Journal Description
Reports — Clinical Practice and Surgical Cases
Reports
— Clinical Practice and Surgical Cases is an international, peer-reviewed, open access journal about the medical cases, images, and videos in human medicine, published quarterly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within ESCI (Web of Science), PubMed, PMC, FSTA, and other databases.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 21.7 days after submission; acceptance to publication is undertaken in 2.6 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: reviewers who provide timely, thorough peer-review reports receive vouchers entitling them to a discount on the APC of their next publication in any MDPI journal, in appreciation of the work done.
Impact Factor:
0.6 (2024)
Latest Articles
Symptomatic Periarticular Fluid Collection After Total Hip Arthroplasty: Septic or Aseptic Complication? A Case Report and Literature Review
Reports 2025, 8(4), 214; https://doi.org/10.3390/reports8040214 - 24 Oct 2025
Abstract
►
Show Figures
Background and Clinical Significance: Adverse reactions to metal debris (ARMD) are a rare but increasingly recognized complication following total hip arthroplasty (THA), with some studies suggesting upwards of 5% of metal-on-metal (MoM) and 3% of metal-on-polyethylene (MoP) prostheses being attributed to this.
[...] Read more.
Background and Clinical Significance: Adverse reactions to metal debris (ARMD) are a rare but increasingly recognized complication following total hip arthroplasty (THA), with some studies suggesting upwards of 5% of metal-on-metal (MoM) and 3% of metal-on-polyethylene (MoP) prostheses being attributed to this. Historically, metallosis due to MoM implant design was the primary cause of ARMD. However, ARMD can also arise in metal-on-polyethylene (MoP) prostheses due to trunnionosis, which involves wear and corrosion at the modular femoral head–neck interface. Clinically, ARMD can resemble periprosthetic joint infection (PJI), complicating both diagnosis and management. Case Presentation: We present the case of a 40-year-old female with a history of systemic degenerative joint disease with bilateral MoP THAs who developed progressive pain and swelling in the upper left thigh, in which the prosthesis was first put in 22 years prior. The patient presented initially in a vascular surgery department for an infected iliopsoas cyst communicating with the hip where she had received surgery 2 years prior. The symptomatology reoccurred, and imaging revealed a large mass near the prosthesis and elevated inflammatory markers. Intraoperatively, a large volume of sero-purulent fluid was encountered, prompting a diagnostic workup for PJI. All cultures returned negative, and histopathology revealed macrophage-dominant infiltration with metallic debris, consistent with ARMD. After infection was definitively excluded, a revision THA was performed with an exchange of all modular components. The patient recovered without complications, and at six months follow-up, she demonstrated stable implant positioning, restored function, and no recurrence of symptoms. Conclusions: This case highlights the diagnostic complexity of PJI in joint arthroplasty and reveals the importance of a protocol-driven approach to exclude it prior to surgical revision. As the incidence of trunnion-related failure becomes more recognized in the literature, clinicians must consider ARMD in the differential diagnosis of late THA complications. Appropriate diagnosis is essential for guiding treatment and avoiding unnecessary complications, morbidity, and treatment related side-effects.
Full article
Open AccessCase Report
Metabolism-Guided LATTICE Radiotherapy in an Elderly Patient with Locally Advanced Head and Neck Cancer Treated with Curative Aim: A Case Report
by
Giuseppe Iati’, Silvana Parisi, Giacomo Ferrantelli and Stefano Pergolizzi
Reports 2025, 8(4), 213; https://doi.org/10.3390/reports8040213 - 23 Oct 2025
Abstract
Background and clinical Significance: The management of head and neck squamous cell carcinoma in elderly patients is a clinical scenario that is currently under debate. Case Presentation: Patients over 65 years old are particularly vulnerable, and the administration of curative oncological
[...] Read more.
Background and clinical Significance: The management of head and neck squamous cell carcinoma in elderly patients is a clinical scenario that is currently under debate. Case Presentation: Patients over 65 years old are particularly vulnerable, and the administration of curative oncological care is challenging. Furthermore, such treatment has the potential to be extremely toxic. Spatially fractionated radiation therapy (SFRT) is a radiotherapy modality that offers a promising approach for treating tumors. This method involves the delivery of a spatially modulated dose, resulting in highly non-uniform dose distributions. This leads to the generation of peaks and valleys of doses within a target volume. In this case study, a patient with an ulcerating lesion on the right cheek was treated with a two-phase radiotherapy regimen. The purpose of the first procedure was to stimulate the immunogenicity of the tumor microenvironment. In the second part of the procedure, standard fractionated irradiation was delivered with curative aim. Conclusions: The clinical response indicates that this combination of high-dose “localized” and low-dose irradiation can produce immunological effects with an acceptable toxicity profile.
Full article
(This article belongs to the Section Oncology)
►▼
Show Figures

Figure 1
Open AccessCase Report
Partial Androgen Insensitivity Syndrome and Congenital Adrenal Hyperplasia—A Case Report of the Coexistence of Two Rare Diseases in One Patient
by
Mariola Krzyścin, Agnieszka Brodowska, Gabriela Furtak, Dominika Pietrzyk, Katarzyna Zając, Bartosz Oder, Adam Przepiera and Elżbieta Sowińska-Przepiera
Reports 2025, 8(4), 212; https://doi.org/10.3390/reports8040212 - 23 Oct 2025
Abstract
►▼
Show Figures
Background and Clinical Significance: In a single phenotypically female patient, we describe the rare co-occurrence of partial androgen insensitivity syndrome (PAIS) and congenital adrenal hyperplasia (CAH). Partial androgen insensitivity syndrome (PAIS) is one of disorder of sex development (DSD) with a 46
[...] Read more.
Background and Clinical Significance: In a single phenotypically female patient, we describe the rare co-occurrence of partial androgen insensitivity syndrome (PAIS) and congenital adrenal hyperplasia (CAH). Partial androgen insensitivity syndrome (PAIS) is one of disorder of sex development (DSD) with a 46 XY karyotype. Congenital adrenal hyperplasia (CAH) is a genetic defect in adrenal steroidogenesis. Case presentation: We present the case of a 26-year-old female patient who was observed to have abnormally formed external genitourinary organs. She was diagnosed at the neonatal period. Tests performed showed a 46 XY karyotype, an absence of sex chromatin with a weakly positive DNA test for the SRY gene, an absence of uterine primordium with the presence of male gonads in the perineal skin folds, and a urethral outlet at the base of an undeveloped genital process. The daily urinary steroid excretion profile was normal. The patient was diagnosed with partial androgen insensitivity syndrome (PAIS). As a 4-year-old child, she underwent a bilateral gonadectomy due to possible further virilization and also the risk of testicular malignancy. Despite treatment, progressive androgenization was observed, the cause of which turned out to be congenital adrenal hyperplasia (CAH) in the course of P450 oxidoreductase (POR) disorder. Conclusions: In this article, we highlight the exceptional rarity of the co-occurrence of PAIS and CAH, underscoring the need for a multidisciplinary and individualized approach in the absence of clear guidelines regarding surgical timing and gender identity. Careful clinical evaluation and ongoing observation are essential for accurate diagnosis and optimal patient care.
Full article

Figure 1
Open AccessArticle
Anatomical Validation of a Selective Anesthetic Block Test to Differentiate Morton’s Neuroma from Mechanical Metatarsalgia
by
Gabriel Camuñas-Nieves, Hector Pérez-Sánchez, Alejandro Fernández-Gibello, Simone Moroni, Felice Galluccio, Mario Fajardo-Pérez, Laura Pérez-Palma and Alfonso Martínez-Nova
Reports 2025, 8(4), 211; https://doi.org/10.3390/reports8040211 - 21 Oct 2025
Abstract
►▼
Show Figures
Background and Objectives: The anesthetic nerve block test is a surgical technique that can assist in the differential diagnosis of forefoot pain. The MTP joint, enclosed by its capsule, may act as a sealed cavity with predictable contrast dispersion, whereas the IM space,
[...] Read more.
Background and Objectives: The anesthetic nerve block test is a surgical technique that can assist in the differential diagnosis of forefoot pain. The MTP joint, enclosed by its capsule, may act as a sealed cavity with predictable contrast dispersion, whereas the IM space, lacking clear boundaries and containing bursae and the plantar digital nerve, favors diffuse spread. Due to the high rate of false positives in suspected cases of Morton’s neuroma with the anesthetic block current procedure in the intermetatarsal space, the aim of this study was to propose an alternative to the current procedure. Material and Methods: Six fresh cadaveric feet were used. Under ultrasound guidance, the 2nd–4th MTP joints received stepwise intra-articular injections of radiopaque contrast. The third common digital nerve was injected within the third intermetatarsal space. Standard radiographs were obtained to assess distribution and proximal spread. Results: A volume of 0.3 mL was sufficient to fully reach the intra-articular cavity and potentially induce effective localized anesthesia. When the third common digital plantar nerve was injected in an anatomically healthy region, the contrast medium showed a proximal diffusion pattern extending up to the mid-diaphyseal level of the third and fourth metatarsal bones. On radiographs, the intra-articular infiltration lines appear sharply demarcated, supporting the interpretation of the metatarsophalangeal joint as a sealed compartment. Conclusions: Low intra-articular anesthetic volumes may yield targeted effects, while Morton’s neuroma injections spread proximally, risking loss of diagnostic specificity; this technique may improve decision-making accuracy and reduce failures.
Full article

Figure 1
Open AccessCase Report
A Rare Case of First-Time Seizure Induced by Cerebral Venous Sinus Thrombosis Following the Use of Tranexamic Acid for Menorrhagia
by
Jennifer Bandt, Emmanuel O. Oisakede and Natalie Walker
Reports 2025, 8(4), 210; https://doi.org/10.3390/reports8040210 - 20 Oct 2025
Abstract
Background and clinical significance: Tranexamic acid (TXA) is commonly used for menorrhagia. Common side effects include diarrhoea, nausea, and vomiting. However, more serious and rare side effects, including embolism, thrombosis, and seizures, are less commonly considered. Case presentation: We report the case of
[...] Read more.
Background and clinical significance: Tranexamic acid (TXA) is commonly used for menorrhagia. Common side effects include diarrhoea, nausea, and vomiting. However, more serious and rare side effects, including embolism, thrombosis, and seizures, are less commonly considered. Case presentation: We report the case of a 39-year-old woman of Asian origin who presented after a first-time seizure while driving, following starting tranexamic acid for menorrhagia seven days prior. She complained of a headache, nausea, neck stiffness, floaters, and blurred vision. Her lactate was elevated on presentation. On examination there were no neurologic abnormalities. A computed tomography (CT) head scan showed acute haemorrhagic foci along the left temporal lobe. This prompted a CT venography, which showed filling defects in the left transverse and sigmoid sinuses, in keeping with cerebral venous sinus thrombosis. MRI of the head further showed a blooming artefact, indicating secondary thrombosis of the lateral tentorial sinus on the left side extending into the vein of Labbe. Following the diagnosis of cerebral venous sinus thrombosis, the patient was started on regular levetiracetam as well as a therapeutic dose of low molecular weight heparin. Since the initial episode, she has been seizure-free for over three months now. Conclusions: This case highlights the importance of considering less common side effects of tranexamic acid in patients who are taking TXA and are presenting with first-time seizures and headaches. These patients should be monitored for embolic-related intracranial events. A careful diagnostic approach, including cerebrovascular imaging, is essential for an accurate diagnosis and effective treatment.
Full article
(This article belongs to the Section Neurology)
►▼
Show Figures
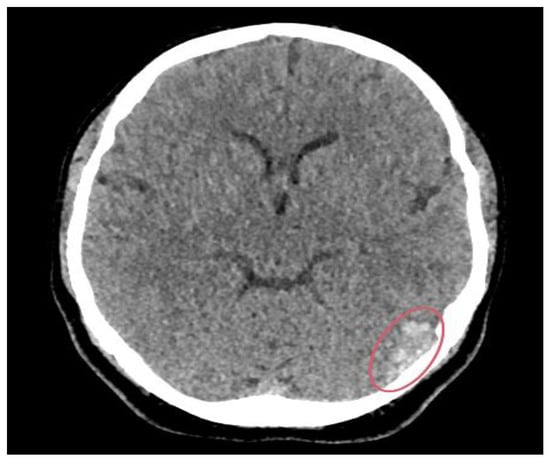
Figure 1
Open AccessCase Report
Pathogenic Glomulin Gene Variant in a Patient with Idiopathic Pulmonary Arterial Hypertension: A Novel Association Case Report
by
Ilias E. Dimeas, George E. Dimeas, George E. Zakynthinos, Cormac McCarthy, Zoe Daniil and Georgia Xiromerisiou
Reports 2025, 8(4), 209; https://doi.org/10.3390/reports8040209 - 20 Oct 2025
Abstract
Background and Clinical Significance: Idiopathic pulmonary arterial hypertension is a rare disorder, often linked to genetic predisposition. Canonical pulmonary arterial hypertension genes such as BMPR2, KCNK3, and TBX4 are well described, but novel associations continue to emerge. Glomulin (GLMN) encodes a protein
[...] Read more.
Background and Clinical Significance: Idiopathic pulmonary arterial hypertension is a rare disorder, often linked to genetic predisposition. Canonical pulmonary arterial hypertension genes such as BMPR2, KCNK3, and TBX4 are well described, but novel associations continue to emerge. Glomulin (GLMN) encodes a protein essential for vascular smooth-muscle biology, classically implicated in glomuvenous malformations, yet not previously associated with pulmonary arterial hypertension. Case Presentation: We present a 49-year-old woman with progressive dyspnea, edema, and persistent hypercapnic respiratory failure. Right-heart catheterization confirmed precapillary pulmonary hypertension. Comprehensive evaluation, including ventilation/perfusion scanning, autoimmune panel, polysomnography, and high-resolution computed tomography, excluded secondary causes. Respiratory assessment revealed diaphragmatic weakness and reduced respiratory muscle pressures, consistent with primary myopathy and explaining the unusual hypercapnic profile. Whole-genome sequencing identified a heterozygous pathogenic GLMN nonsense variant, while canonical pulmonary arterial hypertension genes were negative. No cutaneous or mucosal glomuvenous malformations were found. The patient was treated with oxygen therapy, diuretics, non-invasive ventilation, and dual oral pulmonary arterial hypertension therapy (ambrisentan and tadalafil), with stabilization but persistent hypercapnia. Conclusions: To our knowledge, this is the first reported co-occurrence of idiopathic pulmonary arterial hypertension and a pathogenic GLMN variant. While causality cannot be inferred, glomulin’s role in vascular smooth-muscle maturation provides a plausible link to pulmonary vascular remodeling. This case underscores the importance of assessing respiratory muscle function in idiopathic pulmonary arterial hypertension patients with hypercapnia and highlights the potential relevance of extended genetic testing in rare pulmonary vascular disease.
Full article
(This article belongs to the Section Cardiology/Cardiovascular Medicine)
►▼
Show Figures

Figure 1
Open AccessCase Report
Diphtheria-like Pseudomembranous Corynebacterium striatum Chronic Infection of Left Ventricular Assist Device Driveline Bridged to Heart Transplantation with Dalbavancin Treatment
by
Tommaso Lupia, Marco Casarotto, Simone Mornese Pinna, Silvia Corcione, Alessandro Bondi, Massimo Boffini, Mauro Rinaldi and Francesco Giuseppe De Rosa
Reports 2025, 8(4), 208; https://doi.org/10.3390/reports8040208 - 19 Oct 2025
Abstract
►▼
Show Figures
Background and Clinical Significance: Corynebacterium striatum is an emerging multidrug-resistant pathogen increasingly implicated in infections among immunocompromised patients and patients with indwelling medical devices. Case Presentation: We report the probable first case of pseudomembranous inflammation associated with C. striatum infection in
[...] Read more.
Background and Clinical Significance: Corynebacterium striatum is an emerging multidrug-resistant pathogen increasingly implicated in infections among immunocompromised patients and patients with indwelling medical devices. Case Presentation: We report the probable first case of pseudomembranous inflammation associated with C. striatum infection in a 53-year-old male with an implanted left ventricular assist device (LVAD) awaiting heart transplantation. The patient experienced recurrent episodes of C. striatum bacteremia despite multiple courses of targeted antibiotic therapy, including vancomycin, linezolid, tedizolid, teicoplanin, and dalbavancin. During urgent heart transplantation, pseudomembranous tissue surrounding the LVAD driveline was observed, and cultures confirmed C. striatum device infection. Histopathological analysis revealed necrotic elements and Gram-positive organisms consistent with pseudomembranous inflammation. Conclusions: The case describes the diagnosis and treatment of this rare infection, highlighting the pathogenic potential of C. striatum, its role in device-related infections, and the histopathological evidence of pseudomembrane formation.
Full article

Figure 1
Open AccessArticle
Health-Related Quality of Life and Social Outcomes in Adolescents and Young Adult Survivors of Childhood Cancer: A Single-Center Case–Control Study from Crete, Greece
by
Ioannis Kyriakidis, Iordanis Pelagiadis, Nikolaos Katzilakis, Margarita Pesmatzoglou, Maria Stratigaki, Stylianos Megremis and Eftichia Stiakaki
Reports 2025, 8(4), 207; https://doi.org/10.3390/reports8040207 - 17 Oct 2025
Abstract
Background: Recent advances in childhood cancer treatment and increased survival rates have led to a growing number of adolescents and young adults (AYAs) who are survivors of childhood cancer (CCSs). This study aimed to examine health status, health-related quality of life (HRQoL), and
[...] Read more.
Background: Recent advances in childhood cancer treatment and increased survival rates have led to a growing number of adolescents and young adults (AYAs) who are survivors of childhood cancer (CCSs). This study aimed to examine health status, health-related quality of life (HRQoL), and social outcomes in AYA CCSs. Methods: Sixty-two AYAs who were CCSs (treated within the same tertiary Pediatric Hematology–Oncology Department in Crete, Greece) were enrolled in the study. Self-reported HRQoL was assessed using the Short-Form Health Survey (SF-36). Sixty-five never-ill peers constituted the control group. Results: CCSs reach adolescence and young adulthood without significant deviations in HRQoL from their healthy peers. The presence and severity of late effects were significantly correlated with lower scores in physical health. The cancer type seems to play a pivotal role: Langerhans cell histiocytosis survivors displayed significantly lower scores in mental health, and brain tumor survivors scored substantially lower scores in physical functioning. Acute lymphoblastic leukemia survivors reported the highest scores in mental health. Age at diagnosis of neoplasia was negatively correlated with physical functioning. No significant sex differences were identified. Adherence to multiple healthy lifestyle behaviors (regular exercise, abstaining from alcohol consumption and smoking, and using sun protection) and active employment were correlated with significantly higher scores in mental health. Conclusions: Appropriate therapy and regular follow-up after treatment have led to improved clinical and social outcomes, as assessed by CCSs. More efforts are needed to increase awareness of avoiding harmful behaviors that raise the risk of late effects in this specific group.
Full article
Open AccessCase Report
From Technical Pitfall to Clinical Consequences: Leadless Pacing as a Rescue Solution
by
Fulvio Cacciapuoti, Ciro Mauro, Flavia Casolaro, Antonio Torsi, Salvatore Crispo and Mario Volpicelli
Reports 2025, 8(4), 206; https://doi.org/10.3390/reports8040206 - 17 Oct 2025
Abstract
Background and Clinical Significance: Early lead failure after dual-chamber pacemaker implantation is rare but clinically significant, particularly when associated with thromboembolic complications. Technical pitfalls at the time of implantation, such as suture fixation without protective sleeves, may be predisposed to premature lead damage
[...] Read more.
Background and Clinical Significance: Early lead failure after dual-chamber pacemaker implantation is rare but clinically significant, particularly when associated with thromboembolic complications. Technical pitfalls at the time of implantation, such as suture fixation without protective sleeves, may be predisposed to premature lead damage and abrupt device malfunction. This case highlights the role of device interrogation in diagnosing arrhythmia-related stroke, the challenges of reimplantation in the setting of venous occlusion and anticoagulation, and the value of leadless pacing as a safe rescue strategy. Case Presentation: A 78-year-old man with a history of complete atrioventricular block underwent dual-chamber pacemaker implantation one year earlier. He presented to the emergency department with acute aphasia, right-sided hemiparesis, and facial asymmetry. Stroke was diagnosed, and new-onset atrial fibrillation was documented. Device interrogation revealed an abrupt fall in lead impedance followed by a sharp rise consistent with lead insulation failure and premature battery depletion. Fluoroscopy demonstrated multiple focal narrowings of the leads and complete left subclavian vein occlusion, making conventional transvenous reimplantation unfeasible, while extraction was judged high risk. Right-sided reimplantation was avoided due to hemorrhagic risk under anticoagulation. A leadless pacemaker was implanted successfully in the apico-septal region of the right ventricle via ultrasound-guided femoral access. Hemostasis was secured with a figure-of-8 suture fixed inside a 3-way tap, providing constant compression and preventing hematoma. At two-months follow-up, device function was stable and neurological recovery was favorable (mRS = 2). Conclusions: This case underscores how multiple adverse factors—stroke, arrhythmia detection, early device failure, venous occlusion, and anticoagulation—may converge in a single patient, and demonstrates leadless pacing as a safe and effective rescue strategy in such complex scenarios.
Full article
(This article belongs to the Section Cardiology/Cardiovascular Medicine)
►▼
Show Figures

Figure 1
Open AccessCase Report
Left Atrial Dissection After Mitral and Aortic Valve Replacement: The Importance of Early Diagnosis of a Rare Entity
by
Despoina Sarridou, Sophia Anastasia Mouratoglou, Rafail Ioannidis, Aikaterini Amaniti, Giakoumis Mitos and Eleni Argiriadou
Reports 2025, 8(4), 205; https://doi.org/10.3390/reports8040205 - 17 Oct 2025
Abstract
►▼
Show Figures
Background and Clinical Significance: Left atrial dissection is a rare surgical complication (occurring in 0.16% of cases), which results in the formation of a large cavity between the endocardium and the epicardium. Case Presentation: We report a case of a 78-year-old man
[...] Read more.
Background and Clinical Significance: Left atrial dissection is a rare surgical complication (occurring in 0.16% of cases), which results in the formation of a large cavity between the endocardium and the epicardium. Case Presentation: We report a case of a 78-year-old man who underwent combined aortic and mitral valve replacement. Extensive debridement of the calcified mitral annulus most probably precipitated the formation of a dissection flap detected by transesophageal echocardiography after protamine administration. Profound hypotension and hemodynamic instability were treated with inotropic and vasopressor support and fluid administration without any further surgical intervention. Conclusions: The patient recovered uneventfully under conservative management, highlighting the importance of perioperative echocardiography for prompt diagnosis and tailored intervention.
Full article
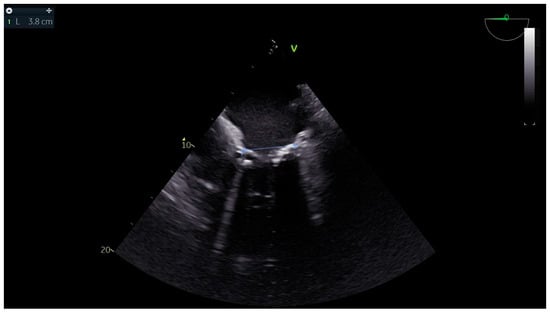
Figure 1
Open AccessCase Report
Arctic Sun Surface Temperature Management Device for Neuroprotection During Pregnancy—A Short Case Report and Review of the Literature
by
Vasileios Vazgiourakis, Konstantinos Mantzarlis, Konstantina Deskata, Asimina Valsamaki, Foteini Bardaka, Dimitra Bagka, George Dimopoulos and Demostenes Makris
Reports 2025, 8(4), 204; https://doi.org/10.3390/reports8040204 - 16 Oct 2025
Abstract
►▼
Show Figures
Targeted temperature management (TTM), particularly the avoidance of hyperpyrexia, is a cornerstone of intensive care, especially in conditions such as cerebral edema and increased intracranial pressure. Management becomes more complex in pregnancy, where maternal neuroprotection must be weighed against fetal safety. Both invasive
[...] Read more.
Targeted temperature management (TTM), particularly the avoidance of hyperpyrexia, is a cornerstone of intensive care, especially in conditions such as cerebral edema and increased intracranial pressure. Management becomes more complex in pregnancy, where maternal neuroprotection must be weighed against fetal safety. Both invasive and noninvasive methods for temperature control have been described, but evidence regarding their safety in pregnancy remains limited. We present the case of a 24-year-old pregnant woman admitted to the ICU with cerebral edema due to subdural empyema. The Arctic Sun surface cooling system was employed for fever control, with continuous maternal and fetal monitoring. The system effectively maintained normothermia without immediate adverse effects on either the mother or the fetus. However, on the third day of its use, the patient experienced a spontaneous preterm delivery of a stillborn fetus. Although a causal link between surface cooling and preterm labor cannot be established from this single case, the event underscores the need for caution and further investigation. This case highlights both the feasibility and the uncertainties of using advanced TTM devices in critically ill pregnant patients. It emphasizes the importance of multidisciplinary monitoring and the urgent need for evidence-based guidelines to balance maternal benefits with fetal safety.
Full article
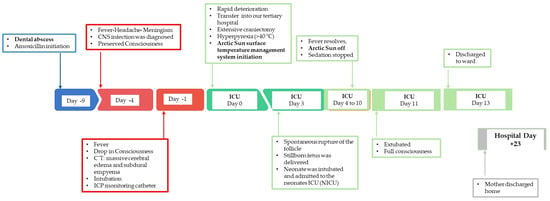
Figure 1
Open AccessCase Report
A Case Report of Fetus Papyraceus in Singleton Pregnancy
by
George Stoyanov, Ivaylo Balabanov, Svetoslava Zhivkova and Hristo Popov
Reports 2025, 8(4), 203; https://doi.org/10.3390/reports8040203 - 13 Oct 2025
Abstract
►▼
Show Figures
Background and Clinical Significance: Fetus papyraceus is a term describing fetal findings associated with miscarriage, wherein the fetus is not expelled, remains in the uterine cavity, and is compressed by neighboring structures, with an inability for fetal resorption due to advanced pregnancy.
[...] Read more.
Background and Clinical Significance: Fetus papyraceus is a term describing fetal findings associated with miscarriage, wherein the fetus is not expelled, remains in the uterine cavity, and is compressed by neighboring structures, with an inability for fetal resorption due to advanced pregnancy. Case Presentation: Herein, we present the case of a 33-year-old primigravida with two previous presentations to our institution due to emotional stress without evidence of physical abuse, the last one being at the 14th week of pregnancy. The latest presentation was with complaints of intermittent lower abdominal pain and an outpatient gynecology consultation describing fetal demise, with fetal parameters corresponding to demise in the 15th to 16th week of gestation. Pregnancy termination was performed with the specimen sent for pathology, revealing fragmented placental parts, which, on section, were firm, with greyish areas and notable calcification, fragments of an umbilical cord appeared normal, and a significantly compressed fetus, which was flattened in the anteroposterior aspect with significant compressive deformation of the limbs—fetus papyraceus characteristics. Histology of the placental fragments revealed fibrin thrombi in large blood vessels, intense fibrosis of the villi with focal fibrin extravasation, and focal necrosis and inflammation, as well as extensive calcium deposits. Conclusions: Fetus papyraceus is a rare complication of intrauterine demise and fetal compression, which can vary in its degree of presenting severity and requires the co-occurrence of specific conditions. The condition is rarely associated with singleton pregnancies.
Full article

Figure 1
Open AccessCase Report
A Conundrum of Colliding Conditions: A Histopathological Case Report of Chiari Type III with Complete Spina Bifida Aperta
by
George Stoyanov, Ivaylo Balabanov, Svetoslava Zhivkova and Hristo Popov
Reports 2025, 8(4), 202; https://doi.org/10.3390/reports8040202 - 12 Oct 2025
Abstract
►▼
Show Figures
Background and Clinical Significance: Spina bifida in the cervical region is closely associated with Chiari malformation, which is an amalgamation of terminology for separate conditions with similar pathophysiological mechanisms and progression from one another. Chiari malformations are associated with varying degrees of
[...] Read more.
Background and Clinical Significance: Spina bifida in the cervical region is closely associated with Chiari malformation, which is an amalgamation of terminology for separate conditions with similar pathophysiological mechanisms and progression from one another. Chiari malformations are associated with varying degrees of dilation of the foramen magnum or lack of fusion of the occipital bone with syringomyelia, herniation of the cerebellum, occipitocele and occipitomyelocele; Case Presentation: A previously healthy 23-year-old primigravida presented to our institution due to fetal demise in the third lunar month, established on routine outpatient maternal consultation. Point-of-care ultrasound revealed an amniotic sac measuring 3 cm in diameter and containing a single fetus, without cardiac function. Due to these, the patient was scheduled for pregnancy termination, during which the cervix was noted to be spontaneously dilated and abrasion accomplished complete evacuation of the amniotic sac, without its rupture. Upon sectioning of the amniotic sac, a fetus, measuring 2.5 cm in length, was noted, with a significant cuffing of the occipital and cervical paraspinal region. Histology revealed fetal structures with an adequate maturation index for its gestational age, but it presented with a pronounced meningoencephalomyelocele in the cervical and thoracic regions, characterized by the complete absence of vertebral arches and spinous processes from the atlanto-occipital to the sacral region; Conclusions: In the present case, not only is a significant and complex form of Chiari type III reported, but the condition is also associated with spina bifida aperta in all spinal regions, leading to meningoencephalomyelocele, incompatible with life.
Full article

Figure 1
Open AccessCase Report
The Impact of Ethnic and Communication Barriers on Fatal Metabolic Emergent Management of Traumatic Injury: A Case Report
by
Yutaka Furuta, Rory J. Tinker, Angela R. Grochowsky and John A. Phillips III
Reports 2025, 8(4), 201; https://doi.org/10.3390/reports8040201 - 10 Oct 2025
Abstract
Background and Clinical Significance: Inherited metabolic disorders can result in fatal metabolic decompensation if not promptly recognized and treated. These conditions are common in Plain communities due to founder effects and the high prevalence of consanguinity. Case Presentation: We present the
[...] Read more.
Background and Clinical Significance: Inherited metabolic disorders can result in fatal metabolic decompensation if not promptly recognized and treated. These conditions are common in Plain communities due to founder effects and the high prevalence of consanguinity. Case Presentation: We present the case of an adult Amish male with maple syrup urine disorder who sustained traumatic injuries and delayed metabolic intervention that contributed to a fatal outcome. Conclusions: This case highlights the critical need for increased awareness among emergency and adult care providers, especially in Plain communities, and emphasizes the importance of early multidisciplinary coordination and preparedness with metabolic resources to ensure timely, life-saving management in adult metabolic emergencies.
Full article
(This article belongs to the Section Critical Care/Emergency Medicine/Pulmonary)
►▼
Show Figures

Figure 1
Open AccessCase Report
Continuous Glucose Monitoring Improves Weight Loss and Hypoglycemic Symptoms in a Non-Diabetic Bariatric Patient 14 Years After RYGB: A Case Report
by
Carolina Pape-Köhler, Christine Stier, Stylianos Kopanos and Joachim Feldkamp
Reports 2025, 8(4), 200; https://doi.org/10.3390/reports8040200 - 8 Oct 2025
Abstract
►▼
Show Figures
Background and Clinical Significance: Roux-en-Y gastric bypass (RYGB) significantly alters glucose metabolism, yet managing glucose variability in patients undergoing bariatric surgery remains challenging. Continuous Glucose Monitoring (CGM) offers real-time insights into glucose fluctuations and may support long-term metabolic management in this population.
[...] Read more.
Background and Clinical Significance: Roux-en-Y gastric bypass (RYGB) significantly alters glucose metabolism, yet managing glucose variability in patients undergoing bariatric surgery remains challenging. Continuous Glucose Monitoring (CGM) offers real-time insights into glucose fluctuations and may support long-term metabolic management in this population. This case highlights the utility of CGM in identifying postprandial glycemic variability and guiding dietary adjustments. Case Presentation: A 45-year-old female, 14 years post-RYGB, presented with symptoms including postprandial fatigue, nocturnal cravings, and unexplained weight gain, despite adherence to nutritional guidelines. Her BMI had decreased from 52 kg/m2 (pre-surgery) to 29 kg/m2. She was provided with a CGM device (FreeStyle Libre 3) by the clinical team and instructed to monitor glucose without modifying her routine initially. Data revealed significant glycemic variability, with peaks up to 220 mg/dL and hypoglycemic dips to 45 mg/dL. Based on this, she adjusted her diet by reducing non-complex carbohydrates and increasing vegetables, proteins, and complex carbohydrates. Within two weeks, her symptoms improved, including better sleep and energy levels, accompanied by a 3 kg weight loss following dietary adjustments informed by CGM feedback. Conclusions: This case suggests how CGM can empower patients having undergone bariatric surgery to manage glucose fluctuations through informed self-management. The patient’s ability to identify and address glucose variability without formal intervention highlights CGM’s potential as a supportive tool in long-term care. While further studies are needed, this case suggests CGM may benefit similar patients experiencing postprandial symptoms or weight regain after bariatric surgery.
Full article

Figure 1
Open AccessCase Report
Clinical Experience Using a Dual-Layer Amniotic Membrane Allograft on a Posterior Upper-Thigh Pressure Ulcer
by
Kirk Mitchell
Reports 2025, 8(4), 199; https://doi.org/10.3390/reports8040199 - 6 Oct 2025
Abstract
►▼
Show Figures
Background and Clinical Significance: The objective of this case study is to report on the clinical outcomes of a hard-to-heal posterior upper-thigh pressure ulcer when managed with a sterile human amniotic membrane tissue allograft. Case Presentation: Retrospective case data of a
[...] Read more.
Background and Clinical Significance: The objective of this case study is to report on the clinical outcomes of a hard-to-heal posterior upper-thigh pressure ulcer when managed with a sterile human amniotic membrane tissue allograft. Case Presentation: Retrospective case data of a patient who received five applications of barreraTM between February 2024 and April 2024 as part of their care regimen for a chronic pressure ulcer was obtained from a single wound care group. Data evaluated consisted of past patient medical history, concomitant medications, previous wound care treatments, wound type, wound size, adjunctive wound therapies and wound outcomes post allograft. The chronic pressure ulcer, measuring at 10.5 cm2 prior to allograft application, achieved complete closure at the last observation post the final, fifth application. Wound size attenuation was seen as early as 1 week post initial allograft application. No adverse events or complications related to barreraTM were observed. Conclusions: Results suggest that the application of dual-layer allografts in the context of chronic ulcers may represent a safe and effective wound management utility.
Full article

Figure 1
Open AccessCase Report
Case Report: Scalpel Sign and Dorsal Arachnoid Cyst—The Importance of an Accurate Diagnosis
by
Matteo Bonetti, Michele Frigerio, Mario Muto, Federico Maffezzoni and Serena Miglio
Reports 2025, 8(4), 198; https://doi.org/10.3390/reports8040198 - 5 Oct 2025
Abstract
Background and Clinical Significance: Thoracic dorsal arachnoid web (DAW) is a rare intradural extramedullary condition characterized by a thin band of arachnoid tissue compressing the dorsal spinal cord. A hallmark imaging feature is the “scalpel sign”, which refers to anterior displacement of
[...] Read more.
Background and Clinical Significance: Thoracic dorsal arachnoid web (DAW) is a rare intradural extramedullary condition characterized by a thin band of arachnoid tissue compressing the dorsal spinal cord. A hallmark imaging feature is the “scalpel sign”, which refers to anterior displacement of the thoracic spinal cord with dorsal cerebrospinal fluid (CSF) accumulation, producing a sagittal profile resembling a surgical scalpel. Although highly specific for DAW, this sign may also appear in other intradural conditions such as idiopathic ventral spinal cord herniation and arachnoid cysts. The clinical presentation is typically progressive and nonspecific, including lower limb weakness, sensory changes, gait disturbances, and, less frequently, sphincter dysfunction. Diagnosis is often delayed due to the subtle nature of the lesion and limited resolution of conventional Magnetic Resonance Imaging (MRI). High-resolution Three-Dimensional Constructive Interference in Steady State (3D-CISS) sequences improve diagnostic accuracy by highlighting indirect signs such as spinal cord deformation and dorsal CSF flow obstruction. Case Presentation: We report the case of a 57-year-old woman presenting with chronic cervico-dorsalgia, bilateral lower limb weakness, paresthesia, and progressive gait instability. Neurological examination revealed spastic paraparesis and hyperreflexia. Conventional MRI was inconclusive. However, sagittal T2-weighted and 3D-CISS sequences demonstrated the scalpel sign at the T4–T5 level, with anterior cord displacement and dorsal subarachnoid space enlargement. Surgical exploration confirmed the presence of a dorsal arachnoid web, which was resected. Postoperative follow-up showed clear improvement in motor function and gait. Conclusions: DAW should be considered in cases of unexplained thoracic myelopathy or cervico-dorsalgia with neurological signs. Early recognition of the scalpel sign using advanced MRI sequences is critical for timely diagnosis and surgical planning, which may lead to significant clinical improvement.
Full article
(This article belongs to the Section Neurology)
►▼
Show Figures

Figure 1
Open AccessCase Report
Highlighting the Importance of Signaling Pathways and Immunohistochemistry Features in HCC: A Case Report and Literature Review
by
Alexandru Madalin Hasan, Ioana Larisa Paul, Simona Cavalu, Ovidiu Laurean Pop, Lorena Paduraru, Ioan Magyar and Mihaela Doina Chirila
Reports 2025, 8(4), 197; https://doi.org/10.3390/reports8040197 - 3 Oct 2025
Abstract
Background and Clinical Significance: In hepatocellular carcinoma (HCC), numerous signaling pathways become aberrantly regulated, resulting in sustained cellular proliferation and enhanced metastatic potential. Tumors that lack PYGO2 may not show the same types of tissue remodeling or regenerative features driven by the Wnt/β-catenin
[...] Read more.
Background and Clinical Significance: In hepatocellular carcinoma (HCC), numerous signaling pathways become aberrantly regulated, resulting in sustained cellular proliferation and enhanced metastatic potential. Tumors that lack PYGO2 may not show the same types of tissue remodeling or regenerative features driven by the Wnt/β-catenin pathway, which could make the tumor behave differently from others that are Wnt-positive. PIK3CA-positive tumors are often associated with worse prognosis due to the aggressive nature of the PI3K/AKT pathway activation. This is linked to higher chances of metastasis, recurrence, and resistance to therapies that do not target this pathway. Case presentation: In this paper we present a rare case of hepatocellular carcinoma with PIK3CA-positive and PYGO2-negative signaling pathways, several key aspects of the tumor’s behavior, prognosis, and treatment options. Although alpha-fetoprotein (AFP) levels were significantly elevated, the CT and MRI examination showed characteristics of malignancy, HCC with secondary hepatic lesions and associated perfusion disturbances. The case particularities and immunohistochemistry features are highlighted in the context of literature review, the PIK3CA mutation suggesting the activation of the PI3K/AKT/mTOR pathway, a critical signaling pathway involved in cell survival, proliferation, and metabolism. Conclusions: Due to the aggressive nature of PIK3CA mutations, close monitoring and consideration of immunotherapy and targeted treatments are of crucial importance.
Full article
(This article belongs to the Section Oncology)
►▼
Show Figures
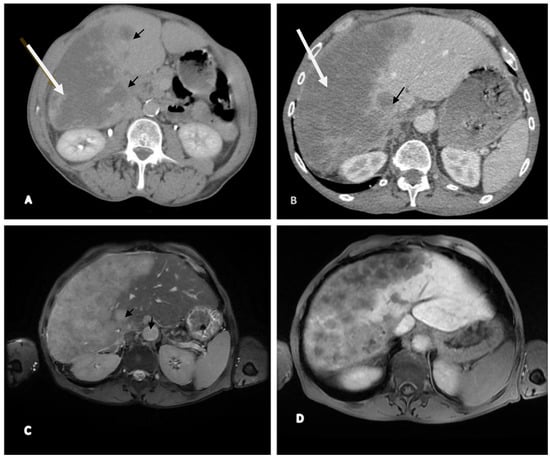
Figure 1
Open AccessCase Report
A Rare Case Presentation of Intraoral Palatal Myoepithelioma
by
Abdullah Saeidi, Albraa Alolayan, Hattan Zaki, Emad Essa, Shadi Alzahrani, Wamiq Fareed and Shadia Elsayed
Reports 2025, 8(4), 196; https://doi.org/10.3390/reports8040196 - 3 Oct 2025
Abstract
►▼
Show Figures
Background and Clinical Significance: Palatal swellings may originate from various pathological disorders. These swellings may include congenital or acquired factors. The posterior hard palate, which contains many minor salivary glands, is a common site for such swellings. Case Presentation: We present a rare
[...] Read more.
Background and Clinical Significance: Palatal swellings may originate from various pathological disorders. These swellings may include congenital or acquired factors. The posterior hard palate, which contains many minor salivary glands, is a common site for such swellings. Case Presentation: We present a rare case of intraoral palatal myoepithelioma in a 45-year-old Egyptian male with a significant history of smoking. Detailed clinical, radiographic, and operative findings are discussed alongside histopathological evaluation, surgical management, and postoperative outcomes. This case highlights the importance of considering myoepithelioma lesions in the differential diagnosis of posterior palatal swelling. Conclusions: Palatal myoepithelioma is a rare but important benign salivary gland tumor that may resemble multiple other intraoral lesions. A complete clinical, radiographic, and histological investigation is required for a definitive diagnosis. Complete surgical excision achieved a favorable outcome. Increased awareness and reporting of this unusual pathology are critical for deepening knowledge and guiding clinical decisions.
Full article

Figure 1
Open AccessCase Report
High-Grade Solid Adenoid Cystic Carcinoma of the Larynx: A Case Report
by
Matteo Aldo Russo, Stefano Patruno, Christian Fiorentino, Pietro Corsa, Teodoro Aragona, Lucia Maria Dimitri, Michele Cassano and Lazzaro Cassano
Reports 2025, 8(4), 195; https://doi.org/10.3390/reports8040195 - 1 Oct 2025
Abstract
►▼
Show Figures
Background and Clinical Significance: Adenoid cystic carcinoma (ACC) is a rare neoplasm of salivary glands, accounting for approximately 2–4% of all ACCs of head and neck malignancies. Adenoid cystic carcinoma (ACC) of the larynx is exceedingly rare, accounting for only 0.07–0.25% of
[...] Read more.
Background and Clinical Significance: Adenoid cystic carcinoma (ACC) is a rare neoplasm of salivary glands, accounting for approximately 2–4% of all ACCs of head and neck malignancies. Adenoid cystic carcinoma (ACC) of the larynx is exceedingly rare, accounting for only 0.07–0.25% of all laryngeal tumors. Within the larynx, ACC may arise in various locations; however, the subglottic region is most commonly affected, representing approximately 64% of cases. ACC typically manifests as a slow-growing tumor with a pronounced tendency for perineural invasion and local recurrence. Current treatment strategies primarily involve surgical resection followed by adjuvant radiotherapy. Chemotherapy demonstrates limited efficacy and is generally reserved for advanced, recurrent, or metastatic disease. Given the rarity of this malignancy and the limited number of cases reported in the literature, we aim to contribute to the existing body of knowledge by presenting a clinical case of laryngeal ACC. Case Presentation: A 77-year-old male with a significant smoking history (more than 20 cigarettes per day for over 40 years) presented to our department in October 2023 with persistent dysphonia lasting several months. Endoscopic evaluation of the upper aerodigestive tract revealed an extensive neoplastic lesion involving the larynx. Contrast-enhanced computed tomography (CT) confirmed the presence and extent of the lesion. The patient subsequently underwent surgical resection and was referred for adjuvant postoperative radiotherapy. Unfortunately, the patient died of a myocardial infarction a few days before radiotherapy could be initiated. Conclusions: Due to the rarity of laryngeal adenoid cystic carcinoma, further studies are necessary to define optimal management strategies. Sharing clinical experiences and outcomes is essential, as there is currently no universally accepted treatment consensus for this uncommon malignancy. At the same time, our aim is to highlight the importance of histological subtype and perineural invasion which have to be considered as important prognostic factors when dealing with ACC.
Full article
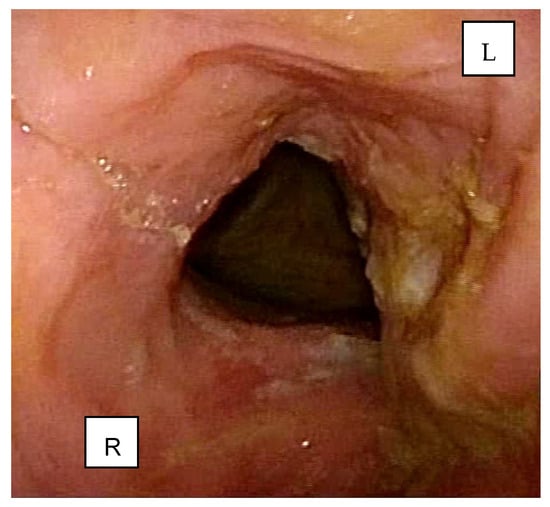
Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Biomedicines, JoF, Pharmaceuticals, Pharmaceutics, Reports, Molecules
Natural Products to Fight Fungal Infections
Topic Editors: Célia Fortuna Rodrigues, Shasank Sekhar SwainDeadline: 30 December 2025
Topic in
Biomedicines, Diseases, JCM, JPM, Uro, Reports
Clinical, Translational, and Basic Research and Novel Therapy on Functional Bladder Diseases and Lower Urinary Tract Dysfunctions
Topic Editors: Hann-Chorng Kuo, Yao-Chi Chuang, Chun-Hou LiaoDeadline: 31 December 2026

Special Issues
Special Issue in
Reports
Oral Disorders in the Pediatric Population
Guest Editors: Athanasios K. Poulopoulos, Vasileios ZisisDeadline: 28 November 2025
Special Issue in
Reports
Artificial Intelligence in Clinical Medicine—Transforming Patient Care Through Innovation
Guest Editors: Ryo Ozuru, Yuji Oyamada, Toshio HattoriDeadline: 31 January 2026
Topical Collections
Topical Collection in
Reports
Health Threats of Climate Change
Collection Editors: Toshio Hattori, Yujiro Nakayama, Hiromu Ito, Kenzo Takahashi, Ayako Sumi, Takatoshi Kasai, Ichiro Onoyama, Shigeru Morinobu
Topical Collection in
Reports
Cardiovascular Disease and Sleep Disordered Breathing—Case Report
Collection Editor: Takatoshi Kasai








