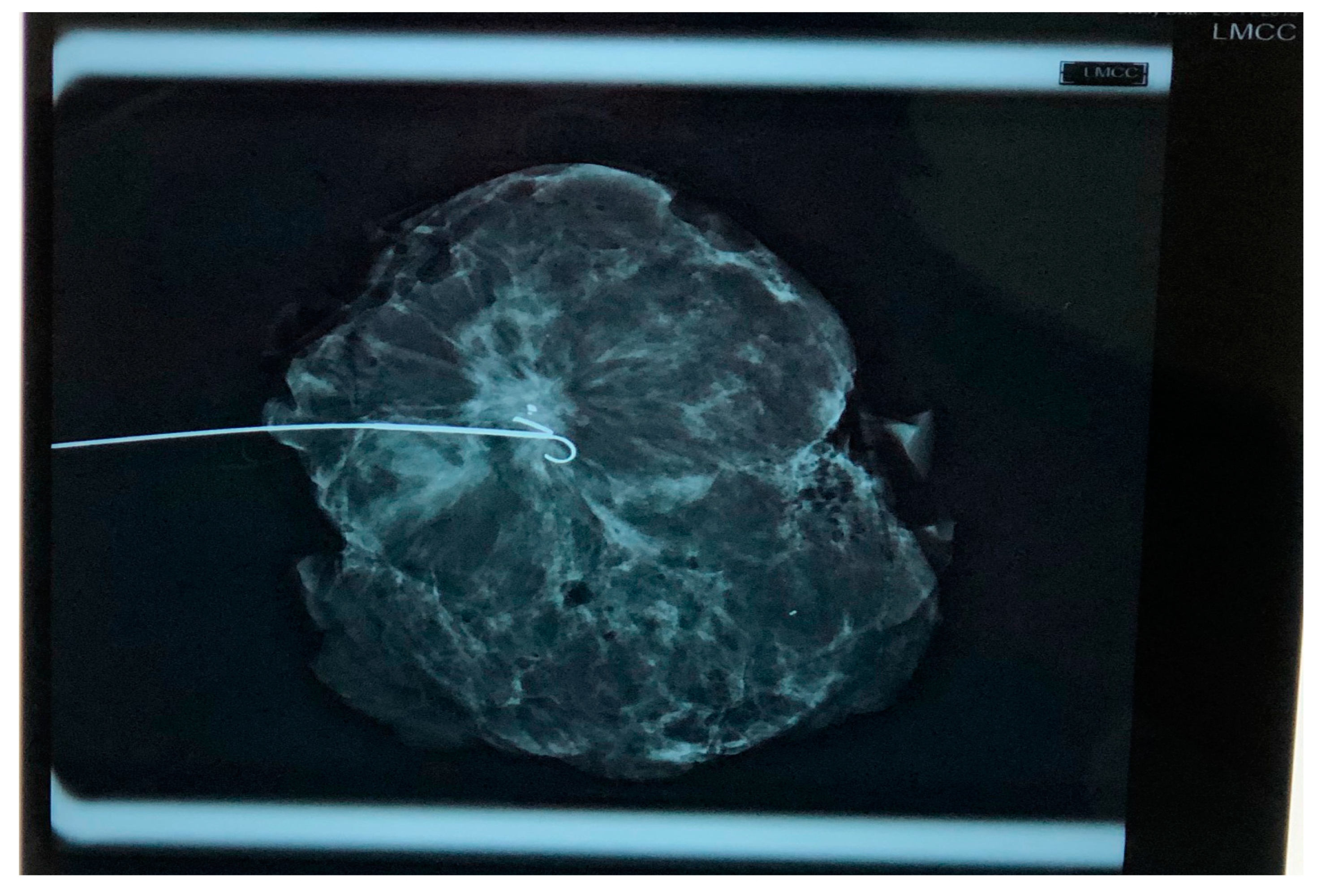
2. Case Presentation Section
Ethics Approval, Statement of Compliance and Clinical Trial Transparency
3. Discussion
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Collins, L.C.; Laronga, C.; Wong, J.S. Breast Ductal Carcinoma in Situ: Epidemiology, Clinical Manifestations, and Diagnosis. Available online: https://www.uptodate.com/contents/breast-ductal-carcinoma-in-situ-epidemiology-clinical-manifestations-and-diagnosis (accessed on 12 March 2020).
- Iatrakis, G. Ductal carcinoma in situ. In Gynecologic Oncology; Desmos Digital Editions; N. Papadopoulos: Athens, Greece, 2018; p. 730. [Google Scholar]
- Alsolami, F.J.; Azzeh, F.S.; Ghafouri, K.J.; Ghaith, M.M.; Almaimani, R.A.; Almasmoum, H.A.; Abdulal, R.H.; Abdulaal, W.H.; Jazar, A.S.; Tashtoush, S.H. Determinants of Breast Cancer in Saudi Women from Makkah Region: A Case-Control Study (Breast Cancer Risk Factors among Saudi Women). BMC Public Health 2019, 19, 1554. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.Y. Factors That Modify Breast Cancer Risk in Women. Available online: https://www.uptodate.com/contents/factors-that-modify-breast-cancer-risk-in-women (accessed on 12 March 2020).
- Collins, L.C.; Laronga, C.; Wong, J.S. Ductal Carcinoma in Situ: Treatment and Prognosis. Available online: https://www.uptodate.com/contents/ductal-carcinoma-in-situ-treatment-and-prognosis (accessed on 9 March 2020).
- Ee, C.; Cave, A.E.; Naidoo, D.; Bilinski, K.; Boyages, J. Weight before and after a Diagnosis of Breast Cancer or Ductal Carcinoma in Situ: A National Australian Survey. BMC Cancer 2020, 20, 113. [Google Scholar] [CrossRef] [PubMed]
- Kerlikowske, K.; Barclay, J.; Grady, D.; Sickles, E.A.; Ernster, V. Comparison of Risk Factors for Ductal Carcinoma in Situ and Invasive Breast Cancer. J. Natl. Cancer Inst. 1997, 89, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Iatrakis, G.; Daures, J.P.; Geahchan, N.; Maudelonde, T.; Bothou, A.; Chraibi, C.; Omar, O.; Voiculescu, S.; Antoniou, E.; Youseff, T.; et al. Manosmed University’s Risk Factor Calculator for Female Breast Cancer: Preliminary Data. Rev. Clin. Pharmacol. Pharmacokinet. Int. Ed. 2018, 32, 23–27. [Google Scholar]
- Demb, J.; Abraham, L.; Miglioretti, D.L.; Sprague, B.L.; O’Meara, E.S.; Advani, S.; Henderson, L.M.; Onega, T.; Buist, D.S.M.; Schousboe, J.T.; et al. Screening Mammography Outcomes: Risk of Breast Cancer and Mortality by Comorbidity Score and Age. J. Natl. Cancer Inst. 2019. [Google Scholar] [CrossRef] [PubMed]
- Zervoudis, S.; Iatrakis, G.; Tomara, E.; Bouga, A.; Grammatikakis, I.; Bothou, A.; Stefos, T.; Navrozoglou, I. Tomosynthesis Improves Breast Cancer Detection: Our Experience. Available online: https://www.researchgate.net/publication/270512753_Tomosynthesis_improves_breast_cancer_detection_Our_experience (accessed on 14 March 2020).
- Elmore, J.G. Screening for Breast Cancer: Strategies and Recommendations. Available online: https://www.uptodate.com/contents/screening-for-breast-cancer-strategies-and-recommendations (accessed on 14 March 2020).
- Sanders, M.A.; Roland, L.; Sahoo, S. Clinical Implications of Subcategorizing BI-RADS 4 Breast Lesions Associated with Microcalcification: A Radiology-Pathology Correlation Study. Breast J. 2010, 16, 28–31. [Google Scholar] [CrossRef] [PubMed]
- Isozaki, H.; Yamamoto, Y.; Murakami, S.; Matsumoto, S.; Takama, T. Significance of Microcalcifications on Mammography in the Surgical Treatment of Breast Cancer Patients with a Preoperative Diagnosis of Ductal Carcinoma in Situ by Core Needle Biopsy. Acta Med. Okayama 2019, 73, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Edderdabi, Z.; Benjelloun, A.T.; Benchrifi, Y.; Moutahir, M.; Benhessou, M.; Ennachit, M.; Elkarroumi, M. EP203 Interest and Reliability of Extemporaneous Examination in Breast Cancer. Int. J. Gynecol. Cancer 2019, 29 (Suppl. 4). [Google Scholar] [CrossRef]
- Santana, R.P.; Morais, N.S.; Samary, Y.R.S.; Bezerra, A.L.R.; Takano, D.M. Evaluation of the accuracy of frozen section in different anatomical sites. J. Bras. Patol. Med. Lab. 2018, 54. [Google Scholar] [CrossRef]
- Zervoudis, S.; Iatrakis, G.; Tomara, E.; Bothou, A.; Papadopoulos, G.; Tsakiris, G. Main Controversies in Breast Cancer. World J. Clin. Oncol. 2014, 5, 359–373. [Google Scholar] [CrossRef] [PubMed]
- Houssami, N.; Turner, R.; Macaskill, P.; Turnbull, L.W.; McCready, D.R.; Tuttle, T.M.; Vapiwala, N.; Solin, L.J. An individual person data meta-analysis of preoperative magnetic resonance imaging and breast cancer recurrence. J. Clin. Oncol. 2014, 201432, 392–401. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.Y.; Kuntz, K.M.; Tuttle, T.M.; Jacobs, D.R., Jr.; Kane, R.L.; Virnig, B.A. The association of preoperative breast magnetic resonance imaging and multiple breast surgeries among older women with early stage breast cancer. Breast Cancer Res. Treat. 2013, 138, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Yoon, G.Y.; Choi, W.J.; Kim, H.H.; Cha, J.H.; Shin, H.J.; Chae, E.Y. Surgical Outcomes for Ductal Carcinoma in Situ: Impact of Preoperative MRI. Radiology 2020, 295, 296–303. [Google Scholar] [CrossRef] [PubMed]
- Lago, V.; Maisto, V.; Gimenez-Climent, J.; Vila, J.; Vazquez, C.; Estevan, R. Nipple-Sparing Mastectomy as Treatment for Patients with Ductal Carcinoma in Situ: A 10-Year Follow-up Study. Breast J. 2018, 24, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.Y.; Kim, H.-J.; Lee, J.; Chung, I.-Y.; Kim, J.-S.; Lee, S.-B.; Son, B.H.; Eom, J.-S.; Kim, S.-B.; Gong, G.-Y.; et al. Recurrence Outcomes After Nipple-Sparing Mastectomy and Immediate Breast Reconstruction in Patients with Pure Ductal Carcinoma In Situ. Ann. Surg. Oncol. 2020. [Google Scholar] [CrossRef]
- Sheaffer, W.W.; Gray, R.J.; Wasif, N.; Stucky, C.C.; Cronin, P.A.; Kosiorek, H.E.; Basu, A.; Pizzitola, V.J.; Patel, B.; Giurescu, M.E.; et al. Predictive Factors of Upstaging DCIS to Invasive Carcinoma in BCT vs Mastectomy. Am. J. Surg. 2019, 217, 1025–1029. [Google Scholar] [CrossRef] [PubMed]
- Bastardis-Zakas, K.; Iatrakis, G.; Navrozoglou, I.; Peitsidis, P.; Salakos, N.; Malakassis, P.; Zervoudis, S. Maximizing the Benefits of Screening Mammography for Women 40–49 Years Old. Clin. Exp. Obstet. Gynecol. 2010, 37, 278–282. [Google Scholar] [PubMed]


© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Antoniou, E.; Zervoudis, S.; Vouxinou, A.; Bothou, A.; Markja, A.; Orovou, E.; Tsikouras, P.; Iatrakis, G. “Harms” Associated with Breast Cancer Screening and Reliability of Frozen Section in Older Women: In the Case of an 80 Year Old Woman. Reports 2020, 3, 15. https://doi.org/10.3390/reports3020015
Antoniou E, Zervoudis S, Vouxinou A, Bothou A, Markja A, Orovou E, Tsikouras P, Iatrakis G. “Harms” Associated with Breast Cancer Screening and Reliability of Frozen Section in Older Women: In the Case of an 80 Year Old Woman. Reports. 2020; 3(2):15. https://doi.org/10.3390/reports3020015
Chicago/Turabian StyleAntoniou, Evangelia, Stefanos Zervoudis, Andriani Vouxinou, Anastasia Bothou, Anisa Markja, Eirini Orovou, Panagiotis Tsikouras, and Georgios Iatrakis. 2020. "“Harms” Associated with Breast Cancer Screening and Reliability of Frozen Section in Older Women: In the Case of an 80 Year Old Woman" Reports 3, no. 2: 15. https://doi.org/10.3390/reports3020015
APA StyleAntoniou, E., Zervoudis, S., Vouxinou, A., Bothou, A., Markja, A., Orovou, E., Tsikouras, P., & Iatrakis, G. (2020). “Harms” Associated with Breast Cancer Screening and Reliability of Frozen Section in Older Women: In the Case of an 80 Year Old Woman. Reports, 3(2), 15. https://doi.org/10.3390/reports3020015