Abstract
Dementia, the most severe expression of cognitive impairment, is among the main causes of disability in older adults and currently affects over 55 million individuals. Dementia prevention is a global public health priority, and recent studies have shown that dementia risk can be reduced through non-pharmacological interventions targeting different lifestyle areas. The FINnish GERiatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER) has shown a positive effect on cognition in older adults at risk of dementia through a 2-year multidomain intervention targeting lifestyle and vascular risk factors. The LETHE project builds on these findings and will provide a digital-enabled FINGER intervention model for delaying or preventing the onset of cognitive decline. An individualised ICT-based multidomain, preventive lifestyle intervention program will be implemented utilising behaviour and intervention data through passive and active data collection. Artificial intelligence and machine learning methods will be used for data-driven risk factor prediction models. An initial model based on large multinational datasets will be validated and integrated into an 18-month trial integrating digital biomarkers to further improve the model. Furthermore, the LETHE project will investigate the concept of federated learning to, on the one hand, protect the privacy of the health and behaviour data and, on the other hand, to provide the opportunity to enhance the data model easily by integrating additional clinical centres.
1. Introduction
Cognitive impairment is common among older adults. Dementia, the most severe expression of cognitive impairment, represents the seventh leading cause of death among all diseases and one of the main causes of disability in older people, currently affecting over 55 million individuals worldwide [1]. As increasing age is the main risk factor for cognitive impairment and dementia, the worldwide aging of populations is driving the exponential growth in the number of affected individuals. Indeed, dementia cases are expected to reach 78 million by 2030 and 130 million in 2050 unless effective preventive and therapeutic interventions become widely available [2]. Dementia has long been considered a non-preventable condition, but a lot of evidence from observational and recent intervention studies has shown the potential for risk reduction and prevention of this disorder and the main underlying diseases, including cerebrovascular disease and Alzheimer´s disease (AD) [1]. The life-course model of prevention summarised by the Lancet Commission on Dementia Prevention, Intervention and Care indicated that twelve modifiable risk factors account for about 40% of all cases of dementia worldwide, which can thus be potentially prevented or delayed [3]. These factors are low schooling, hypertension, hearing impairment, smoking, obesity, depression, physical inactivity, diabetes, low social contact, excessive alcohol consumption, traumatic brain injury, and air pollution [3]. Observational studies from Western countries reported a decreasing trend in the age-specific incidence of dementia, probably related to improvements in education, healthcare, and lifestyle, further supporting the potential benefits of change in risk factor profiles [3]. Europe has been at the forefront of intervention studies, testing innovative preventive approaches for dementia risk reduction and prevention. The Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER, ClinicalTrials.gov Identifier: NCT01041989) is the first large and long-term randomised clinical trial (RCT) that showed a positive effect on cognition after a 2-year multidomain intervention that targeted lifestyle and vascular risk factors simultaneously [4]. The FINGER RCT included two arms: multidomain intervention, which consisted of physical activity, diet, social stimulation, cognitive training, and vascular and metabolic risk factor control, and the control group, which received regular health advice. FINGER was the first RCT to show the feasibility of preventing cognitive decline using a multidomain intervention among older individuals at risk of dementia [4]. Long-term follow-ups with the FINGER study participants are ongoing (5- and 7-year follow-up completed; 11-year follow-up ongoing) to assess the long-term effects of the multidomain intervention on cognition. Other European, large multidomain prevention trials (MAPT: Multidomain Alzheimer Preventive Trial; PreDIVA: Prevention of Dementia by Intensive Vascular Care), despite failing to report beneficial cognitive changes in their respective primary outcomes, reported significant positive effects on cognition in secondary analyses for participants with specific risk profiles [5,6]. Overall, these RCTs have highlighted the need for accurate risk prediction and stratification to optimise the efficacy of multidomain preventive interventions. The recent guidelines from the World Health Organisation (WHO) for reducing the risk of cognitive decline and dementia represent a milestone in the field of dementia prevention and highlight the need to further test and develop the FINGER model to define, on a global scale, effective and feasible preventive strategies [7]. The evidence synthetised in the WHO guidelines indicates that risk reduction for dementia can be achieved at individual and population levels through multidomain interventions tailored to specific risk profiles. In this landscape, the availability of models for accurately predicting dementia risk is pivotal to identify and monitor at-risk groups that can benefit from specific interventions. The development of predictive modelling of the onset and progression of dementia can leverage on large multidimensional data, reflecting nonmodifiable (e.g., age, sex, genetics) and modifiable risk factors (e.g., lifestyle, vascular and metabolic factors), as well as clinical information, such as cognitive status, and biological parameters (e.g., neuroimaging, blood markers). Increasing the availability of information and communication technologies (ICT) has also prompted research on digital biomarkers which can support non-invasive longitudinal monitoring of risk and inform personalised preventive approaches to maximise adherence to and benefits of preventive interventions. Artificial Intelligence (AI) tools can handle large and complex data but have not yet been used to develop predictive modelling of the onset and progression of dementia based on the above-listed data. To this end, the European LETHE project was launched in 2021 to develop a data-driven risk factor prediction model for older individuals at risk of cognitive decline by leveraging observational and intervention studies. The LETHE project capitalises on a multidisciplinary consortium, which includes the research teams who developed the FINGER model, clinical teams, and partners with strong technical expertise. In the last decade, several scientific research profects and deployments of proof-of-concept addressing technologies for smart and healthy living have been developed by partners of the LETHE consortium, significantly contributing to progress in the field of ICT solutions and services for older people.
2. Background
2.1. Ageing, Cognitive Decline, and Dementia
Dementia is usually preceded by mild cognitive impairment (MCI), and even subjective cognitive symptoms have been associated with increased risk of later cognitive decline. Subjective cognitive decline (SCD) is characterised by self-experienced, persistent cognitive decline, which can evolve into the appearance of objective cognitive impairment. In the absence of objective neuropsychological dysfunction, older adults with SCD are increasingly viewed as at-risk for non-normative cognitive decline and potential progression to MCI and AD dementia. MCI might be considered a pre-stage of dementia, characterised by incipient cognitive dysfunction, as documented in neuropsychological tests, and occurring in up to a fifth of people aged older than 65 years [8]. MCI represents a heterogeneous syndrome, and therefore, the prognosis can differ between each individual. Persons with MCI can either progress to dementia, remain in a stable state, or reverse to normal functioning [8]. The annual conversion rate varies between 5 and 15 percent in the existing literature, with higher rates observed in studies carried out in clinical settings. MCI is seen as a great opportunity for an early targeted intervention, thereby delaying or even preventing the conversion to overt dementia. Increasing evidence from epidemiological, clinical, and biomarker studies suggests that the development of neuropathological changes leading to dementing diseases, especially AD, starts many years before clinical symptoms become apparent, thereby indicating that AD starts as a clinically silent disorder. For instance, research in persons with familial autosomal dominant AD has revealed pre-symptomatic changes in multiple markers of disease in blood, cerebrospinal fluid (CSF), and neuroimaging [9,10]. Different biomarkers seem to be a good proxy for incipient neuropathological changes. The accumulation of Amyloid-Beta (Aβ) or neurofibrillary tangles—the major hallmarks of AD—can either be depicted through positron emission tomography (PET)-Imaging or examination of cerebrospinal fluid (CSF) [10]. Magnetic resonance imaging (MRI) gives insights into neurodegenerative processes through structural brain changes, such as cortical thickness or specific atrophy patterns. Ongoing studies are examining the use of blood-based analysis for a cheaper and minimally invasive assessment of AD biomarkers [11,12], with the aim of providing tools for the early detection of at-risk individuals, who can benefit from preventative interventions. Subjects in asymptomatic at-risk stages can be identified through dementia risk scores, which are weighted composites of non-modifiable and modifiable risk factors that reflect the likelihood of an individual developing dementia [13]. Overall, focus has shifted towards detecting pre-clinical non-symptomatic (or early symptomatic) persons at risk of developing dementia, as they are believed to provide a unique target group for preventive and/or disease-modifying interventions. Given the role of modifiable factors related to lifestyle and vascular health, prevention trials have focused on multidomain approaches, where multiple risk factors are simultaneously addressed to maximise benefits. In the following section, we present a brief summary of evidence on the main modifiable risk and protective factors for late-life cognitive impairment and dementia, which are targeted in multidomain prevention studies and are in the focus of the LETHE project.
2.1.1. Physical Activity
Engagement in regular physical activity has been linked to a lower risk of cognitive decline, dementia, and AD in many prospective studies. The association is observed when investigating physical activity in midlife, but older adults who exercise are also more likely to maintain cognition than those who do not exercise [1]. The results of one meta-analysis of 15 prospective cohort studies following up on 33,816 individuals without dementia for 1–12 years reported that physical activity had a significant protective effect against cognitive decline, with high levels of activity being the most protective (hazard ratio ((acrshorthr) 0.62, 95% CI 0.54–0.70) [14]. Another meta-analysis included 16 studies with 163,797 participants without dementia and found that the risk ratio (RR) of dementia in the highest physical activity groups compared with the lowest was 0.72 (95% CI 0.60–0.86), and the RR of AD was 0.55 (95% CI 0.36–0.84) [15]. From the point of view of preventive interventions, the WHO guidelines on physical activity for global health have been integrated into the guidelines for dementia risk reduction [7].
2.1.2. Cardiovascular Risk Factors—Diabetes, Hypertension, Hypercholesterolaemia, and Obesity
Several studies consistently reported an increased risk of dementia and AD in association with vascular and metabolic risk factors, such as hypertension, hypercholesterolaemia, and obesity at midlife (≤65 years) [1]. Adequate management of these cardiovascular risk factors is pivotal in reducing cardiovascular morbidity in older populations and is thus recommended in midlife, while specific considerations apply for more advanced ages, as in this age group, evidence on some pharmacological interventions (e.g., statins) is mixed. Active treatment of hypertension in middle-aged (45–65 years) and older people (aged older than 65 years) without dementia is recommended to reduce dementia incidence [1]. For diabetes, the association with the increased risk of dementia and AD has been shown for all of adult life, with the risk being stronger when diabetes occurs in midlife than in late-life [1]. At an older age, management of diabetes is recommended through standard glycaemic control rather than intense glycaemic control due to the increased vulnerability of older adults to hypoglycaemia, which can increase dementia risk.
2.1.3. Social Interaction
Social isolation might be a prodrome or a part of the dementia syndrome [3]. However, growing evidence has shown that a lack of social engagement is also a risk factor for dementia, while social contact—from being in a relationship, having contact and exchanging support with family members or friends, participating in community groups, or engaging in paid work—can be beneficial [3]. Cognitive benefits of social engagement, although of modest size in some studies, seem to be consistent across studies conducted in diverse populations, supporting the significance of social activity in different settings and cultures, and highlighting the importance of considering social engagement in older people and not only their physical and mental health.
2.1.4. Nutrition
Diet across the whole lifespan has a major effect on health and is linked to late-life cognition and dementia risk, both directly and through its role on cardiovascular risk factors related to dementia, such as diabetes mellitus, obesity, and hypertension. Observational studies and RCTs have reported a reduced risk of cognitive impairment, dementia, and AD in subjects with high adherence to specific diets, including the Mediterranean Diet, the Nordic Diet, DASH (Dietary Approaches to Stop Hypertension), and the hybrid MIND (Mediterranean-DASH Intervention for Neurodegenerative Delay) diet. Common elements of these diets are the high intake of vegetables, nuts, and legumes; preference for whole grains; and low consumption of red meat and high-saturated-fat foods. Differences in the three dietary profiles entail specific indications of the quantity/quality of fruit and vegetable oils (in general high consumption), as well as fish, poultry, and dairy products (low-moderate intake) [1,3].
2.1.5. Cognitive Stimulating Activity
Mentally stimulating activities across the lifespan, including education, occupational mental demands, and cognitively stimulating leisure activities, have been associated with better late-life cognition and decreased risk of cognitive impairment, AD, and dementia. Such a protective effect might be attributed to mechanisms related to the reduced accumulation of AD neuropathology (i.e., resistance to AD), or the ability to delay or avoid the clinical expression of underlying neuropathology, or resilience to AD [16]. Cognitive stimulation can continue into late life and can be promoted through various activities, including cognitive stimulation therapy, which implies participation in a range of activities aimed at improving cognitive and social functioning, and/or cognitive training, consisting of a guided practice of specific standardised tasks designed to enhance particular cognitive functions, such as memory, attention, or problem solving [17]. Computerised cognitive training is increasingly available and evidence from intervention studies in cognitively healthy older adults and subjects with MCI is encouraging, although methodological limitations exist, and findings needs to be further verified [3,7].
2.1.6. Sleep, Meditation and Relaxation
Sleep disorders have received attention in recent years for their potential role in the development of cognitive impairment [18]. A main challenge in assessing the current evidence stems from the methodological heterogeneity of studies carried out so far, including different designs (cross-sectional, longitudinal), study populations (some cohorts included cases with cognitive impairment), and heterogeneity of sleep-related parameters assessed (quality, measured through different indicators, and duration). Two meta-analyses reported that sleep disturbances were associated with a higher risk of all-cause dementia (RR 1.2; 95% CI 1.1–1.3) and AD dementia (RR 1.6; 95% CI 1.3–1.9) compared with the absence of sleep disturbance [19,20]. Even if less evidence is available on the potential cognitive benefits of meditation, relaxation, and spirituality, there is growing interest in these factors, as they have been suggested to be related to AD risk [21].
2.2. Predicting Dementia and Cognitive Decline
Up to date, most models have applied regression methods to predict dementia [22]. Recently, Pekkala et al. developed a late-life dementia prediction index using supervised machine learning based on data from a population-based Cardiovascular Risk Factors, Aging, and Incidence of Dementia (CAIDE) study [23,24], and they reported good results for shorter-term dementia prediction [25]. It has also been shown that deep learning methods are promising for predicting cognitive decline [26]. Generally, predicting dementia or cognitive decline requires a quantitative parameter to derive information from. Accurate risk prediction of dementia can leverage on a wide range of data—lifestyle, health-related, etc.—which can be cumbersome to determine. Walters et al. attempted to circumvent this problem by using data routinely collected in primary care settings for dementia prediction using a regression model, which showed good results for an age range between 60 and 79 years [27].
Besides these global architectures targeted at the prediction of dementia, the detection of specific dementia-relevant early symptoms using wearable technology has also already be demonstrated. For example, it was shown that smart glasses can be used to monitor eye blinks [28], which can help to distinguish between essential tremor and essential tremor-Parkinson’s disease [29] and it was demonstrated that reliable wearable medical monitoring systems can nowadays easily be implemented on mobile devices [30].
A consequent extension of current methods would be a combination of modern machine learning methods and routinely—or even better, continuously—acquired data to improve predictions on an individual level.
2.3. Sharing of Health Data
AI and machine learning technologies require large, diverse, and high-quality data sets to ensure thorough training of the algorithms and to maintain the inclusion of all relevant aspects. Collaborative data from various sources therefore greatly fosters data-driven machine learning methods to yield robust and bias-free models which generalise well to new unseen data [31,32,33]. However, especially in the healthcare domain, sharing of health data for collaborative efforts is accompanied by numerous barriers [34,35] since the data are highly sensitive in terms of data protection and data privacy since confidential patient data are not to be shared with unwanted third parties under any circumstances. Therefore, the usage of these data are strongly regulated to preserve patient rights, and compliance to data protection must be carefully assessed before data sharing [36,37]. Besides regulatory considerations, sharing and subsequently merging data from multiple institutions also comprises technical challenges regarding data curation and data harmonisation [38]. A way to bypass this problem is to omit central storage of the data, perform calculations at the data source, and only communicate model updates based on the local data without ever transmitting the data itself. This approach, termed federated learning [39], has the potential to revolutionise future studies in the healthcare sector since the amount of training data can be drastically increased, while security issues can be handled easier.
3. The LETHE Project Approach
The aim of the LETHE project is to implement the promising FINGER intervention model through ICT sensing and intervention technology and establish new digital biomarkers and models which allow monitoring and projecting cognitive decline and related risk factor progression. The aim is a fully integrated and validated approach to positively influence the above-mentioned modifiable risk factors based on big data collection and advanced health monitoring, AI-based personalised risk detection, and personalised early interventions. LETHE will base the initial AI model on unique long-term data collection from key European clinical partners active in dementia research. Furthermore, the LETHE consortium includes partners representing the target group of the LETHE model (Alzheimer Europe advocacy group and LETHE Advisory Board composed of lay people), as well as experienced ICT development and research partners in the field of sensing, intervention technology, AI, big data infrastructure and behaviour psychology expertise, and data protection experts. This joint expertise makes it possible to address the planned concept, taking into account all necessary requirements. LETHE goes beyond previous prevention trials by first developing a robust prediction model building up on big data from several datasets and including people in pre-stages of dementia or early dementia and second by planning an ICT-based multidomain lifestyle intervention, which will be continuously optimised during an 18-month validation trial by generating new individual data (digital biomarkers) via wearables.
LETHE will perform this by:
- Using existing data from multinational, European clinical observational cohorts, and population-based observational and intervention studies (including the FINGER RCT, with data from an up to 11-year follow-up, assessing the long-term effects of a 2-year multidomain intervention) to develop initial prediction models for the progression of dementia and related risk factors;
- Using results from former ICT-based EU projects to implement a mainly automated ICT-based FINGER intervention model supported by validated sensing and interaction technology;
- Extending and validating the personalised prediction models using digital biomarkers collected in an 18-month validation trial in subjects at-risk of dementia, which will include two arms: ICT-assisted structured multimodal intervention and self-guided intervention group;
- Implementing a big data framework which allows a multicentre model optimisation and roll out;
- Providing knowledge for individuals and care professionals about dementia risk factors and risk of disease onset and progression, integrating information on lifestyle parameters, individual health data, and AD-related biomarkers, such as MRI (structural brain change) and blood-based biomarkers (APOE genotype, plasma markers related to AD: amyloid-42, amyloid-40, phosphorylated (p)-Tau181, p-Tau231, neurofilament light chain), thereby assessing their individual potential to benefit from multidomain preventive interventions.
Figure 1 visualises the overall approach defining the five core modules of LETHE. These are (i) the mixed knowledge models based on big data analysis of previous large-scale cross-sectional, longitudinal, and interventional trials from different European Countries; (ii) the personalised ICT-assisted intervention protocol based on model simulations; (iii) the intervention framework targeting seven main dementia modifiable factors; (iv) the data collection framework based on multicentre passive and active ICT-supported data collection; (v) the knowledge discovery and visualisation for the person in the risk group as well as professionals.
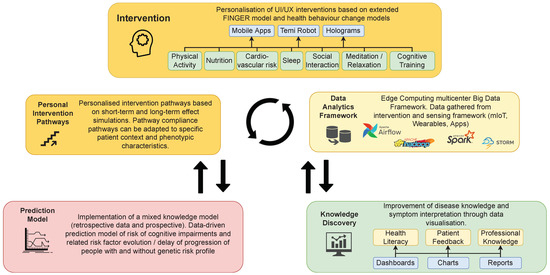
Figure 1.
The LETHE overall approach.
3.1. Technical Architecture of LETHE
Figure 2 visualises the detailed technical architecture of the LETHE solution. The distribution of the modules regarding cloud infrastructure deployment as well as federate computing machine learning models is not considered here. Core parts of the architecture are the following: data generation over standardised protocols and utilising the RADAR-BASE middleware (https://radar-base.org/, accessed on 10 May 2022). LETHE will integrate third-party wearables, apps, and mIoT (mobile Internet of Things) devices (such as a blood pressure meter) over standardised interfaces such as RESTful API, MQTT, etc., also available in RADAR-BASE. LETHE will contribute to the open source RADAR-BASE community by providing APIs not yet available on the platform. The data generation technology in LETHE is application-independent and allows adapting the data collection technology (provider) depending on other setups or technology updates in the next few years.
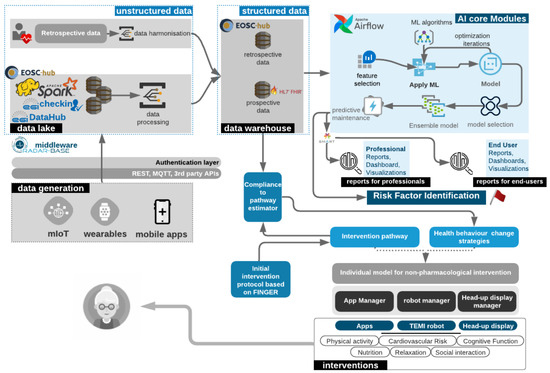
Figure 2.
LETHE detailed technical architecture.
The core modules Data Lake and Data Warehouse comprise big data collection, harmonisation, structuring, and pre-processing in the data lakes and integration into the data warehouse. Data Lake thereby represents a repository of data stored in their raw format. LETHE will employ big data frameworks based on EGI-federated cloud infrastructure (https://www.egi.eu/federation/egi-federated-cloud/, accessed on 10 May 2022) using Apache Hadoop and Spark and EGI/EOSC services for distributed large-scale data management. In phase I of the project, LETHE will resort to and optimise existing data. Clinical relevant data will be structured and saved in the HL7 FHIR standard. This will allow a standardised and secure exchange of data as well as enable additional parties to provide target-group-specific visualisations integrated into third-party electronic health records (EHRs) or hospital systems (for example, using SMART on FHIR (https://docs.smarthealthit.org/, accessed on 10 May 2022). Structured and unstructured data will be hosted in an European open science cloud (EOSC) environment, which ensures secure and protected data storage. The AI core modules form the third major group in LETHE’s architecture, integrating several modules and phases. Feature selection is applied for regression machine learning (ML) modules; otherwise, deep learning models will be used. Model development will apply different approaches, which will be tested and optimised iteratively. Initial models will be based on training with existing data, whereas final models will integrate new features based on digital biomarkers. For the final model selection, the model ensemble will then be analysed in validation trials. The workflow from data retrieval to model optimisation will be orchestrated by Apache Airflow. LETHE will distribute the models over the different trial sites (distributed ML).
3.2. Prediction Models
The development of the LETHE prediction model will be comprised of two phases (see Figure 3). Phase I will utilise retrospective data from multiple institutions to train an initial prediction model to predict the possible onset of cognitive decline among older adults at risk of dementia. Retrospective data include features regarding demographics, clinical markers, cognition, health status, functional status, lifestyle, mood, and quality of life. Due to different designs of the involved studies, however, only parameters acquired in the majority of these studies can be used in phase I to provide a sufficiently large data set. In phase II, the baseline prediction model will be extended to include continuous monitoring data about individual behaviours, lifestyle, and digital biomarkers gathered from a variety of wearable technologies. An overview of available data in each phase is shown in Table 1.
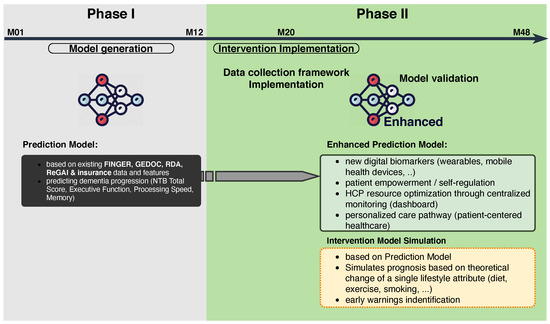
Figure 3.
Two phases of the LETHE model implementation: Phase I—model generation based on retrospective data; Phase II—model extension and model validation.

Table 1.
Available data for phases I and II of the LETHE project.
The employment of AI algorithms based on multimodal learning will allow for the joined exploitation of structured and unstructured data to investigate the relations between digital biomarkers, medical, and user-generated datasets. Unsupervised AI algorithms will be developed (e.g., deep autoencoders and clustering algorithms) to discover new knowledge, such as previously unexplored relations between retrospective and behavioural data. Furthermore, supervised predictive models will be developed, e.g., Long Short-term Memory (LSTMs) Neural Networks, which are specialised for handling data with the temporal component. The time modelling will allow for the identification and prediction of disease/treatment trajectories and relapse. Recently, the use of deep learning models has attracted attention for the prediction of cognitive decline in elderly people [26,40,41]. The new knowledge, patient similarities, and predicted trajectories will be utilised to monitor new patients based on patients with similar profiles.
4. Discussion
4.1. Leveraging Big Data Analytics, AI and Biomarkers for Personalised Early Risk Prediction of Cognitive Decline
LETHE aims to advance the FINGER multidomain prevention approach with the integration of AI-based prediction models, enabling accurate assessment and monitoring of dementia risk and cognitive trajectories and implementing an ICT-based multidomain lifestyle intervention, which will be tested in a validation trial in subjects at risk of dementia. In this framework, state-of-the art and innovation technologies from three different technical domains are combined: big data, AI analytics, and visualisation. In recent years, big data has proven to be a disruptive technology that has found its way into our daily lives to predict our behaviour and tailor services to our individual needs. In LETHE, there is a similar goal for cognitive decline and risk of dementia: to meet the short-term and long-term needs for people at-risk by providing personal risk assessment and predicting cognitive changes based on past and current behaviour and health data. The availability of modern technology serves as a beacon for the creation of new, previously unthought of ways of risk assessment and prevention in at-risk stages in subjects with no or subtle cognitive symptoms. Moreover, integrating data from technologies commonly present in all levels of society such as intelligent Electronic Health Records (EHRs), innovative biomarkers, mobile devices, smart sensors, and wearables exponentially increases this potential. As there have been considerable technological developments in big data and analytics, some of the early challenges have been largely solved. However, many remain that can profoundly influence the success of the LETHE project and future projects. As such, it is our goal to address all these challenges and provide practical solutions. The main challenges that need to be solved include:
- Scalability and adaptation to data growth;
- Generation of information and insights on the temporal evolution of cognitive decline in predementia stages;
- Integration of heterogeneous sources of structured and unstructured data;
- Acquisition of high-quality data, their validation and verification;
- Securing of health data and anonymisation despite personalisation.
To date, some studies using mIoT, sensors, and/or wearables have addressed many of these issues in several different ways. Bashir et al. [42] suggested a big data framework for data analytics collected from smart mIoT and wearable data using a combination of Cloudera Hadoop and PySpark. Zhang et al. [43] proposed the use of Firework, which provides virtual data views on physically distributed data, allowing them to be treated as a single data source. Yet another approach by Rathore et al. [44] stipulates the use of the MapReduce Hadoop ecosystem in a real environment, whereby data are collected by deploying different smart sensors and IoT devices and exploited through big data analytics.
Regarding prediction models for dementia, there are several risk factors and biomarkers linked to cognitive impairment, dementia, and AD, but their clinical utility is still limited. Several risk prediction models have already been developed, e.g., the CAIDE dementia risk score [45] that was developed by the members of the LETHE consortium and that has been already used as an educational tool to disseminate information on dementia risk factors and also as a screening instrument to select at-risk persons for the FINGER trial. However, much work is still needed until accurate and reliable prediction tools can be used in practice for decision-making related to the early detection of risk and the prevention of dementia. LETHE builds up on these achievements and the availability of other findings in the area of dementia risk assessment to define optimal recommendations for dementia risk assessment and prediction use cases and improve on them or find new models and tools if needed. Accurate dementia prediction requires tools that are able to handle large amounts of complex multimodal data, e.g., cognitive, clinical, blood, genetic, and environmental risk factors, and their temporal dynamics but also novel digital biomarkers from, e.g., wearables. Data mining should be transparent and reliable, i.e., not just a dementia probability number but also a comprehensive and objective signature of risk and prevention potential to support clinicians in decision-making [25,46]. Such models have already been developed using machine learning methods by the consortium members, and a similar approach can be further developed with novel risk signature data collected within the LETHE project. Within the LETHE project, we will develop prediction models for cognitive decline with better sensitivity to change over time, determining intervention-related change in overall dementia risk. For the first time, the long-term risk prediction model can be developed with detailed long-term data (up to 11 years) of at-risk individuals within an actual preventive clinical trial as well as with a new 18-month preventive trial collecting rich digital biomarker data. These models can be used in clinical practice but also as tools to identify target populations for the next generation of digital RCTs to prevent dementia in the future.
4.2. Long Term Disease Knowledge
Cognitive impairment, dementia, and AD are complex and heterogeneous disorders, and their complexity unfolds on different levels (e.g., shared risk factors and pathogenic interactions of neurodegenerative and vascular underpinnings of cognitive impairment, synergistic effects on cognition). Addressing the complexity and heterogeneity of dementia and AD by incorporating multidimensional data reflecting risk factors, disease-driving mechanisms, and age-related processes, together with novel digital biomarkers, into prediction models, as proposed in the LETHE project, will accelerate the development of effective strategies for dementia prediction and prevention. Neurodegenerative processes and disease-related early behavioural changes might affect biological factors in presymptomatic stages of dementia [47]; thus, the time-dependent effect of specific risk factors implies that a life-course approach is crucial to understanding the effect of a specific exposure on the risk of dementia. The early identification of individuals at a higher risk of developing dementia becomes critical, as this may provide a window of opportunity to adopt lifestyle changes to reduce the risk of dementia [48]. However, there is still a considerable gap between the epidemiological evidence and its underlying biological mechanisms. Personalised prediction and intervention implies comprehensive phenotyping of the subjects at risk in order to establish risk and prevention potential and assign persons to tailored interventions. Further information on cognitive function, brain imaging, and blood biomarkers is needed to establish what should be measured and what treatment effect size should be determined in future prevention trials. As neuropathological changes (e.g., cerebral accumulation of beta-amyloid and neurofibrillary tangles in the case of Alzheimer’s disease) can precede the onset of cognitive problems [9,10] by a few decades, in vivo biomarkers mirroring such changes are risk indicators which can inform risk assessment and monitoring. Evaluation of blood biomarkers linked to AD is a rapidly growing research area, as it is expected to become a cost-effective and minimally invasive approach. These biomarkers might be used to identify and characterise higher-risk individuals to take part in trials. A recent study showed that low amyloid-42 and high NfL plasma levels are each independently and in combination strongly associated with the risk of all-cause and AD dementia. These data indicate that plasma NfL and amyloid-42 levels can be used to assess the risk of developing dementia in a non-demented population. Additionally, the ApoE 4 allele—the largest sole genetic risk factor for AD—is nowadays commonly used for risk stratification in clinical trials, thereby showing different responses on interventional approaches in ApoE4 carriers and non-carriers [49]. On the other side, blood biomarkers could be used for monitoring the progression of the disease or even the efficacy of intervention, especially if intervention is to be given to cognitively and functionally intact individuals long before dementia onset, as clinical endpoints (e.g., clinical diagnosis) often used in RCTs targeting symptomatic subjects might be not feasible in earlier at-risk stages. In line with this, in cognitively healthy adults at risk for AD, moderate physical activity was shown to lead to lower levels of pTau/Ab42 and tTau/Ab42 ratios as well as higher levels of Ab in CSF [50]. Plasma NfL levels may be additionally useful in this regard [50]. Blood biomarkers might represent a clinically applicable alternative surrogate endpoint for trials that would be both cost-effective and minimally invasive, but little is known about their value as surrogate endpoints for treatment responses in the prevention of AD dementia [51]. Up to now, data from longitudinal studies concerning the beneficial effect of physical activity on AD biomarkers is scarce. Aerobic exercise is hypothesised to induce widespread and permanent molecular and cellular changes that underlie both neurodegeneration and neurogenesis [52]. In contrast, cognitive training is hypothesised to induce minor brain structural changes but contribute to functional changes in trained cognitive domains [53]. MRI changes on regional brain volumes and cortical thickness have been evaluated in the FINGER RCT, and exploratory analysis indicated that MRI parameters can predict cognitive benefits to multidomain interventions and could thus support risk stratification [54].
Based on the state-of-the art knowledge, the LETHE trial will integrate several biomarkers, including brain MRI, APOE4 genotype, and blood biomarkers (plasma amyloid-42, NfL, p-tau181, p-tau231), which will be used in LETHE for stratifying individuals regarding their underlying biological risk and predicting the response to the ICT-supported multidomain intervention.
5. Conclusions
Understanding the complex and multifactorial causes of dementia is still an unmet goal in dementia research. The collection of behaviour and medical data is therefore a key part of the LETHE project and requirement for personalised and smart interventions. The LETHE project aims to leverage large multidimensional data about individual behaviours, lifestyle, health, and digital biomarkers on a previously unprecedented scale. Furthermore, by supporting the utilisation of a plethora of mIoT and wearable technologies for home-based dementia prevention and health promotion, high levels of accuracy in monitoring can be achieved, and patterns of very early cognitive and behavioural changes that predict cognitive decline can be detected among older adults at risk of dementia.
Author Contributions
Conceptualisation: S.H., M.B., B.N., and E.S.; Methodology: S.H., M.B., B.N., E.S., T.N., F.M., P.M., and H.U.; Investigation: S.H., M.B., B.N., and E.S.; Writing—original draft preparation: S.H., M.B., B.N., E.S., and H.U.; Writing—review and editing: S.H., M.B., B.N., E.S., and F.M.; Visualisation: S.H., M.B., and B.N.; Supervision: S.H.; Project administration: S.H.; Funding acquisition: S.H. and E.S. All authors have read and agreed to the published version of the manuscript.
Funding
The LETHE-Project has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement no 101017405 (https://cordis.europa.eu/project/id/101017405, accessed on 10 May 2022).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
This research is supported by a larger consortium, including Alzheimer Europe, Idryma Technologias kai Erevnas, Universiteit Maastricht, Kaasa Solution GmbH, i2Grow, Stichting EGI, Extra Red SRL, Infotrend Innovations Company Limited, Combinostics Oy, The Lisbon Council for Economic Competitiveness ASBL.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kivipelto, M.; Mangialasche, F.; Ngandu, T. Lifestyle interventions to prevent cognitive impairment, dementia and Alzheimer disease. Nat. Rev. Neurol. 2018, 14, 653–666. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Status Report on the Public Health Response to Dementia; WHO: Geneva, Switzerland, 2021.
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C.; et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef]
- Ngandu, T.; Lehtisalo, J.; Solomon, A.; Levälahti, E.; Ahtiluoto, S.; Antikainen, R.; Bäckman, L.; Hänninen, T.; Jula, A.; Laatikainen, T.; et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomised controlled trial. Lancet 2015, 385, 2255–2263. [Google Scholar] [CrossRef]
- Andrieu, S.; Guyonnet, S.; Coley, N.; Cantet, C.; Bonnefoy, M.; Bordes, S.; Bories, L.; Cufi, M.N.; Dantoine, T.; Dartigues, J.F.; et al. Effect of long-term omega 3 polyunsaturated fatty acid supplementation with or without multidomain intervention on cognitive function in elderly adults with memory complaints (MAPT): A randomised, placebo-controlled trial. Lancet Neurol. 2017, 16, 377–389. [Google Scholar] [CrossRef]
- Moll van Charante, E.P.; Richard, E.; Eurelings, L.S.; van Dalen, J.W.; Ligthart, S.A.; van Bussel, E.F.; Hoevenaar-Blom, M.P.; Vermeulen, M.; van Gool, W.A. Effectiveness of a 6-year multidomain vascular care intervention to prevent dementia (preDIVA): A cluster-randomised controlled trial. Lancet 2016, 388, 797–805. [Google Scholar] [CrossRef] [Green Version]
- WHO. Risk Reduction of Cognitive Decline and Dementia: WHO Guidelines; WHO: Geneva, Switzerland, 2019.
- Petersen, R.C.; Lopez, O.; Armstrong, M.J.; Getchius, T.S.D.; Ganguli, M.; Gloss, D.; Gronseth, G.S.; Marson, D.; Pringsheim, T.; Day, G.S.; et al. Practice guideline update summary: Mild cognitive impairment: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology 2018, 90, 126–135. [Google Scholar] [CrossRef]
- Bateman, R.J.; Xiong, C.; Benzinger, T.L.S.; Fagan, A.M.; Goate, A.; Fox, N.C.; Marcus, D.S.; Cairns, N.J.; Xie, X.; Blazey, T.M.; et al. Clinical and biomarker changes in dominantly inherited Alzheimer’s disease. N. Engl. J. Med. 2012, 367, 795–804. [Google Scholar] [CrossRef] [Green Version]
- Jack, C.R.; Bennett, D.A.; Blennow, K.; Carrillo, M.C.; Dunn, B.; Haeberlein, S.B.; Holtzman, D.M.; Jagust, W.; Jessen, F.; Karlawish, J.; et al. NIA-AA Research Framework: Toward a biological definition of Alzheimer’s disease. Alzheimer’s Dement. 2018, 14, 535–562. [Google Scholar] [CrossRef]
- Mattsson, N.; Andreasson, U.; Zetterberg, H.; Blennow, K.; Alzheimer’s Disease Neuroimaging Initiative. Association of Plasma Neurofilament Light with Neurodegeneration in Patients with Alzheimer Disease. JAMA Neurol. 2017, 74, 557–566. [Google Scholar] [CrossRef]
- Verberk, I.M.W.; Slot, R.E.; Verfaillie, S.C.J.; Heijst, H.; Prins, N.D.; van Berckel, B.N.M.; Scheltens, P.; Teunissen, C.E.; van der Flier, W.M. Plasma Amyloid as Prescreener for the Earliest Alzheimer Pathological Changes. Ann. Neurol. 2018, 84, 648–658. [Google Scholar] [CrossRef]
- Anstey, K.J.; Zheng, L.; Peters, R.; Kootar, S.; Barbera, M.; Stephen, R.; Dua, T.; Chowdhary, N.; Solomon, A.; Kivipelto, M. Dementia Risk Scores and Their Role in the Implementation of Risk Reduction Guidelines. Front. Neurol. 2022, 12, 765454. [Google Scholar] [CrossRef] [PubMed]
- Sofi, F.; Valecchi, D.; Bacci, D.; Abbate, R.; Gensini, G.F.; Casini, A.; Macchi, C. Physical activity and risk of cognitive decline: A meta-analysis of prospective studies. J. Intern. Med. 2011, 269, 107–117. [Google Scholar] [CrossRef] [PubMed]
- Hamer, M.; Chida, Y. Physical activity and risk of neurodegenerative disease: A systematic review of prospective evidence. Psychol. Med. 2009, 39, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Arenaza-Urquijo, E.M.; Vemuri, P. Improving the resistance and resilience framework for aging and dementia studies. Alzheimer’s Res. Ther. 2020, 12, 41. [Google Scholar] [CrossRef] [Green Version]
- Bahar-Fuchs, A.; Clare, L.; Woods, B. Cognitive training and cognitive rehabilitation for persons with mild to moderate dementia of the Alzheimer’s or vascular type: A review. Alzheimer’s Res. Ther. 2013, 5, 35. [Google Scholar] [CrossRef]
- Irwin, M.R.; Vitiello, M.V. Implications of sleep disturbance and inflammation for Alzheimer’s disease dementia. Lancet Neurol. 2019, 18, 296–306. [Google Scholar] [CrossRef]
- Bubu, O.M.; Brannick, M.; Mortimer, J.; Umasabor-Bubu, O.; Sebastião, Y.V.; Wen, Y.; Schwartz, S.; Borenstein, A.R.; Wu, Y.; Morgan, D.; et al. Sleep, Cognitive impairment, and Alzheimer’s disease: A Systematic Review and Meta-Analysis. Sleep 2016, 40, zsw032. [Google Scholar] [CrossRef]
- Shi, L.; Chen, S.J.; Ma, M.Y.; Bao, Y.P.; Han, Y.; Wang, Y.M.; Shi, J.; Vitiello, M.V.; Lu, L. Sleep disturbances increase the risk of dementia: A systematic review and meta-analysis. Sleep Med. Rev. 2018, 40, 4–16. [Google Scholar] [CrossRef]
- Khalsa, D.S.; Newberg, A.B. Spiritual Fitness: A New Dimension in Alzheimer’s Disease Prevention. J. Alzheimer’s Dis. 2021, 80, 505–519. [Google Scholar] [CrossRef]
- Tang, E.Y.H.; Harrison, S.L.; Errington, L.; Gordon, M.F.; Visser, P.J.; Novak, G.; Dufouil, C.; Brayne, C.; Robinson, L.; Launer, L.J.; et al. Current Developments in Dementia Risk Prediction Modelling: An Updated Systematic Review. PLoS ONE 2015, 10, e0136181. [Google Scholar] [CrossRef] [Green Version]
- Kivipelto, M. Midlife vascular risk factors and Alzheimer’s disease in later life: Longitudinal, population based study. BMJ 2001, 322, 1447–1451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Solomon, A.; Ngandu, T.; Soininen, H.; Hallikainen, M.M.; Kivipelto, M.; Laatikainen, T. Validity of dementia and Alzheimer’s disease diagnoses in Finnish national registers. Alzheimer’s Dement. 2013, 10, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Pekkala, T.; Hall, A.; Lötjönen, J.; Mattila, J.; Soininen, H.; Ngandu, T.; Laatikainen, T.; Kivipelto, M.; Solomon, A. Development of a Late-Life Dementia Prediction Index with Supervised Machine Learning in the Population-Based CAIDE Study. J. Alzheimer’s Dis. 2017, 55, 1055–1067. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stamate, D.; Smith, R.; Tsygancov, R.; Vorobev, R.; Langham, J.; Stahl, D.; Reeves, D. Applying Deep Learning to Predicting Dementia and Mild Cognitive Impairment. In IFIP Advances in Information and Communication Technology; Springer International Publishing: Cham, Switzerland, 2020; pp. 308–319. [Google Scholar]
- Walters, K.; Hardoon, S.; Petersen, I.; Iliffe, S.; Omar, R.Z.; Nazareth, I.; Rait, G. Predicting dementia risk in primary care: Development and validation of the Dementia Risk Score using routinely collected data. BMC Med. 2016, 14, 6. [Google Scholar] [CrossRef] [Green Version]
- Sciarrone, A.; Bisio, I.; Garibotto, C.; Lavagetto, F.; Staude, G.H.; Knopp, A. Leveraging IoT Wearable Technology Towards Early Diagnosis of Neurological Diseases. IEEE J. Sel. Areas Commun. 2021, 39, 582–592. [Google Scholar] [CrossRef]
- Arabia, G.; Lupo, A.; Manfredini, L.I.; Vescio, B.; Nisticò, R.; Barbagallo, G.; Salsone, M.; Morelli, M.; Novellino, F.; Nicoletti, G.; et al. Clinical, electrophysiological, and imaging study in essential tremor-Parkinson’s disease syndrome. Park. Relat. Disord. 2018, 56, 20–26. [Google Scholar] [CrossRef]
- Li, Z.; Lian, L.; Pei, J.; She, Y. Design and implementation of wearable medical monitoring system on the internet of things. J. Ambient. Intell. Humaniz. Comput. 2021, 1–14. [Google Scholar] [CrossRef]
- Wang, F.; Casalino, L.P.; Khullar, D. Deep Learning in Medicine—Promise, Progress, and Challenges. JAMA Intern. Med. 2019, 179, 293–294. [Google Scholar] [CrossRef]
- De Fauw, J.; Ledsam, J.R.; Romera-Paredes, B.; Nikolov, S.; Tomasev, N.; Blackwell, S.; Askham, H.; Glorot, X.; O’Donoghue, B.; Visentin, D.; et al. Clinically applicable deep learning for diagnosis and referral in retinal disease. Nat. Med. 2018, 24, 1342–1350. [Google Scholar] [CrossRef]
- Peiffer-Smadja, N.; Maatoug, R.; Lescure, F.X.; D’Ortenzio, E.; Pineau, J.; King, J.R. Machine Learning for COVID-19 needs global collaboration and data-sharing. Nat. Mach. Intell. 2020, 2, 293–294. [Google Scholar] [CrossRef]
- Van Panhuis, W.G.; Paul, P.; Emerson, C.; Grefenstette, J.; Wilder, R.; Herbst, A.J.; Heymann, D.; Burke, D.S. A systematic review of barriers to data sharing in public health. BMC Public Health 2014, 14, 1144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pezoulas, V.C.; Exarchos, T.P.; Fotiadis, D.I. (Eds.) Chapter 3—Medical data sharing. In Medical Data Sharing, Harmonization and Analytics; Academic Press: Cambridge, MA, USA, 2020; pp. 67–104. [Google Scholar]
- Hulsen, T. Sharing Is Caring-Data Sharing Initiatives in Healthcare. Int. J. Environ. Res. Public Health 2020, 17, 3046. [Google Scholar] [CrossRef] [PubMed]
- Pezoulas, V.C.; Exarchos, T.P.; Fotiadis, D.I. (Eds.) Chapter 4—Data protection. In Medical Data Sharing, Harmonization and Analytics; Academic Press: Cambridge, MA, USA, 2020; pp. 105–136. [Google Scholar]
- Pezoulas, V.C.; Exarchos, T.P.; Fotiadis, D.I. (Eds.) Chapter 5—Medical data harmonization. In Medical Data Sharing, Harmonization and Analytics; Academic Press: Cambridge, MA, USA, 2020; pp. 137–183. [Google Scholar]
- McMahan, H.B.; Moore, E.; Ramage, D.; Hampson, S.; y Arcas, B.A. Communication-Efficient Learning of Deep Networks from Decentralized Data. arXiv 2017, arXiv:cs.LG/1602.05629. [Google Scholar]
- Nori, V.S.; Hane, C.A.; Sun, Y.; Crown, W.H.; Bleicher, P.A. Deep neural network models for identifying incident dementia using claims and EHR datasets. PLoS ONE 2020, 15, e0236400. [Google Scholar] [CrossRef] [PubMed]
- Almubark, I.; Chang, L.C.; Shattuck, K.F.; Nguyen, T.; Turner, R.S.; Jiang, X. A 5-min Cognitive Task with Deep Learning Accurately Detects Early Alzheimer’s Disease. Front. Aging Neurosci. 2020, 12, 603179. [Google Scholar] [CrossRef] [PubMed]
- Bashir, M.R.; Gill, A.Q. Towards an IoT Big Data Analytics Framework: Smart Buildings Systems. In Proceedings of the 2016 IEEE 18th International Conference on High Performance Computing and Communications; IEEE 14th International Conference on Smart City; IEEE 2nd International Conference on Data Science and Systems (HPCC/SmartCity/DSS), Sydney, Australia, 12–14 December 2016; pp. 1325–1332. [Google Scholar]
- Zhang, Q.; Zhang, X.; Zhang, Q.; Shi, W.; Zhong, H. Firework: Big Data Sharing and Processing in Collaborative Edge Environment. In Proceedings of the 2016 Fourth IEEE Workshop on Hot Topics in Web Systems and Technologies (HotWeb), Washington, DC, USA, 24–25 October 2016; pp. 20–25. [Google Scholar]
- Rathore, M.M.; Ahmad, A.A.; Paul, A. IoT-based smart city development using big data analytical approach. In Proceedings of the 2016 IEEE International Conference on Automatica (ICA-ACCA), Curico, Chile, 19–21 October 2016. [Google Scholar]
- Kivipelto, M.; Ngandu, T.; Laatikainen, T.; Winblad, B.; Soininen, H.; Tuomilehto, J. Risk score for the prediction of dementia risk in 20 years among middle aged people: A longitudinal, population-based study. Lancet Neurol. 2006, 5, 735–741. [Google Scholar] [CrossRef]
- Hall, A.; Pekkala, T.; Polvikoski, T.; van Gils, M.; Kivipelto, M.; Lötjönen, J.; Mattila, J.; Kero, M.; Myllykangas, L.; Mäkelä, M.; et al. Prediction models for dementia and neuropathology in the oldest old: The Vantaa 85+ cohort study. Alzheimer’s Res. Ther. 2019, 11, 11. [Google Scholar] [CrossRef] [Green Version]
- Tolppanen, A.M.; Solomon, A.; Soininen, H.; Kivipelto, M. Midlife vascular risk factors and Alzheimer’s disease: Evidence from epidemiological studies. J. Alzheimer’s Dis. 2012, 32, 531–540. [Google Scholar] [CrossRef]
- Goerdten, J.; Čukić, I.; Danso, S.O.; Carrière, I.; Muniz-Terrera, G. Statistical methods for dementia risk prediction and recommendations for future work: A systematic review. Alzheimer’s Dement. 2019, 5, 563–569. [Google Scholar] [CrossRef]
- Solomon, A.; Turunen, H.; Ngandu, T.; Peltonen, M.; Levälahti, E.; Helisalmi, S.; Antikainen, R.; Bäckman, L.; Hänninen, T.; Jula, A.; et al. Effect of the Apolipoprotein E Genotype on Cognitive Change During a Multidomain Lifestyle Intervention: A Subgroup Analysis of a Randomized Clinical Trial. JAMA Neurol. 2018, 75, 462–470. [Google Scholar] [CrossRef]
- De Wolf, F.; Ghanbari, M.; Licher, S.; McRae-McKee, K.; Gras, L.; Weverling, G.J.; Wermeling, P.; Sedaghat, S.; Ikram, M.K.; Waziry, R.; et al. Plasma tau, neurofilament light chain and amyloid-β levels and risk of dementia; a population-based cohort study. Brain 2020, 143, 1220–1232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, D.; Mielke, M.M.; Bell, W.R.; Reilly, C.; Zhang, L.; Lin, F.V.; Yu, F. Blood biomarkers as surrogate endpoints of treatment responses to aerobic exercise and cognitive training (ACT) in amnestic mild cognitive impairment: The blood biomarkers study protocol of a randomized controlled trial (the ACT Trial). Trials 2020, 21, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burns, J.M.; Cronk, B.B.; Anderson, H.S.; Donnelly, J.E.; Thomas, G.P.; Harsha, A.; Brooks, W.M.; Swerdlow, R.H. Cardiorespiratory Fitness and Brain Atrophy in Early Alzheimer’s Disease. Neurology 2008, 71, 210–216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, F.; Heffner, K.L.; Ren, P.; Tivarus, M.E.; Brasch, J.; Chen, D.G.; Mapstone, M.; Porsteinsson, A.P.; Tadin, D. Cognitive and Neural Effects of Vision-Based Speed-of-Processing Training in Older Adults with Amnestic Mild Cognitive Impairment: A Pilot Study. J. Am. Geriatr. Soc. 2016, 64, 1293–1298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stephen, R.; Liu, Y.; Ngandu, T.; Antikainen, R.; Hulkkonen, J.; Koikkalainen, J.; Kemppainen, N.; Lötjönen, J.; Levälahti, E.; Parkkola, R.; et al. Brain volumes and cortical thickness on MRI in the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER). Alzheimer’s Res. Ther. 2019, 11, 53. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).